Introduction
As one of the most common anorectal diseases, the
incidence of anal fistula is reported to be ~3.6% (1). When the fistula involves more than
1/3 of the external sphincter and contains two or more external
mouths connected to the internal opening through the fistula or
complicated with branching fistulas, it is called an high complex
anal fistula (HCAF). Surgery is the primary treatment for the anal
fistula (2,3). The fistula of HCAF involves an
integral part of the sphincter complex [internal anal sphincter
(IAS) and external anal sphincter (EAS)]. Therefore, when the
sphincter is damaged, it may lead to anal incontinence (4). How to improve the cure rate of HCAF,
reduce the rate of postoperative complications and recurrence and
improve the quality of life of patients under the premise of
maximum preservation of anal sphincter function has always been one
of the main problems faced by anorectal surgeons and also one of
the key areas of current research.
Traditional surgery, such as anal fistulectomy, has
become the gold standard for anal fistula due to its high success
rate. However, it is easy to damage the anal sphincter and the anal
sphincter injury can lead to anal incontinence, so it is unsuitable
for HCAF (5). With the promotion
of the minimally invasive concept, sphincter-preserving surgery has
gradually received more attention. Although some sphincter-sparing
surgical procedures have emerged, such as ligation of
intersphincteric fistula tract (LIFT), video-assisted anal fistula
treatment (VAAFT), fistula laser closure (FiLaC) and anal fistula
plug (AFP) (6-8),
these surgical methods may markedly reduce the occurrence of
postoperative anal incontinence, but the cure rate is not
satisfactory.
In 2017, Garg (9)
proposed a new surgical method to treat HCAF and termed it the
transanal opening of intersphincteric space (TROPIS). Through the
transanal approach, the IAS part of the fistula is opened and the
EAS retained. It is reported that the postoperative cure rate of
TROPIS is 90.4% (9). However, as a
new surgical method, it inevitably needs more research data on
large samples and the long-term efficacy and safety need to be
further observed.
The present study aimed to evaluate the efficacy and
safety of the surgery by systematically searching the relevant
literature, collecting data and analyzing the cure rate and anal
incontinence rate following TROPIS.
Materials and methods
Search strategy
The Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) screening guidelines were followed,
while all the literature from inception through April 2024 was
searched in the electronic databases PubMed, Cochrane Library,
China National Knowledge Infrastructure and the Wanfang Database.
Articles assessing TROPIS were collected by including the following
keywords in combination with free words: ‘transanal opening of
intersphincteric space,’ ‘anorectal fistula,’ ‘fistula-in-ano,’
‘high anal fistula,’ ‘complex anal fistula,’ ‘rectal fistula,’
‘FIA’ and ‘TROPIS.’
Inclusion and exclusion criteria
The inclusion criteria were as follows: The disease
was diagnosed as HCAF; the surgical procedure was TROPIS; and
clinical research. The exclusion criteria were as follows: Studies
in which the demographic data of patients were incomplete and the
original data could not be extracted for statistical analysis;
republished literature; irrelevant articles, editorials, letters,
case reports, reviews and meta-analysis; and studies that did not
report the cure, complication and anal incontinence rates following
the operation.
Data extraction
Then two investigators screened the retrieved
studies independently according to the inclusion and exclusion
criteria and then cross-checked them. Controversial studies were
evaluated by a third party and unified by discussion. The two
investigators extracted relevant information from the included
studies, including first author, publication year, publication
country, sample size, age, sex, follow-up time, cure rate,
complication rate, management of recurrence and anal incontinence
score.
Procedure of TROPIS
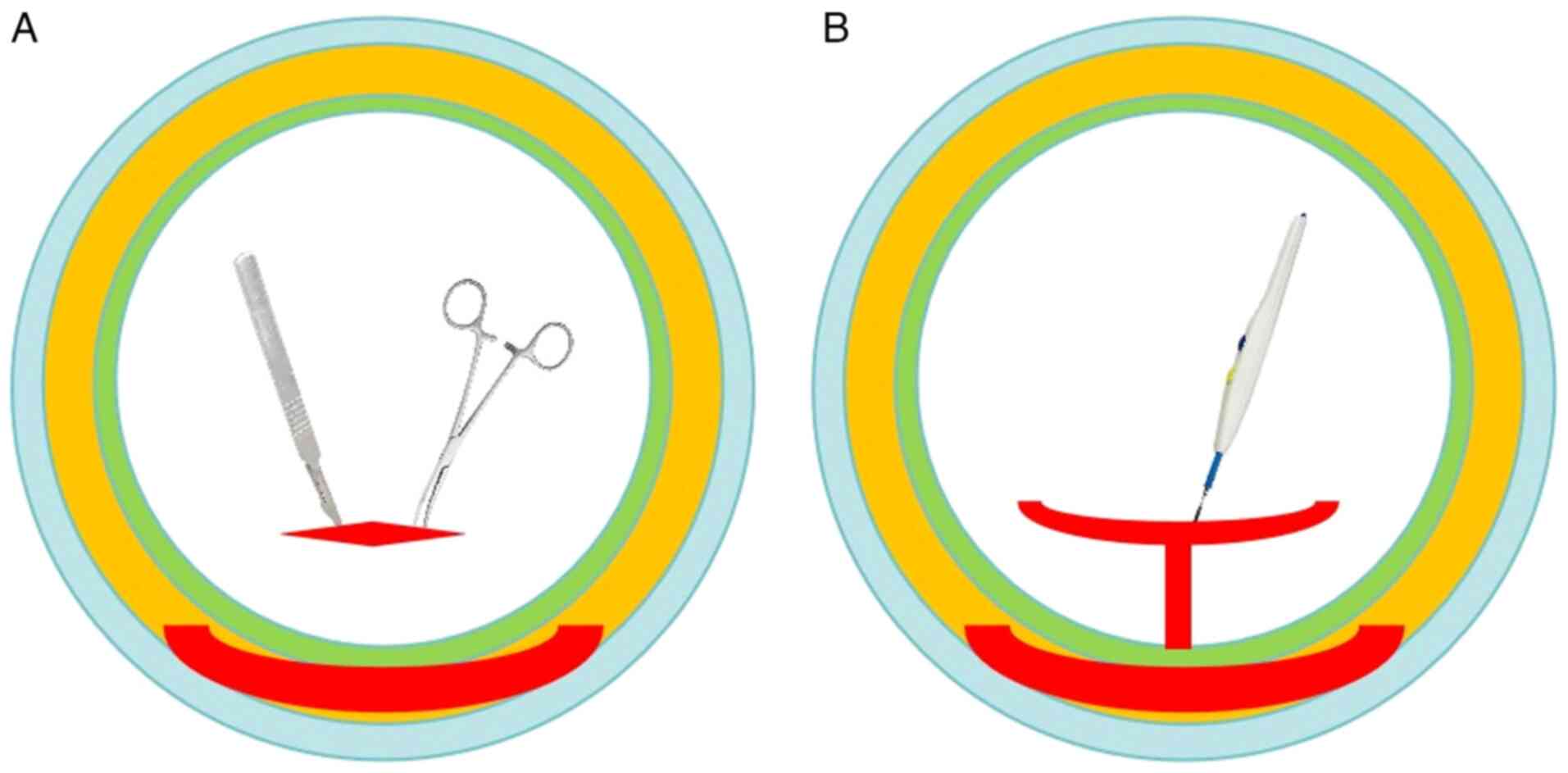
As shown in Fig. 1,
a curved artery forceps is inserted through the internal opening
into the intersphincteric part of the fistula tract. The mucosa and
the internal sphincter over the artery forceps are cut with
electrocautery. Thus, the intersphincteric space is opened into the
anal canal. This wound is left open to heal by secondary intention.
The lateral fistula tract (external) to the EAS can be managed by
any method convenient to the surgeon (including excision and
curettage) (9).
Statistical analysis
The present study performed statistical analysis
using the Cochrane Collaboration Revman 5.3. Dichotomous variables
are presented as risk differences (RD) and 95% confidence interval
(CI). Continuous variables were presented as mean differences (MD)
and 95% CI). Heterogeneity was evaluated by I2 tests.
Studies with values of I2>75% indicated substantial
heterogeneity, using the random effects model to estimate the
pooled OR or MD. Otherwise, the fixed effects model was adopted.
The Z test was used to determine the pooled OR and MD. Forest plots
were conducted to investigate possible bias. P<0.05 was
considered to indicate a statistically significant difference.
Results
Eligible studies
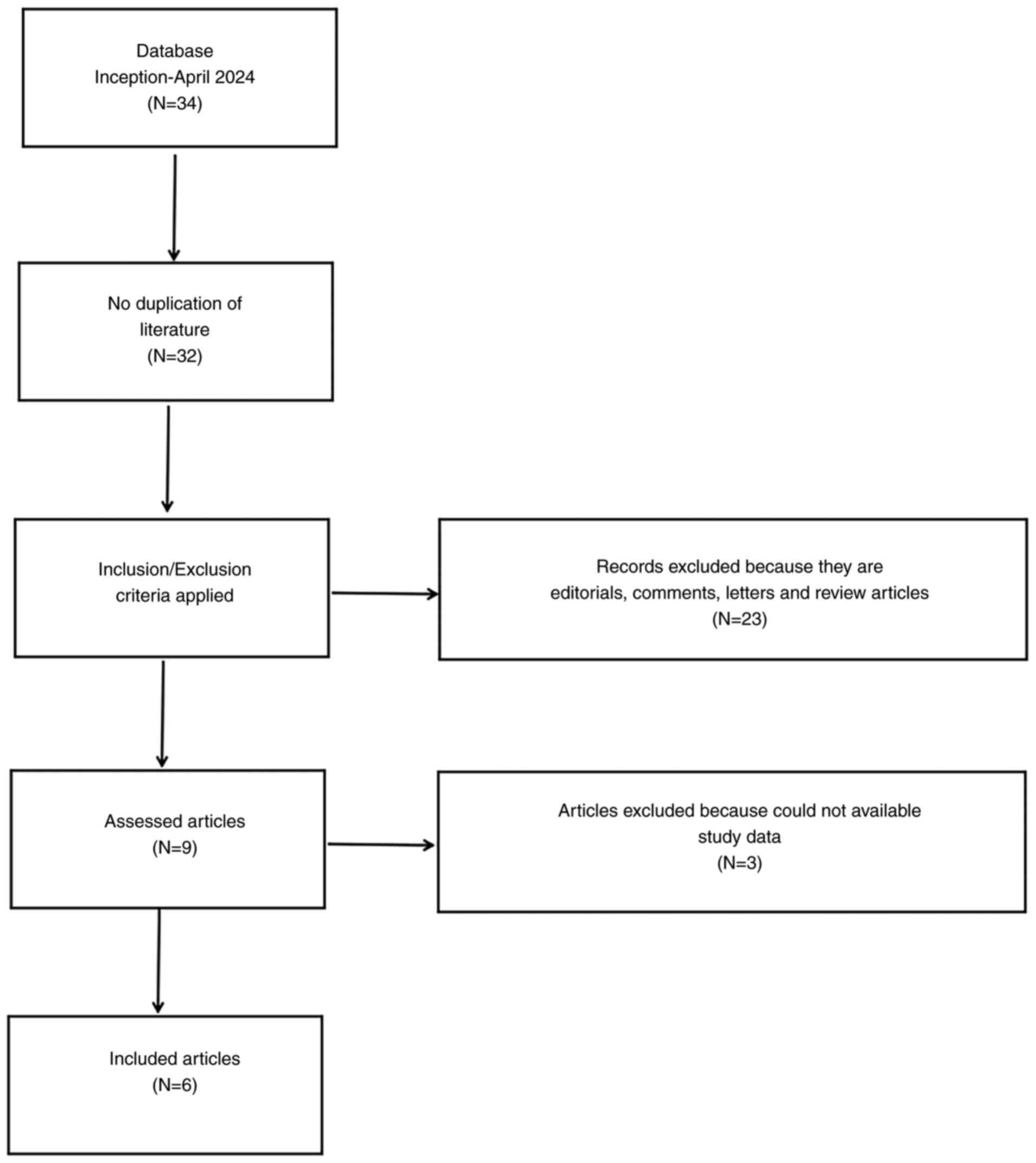
A total of 34 relevant articles were found in this
meta-analysis. By carefully reading the titles and abstracts and
screening the articles by inclusion and exclusion criteria, nine
reports were obtained and re-excluded by reading the complete text.
Finally, six articles (10-15)
were included in the present study. Specific retrieval and
screening process are shown in Fig.
2.
Primary characteristics of included
literature
A total of six articles, including 485 patients,
were included in this analysis. These articles were published
between 2021 and 2023, with four articles from China and two from
India. The primary characteristics of the included studies are
provided in Table I.
 | Table IPrimary characteristics of the
included studies. |
Table I
Primary characteristics of the
included studies.
| First author/s,
year | Country | Patients, n
(male/female) | Mean age,
years | Follow-up time
(months) | (Refs.) |
|---|
| Huang et al
(2021) | China | 48 (41/7) | 40±11.7 | 12 | (10) |
| Garg et al
(2021) | India | 306 | 39.9±10.9 | 36 | (11) |
| Mishra et al
(2023) | India | 35 (30/5) | 33.32±10.52 | 3 | (12) |
| Hou et al
(2022) | China | 27 (24/3) | 41.96±12.28 | 10.19 | (13) |
| Chen et al
(2022) | China | 28 (21/7) | 39.5±9.0 | 6.00 | (14) |
| Li et al
(2021) | China | 41 (35/6) | 38.6±13.2 | 22.2 | (15) |
Cure rate
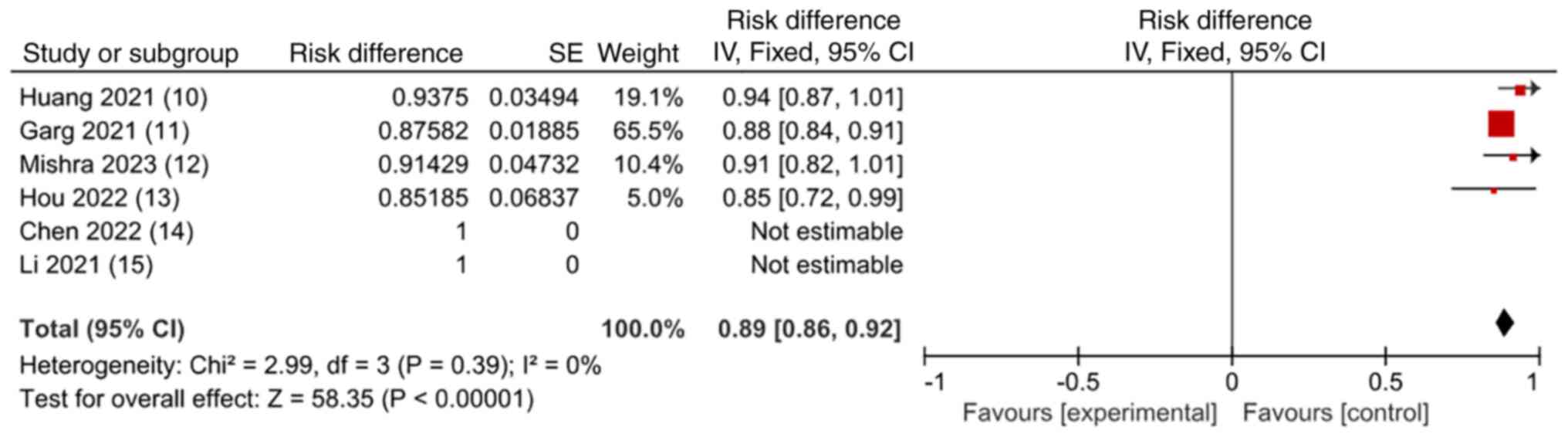
The six articles reported cure rates in HCAF. The
inverse variance statistical method was used to estimate the
fixed-effects model and the results showed that the weighted
average cure rate of each study was 89% (RD=0.89; 95% CI=0.86-0.92;
I2=0%; P<0.00001) as shown in Table II and Fig. 3.
 | Table IIHealing rate and management of
recurrence. |
Table II
Healing rate and management of
recurrence.
| First author/s,
year | Primary healing
rate (%) | Final healing rate
(%) | Management of
recurrence (n) | (Refs.) |
|---|
| Huang et al
(2021) | 87.5 | 93.8 (45/48) | TROPIS (6) | (10) |
| Garg et al
(2021) | 78.4 (240/306) | 87.6 (268/306) | TROPIS (35);
fistulatomy (1); no surgery (30) | (11) |
| Mishra et al
(2023) | 82.86 (29/35) | 91.4 (32/35) | Curettage (6) | (12) |
| Hou et al
(2022) | 85.19 | 85.19 (23/27) | Incision and
drainage (1) | (13) |
| Chen et al
(2022) | 100 | 100 (28/28) | No | (14) |
| Li et al
(2021) | 85.3 (35/41) | 100 (41/41) | Loose seton (2);
fistulatomy (4) | (15) |
Complications rate
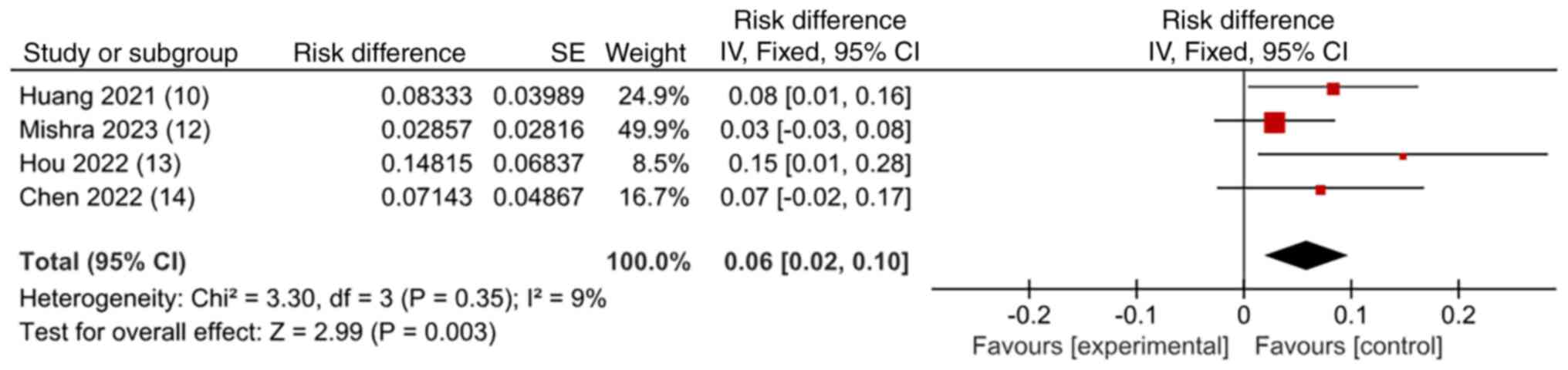
A total of four studies reported complication rates
in the HCAF. A total of 11 patients (8%) developed
postoperative-related complications, including four cases of
urinary retention (36.4% of the total complication rate), six cases
of bleeding (54.5% of the total complication rate) and one case of
incontinence to flatulence (9.1% of the total complication rate).
The inverse variance statistical method was used to estimate the
fixed-effects model and the results showed that the weighted
average complications rate of each study was 6% (RD=0.06, 95%;
CI=0.02-0.10; I2=9%; P=0.003) as shown in Table III and Fig. 4.
 | Table IIIComplications and type of
complication. |
Table III
Complications and type of
complication.
| First author/s,
year | Complications
(%) | Type of
complication (n) | (Refs.) |
|---|
| Huang et al
(2021) | 8.3 | Bleeding (3);
urinary retention (1) | (10) |
| Mishra et al
(2023) | 2.9 | Flatulent
incontinence (1) | (12) |
| Hou et al
(2022) | 14.8 | Bleeding (1);
urinary retention (3) | (13) |
| Chen et al
(2022) | 7.1 | Bleeding (2) | (14) |
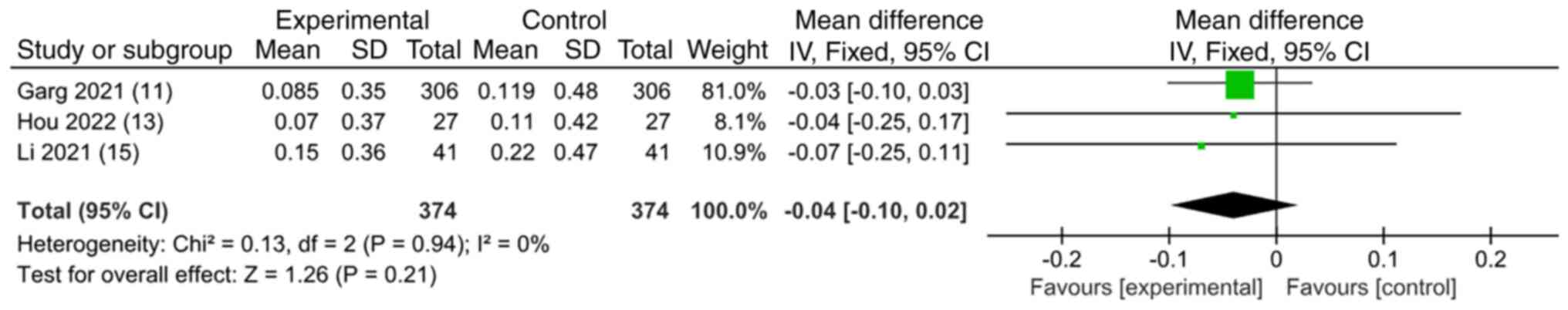
Anal incontinence rate
In three articles, including 374 patients, the anal
function score showed no heterogeneity in the preoperative vs.
postoperative (P=0.94; I2=0%). The inverse variance statistical
method and estimate of the fixed-effects model were used for
analysis (MD=-0.04; 95% Cl=-0.10 to 0.02; I2=0%;
P=0.21). Detailed data are shown in Table IV and Fig. 5.
 | Table IVAnal incontinence score. |
Table IV
Anal incontinence score.
| First author/s,
year | Anal incontinence
score (preoperative) | Anal incontinence
score (postoperative) | (Refs.) |
|---|
| Garg et al
(2021) | 0.085±0.35 | 0.119±0.48 | (11) |
| Hou et al
(2022) | 0.07±0.37 | 0.11±0.42 | (13) |
| Li et al
(2021) | 0.15±0.36 | 0.22±0.47 | (15) |
Discussion
HCAF is a refractory disease in colorectal anal
surgery. The main reasons for this are difficulty in understanding
the pathophysiology, risk of copracrasia and high recurrence rates
(16-18).
Since Eisenhammer (19) emphasized
the importance of the inner sphincter plane in the pathogenesis and
spread of the fistula in 1953, the role of the sphincter space in
the pathogenesis of the anal fistula is gaining increasing
recognition (20,21). Studies have found that sphincter
space infection is an important cause of the pathogenesis of most
complicated anal fistulas (22-24).
Therefore, recent research in the management of high complex
fistula has highlighted three essential principles: First, the
intersphincteric tract is like an abscess in a closed space (ISTAC)
and it is necessary to open it up and drain it adequately; second,
drain all pus and ensure continuous drainage (DRAPED) until the
wound is healed; third, remove the sinus tract as intact as
possible and simultaneously reduce the sphincter injury (16,22).
Although the surgical methods used to treat HCAF, such as LIFT,
VAAFT and fibrin glue, reduce the risk of anal sphincter injury,
they are not satisfactory regarding cure rate and recurrence rate
results. According to the relevant research reports, the cure rate
of LIFT is 76%, the cure rate of VAAFT is 76.01-82.3% and fibrin
glue in the treatment of complex anal fistula cure rate is even
less than 10% (25-29).
The overall cure rate is still suboptimal (30).
In view of the research on the theory of sphincter
space infection, the TROPIS surgical approach was proposed by Garg
(9) for the treatment of HCAF. In
2021, Garg et al (11)
reported the clinical efficacy of TROPIS in 306 HCAF, with a cure
rate of 87.6%. Although its good therapeutic effect has been
confirmed by a number of studies, as a new surgical method, it
inevitably lacks large samples and its long-term efficacy and
safety in HCAF need to be further observed (9).
A total of six articles, including 485 patients,
were included in the present study. The results showed that the
mean preoperative anal incontinence score was 0.061±0.22 and the
mean postoperative anal incontinence score was 0.09±0.27. There was
no statistically significant difference between the preoperative
and postoperative anal incontinence scores, indicating that the
anal sphincter function was well preserved in patients undergoing
TROPIS surgery. The leading cause of anal incontinence following
anal surgery is anal sphincter injury, especially EAS, which is
more critical than IAS (31).
TROPIS opens the fistulous sinus tract through the sphincter space
and although the external anal sphincter is preserved, the internal
anal sphincter is inevitably partly cut. As an essential part of
the muscles around the anal canal, the internal anal sphincter is
mainly responsible for maintaining the resting anal pressure. It
plays a vital role in anal self-control. The damage of IAS can lead
to anal incontinence, especially urge and flatulence incontinence
(32-34).
However, this type of anal incontinence is usually reversible. Some
studies have shown that cutting the internal anal sphincter and
opening the sphincter space fistula during anal fistula surgery is
safe and effective (35,36).
The analysis of the present study showed that the
weighted final healing rate of TROPIS was 89%. Improving the cure
rate of HCAF while avoiding anal incontinence has always been the
goal of anorectal doctors. Certain surgical methods, such as LIFT,
AFP, VAAFT and FiLaC, reduce the damage to the anal sphincter and
avoid the occurrence of anal incontinence to some extent. However,
AFP, VAAFT and FiLaC are not consistent with the ISTAC and DRAPED
principles and perhaps this is the reason why the postoperative
cure rate of these surgical methods is unsatisfactory (37). A recent comparative meta-analysis
of sphincter-sparing surgical procedures showed the highest cure
rate for TROPIS (38). For
complete healing of the fistula, all three components of the
fistula, internal opening, intersphincteric portion of the fistula
and the external tract in the ischiorectal fossa (the lateral part
of the fistula outside the external anal sphincter), need to be
totally healed.
Previous study hypothesized that inaccuracy or
inability in finding the internal orifice (IO) is the only
important reason for the recurrence of anal fistula (39). Most popular surgical methods, such
as LIFT, VAAFT and fibrin glue, all try to close the IO (29). However, recent studies have shown
that TROPIS has an improved therapeutic effect, even if the
location of the IO cannot be determined; this is a big advantage
that is different from other surgical methods. Garg et al
(40) found that TROPIS surgery in
546 patients (IO found) and 154 patients (IO not found) had roughly
the same cure rate (89 vs. 90.9%) and there was no significant
difference in postoperative anal incontinence scores between the
two groups. This was subsequently confirmed by Yagnik et al
(41) who showed that even if the
IO cannot be determined, the cure rate of TROPIS can reach
87.8%.
For HCAF, it is necessary to open the sphincter
space, maintain continuous drainage and remove the sinus tract as
completely as possible while reducing sphincter injury. LIFT
surgery ligates the fistula bundle in the sphincter space, accord
the ISTAC principle and it preserves the IAS and the EAS, which
greatly avoids the risk of anal incontinence (42). However, LIFT has high technical
requirements for the surgeon; how to correctly find the plane
between two sphincters (IAS and EAS) and identify the sinus tract
through the sphincter gap is a great challenge. In addition, since
the wound is primary healing, it can greatly shorten the recovery
time. However, it does not meet the DRAPED principle due to
incomplete handling of infected anal recess glands. In TROPIS,
direct incision of the IO and fistula involving the internal
sphincter is easy to operate without risk of entering the wrong
spatial plane of the sphincter. The wound is completely open with
continuous drainage and secondary healing, in line with the
principles of ISTAC and DRAPED. Of course, the TROPIS also has some
disadvantages, such as the long recovery time of secondary healing,
the partial incision of the IAS leading to the occurrence of anal
incontinence in the short term (although long-term follow-up shows
that anal incontinence does not deteriorate or become markedly
worse) (43).
A study suggested that sepsis is present in almost
all the sphincter spaces of an HCAF, presenting as an abscess in
the closed space, ignoring that this sepsis is one of the causes of
recurrence and that therefore the intersphincteric part of the
fistula should also be drained appropriately (23). In patients with acute fistula
abscess, inflammation causes swelling around the IO and blockage,
causing a clinically difficult examination (42). It has been reported that in up to
88% of patients cannot be accurately located the IO by doctors,
which is identified as a major bottleneck in the definitive
treatment of acute fistula abscess (44). When infection is present in the
sphincter space, the infection can easily induce local tissue
degeneration and necrosis and severe inflammatory response, and the
epidermis can regenerate only when the infection is controlled and
the necrotic tissue is cleared, which may be the reason for the
high healing rate of TROPIS in complex fistulas (11). A recent study showed that the cure
rate of TROPIS in acute fistula-abscess was 85.2% (155/182)
(41).
In the present meta-analysis, the weighted average
complication rate of TROPIS was 6%. Compared with other
postoperative complication rates such as LIFT (13.9%) and VAAFT
(11%), the rate of postoperative complications after TROPIS is low
and acceptable to patients and surgeons (29,45).
Of 138 patients in the present study, only four had postoperative
urinary retention, six had postoperative bleeding and one had
flatulence incontinence. This may be related to incomplete
intraoperative hemostasis and poor postoperative management and has
no apparent relationship with the surgical technique. Moreover,
most of these complications were mild and did not cause significant
adverse effects on the patients.
Limitations of the present study may affect the
results and conclusions of the analysis. First, the main limitation
was the small number of articles and patients included. In
addition, since the study statistics of Garg et al (11) accounted for >50% of the total
analysis, this may bias the results of the present study. Second,
the short follow-up of patients in most included studies prevents
drawing any firm conclusions on the long-term outcome of the
technique. Therefore further prospective studies are required.
However, despite its limitations, the present study provided a
reference value for subsequent analyses.
The present study found that TROPIS surgery is a
sphincter-sparing procedure that deserves further investigation.
TROPIS has a high cure rate, a favorable anal incontinence score,
few types of postoperative complications and a low complication
rate. It can be used as a minimally invasive and
sphincter-preserving surgical method for treating HCAF. It is
worthy of further promotion and research in clinical practice.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
TH and XW participated in the whole process of
literature selection, inclusion, quality evaluation and bias risk
assessment. CW conducted data analysis, article writing and table
and figure production. CW and TH confirm the authenticity of all
the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Felt-Bersma RJ and Bartelsman JF:
Haemorrhoids, rectal prolapse, anal fissure, peri-anal fistulae and
sexually transmitted diseases. Best Pract Res Clin Gastroenterol.
23:575–592. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cooper CR and Keller DS: Response to
letter to the editor on ‘Resident's Corner: Perianal Fistulas’. Dis
Colon Rectum. 63(e515)2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ribaldone DG, Resegotti A, Pellicano R,
Astegiano M, Saracco GM and Morino M: The role of topical therapy
for perianal fistulizing Crohn's disease: Are we forgetting
something? Minerva Gastroenterol Dietol. 65:130–135.
2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Garg P, Sodhi SS and Garg N: Management of
complex cryptoglandular anal fistula: Challenges and solutions.
Clin Exp Gastroenterol. 13:555–567. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abramowitz L, Soudan D, Souffran M,
Bouchard D, Castinel A, Suduca JM, Staumont G, Devulder F, Pigot F,
Ganansia R, et al: The outcome of fistulotomy for anal fistula at 1
year: A prospective multicentre French study. Colorectal Dis.
18:279–285. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Regusci L, Fasolini F, Meinero P, Caccia
G, Ruggeri G, Serati M and Braga A: Video-Assisted anal fistula
treatment (VAAFT) for complex anorectal fistula: Efficacy and risk
factors for failure at 3-year follow-up. Tech Coloproctol.
24:741–746. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Narang SK, Keogh K, Alam NN, Pathak S,
Daniels IR and Smart NJ: A systematic review of new treatments for
cryptoglandular fistula in ano. Surgeon. 15:30–39. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lin H, Jin Z, Zhu Y, Diao M and Hu W: Anal
fistula plug vs rectal advancement flap for the treatment of
complex cryptoglandular anal fistulas: A systematic review and
meta-analysis of studies with long-term follow-up. Colorectal Dis.
21:502–515. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Garg P: Transanal opening of
intersphincteric space (TROPIS)-A new procedure to treat high
complex anal fistula. Int J Surg. 40:130–134. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Huang B, Wang X, Zhou D, Chen S, Li B,
Wang Y and Tai J: Treating highly complex anal fistula with a new
method of combined intraoperative endoanal ultrasonography (IOEAUS)
and transanal opening of intersphincteric space (TROPIS). Wideochir
Inne Tech Maloinwazyjne. 16:697–703. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Garg P, Kaur B and Menon GR: Transanal
opening of the intersphincteric space: A novel sphincter-sparing
procedure to treat 325 high complex anal fistulas with long-term
follow-up. Colorectal Dis. 23:1213–1224. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mishra S, Thakur DS, Somashekar U, Verma A
and Sharma D: The management of complex fistula in ano by transanal
opening of the intersphincteric space (TROPIS): Short-term results.
Ann Coloproctol: Mar 31, 2023 (Epub ahead of print).
|
|
13
|
Hou XT, Chen H, Chen YN and Zhang R:
Transanal opening of intersphincteric space to treat complex anal
fistula. Mod Med J. 50:588–591. 2022.
|
|
14
|
Chen XQ, Ren YY, Li YY, Sun F, Zhao YC and
Jin X: Clinical efficacy of anal sphincter otomy (TROPIS) in the
treatment of high sphincter type anal fistula. Journal of
Colorectal & Anal Surgery. 28:479–487. 2022.(In Chinese).
|
|
15
|
Li YB, Chen JH, Wang MD, Fu J, Zhou BC, Li
DG, Zeng HQ and Pang LM: Transanal opening of intersphincteric
space for Fistula-in-Ano. Am Surg. 88:1131–1136. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wlodarczyk M, Wlodarczyk J,
Sobolewska-Wlodarczyk A, Trzcinski R, Dziki L and Fichna J: Current
concepts in the pathogenesis of cryptoglandular perianal fistula. J
Int Med Res. 49(300060520986669)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jeong HY, Song SG, Nam WJ and Lee JK:
puborectalis muscle involvement on magnetic resonance imaging in
complex fistula: A new perspective on diagnosis and treatment. Ann
Coloproctol. 37:51–57. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jayne DG, Scholefield J, Tolan D, Gray R,
Senapati A, Hulme CT, Sutton AJ, Handley K, Hewitt CA, Kaur M, et
al: A multicenter randomized controlled trial comparing safety,
efficacy and cost-effectiveness of the surgisis anal fistula plug
versus surgeon's preference for transsphincteric Fistula-in-Ano:
The FIAT Trial. Ann Surg. 273:433–441. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Eisenhammer S: The internal anal
sphincter; its surgical importance. S Afr Med J. 27:266–270.
1953.PubMed/NCBI
|
|
20
|
Garcia-Aguilar J, Belmonte C, Wong WD,
Goldberg SM and Madoff RD: Anal fistula surgery. Factors associated
with recurrence and incontinence. Dis Colon Rectum. 39:723–729.
1996.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Jordan J, Roig JV, Garcia-Armengol J,
Garcia-Granero E, Solana A and Lledo S: Risk factors for recurrence
and incontinence after anal fistula surgery. Colorectal Dis.
12:254–260. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Garg P: A new understanding of the
principles in the management of complex anal fistula. Med
Hypotheses. 132(109329)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Garg P: Intersphincteric component in a
complex Fistula-in-Ano is like an abscess and should be treated
like one. Dis Colon Rectum. 61(e26)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhang H, Zhou ZY, Hu B, Liu DC, Peng H,
Xie SK, Su D and Ren DL: Clinical significance of 2 deep posterior
perianal spaces to complex cryptoglandular fistulas. Dis Colon
Rectum. 59:766–774. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Emile SH, Elfeki H, Shalaby M and Sakr A:
A Systematic review and meta-analysis of the efficacy and safety of
video-assisted anal fistula treatment (VAAFT). Surg Endosc.
32:2084–2093. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Gottgens KW, Smeets RR, Stassen LP, Beets
G and Breukink SO: Systematic review and meta-analysis of surgical
interventions for high cryptoglandular perianal fistula. Int J
Colorectal Dis. 30:583–593. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cestaro G, De Rosa M and Gentile M:
Treatment of fistula in ano with fibrin glue: Preliminary results
from a prospective study. Minerva Chir. 69:225–228. 2014.PubMed/NCBI
|
|
28
|
Damin DC, Rosito MA, Contu PC and Tarta C:
Fibrin glue in the management of complex anal fistula. Arq
Gastroenterol. 46:300–303. 2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Emile SH, Khan SM, Adejumo A and Koroye O:
Ligation of intersphincteric fistula tract (LIFT) in treatment of
anal fistula: An updated systematic review, meta-analysis and
meta-regression of the predictors of failure. Surgery. 167:484–492.
2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Prosst RL and Joos AK: Short-term outcomes
of a novel endoscopic clipping device for closure of the internal
opening in 100 anorectal fistulas. Tech Coloproctol. 20:753–758.
2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Matos D, Lunniss PJ and Phillips RK: Total
sphincter conservation in high fistula in ano: Results of a new
approach. Br J Surg. 80:802–804. 1993.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sainio P: A manometric study of anorectal
function after surgery for anal fistula, with special reference to
incontinence. Acta Chir Scand. 151:695–700. 1985.PubMed/NCBI
|
|
33
|
Soltani A and Kaiser AM: Endorectal
advancement flap for cryptoglandular or Crohn's fistula-in-ano. Dis
Colon Rectum. 53:486–495. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Uribe N, Balciscueta Z, Minguez M, Martin
MC, Lopez M, Mora F and Primo V: ‘Core out’ or ‘curettage’ in
rectal advancement flap for cryptoglandular anal fistula. Int J
Colorectal Dis. 30:613–619. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Omar W, Alqasaby A, Abdelnaby M, Youssef
M, Shalaby M, Anwar Abdel-Razik M and Emile SH: Drainage seton
versus external anal sphincter-sparing seton after rerouting of the
fistula tract in the treatment of complex anal fistula: A
randomized controlled trial. Dis Colon Rectum. 62:980–987.
2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
El-Said M, Emile S, Shalaby M, Abdel-Razik
MA, Elbaz SA, Elshobaky A, Elkaffas H and Khafagy W: Outcome of
Modified Park's technique for treatment of complex anal fistula. J
Surg Res. 235:536–542. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Garg P, Song J, Bhatia A, Kalia H and
Menon GR: The efficacy of anal fistula plug in fistula-in-ano: A
systematic review. Colorectal Dis. 12:965–970. 2010.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Garg P, Kaur B, Goyal A, Yagnik VD, Dawka
S and Menon GR: Lessons learned from an audit of 1250 anal fistula
patients operated at a single center: A retrospective review. World
J Gastrointest Surg. 13:340–354. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Mei Z, Wang Q, Zhang Y, Liu P, Ge M, Du P,
Yang W and He Y: Risk Factors for Recurrence after anal fistula
surgery: A meta-analysis. Int J Surg. 69:153–164. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Garg P, Kaur B, Singla K, Menon GR and
Yagnik VD: A simple protocol to effectively manage anal fistulas
with no obvious internal opening. Clin Exp Gastroenterol. 14:33–44.
2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yagnik VD, Kaur B, Dawka S, Sohal A, Menon
GR and Garg P: Non-Locatable internal opening in anal fistula
associated with acute abscess and its definitive management by garg
protocol. Clin Exp Gastroenterol. 15:189–198. 2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Rojanasakul A, Booning N, Huimin L,
Pongpirul K and Sahakitrungruang C: Intersphincteric exploration
with ligation of intersphincteric fistula tract or attempted
closure of internal opening for acute anorectal abscesses. Dis
Colon Rectum. 64:438–445. 2021.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Garg P: Comparison between recent
sphincter-sparing procedures for complex anal fistulas-ligation of
intersphincteric tract vs transanal opening of intersphincteric
space. World J Gastrointest Surg. 14:374–382. 2022.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Tang CL, Chew SP and Seow-Choen F:
Prospective randomized trial of drainage alone vs. drainage and
fistulotomy for acute perianal abscesses with proven internal
opening. Dis Colon Rectum. 39:1415–1417. 1996.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Tian Z, Li YL, Nan SJ, Xiu WC and Wang YQ:
Video-assisted anal fistula treatment for complex anorectal
fistulas in adults: A systematic review and meta-analysis. Tech
Coloproctol. 26:783–795. 2022.PubMed/NCBI View Article : Google Scholar
|