Introduction
A mixed epithelial and stromal tumor (MEST) is a
rare neoplasm of the kidney, representing a small fraction of renal
tumors, typically occurring in perimenopausal women (female:male
ratio, 7:1) (1,2). The exact incidence rate is not well
documented due to its rarity. Most of the data on MEST comes from
case reports and small case series rather than large
epidemiological studies. Research is generally limited to
retrospective analyses and case series in the medical literature,
describing ~100 cases to date. There are no large-scale registries
dedicated to tracking MEST specifically, which makes global
incidence rates difficult to determine accurately (1,2).
According to the World Health Organization, MESTs
are characterized by a combination of both epithelial cysts and
solid component of spindle-shaped cells (3). A number of studies indicate that
MESTs are correlated with usage of hormonal therapy both in males
and females (4-6).
Most cases of MEST are benign, and complete surgical resection is
often curative (7,8). However, rare cases of malignant
transformation have been reported (4,9,10),
with one case reported in a pediatric transplant patient (11), highlighting the importance of close
follow-up in patients diagnosed with MEST. The prognosis for MEST
is generally favorable, especially in cases where the tumor is
completely excised and it demonstrates no evidence of malignancy
(3-10).
In the present case report, MEST with
myopericytoma/myofibroma as a stromal component is presented,
which, according to the best of our knowledge, is the first
described case in the literature.
Case report
A 75-year-old male patient was admitted to the
Clinic of Urology, University Clinical Center of Serbia (Belgrade,
Serbia), in January 2024 for surgery due to the incidental finding
of a kidney tumor during an ultrasound scan (USS) of the abdominal
cavity, which was performed at a yearly routine check-up. The
patient did not have any clinical symptoms or signs of disease.
Laboratory findings and urine analysis were within the normal
ranges. Kidney function was preserved, and none of the tested tumor
marker levels were elevated (Table
SI). From the USS, the tumor was described as a nodular mass
that was partly cystic and partly solid on the upper pole of the
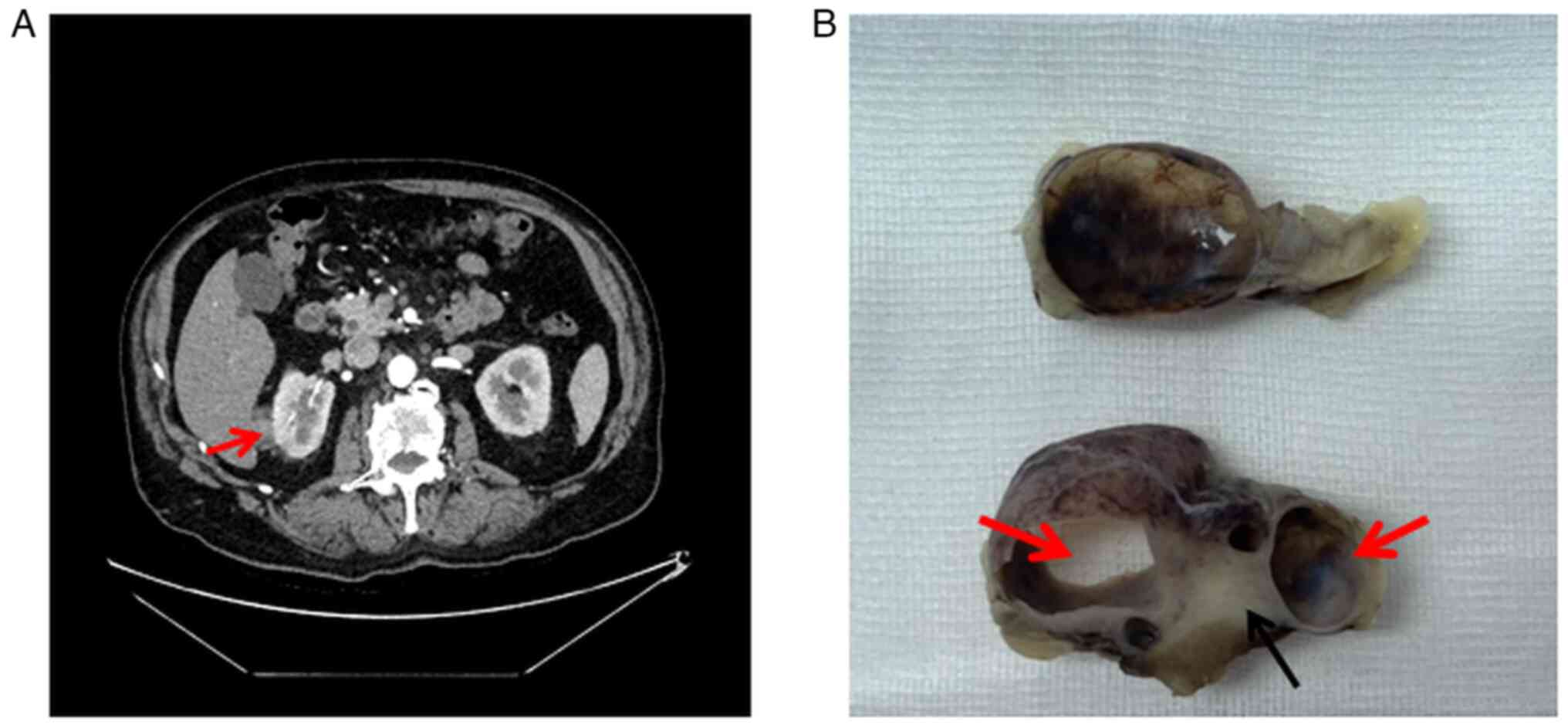
right kidney. On the computed tomography scan (CT), interpolar
towards the upper half of the right kidney, a partly solid, partly
cystic elongated structure was observed with a maximum diameter of
54 mm along the coronal plane. The soft-tissue component of this
structure was opacified by the contrast agent and disrupted the
lateral contour of the kidney, and was classified as Bosniak grade
IV (Fig. 1A), according to Bosniak
Classification of Cystic Renal Masses, Version 2019(12). A partial nephrectomy was performed
due to the position of the tumor and accessibility for surgery. On
gross section (Fig. 1B), the tumor
was 26 mm at the maximal diameter, with a partially cystic and
partially solid appearance, as previously seen on CT.
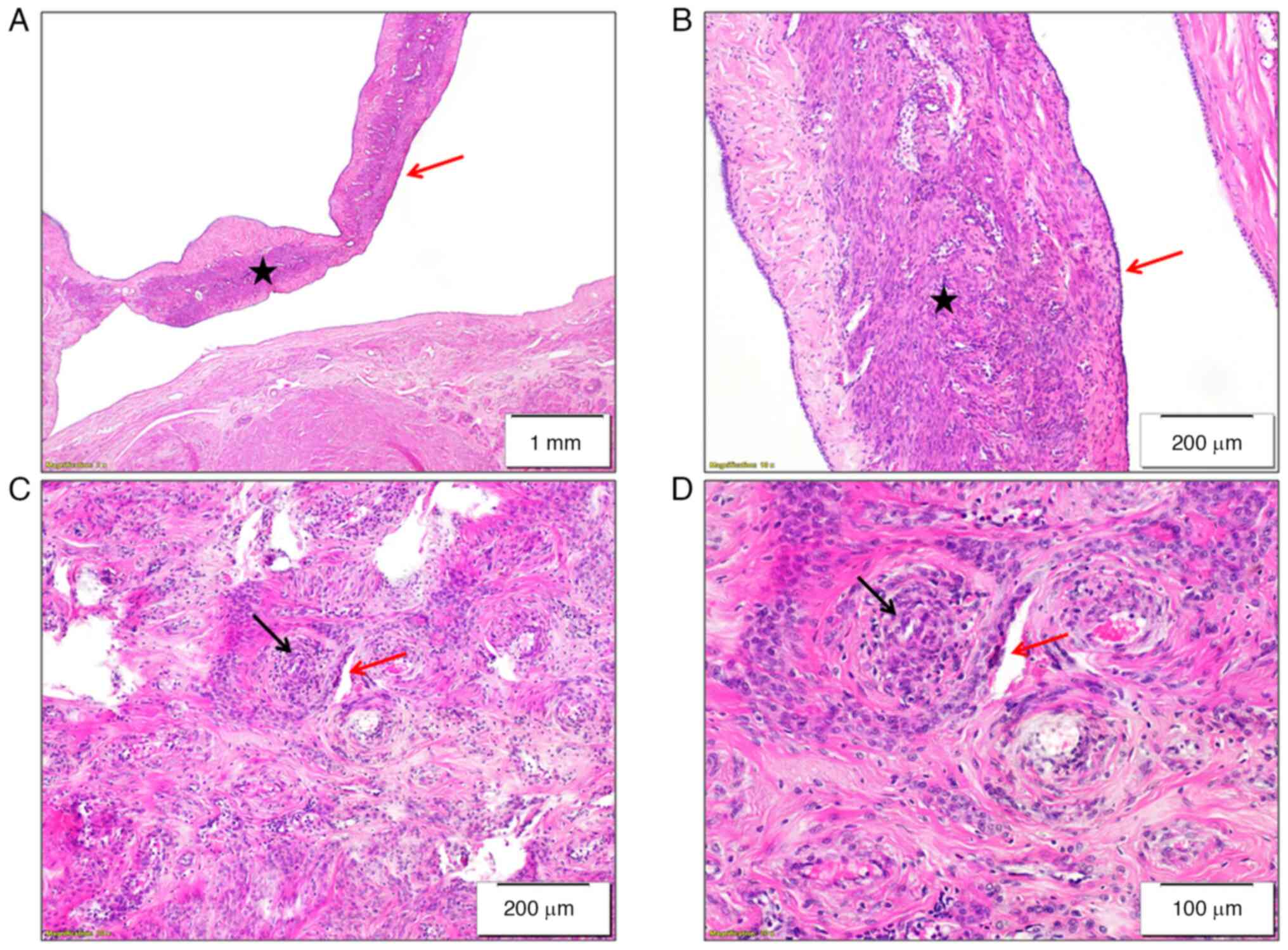
Microscopically, the tumor was composed of cysts
lined with a single layer of cuboidal cells, surrounded with
ovarian-like stroma. Sharp demarcation between the cystic component
and solid component was observed. The solid component of the tumor
consisted of bundles of elongated cells with eosinophilic
cytoplasm, oval nuclei without atypia and exhibited angiocentric
growth. Nuclear atypia and mitoses were not observed. Focally, a
ribbon-like hyalinized matrix was present between the cells. The
number of small blood vessels was increased, which were small and
with slit-like lumina (Fig.
2).
Immunohistochemistry was performed on formalin
fixed-paraffin embedded tissue according to the established
protocol: Addition of formalin for 24 h at room temperature (RT),
96% ethanol for 24 h at RT, 100% ethanol for 8 h at RT and xylene
for 12 h at RT, before paraffin fixation at 52-54˚C for 24 h, and
embedding with paraffin at 58˚C. The slides were cut into 4-µm
thick sections. Protocols for immunostaining and the list of
antibodies are provided in Table
SII. All antigen retrieval procedures were performed in an
automated manner using Thermo Scientific PT MODULE (Thermo
Scientific, Inc.) and DAKO PT Link (Dako; Agilent Technologies,
Inc.) for subsequent staining in corresponding automated
immunostainers: Thermo Scientific Lab Vision Autostainer 360
[detection system: Epredia-UltraVision Quanto Detection System HRP
DAB (REF TL-125-QHD)] and DAKO Autostainer Link 48 [detection
system: Agilent Technologies-EnVision FLEX High pH (Link) (REF
K8000)]. Moreover, the Ventana BenchMark Ultra was used, as a known
closed system containing antigen retrieval procedures (ultraView
Universal DAB Detection Kit) and staining steps together. Finally,
slides from the automated strainers were removed and dehydrated
using 96 and 100% ethanol, xylene and 100% ethanol (1:1), and
xylene, and covered with coverslips using Canada balsam.
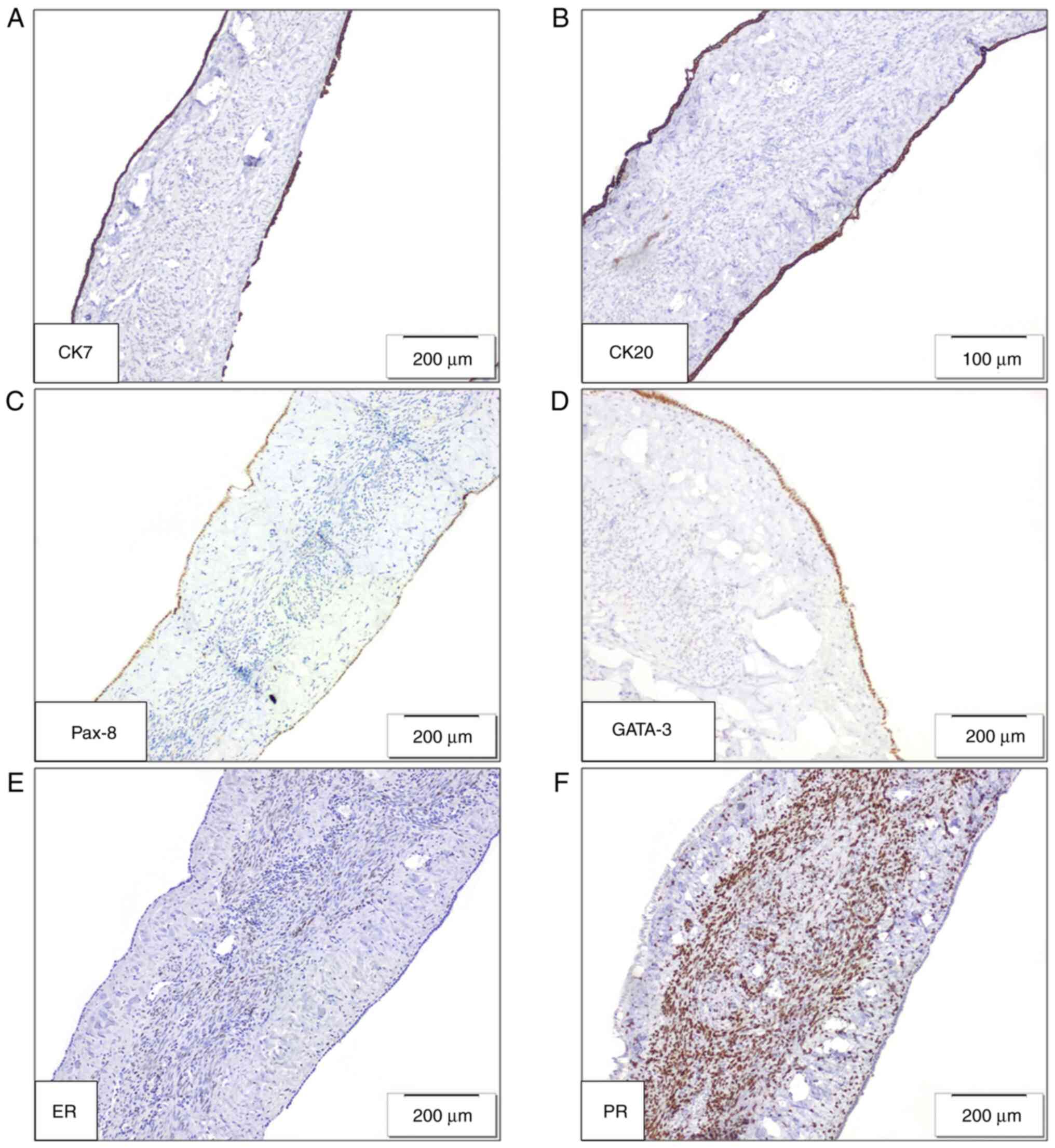
The epithelial components demonstrated diffuse
positive staining for CK7, CK20, Pax-8, GATA-3, estrogen receptor
(ER) and progesterone receptor (PR) (Fig. 3). The stromal component
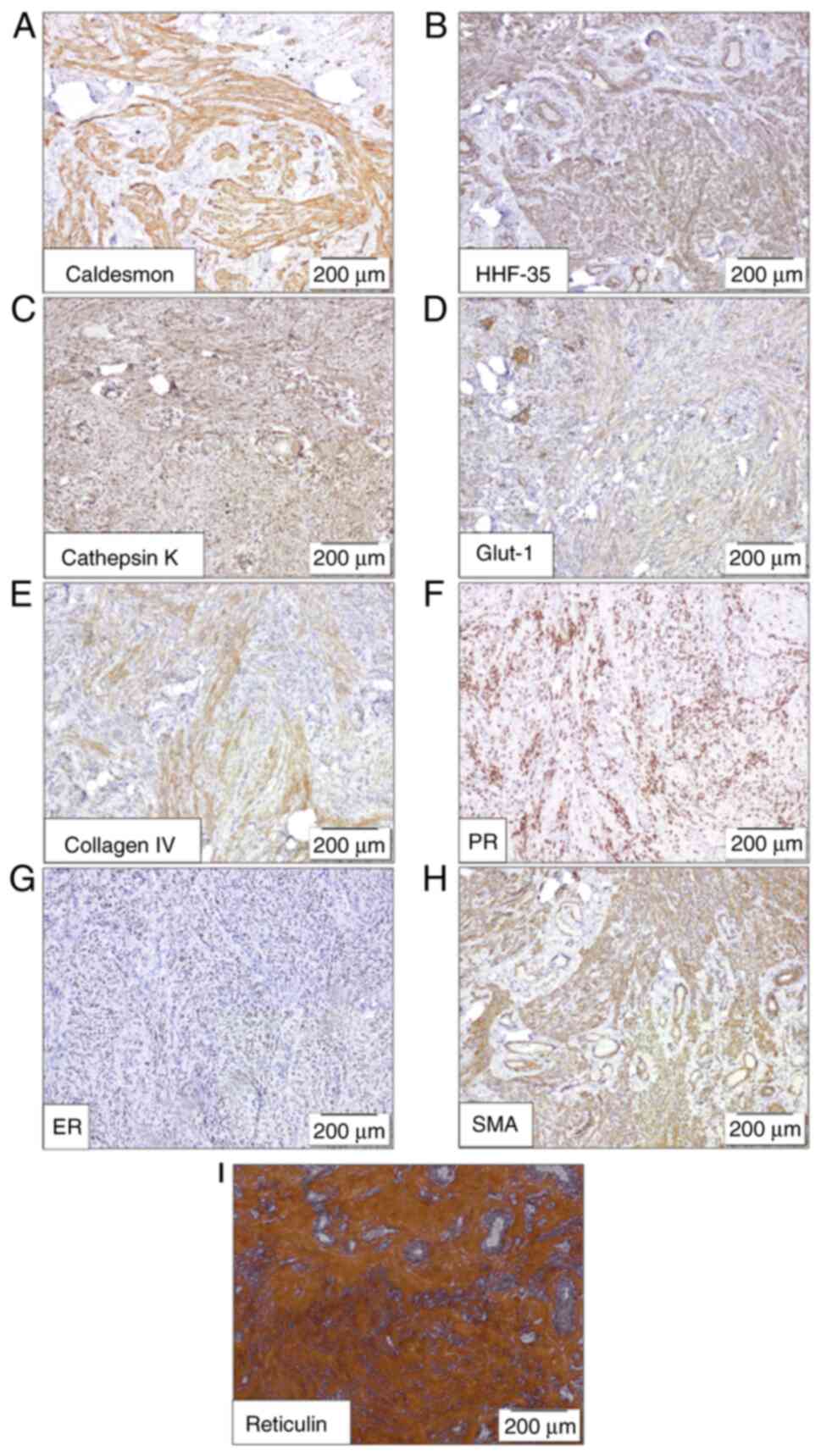
demonstrated immunopositivity for Caldesmon, muscle-specific actin
(HHF-35), cathepsin K, Glut-1, Collagen IV, PR (diffusely), ER
(focally) and smooth muscle actin (SMA) (Fig. 4A-H). Furthermore, histochemical
staining demonstrated diffuse positive staining for reticulin,
performed using a Reticulin Contrast kit (cat. no. RET-100T; Lot
no. RET-163-1/23; BioGnost, Ltd.) according to the manufacturer's
instructions (Fig. 4I). A lack of
staining was found for desmin, along with a lack of staining for
CD34, CD31 and CD99, excluding leiomyoma differentiation (Fig. S1). Finally, the diagnosis of MEST
with myopericytoma/myofibroma differentiation of the stromal
component was made, based on the specific immunohistochemical
findings.
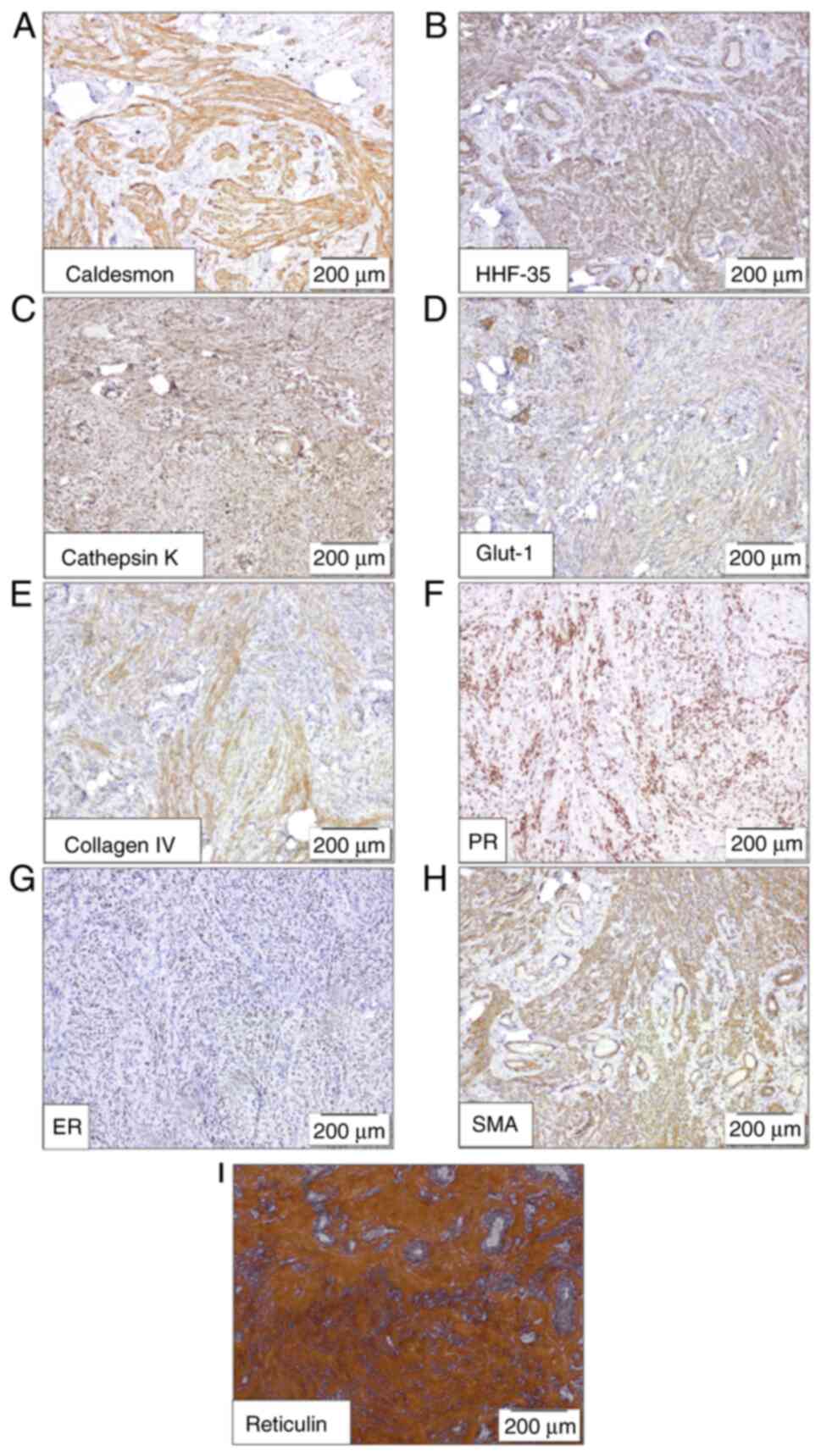 | Figure 4Solid component of the mixed
epithelial and stromal tumor. Immunohistochemical and histochemical
staining demonstrated diffuse positive staining for (A) caldesmon,
(B) HHF-35, (C) cathepsin K, (D) Glut 1, (E) collagen IV, (F) PR
and (G) ER, (H) SMA, (I) reticulin.. PR, progesterone receptor; ER,
estrogen receptor; Glut-1, solute carrier family 2 facilitated
glucose transporter member 1; HHF-35, muscle-specific actin; SMA,
smooth muscle actin. |
At the time of writing, 4 months after the partial
nephrectomy, the patient had recovered completely without any
complications. The first postoperative imaging will be performed 6
months after surgery.
Discussion
MESTs of the kidney are rare neoplasms that occur
mostly in women (13), and ~25% of
known diagnosed MESTs are asymptomatic. Long-term hormonal
treatment has been suggested to be involved in MEST development
(1-30).
In the present case study, the patient was male with no history of
hormonal exposure. MESTs are characterized by a combination of both
epithelial and stromal elements within the tumor tissue, usually
presenting as a well-circumscribed mass, often with a cystic
component (15). The histological
features of MESTs include epithelial structures such as cysts lined
by cuboidal or flat epithelial cells, with ovarian-like stroma
between cysts, and a stromal component mostly described as spindle
cells resembling leiomyoma (16).
Immunohistochemical staining can aid in the diagnosis of MEST, with
epithelial components typically positive for CKs, such as CK7 and
CK20, and stromal components typically positive for smooth muscle
markers, such as SMA and desmin (15).
Karafin et al (19) reported that the epithelium in MESTs
highly expresses Pax-2/Pax-8, while generally lacking ER markers.
This pattern suggests that the epithelial aspect of MEST might be
undergoing a form of renal tubular differentiation, altering its
structure and cellular characteristics in tandem with the stromal
part of the tumor. The precise nature of this epithelial component,
whether it is simply trapped renal tubule cells or an aspect of the
malignancy of the tumor remains uncertain. In the present case
report, the epithelial component stained positive for Pax-8/Pax-2,
but also demonstrated positive staining for ER. Furthermore, the
histomorphological characteristics of the stromal component
demonstrated myopericyte differentiation, which was
immunohistochemically confirmed with the positive staining for SMA,
HHF-35, Caldesmon, ER, PR, Glut-1, reticulin and collagen IV, and
the negative staining for desmin, CD31, CD34 and CD99.
Angiomyolipoma with epithelial cysts is primarily
composed of smooth muscle and lacks notable fat content (19,20);
it also features epithelial cysts and contains a combination of
solid and cystic structures (21).
Therefore, both angiomyolipoma with epithelial cysts and MEST
lesions share similar morphological characteristics. However, the
presence of melanocytic markers in angiomyolipoma with epithelial
cysts (21,22), which are absent in MEST (23), serves as a distinguishing feature
between these two types of lesions (19-23).
Cystic nephroma (CN) is another neoplasm that shares
similar characteristics with MEST (1,24).
In the World Health Organization Classification of Tumors of the
Urinary System and Male Genital Organs from 2022, CN in adults is
described as subtype of MEST but with distinguishable
characteristics, while on the other hand, CN in the pediatric
population is classified as a separate entity altogether (1). CN is a predominantly cystic tumor
composed entirely of differentiated tissues without solid
components (25).
Compared with MEST, CN contains larger cysts,
thinner septa and a lower stromal to epithelial ratio (26). Likewise, it has been reported that
all CN have mutations in the DICER1 gene, in contrast to
MESTs (1). Moreover, the exact
etiology of MESTs is unclear, but hormonal factors, as well as
obesity, may serve a role in their development (28). However, the present patient had no
history of hormone usage or obesity problems.
In conclusion, most cases of MEST are benign and
complete surgical resection is often curative. However, rare cases
of malignant transformations have been reported, highlighting the
importance of close follow-up in patients diagnosed with MEST,
particularly those with described transformations, due to the
aggressive progression and worse prognosis (18). Finally, considering that, to the
best of our knowledge, myopericytoma/myofibroma as a stromal
differentiation component in MEST was described for the first time
in the present case study, a close follow-up is warranted, since
the biological behavior is not well established.
Supplementary Material
Immunohistochemical stains of (A)
CD34, (B) CD31, (C) CD99 and (D) desmin were negative in the solid
component of the MEST, with an internal positive control for CD34
and CD31 in the endothelium.
Laboratory findings at the time of
surgery.
Immunohistochemistry procedure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
GN, AM and LS wrote the manuscript. GN, AM, LS, JS,
LC, MZ and MJ obtained data and made substantial contributions to
the conception and design of the manuscript. GN, VM, LS, JS, LC, JJ
and MZ performed the microscopic examination of the tissues,
obtained data and made substantial contributions to the
interpretation of data. GN, LS, MZ, MJ, JJ and SRS performed the
histopathology examination. GN and SRS confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
participation in the case report.
Patient consent for publication
The patient provided written informed consent for
the publication of any data and/or accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization. Urinary and
Male Genital Tumours. In: WHO Classification of Tumours. 5th
Edition. Volume 8. International Agency for Research on Cancer,
Lyon, 2022.
|
|
2
|
Caliò A, Eble JN, Grignon DJ and Delahunt
B: Mixed epithelial and stromal tumor of the kidney: A
clinicopathologic study of 53 cases. Am J Surg Pathol.
40:1538–1549. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zhou M and Magi-Galluzzi C: Genitourinary
pathology: A volume in the series: Foundations in diagnostic
pathology. Elsevier Health Sciences; 2013.
|
|
4
|
Adsay NV, Eble JN, Srigley JR, Jones EC
and Grignon DJ: Mixed epithelial and stromal tumor of the kidney.
Am J Surg Pathol. 24:958–970. 2000.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Suzuki T, Hiragata S, Hosaka K, Oyama T,
Kuroda N, Hes O and Michal M: Malignant mixed epithelial and
stromal tumor of the kidney: Report of the first male case. Int J
Urol. 20:448–450. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhou M, Kort E, Hoekstra P, Westphal M,
Magi-Galluzzi C, Sercia L, Lane B, Rini B, Bukowski R and Teh BT:
Adult cystic nephroma and mixed epithelial and stromal tumor of the
kidney are the same disease entity: Molecular and histologic
evidence. Am J Surg Pathol. 33:72–80. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sun BL, Abern M, Garzon S and Setty S:
Cystic nephroma/mixed epithelial stromal tumor: A benign neoplasm
with potential for recurrence. Int J Surg Pathol. 23:238–242.
2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zam NA, Lau WK, Yip SK, Cheng CW and Tan
PH: Mixed epithelial and stromal tumour (MEST) of the kidney: A
clinicopathological report of three cases. Pathology. 41:403–406.
2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Holkar PS, Jain T, Kavishwar V and Pandya
JS: Metastasis in mixed epithelial stromal tumour of the kidney: A
rare presentation. BMJ Case Rep. 12(e229293)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dan C, Sahai A, Suri P, Singh J and Trehan
RS: Mixed epithelial stromal tumor of the kidney with a mesenteric
lymph node: A case report and literature review. Cureus.
27(e46058)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ferdjallah A, Gordon P, Kirankumar V,
Dietz K, Bu L and Verghese P: Mixed epithelial and stromal tumor
after pediatric kidney transplant. Pediatric Transplant.
23(e13575)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Silverman SG, Pedrosa I, Ellis JH, Hindman
NM, Schieda N, Smith AD, Remer EM, Shinagare AB, Curci NE, Raman
SS, et al: Bosniak classification of cystic renal masses, version
2019: An update proposal and needs assessment. Radiology.
292:475–488. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Baniak N, Barletta JA and Hirsch MS: Key
renal neoplasms with a female predominance. Adv Anat Pathol.
28:228–250. 2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gokden N, Dawson K and Lindberg M:
Malignant rhabdoid tumor arising in a mixed epithelial, stromal
tumor of kidney: Report of a male case, review of the literature.
Pathol Res Pract. 216(153151)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kalinowski P, Kalinowski T, Kucharz J,
Kamecki H, Adamowicz B, Sikora K, Podgórska J and Demkow T: Mixed
epithelial and stromal tumor of the kidney: A case report. Oncol
Lett. 25:1–5. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Darouichi M, Till JP and Constanthin PE:
Renal cystic nephroma: Histologic and immunohistochemical analyses
and review of literature. Arch Clin Biomed Res. 3:003–011.
2019.
|
|
17
|
Tinguria M and Chorneyko K: Mixed
epithelial and stromal tumor: A rare renal neoplasm-case report
with clinicopathologic features and review of the literature. Case
Rep Pathol. 4(3528377)2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Caliò A, Cheng L, Martignoni G, Zhang S,
Brunelli M and Eble JN: Mixed epithelial and stromal tumours of the
kidney with malignant transformation: A clinicopathological study
of four cases. Pathology. 54:707–720. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Karafin M, Parwani AV, Netto GJ, Illei PB,
Epstein JI, Ladanyi M and Argani P: Diffuse expression of PAX2 and
PAX8 in the cystic epithelium of mixed epithelial stromal tumor,
angiomyolipoma with epithelial cysts, and primary renal synovial
sarcoma: Evidence supporting renal tubular differentiation. Am J
Surg Pathol. 35:1264–1273. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fine SW, Reuter VE, Epstein JI and Argani
P: Angiomyolipoma with epithelial cysts (AMLEC): A distinct cystic
variant of angiomyolipoma. Am J Surg Pathol. 30:593–599.
2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Varshney B, Vishwajeet V, Madduri V,
Chaudhary GR and Elhence PA: Renal angiomyolipoma with epithelial
cyst. Autops Case Rep. 11(e2021308)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fejes Z, Sánta F, Jenei A, Király IE,
Varga L and Kuthi L: Angiomyolipoma of the
kidney-Clinicopathological analysis of 52 cases. Pathol Oncol Res.
28(1610831)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Demır H, Sahın Z, Ozman O, Demırbılek M,
Ozden SB, Gurses I, Durak H, Uygun N and Onal B: Mixed epithelial
and stromal tumor family of kidney (adult cystic nephroma, mixed
epithelial and stromal tumor): Retrospective clinicopathological
evaluation. Turk Patoloji Derg. 38:251–260. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Vujanić GM and Đuričić SM: Renal tumours
of childhood: A review. Scr Med. 53:337–345. 2022.
|
|
25
|
Joshi VV and Beckwith JB: Multilocular
cyst of the kidney (cystic nephroma) and cystic, partially
differentiated nephroblastoma. Terminology and criteria for
diagnosis. Cancer. 64:466–479. 1989.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Arshad W, Amir A, Malik MN, Maqbool S,
Anwar MI and Lee KY: Rare case of mixed epithelial and stromal
tumor (MEST) of the kidney and its diagnostic and therapeutic
approach: A case report. Int J Surg Case Rep.
102(107882)2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Compérat E and Varinot J: Classification
of adult renal tumors: An update. Semin Ultrasound CT MR. 38:2–9.
2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Czarnecka AM, Niedzwiedzka M, Porta C and
Szczylik C: Hormone signaling pathways as treatment targets in
renal cell cancer (Review). Int J Oncol. 48:2221–2235.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Antic T, Perry KT, Harrison K, Zaytsev P,
Pins M, Campbell SC and Picken MM: Mixed epithelial and stromal
tumor of the kidney and cystic nephroma share overlapping features:
Reappraisal of 15 lesions. Arch Pathol Lab Med. 130:80–85.
2006.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang Y, Yuan J, Wang J and Fu Q: Mixed
epithelial and stromal tumor of the kidney: Report of a rare case
and review of literature. Int J Clin Exp Pathol. 8:11772–11775.
2015.PubMed/NCBI
|