Introduction
ADEM, known as acute disseminated encephalomyelitis,
is an inflammatory demyelinating disorder affecting the central
nervous system. This autoimmune disorder predominantly manifests in
pediatric and adolescent populations, frequently as a consequence
of an infection or immunization (1). ADEM is a rare disease affecting the
central nervous system, characterized by an inflammatory response
in the brain and spinal cord. It is an acute condition that tends
to proceed rapidly (1,2). It is usually monophasic, but some
patients may have either recurrences or an ADEM-like presentation
as the first attack of a chronic demyelinating disease such as
multiple sclerosis (MS) or neuromyelitis optica (2). The wide range of clinical
manifestations and progression of ADEM poses difficulties in
determining the optimal therapy strategy for each patient. The
present study addresses both the potential consequences that may
occur with the progression of the disease and emphasizes the
beneficial effects of targeted and symptomatic therapy.
The present paper provides an overview of the
clinical symptoms, diagnostic methods and treatment options for
ADEM. It highlights the effectiveness of intravenous
methylprednisolone and immunoglobulin in improving the condition.
The paper specifically emphasizes the significance of neurological
symptoms and the need to correlate them with biological and imaging
results.
Case report
A 19-year-old male, without any previous medical
conditions, arrived at the Neurology Clinic of ‘Sf. Ap Andrei’
Emergency County Clinical Hospital (Constanta, Romania) with a
sudden onset of speech difficulties, motor impairment in the right
arm and paresthesia on the right side of the body. The patient was
admitted to the ‘Sf. Ap Andrei’ Emergency County Clinical Hospital
in Constanta, Romania, in October 2023 and was discharged following
a 19-day hospitalization period.
On admission, neurological examination indicated
that the patient was conscious and alert, experienced difficulties
mobilizing the right limbs during tests for paresis tests and
displayed signs of expressive aphasia. The native computed
tomography (CT) scan of the brain revealed a hypodense area in the
left corona radiata, but the blood tests showed normal results.
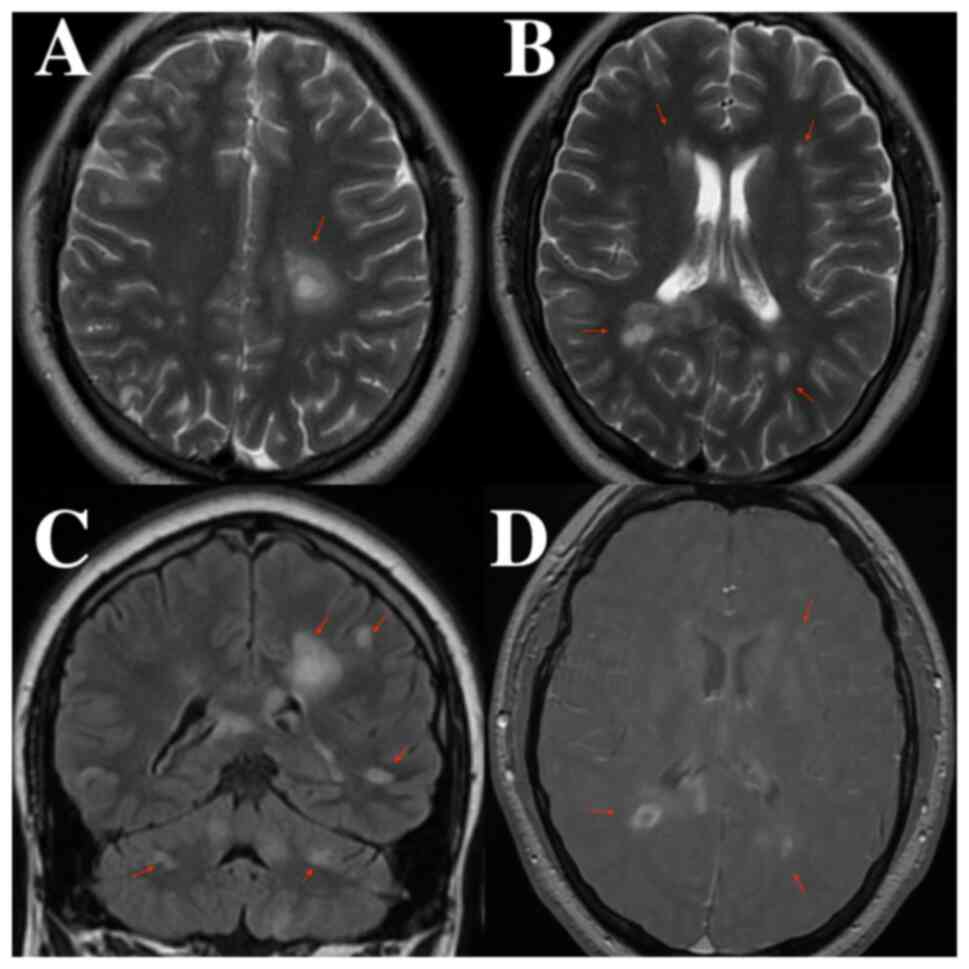
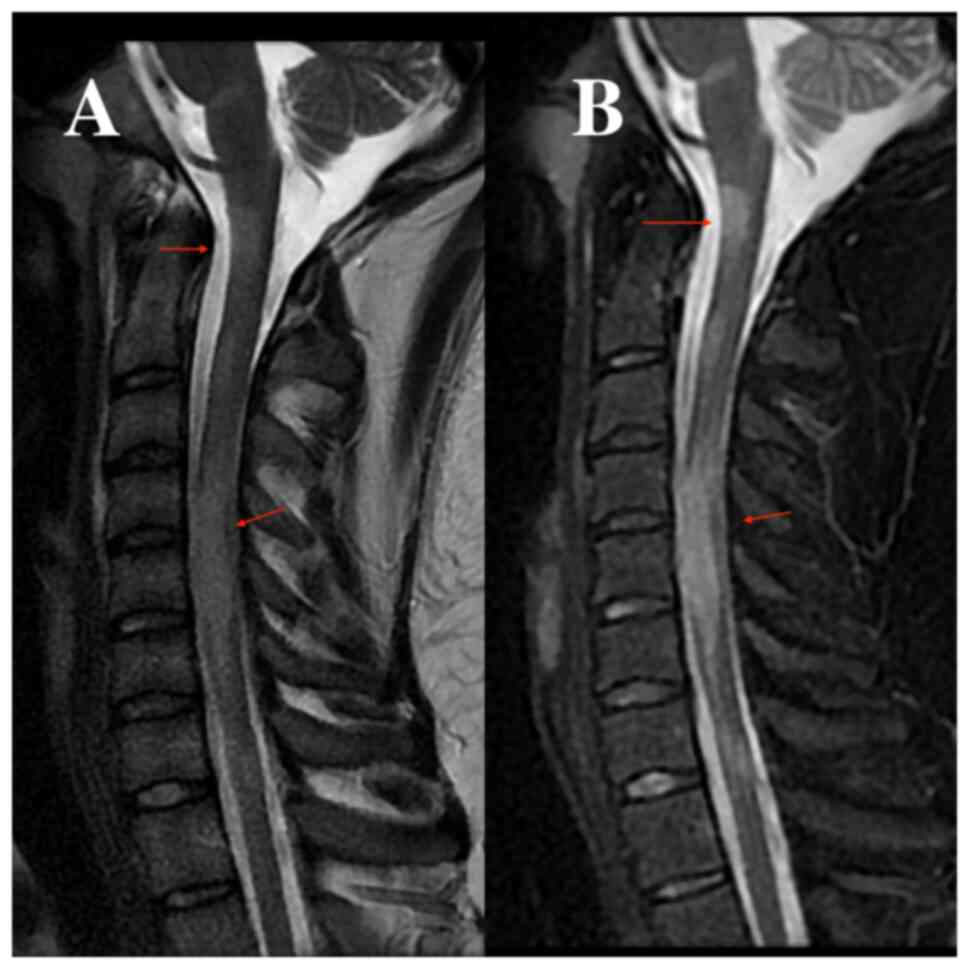
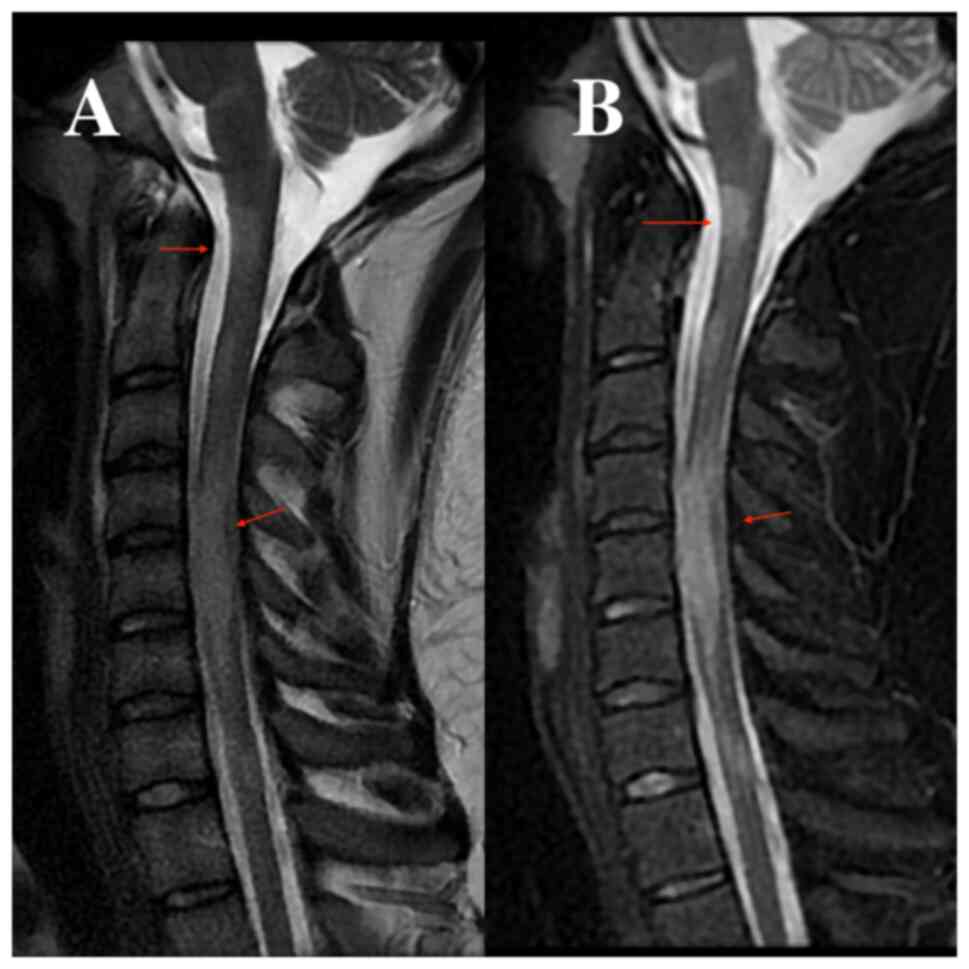
At 2 days after admission, the patient underwent a
brain and cervical spine MRI with and without a gadolinium-based
contrast substance. The results indicated demyelinating lesions,
intracerebral, both infratentorial and supratentorial, cervical and
dorsal spinal cord, some of them metabolically active, suggestive
for the diagnosis of multiple sclerosis (Fig. 1, Fig.
2 and Fig. 3). On day 5 after
admission, the neurologist decided to perform the following tests:
MOG antibody, anti-aquaporin 4 antibody, HIV 1+2, VDRL,
anti-Borellia bugdoferi antibody, anti-toxoplasma antibody,
anti-cytomegalovirus antibody, anti-double-stranded DNA antibodies
and extended ANA blot profile serum (Table I). All test results were
negative.
 | Table IResults of the blood tests. |
Table I
Results of the blood tests.
| Parameter | Result | Normal result |
|---|
| MOG antibody | Negative | Negative |
| Anti-aquaporin 4
antibody | <1/10 | <1/10 |
| HIV 1+2 | Negative | Negative |
| VDRL | Negative | Negative |
| Anti-toxoplasma
antibody | Negative | Negative |
| Anti-cytomegalovirus
antibody | Negative | Negative |
| Anti-double-stranded
DNA antibodies | Negative | Negative |
| ANA blot profile
serum testing | Negative | Negative |
Based on the aforementioned findings, the treatment
commenced with methylprednisolone therapy at a dosage of 500 mg
administered twice daily for a duration of 5 days. Following a
6-day period, a lumbar puncture was conducted. Macroscopically, the
cerebrospinal fluid (CSF) exhibited minor hemorrhaging in the first
sample tube, whereas the second sample tube appeared transparent
and clear. In the complete CSF examination, albuminorachia,
glycorrhachia and a total of 66 elements were identified. Positive
results were obtained while testing for oligoclonal bands in the
cerebrospinal fluid (Table
II).
 | Table IIFindings from cerebrospinal fluid
analyses. |
Table II
Findings from cerebrospinal fluid
analyses.
| Parameter | Value | Normal value |
|---|
| CSF albumin | 508 | 350 |
| CSF chloride | 123 | 120-130 |
| CSF glucose | 90 | 45-80 |
| Number of
elements | 66 | ≤3 |
| Anti-WNV MAbs | Negative | Negative (<0) |
| Oligoclonal
bands | Positive | Negative |
| Mycobacterium
tuberculosis | Negative | Negative |
Based on the aforementioned investigations, there
was a suspicion of acute disseminated encephalitis. Subsequent
evaluations and discussions were conducted in accordance with this.
Furthermore, a 5-day prescription of human immunoglobulin therapy
was commenced. The neurological condition of the patient
demonstrated a progressive improvement from day 5 until the patient
was discharged.
The infectious disease specialist recommended IgM
for Epstein-Barr virus, including a repeat lumbar puncture to
extract cerebrospinal fluid for HIV 1+2 testing, IgM for West Nile
virus and Koch's bacillus from cerebrospinal fluid (Table II). The results of all mentioned
investigations were negative.
Following a 19-day hospitalization, the patient's
health state showed improvement, leading to his subsequent
discharge. The neurological examination revealed that the patient
was conscious, temporally and spatially oriented, without neck
stiffness, normal oculomotor function, denies diplopia, no
nystagmus, symmetrical facial expression, normal speech, no
swallowing difficulties, no motor deficits, hypoesthesia in the
right limbs, ataxia in the right upper limb, bilateral vibratory
hypoesthesia in the lower limbs (4/8), and in the upper limbs (6/8)
bilaterally. Ataxic gait possibly without support, bilateral
Babinski sign and non-systematized positive Romberg sign.
Discussion
Autoimmune demyelinating disorders such as ADEM can
pose a significant challenge in differentiating it from multiple
sclerosis, leading to delays in achieving a timely and precise
diagnosis (3). MRI is currently
the most valuable tool in diagnosis and differential diagnosis.
However, complex radiological findings can overlap, leading to
misinterpretation, confusion or misdiagnosis (4,5).
The present patient represented a challenge in both
diagnosis and treatment, primarily because of the diversity of
possible differential diagnosis. In the case of this 19-year-old
male patient, the main focus of the differential diagnosis was
primarily between acute disseminated encephalitis and multiple
sclerosis.
In order to support the diagnosis of multiple
sclerosis, a series of tests were conducted, encompassing MOG
antibody, anti-aquaporin 4 antibody, HIV 1+2, VDRL,
anti-Borellia burgdorferi antibody, anti-toxoplasma
antibody, anti-cytomegalovirus antibody, anti-double-stranded DNA
antibodies and extended ANA blot profile serum testing. However,
all findings has negative results. Lumbar puncture was performed.
In the complete CSF examination, albuminorachia, glycorrhachia and
a total of 66 elements were identified. Oligoclonal bands were also
tested in the cerebrospinal fluid with positive results. They were
suggestive for identifying the autoimmune mechanism of the
diagnosis. At the time of admission, patient assessments included
determining any recent exposure to COVID-19 and the patient's
vaccination status against SARS-CoV-2 infection. The pandemic that
resulted from the spread of SARS-CoV-2 viral infections has
affected the population worldwide but has characteristically shown
a preponderance for affecting adults (6,7).
In the case of the presented patient, he had not
been vaccinated during the pandemic and had not recently
experienced symptoms that would raise suspicion of SARS-CoV-2
infection. The brain and cervical spine MRI, performed native and
with gadolinium-based contrast substance, indicated the presence of
demyelinating lesions. These lesions were observed intracerebrally,
encompassing both infratentorial and supratentorial regions, as
well as in the cervical and dorsal spinal cord.
The differential diagnosis also considered limbic
encephalitis; however, the distribution of the lesions on the MRI
did not align. The typical involvement sites in limbic encephalitis
are the mesial temporal lobes and limbic systems, usually
characterized by cortical thickening and increased T2/FLAIR signal
intensity in these regions (5).
Given all the evidence and a careful differential diagnosis, the
final diagnosis was acute disseminated encephalomyelitis.
We want to underline the importance of adding more
identification points between ADEM and multiple sclerosis,
highlighting that the use of cerebral MRI images and blood test
results is crucial for differentiation and accurate diagnosis of
these conditions. These additional details are essential to ensure
precise assessments and to avoid confusion between the two medical
conditions.
Neurological diseases, particularly those associated
with demyelination and inflammation, pose substantial challenges in
terms of diagnosis and subsequent management (8). These diseases can present with a wide
range of symptoms, which can often overlap with other conditions,
making accurate diagnosis difficult (9). Additionally, the progression of these
diseases can vary widely from person to person, further
complicating treatment plans. Research into the underlying causes
of neurological diseases, as well as potential new treatments, is
ongoing (10). Advances in genetic
testing and imaging techniques continue to improve our
understanding of these conditions and may lead to better diagnostic
tools and targeted therapies in the future (9,10).
Accurate diagnosis plays a pivotal role in guiding therapeutic
decisions, facilitating disease monitoring and optimizing patient
outcomes (11). However, due to
the intricate nature of these disorders, identifying the correct
diagnosis can be a daunting task for healthcare professionals. The
present study underscores the significance of precise diagnosis in
demyelinating and inflammatory diseases, the complexities involved
in their identification and the implications of misdiagnosis
(11-13).
In conclusion, the case discussed in the current
paper effectively illustrated the obstacles that must be addressed
in order to establish a precise diagnosis. The wide array of
possible diagnoses presented a substantial difficulty in assessing
the clinical and radiological presentation of our patient. Timely
diagnosis is crucial in commencing suitable therapeutic
interventions, which in turn can enhance prognosis results for
patients with encephalomyelitis. Yet, the intricate relationship
between ADEM and MS presents difficulty in establishing definitive
links and comprehending the underlying mechanisms. Ongoing research
is being conducted to understand the complex relationship between
these disorders and to discover diagnostic markers that might
assist in differentiating between them. The progress made in
comprehending the connections between ADEM and MS shows potential
for developing improved diagnostic tools and adjusting therapy
approaches to provide better care for patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are not
publicly available as the data were obtained from Constanta County
Emergency Clinical Hospital and, therefore, third-party data
restrictions apply. However, the data may be requested from the
corresponding authors with the permission of the Institutional
Ethics Committee of Clinical Studies of the Constanta County
Emergency Clinical Hospital.
Authors' contributions
RACB, AZS and MLF conceptualized the study. DM, SDA,
RAB, RB, AEG, DCJ and CEF designed the methodology. RAB and RB were
responsible for the imaging software and the interpretation of the
figures. RACB, AZS, RAB, RB, AEG, DCJ, CEF and MLF validated the
diagnosis and treatment plan through appropriate investigative
methods. DMV and CRT formally analyzed the data. RACB, AZS and MLF
conducted a thorough literature review to gather information from
reliable sources. RACB, AZS and MLF provided the informational
resources for the conceptual data of the article. RACB, AZS and MLF
curated the data and obtained the medical images. AEG, DCJ and CEF
wrote and prepared the original draft. RACB, AZS and MLF wrote,
reviewed and edited the paper, provided and edited the imaging data
in the manuscript, supervised the study, were project
administrators and acquired funding. RACB, AZS, MLF, DM, SDA, RAB,
RB, AEG, DCJ and CEF confirm the authenticity of all the raw data.
All authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the
Declaration of Helsinki, and approved by the Ethics Committee of
‘Sf. Ap. Andrei’ Emergency County Clinical Hospital (approval no.
1/11.01.2024).
Patient consent for publication
Written informed consent has been obtained from the
patient to publish this paper.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Carlisi E, Pavese C, Mandrini S, Carenzio
G and Dalla Toffola E: Early rehabilitative treatment for pediatric
acute disseminated encephalomyelitis: Case report. Eur J Phys
Rehabil Med. 51:341–343. 2015.PubMed/NCBI
|
|
2
|
Paolilo RB, Deiva K, Neuteboom R, Rostásy
K and Lim M: Acute disseminated encephalomyelitis: Current
perspectives. Children (Basel). 7(210)2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Eckstein C, Saidha S and Levy M: A
differential diagnosis of central nervous system demyelination:
Beyond multiple sclerosis. J Neurol. 259:801–816. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wildner P, Stasiołek M and Matysiak M:
Differential diagnosis of multiple sclerosis and other inflammatory
CNS diseases. Mult Scler Relat Disord. 37(101452)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tüzün E and Dalmau J: Limbic encephalitis
and variants: Classification, diagnosis and treatment. Neurologist.
13:261–271. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mihai CM, Chisnoiu T, Cambrea CS, Frecus
CE, Mihai L, Balasa AL, Stroe AZ, Gogu AE and Docu Axelerad A:
Neurological manifestations found in children with multisystem
inflammatory syndrome. Exp Ther Med. 23(261)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sirbu CA, Dantes E, Plesa CF, Docu
Axelerad A and Ghinescu MC: Active pulmonary tuberculosis triggered
by interferon beta-1b therapy of multiple sclerosis: Four case
reports and a literature review. Medicina (Kaunas).
56(202)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pirko I and Noseworthy JH: Chapter 48 -
Demyelinating Disorders of the Central Nervous System. In: Textbook
of Clinical Neurology. 3rd edition. Elsevier, pp1103-1133,
2007.
|
|
9
|
Tillema JM and Pirko I: Neuroradiological
evaluation of demyelinating disease. Ther Adv Neurol Disord.
6:249–268. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Heath F, Hurley SA, Johansen-Berg H and
Sampaio-Baptista C: Advances in noninvasive myelin imaging. Dev
Neurobiol. 78:136–151. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hancu A, Mihai MC and Axelerad AD:
Wilson's disease: A challenging diagnosis. Clinical manifestations
and diagnostic procedures in 12 patients. Rev Med Chir Soc Med Nat
Iasi. 115:58–63. 2011.PubMed/NCBI
|
|
11
|
Docu Axelerad A, Stroe AZ, Arghir OC, Docu
Axelerad D and Gogu AE: Respiratory dysfunctions in Parkinson's
disease patients. Brain Sci. 11(595)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gogu AE, Motoc AG, Stroe AZ, Docu Axelerad
A, Docu Axelerad D, Petrica L and Jianu DC: Plasminogen activator
inhibitor-1 (PAI-1) gene polymorphisms associated with
cardiovascular risk factors involved in cerebral venous sinus
thrombosis. Metabolites. 11(266)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Budisteanu M, Andrei E, Linca F, Hulea DS,
Velicu AC, Mihailescu I, Riga S, Arghir A, Papuc SM, Sirbu CA, et
al: Predictive factors in early onset schizophrenia. Exp Ther Med.
20(210)2020.PubMed/NCBI View Article : Google Scholar
|