Introduction
Myelolipoma is a rare benign tumor, consisting of
mature adipose tissue and normal hematopoietic cells. According to
autopsy studies, myelolipoma has an incidence of ~0.08-0.4%. It was
first described by Gierke in 1905 and named ‘bone marrow lipoma’ by
Oberling in 1929 (1-3).
Most patients with myelolipoma exhibit no clinical symptoms
(4,5). However, when these tumors increase in
size and exert pressure on surrounding vital organs, clinical
symptoms can include organ insufficiency, bleeding, or local site
pain (6). Myelolipomas most
frequently occur in the adrenal glands, are more frequent in women
than in men, and are usually singular lesions (4). Extra-adrenal myelolipomas (EAM) are
relatively rare and have been observed in the lung (7) and in the presacral (6,8),
vertebral (9) and mediastinal
(10,11) regions. We identified only two cases
of EAM in the central nervous system that have been reported, one
in the cerebellum (12) and one in
the lateral ventricles (13). The
present study reports the case of a 56-year-old woman who presented
with an intracranial primary EAM.
Case report
In October 2022, a 56-year-old woman presented with
a persistent right-sided headache for 8 days with no apparent
trigger and a past history of an intracranial lesion. The patient
was admitted to Jinhua Hospital Affiliated to Zhejiang University
in October 2022. The headache was not severe, but it worsened at
night or when the patient's head was lowered. Physical examination
results were negative.
Four years prior to presentation, the patient had
undergone a cranial computed tomography (CT) that had revealed a
calcified mass in the right frontal region, possibly a meningioma.
The patient was followed up regularly until August 2021, without
any changes in the lesion.
Admission laboratory test results were as follows:
Total erythrocyte count 3.81x1012/l, total hemoglobin
117 g/l, total platelet count 270x109/l, total leukocyte
count 6.51x109/l, ferritin 55.56 ng/ml, folic acid 50.13
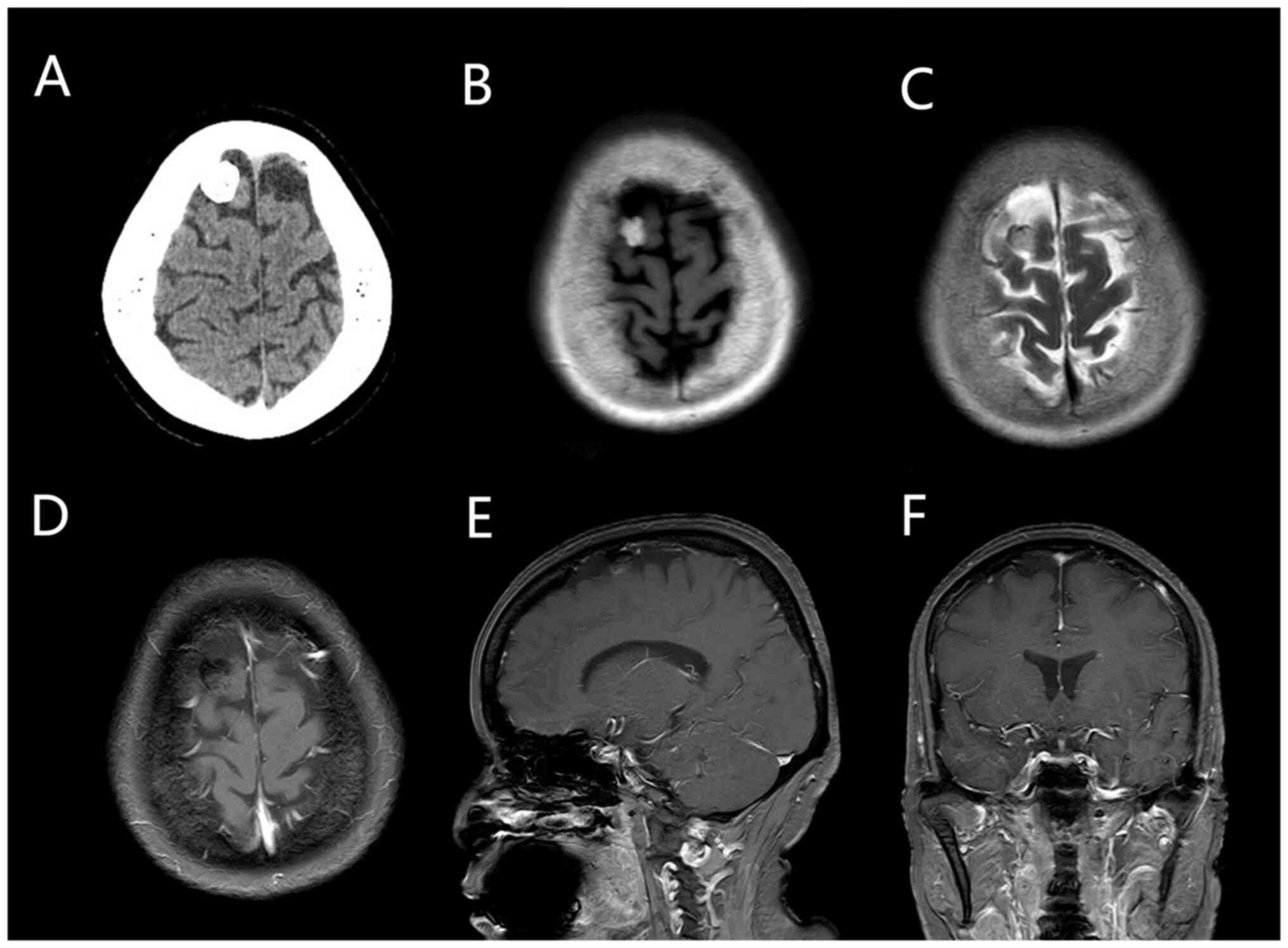
nmol/l and erythropoietin 18 mU/ml. Cranial CT scan results showed
a high-density, space-occupying lesion in the right frontal area,
possibly an osteoma or calcified meningioma. Thus, magnetic
resonance imaging (MRI) was recommended. Cranial enhancement and
perfusion MRI revealed an abnormal signal shadow of the nodule in
the right frontal area. The size of the lesion was ~1.5x1.2 cm. The
T1 image revealed a high signal focus; T2, diffusion-weighted
imaging and apparent diffusion coefficient images revealed low
signal focus; and the enhancement scan did not show significant
enhancement. On perfusion-weighted imaging, the lesion was unclear,
indicating the possibility of a meningioma with calcification
(Fig. 1).
In October 2022, craniotomy was performed under
general anesthesia. Intraoperatively, a white, hard, round-like
mass with a normal blood supply was observed. The base was in the
frontal dura. Tissue specimens were fixed in 10% neutral buffered
formalin for 24 h at room temperature (18-25˚C). The specimens were
dehydrated in a conventional series of gradient alcohols, cleared
in xylene, dipped in wax, embedded in paraffin, sectioned to 3 µm,
stained with conventional hematoxylin-eosin (HE) staining using a
Sakura autostainer (Sakura Finetek USA, Inc.), cleared and sealed.
Finally, the sections were examined microscopically at x400
magnification using an Olympus light microscope (Olympus
Corporation).
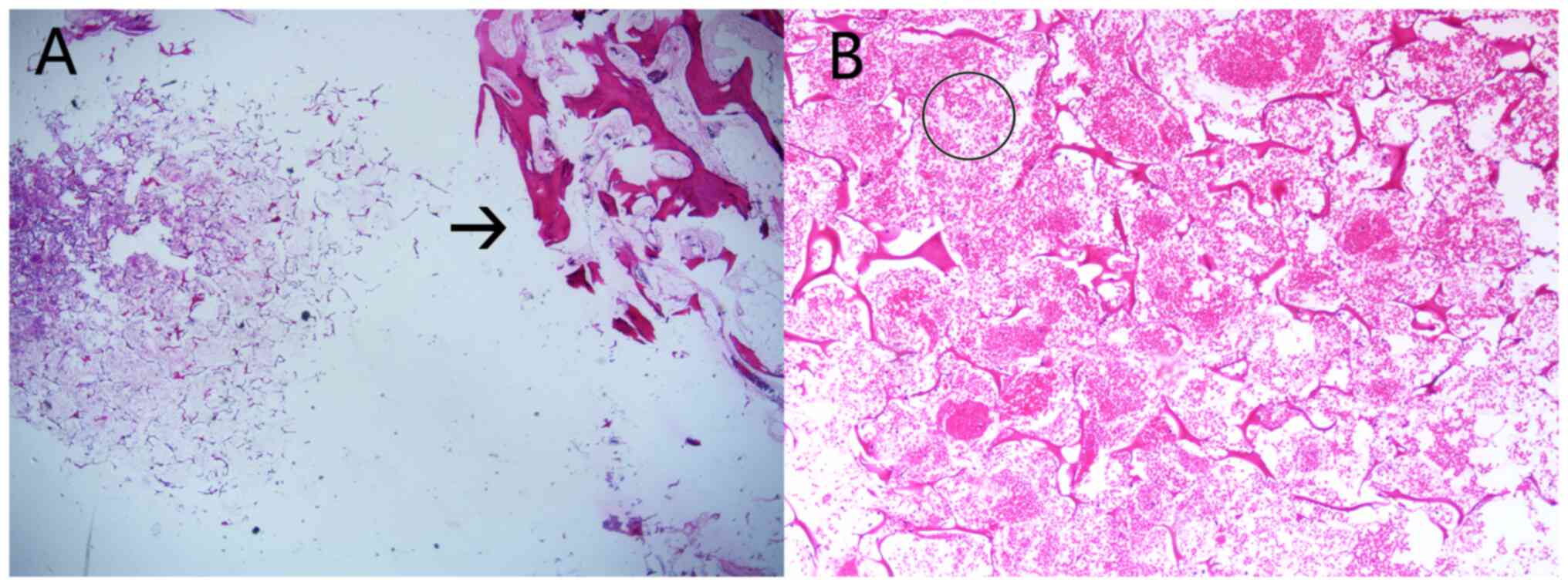
Histopathological analysis revealed that the tumor
wase composed of adipocytes with hyperplasia of small vessels and
infiltration of inflammatory cells scattered among heterogeneous
large cells, with considerable interstitial bleeding; hence, these
were considered to be adipogenic tumors (Fig. 2).
Subsequently, tissue specimens were fixed in 10%
neutral buffered formalin for 24 h, dehydrated in a conventional
series of gradient alcohols, made transparent with xylene, dipped
in wax, paraffin embedded into paraffin tissue blocks and sectioned
to 3 µm. Immunohistochemical detection was performed using an
EnVision technology system (Agilent Technologies, Inc.), using a
Leica Bond Max fully automatic immunohistochemistry instrument
(Leica Microsystems, Inc.). The sections were examined
microscopically using an Olympus light microscope (Olympus
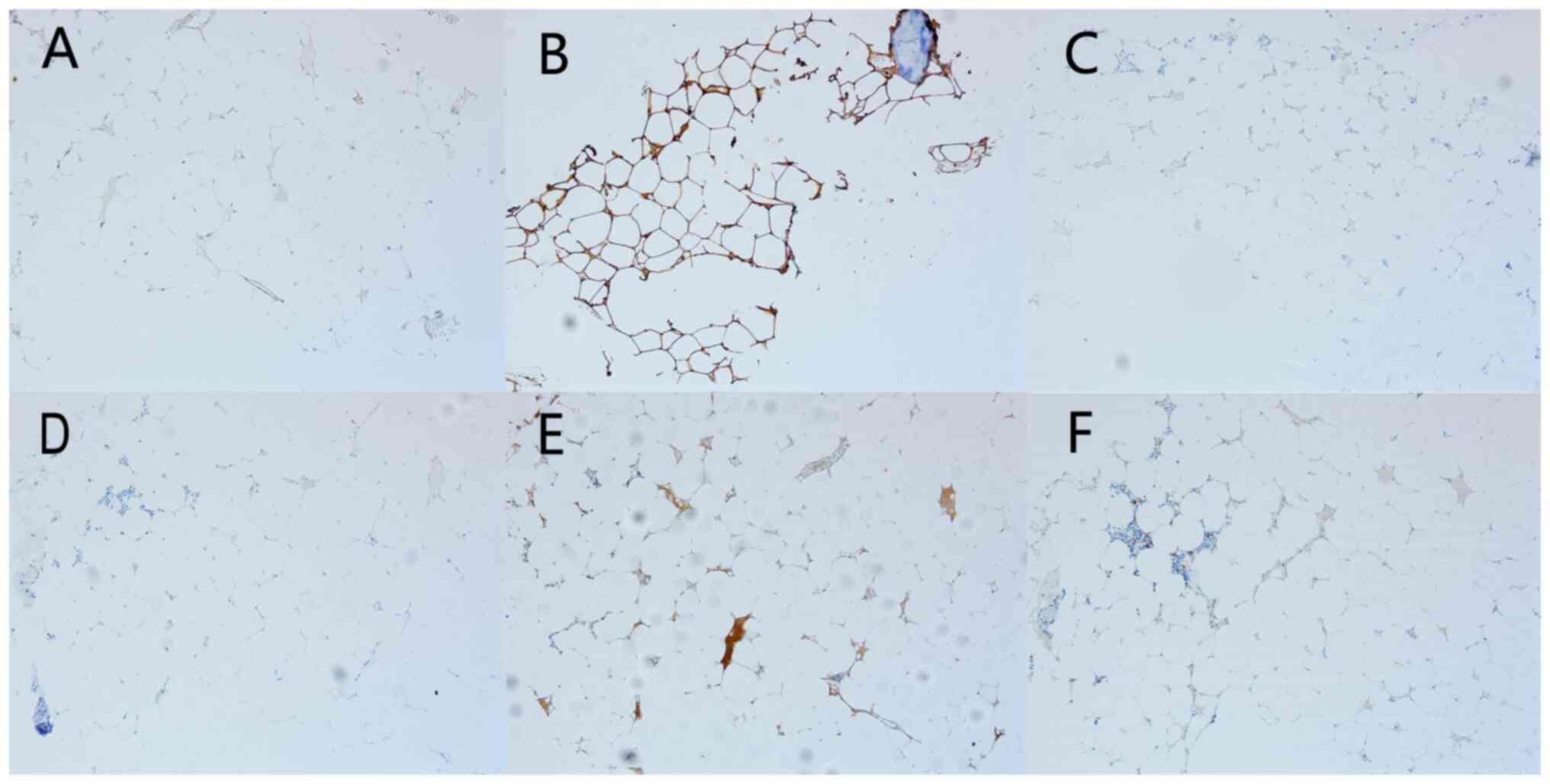
Corporation). Immunohistochemical analysis was negative for SSTR2
(clone EP149; cat. no. ZA-0587; ZSGB-BIO), E-Cad (clone MX020; cat.
no. MAB-0738; Fuzhou Maixin Biotech. Co., Ltd.), EMA (clone GP1.4;
cat. no. ZM-0095; ZSGB-BIO), STAT6 (clone EP325; cat. no. ZA-0647;
ZSGB-BIO), CK-P (clone AE1/AE3; cat. no. Kit-009; Fuzhou Maixin
Biotech, Co., Ltd.), HMB45 (cat. no. ZM-0187; ZSGB-BIO) and S100
(clone 5E2E2+4C4.9; cat. no. ZM-0224; ZSGB-BIO) (Fig. 3). The pathological diagnosis was of
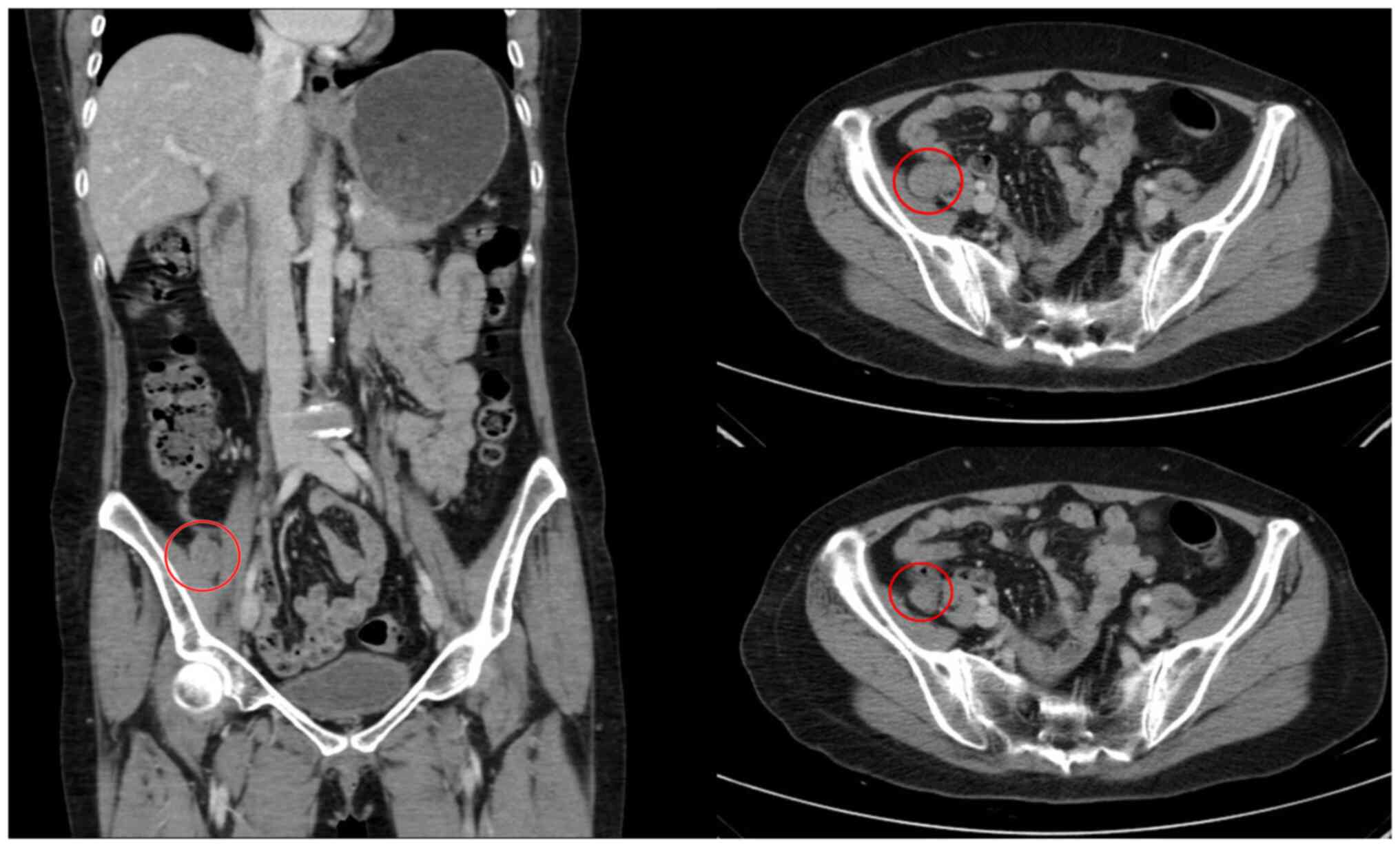
an intracranial myelolipoma. Postoperative renal B-ultrasonography
showed no significant infiltration of both adrenal areas.
Whole-abdominal enhanced CT revealed a low-density shadow in the
right presacral area, which was 2.0 cm in diameter with a clear
margin, and mild to moderate progressive enhancement (Fig. 4). The patient recovered well after
the surgery without adjuvant therapy. The multiplicity of
myelolipoma was also considered during the 3-month postoperative
follow-up period. Therefore, the patient underwent a CT of the
chest, an enhanced CT of the whole abdomen and an MRI of the whole
spinal cord. Except for the presacral mass, the other tumors were
not found on examination. To date, no tumor recurrence or
metastasis has been observed.
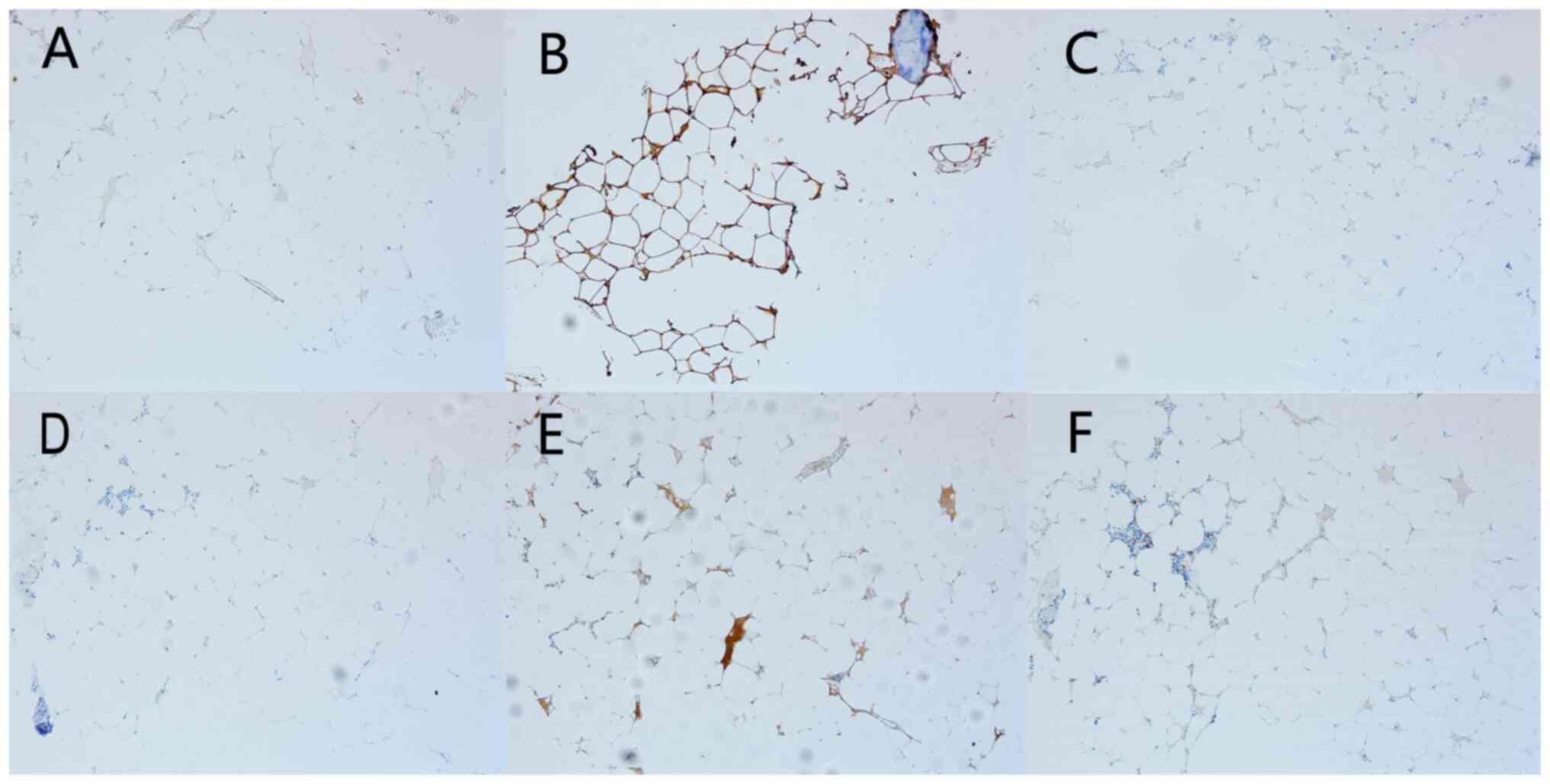 | Figure 3Microscopic findings (original
magnification, x100). Immunohistochemical staining of the tumors
revealed negative immunoreactions for (A) SSTR2, (B) S100, a
calcium binding protein localized in astroglial cells of the
central nervous system, (C) PR, (D) CK Pan; (E) E-Cad; and (F) EMA.
SSTR2, Human somatostatin receptor subtype-2; PR, progesterone
receptor; CK Pan, pan-cytokeratin; E-Cad, E-cadherin; EMA,
epithelial membrane antigen. |
Discussion
Myelolipoma is a rare tumor composed of
hematopoietic cells and mature adipose tissue (14). The hematopoietic element is
described as extramedullary (15).
The tumor usually develops in the adrenal glands (4). Most of the lesions are isolated,
while a few are multifocal (6,8-10).
The majority of EAMs occur in the anterior sacral region,
peritoneal space and mediastinum (6,10).
EAMs are rarely observed in other locations, and myelolipoma of the
central nervous system is extremely rare (16), with only two cases reported.
In 1982, Nalesnik et al (12) reported the case of a 74-year-old
woman with persistent headaches and progressive difficulty in
walking for 4 months; space-occupying lesions in the posterior
cranial fossa were observed. In the second case, in 2008, Suri
et al (13) reported the
case of a 72-year-old man who suffered from recurrent right-sided
focal seizures, limb weakness, and inability to speak for 15 days.
A space-occupying lesion was found in the left lateral ventricle.
Postoperative pathology confirmed a primary myelolipoma of the
central nervous system. Based on a literature search, the present
study is the third reported case of an intracranial myelolipoma.
However, to the best of our knowledge, this is the first report of
a myelolipoma in the frontal lobe. Additionally, this tumor was
complicated by another space-occupying lesion in the right
presacral area, which was considered to be a large myelolipoma on
imaging. However, as the pathology was not clear, the patient was
not informed. The patient chose to undergo regular follow-up.
While the pathogenesis of myelolipomas remains
unclear, one widely accepted theory states that myelolipomas are
caused by reticuloendothelial cell metaplasia (6,11).
Histologically, myelolipomas are considered a manifestation of
extramedullary hematopoiesis. In the present study, the tumor
contained mature adipose tissue, which did not contain adipocytes,
and resembled bone marrow hematopoietic tissue. Hematopoietic
tissue consists of three lineages of normal hematopoietic cells,
including granulocytes, erythrocytes, megakaryocytes and, in
certain cases, lymphocytes. In contrast to bone marrow
hematopoietic tissue, no reticular sinus or bone beam is present
(4,9,17).
Bishop et al (18) found
that most myelolipomas showed non-random chromosomal inactivation,
and the common chromosomal abnormalities were t(3;21)(q25/26;p11)
translocation. This suggested that myelolipomas are derivatives of
misaligned hematopoietic cells, possibly indicating a clonal origin
of these tumors (19). Mete et
al (20) found that the
occurrence of renal myelolipoma is related to chronic anemia and an
abnormal increase in erythropoietin. In patients with chronic
anemia, an increase in erythropoietin concentration may stimulate
the development of adrenal myelolipomas (5). However, our patient, like most others
with EAMs, showed no anemia or erythropoietin abnormalities.
Myelolipomas have characteristic imaging features.
Enhanced MRI typically shows mixed density with no significant
enhancement in the tumor area, and high-density shadows are
commonly observed on CT (21,22).
However, the incidence of myelolipoma is very low; hence,
misdiagnosis is common. Therefore, the present case was considered
to be a calcifying meningioma before and after admission.
Myelolipomas are distinct from other common intracranial epidural
tumors, such as meningioma, primary lung cancer, breast cancer,
other adenocarcinomas and primary dural lymphoma (PDL). Meningioma
is characterized by enhanced cranial MRI showing 60% thickening and
enhancement of the peripheral meninges, known as the meningeal tail
sign. It grows inward and exerts pressure on the brain tissue,
forcing the cortex to shift. Cerebrospinal fluid and blood vessel
crevasses are also observed around these tumors (23). Primary lung cancer, breast cancer
and other adenocarcinomas metastasize to the brain and can invade
the adjacent skull and dura mater. In these cases, enhanced MRI
shows considerable enhancement, and certain dural tail signs can be
observed (24). PDL also
frequently occurs in middle-aged women. In these cases, CT shows
high signal, similar to that of EAMs, and MRI-T2 sequences show
equal or low signal, marked, uneven enhancement, and blurred
interbrain space (25).
Myelolipoma is a nonfunctional benign tumor.
Currently, it is not considered to be a degenerative condition.
Similar to that in the present case, most patients are
asymptomatic. When a lipoma induces a mass effect or ruptures,
bleeding may occur. The largest myelolipoma has been reported to be
located in the adrenal gland, with a maximum diameter of ~30 cm
(26). In contrast to adrenal
myelolipoma, surgery is recommended when the tumor is >6 cm,
when there is a space-occupying effect, or bleeding (4). The possible progressive enlargement
of the mass caused neurological deficits similar to those observed
in previous studies, on patients with secondary symptomatic
epilepsy or hydrocephalus, resulting in unsteady gait and other
symptoms. Complete surgical resection of the tumor is recommended
to understand its nature (4,9). No
significant recurrence of myelolipoma has been reported in the
current literature (9,12,15).
There is some limitation in this study. First, we were unable to
obtain previous imaging of the patient. Second, as the patient had
no desire for further treatment, the nature of the presacral mass
could not be further determined. Therefore, a longer follow-up is
needed to summarize the disease. Finally, the present study is a
single and rare case and the available information is limited.
Consequently, more reports of this rare disease are needed to
increase our knowledge.
Owing to the rarity of central nervous system
myelolipomas, limited cases have been reported to date. Therefore,
these tumors are likely to be misdiagnosed. Currently, no tendency
for relapse after surgical dissection of central nervous system
myelolipoma has been reported. Surgery is recommended to identify
the pathology and complete resection can be used as a radical
treatment. To the best of our knowledge, this is the first reported
case of myelolipoma in the intracranial frontal lobe. Finally, it
is hoped that the present report will be helpful to others in
analyzing and summarizing the characteristics of central nervous
system myelolipomas.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by Zhejiang Natural
Science Foundation (grant no. LQ22H160056), Zhejiang Province
Medicine and Health Science and Technology Program Project Research
Fund Project (grant no. 2022KY425) and Key Research and Development
Projects of Social Development of Jinhua Science and Technology
Bureau (grant no. 2019-3-008).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ZX, SY and QT conceptualized and designed the study.
HC and MT performed the surgery. PH and LiW obtained MRI and CT
scans images. LuW advised on patient treatment and analyzed patient
data. HC and PH wrote the manuscript. MT and QT gathered the data
and revised the manuscript. ZX and HC confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Jinhua Hospital
Affiliated to Zhejiang University Institutional Review Board,
(approval no 2020-141-001; Qingdao, China).
Patient consent for publication
Written informed consent was provided by the patient
for publication of data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Plaut A: Myelolipoma in the adrenal cortex
(myeloadipose structures). Am J Pathol. 34:487–515. 1958.PubMed/NCBI
|
|
2
|
Kenney PJ, Wagner BJ, Rao P and Heffess
CS: Myelolipoma: CT and pathologic features. Radiology. 208:87–95.
1998.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rao P, Kenney PJ, Wagner BJ and Davidson
AJ: Imaging and pathologic features of myelolipoma. RadioGraphics.
17:1373–1385. 1997.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Calissendorff J, Juhlin CC, Sundin A,
Bancos I and Falhammar H: Adrenal myelolipomas. Lancet Diabetes
Endocrinol. 9:767–775. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lam AK: Update on adrenaltumours in 2017
World Health Organization (WHO) of endocrinetumours. Endocr Pathol.
28:213–227. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sethi S, Thakur S, Jacques S, Aoun HD and
Tranchida P: Myelolipoma of the pelvis: A casereport and review of
literature. Front Oncol. 8(251)2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mašić S, Vučić M and Seiwerth S: Pulmonary
myelolipoma containing osseous tissue: An unexpected finding at
autopsy. Respir Med Case Rep. 22:254–256. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sakamoto A, Nagamatsu I, Shiba E, Okamoto
T, Hisaoka M and Matsuda S: Presacral myelolipoma as a possible
parasymptom of cancer: A case report. Rare Tumors.
10(2036361318772124)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rezaee H, Tavallaii A, Keykhosravi E,
Abouei Mehrizi MA, Safdari Z, Pishjoo M, Aminzadeh B and Alenabi A:
Spinal myelolipoma-an extremely rare pathology within the lumbar
spine: A case report and literature review. Br J Neurosurg.
37:1805–1808. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hosaka T, Hata Y, Makino T, Otsuka H,
Koezuka S, Azumi T, Ejima K, Tochigi N, Shibuya K and Iyoda A:
Mediastinal myelolipoma showing gradual enlargement over 9 years: A
case report. J Cardiothorac Surg. 11(91)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zombori T, Tóth N, Furák J, Berényi Z and
Tiszlavicz L: Tumor of posterior mediastinum-rare case of
extramedullar myelolipoma. Magy Seb. 70:74–77. 2017.PubMed/NCBI View Article : Google Scholar : (In Hungarian).
|
|
12
|
Nalesnik MA, Martinez AJ and Heros RC:
Intracranial lipoma with hematopoietic elements (myelolipoma):
Report of a case with successful surgical resection. Cancer.
50:295–299. 1982.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Suri V, Sharma MC, Suri A, Karak AK, Garg
A, Sarkar C and Jain D: Myelolipomatous change in an
interhemispheric lipoma associated with corpus callosum agenesis:
Case report. Neurosurgery. 62(E745)2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Noble MJ, Montague DK and Levin HS:
Myelolipoma: An unusual surgical lesion of the adrenal gland.
Cancer. 49:952–958. 1982.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hasan M, Siddiqui F and Al-Ajmi M: FNA
diagnosis of adrenal myelolipoma: A rare entity. Diagon Cytopathol.
36:925–926. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
16
|
Cao J, Huang X, Cui N, Wang X, You C, Ni
X, Gao X, Wang J and Liu T: Surgical management and outcome of
Extra-adrenal myelolipomas at unusual locations: A report of 11
cases in a single center. J Bone Oncol. 35(100438)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Yildiz BD: Giant: Giant Extra-adrenal
retroperitoneal myelolipoma within cidentalgastric mesenchy maln
eoplasias. Int Surg. 100:1018–1020. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bishop E, Eble JN, Cheng L, Wang M, Chase
DR, Orazi A and O'Malley DP: Adrenal myelolipomas show nonrandom
X-chromosome inactivation in hematopoietic elements and fat:
Support for a clonal origin of myelolipomas. Am J Surg Pathol.
30:838–843. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chang KC, Chen PI, Huang ZH, Lin YM and
Kuo PL: Adrenal myelolipoma with translocation (3;21) (q25; p11).
Cancer Genet Cytogenet. 134:77–80. 2002.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mete O, Erickson LA, Juhlin CC, de Krijger
RR, Sasano H, Volante M and Papotti MG: Overview of the 2022 WHO
classification of adrenal cortical tumors. Endocr Pathol.
33:155–196. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Bracci B, De Santis D, Del Gaudio A,
Faugno MC, Romano A, Tarallo M, Zerunian M, Guido G, Polici M,
Polidori T, et al: Adrenal lesions: Areview of imaging. Diagnostics
(Basel). 12(2171)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Itani M, Wasnik AP and Platt JF:
Radiologic-pathologic correlation in extra-adrenal myelolipoma.
Abdom Imaging. 39:394–397. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Huang RY, Bi WL, Griffith B, Kaufmann TJ,
la Fougère C, Schmidt NO, Tonn JC, Vogelbaum MA, Wen PY, Aldape K,
et al: Imaging and diagnostic advances for intracranial
meningiomas. Neuro Oncol. 21 (Suppl 1):i44–i61. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Macdonald DR, Megyesi JF and Potvin KR:
P13.06 Dural metastases from breast cancer-case series. Neuro
Oncol. 18 (Suppl 4)(iv70)2016.
|
|
25
|
Kiewe P, Fischer L, Martus P, Thiel E and
Korfel A: Meningeal dissemination in primary CNS lymphoma:
Diagnosis, treatment, and survival in a large monocenter cohort.
Neuro Oncol. 12:409–417. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Łebek-Szatańska A, Nowak KM, Samsel R,
Roszkowska-Purska K, Zgliczyński W and Papierska L: Adrenocortical
carcinoma associated with giant bilateral myelolipomas in classic
congenital adrenal hyperplasia. Pol Arch Intern Med. 129:549–550.
2019.PubMed/NCBI View Article : Google Scholar
|