Introduction
Parapelvic renal cyst is a special type of renal
cyst which originates from the renal parenchyma and extends to the
renal sinuses. It is rare in clinical practice, with an incidence
of 1-3%. Parapelvic renal cysts are cystic lesions of the kidney;
the majority of patients with peripelvic cysts are asymptomatic and
most are detected by physical examination. The anatomical location
usually occurs near the renal collecting system, so when a small
cyst is found, pressure can be formed on the renal collecting
system or pedicle vessels, which can cause a series of clinical
symptoms such as low back pain, urinary tract infection, hematuria.
Prolonged effects can lead to other symptoms such as stones,
hydronephrosis, renal hypertension, cyst rupture or hemorrhage
(1). Clinically, the main
treatment options for peripelvic cysts include continued
observation, percutaneous renal cyst puncture and cure,
ultrasound-guided percutaneous renal cyst drainage and laparoscopic
renal cyst roof decompression. Considering the complexity of the
cyst itself and its proximity to the hilar arteriovenous and
collecting system, laparoscopic dermalization of peripelvic cysts
requires advanced surgical techniques compared with simple renal
cysts. With the progress of clinical instruments and other
technologies, it has been reported that flexible ureteroscopy has
become increasingly advantageous in the treatment of peripelvic
cysts (2,3). Anatomically, parapelvular cysts are
characterized by complexity and proximity to the hilar structure.
Endoscopic surgery can reduce or avoid the risk of damage to the
renal hilar structure and does not require complex surgical
techniques by the surgeon to perform laparoscopic surgery. A recent
technology called laser vaporization has been reported for
prostatectomy (4). After reviewing
a number of treatment guidelines, it was found that there is no
definitive treatment for parapelvic cysts and that there is no
definitive choice between flexible ureteroscopy incision and
drainage and laparoscopic parapelvic decompression. To address this
question, a systematic review and meta-analysis of eight studies
was conducted to evaluate and compare the efficacy of flexible
ureteroscopy compared with laparoscopic treatment of parapelvic
renal cysts.
Materials and methods
Search strategy
An overall systematic review was conducted in
accordance with the Cochrane guidelines (5). This search strategy used the
following databases to retrieve and identify the corresponding
articles: PubMed https://pubmed.ncbi.nlm.nih.gov/ (December
1980-December 2022), EMBASE https://www.embase.com/ (December 1980-December 2022),
Cochrane Central Register of Controlled Trials-CENTRAL https://www.cochranelibrary.com/advanced-search,
CONAHL https://www.ebsco.com/zh-cn/products/research-databases/cinahl-complete
(December 1980-December 2022), Clinicaltrials.gov https://classic.clinicaltrials.gov/, Google Scholar
https://scholar.google.com/ and CNKI
https://www.cnki.net/ (December 1980-December
2022), WanFANG DATA https://www.wanfangdata.com.cn/index.html (December
1980-December 2022).
Search terms used in conjunction with each other
included: ‘Cyst deroofing renal’ and ‘laparoscopic renal cyst
unroofing’ and ‘ureteroscopic incision and draining’.
Medical Subject Headings (MeSH):
((ureteroscopic) AND (laparoscopic)) AND (parapelvic
renal cysts) (‘ureteroscope s’(All Fields) OR ‘ureteroscopes’(MeSH
Terms) OR ‘ureteroscopes’(All Fields) OR ‘ureteroscope’(All Fields)
OR ‘ureteroscopic’(All Fields) OR ‘ureteroscopically’(All Fields)
AND (‘laparoscopes’(MeSH Terms) OR ‘laparoscopes’(All Fields) OR
‘laparoscope’(All Fields) OR ‘laparoscopical’(All Fields) OR
‘laparoscopically’(All Fields) OR ‘laparoscopics’(All Fields) OR
‘laparoscopy’(MeSH Terms) OR ‘laparoscopy’(All Fields) OR
‘laparoscopic’(All Fields)) AND (‘parapelvic’(All Fields) AND
(‘renal’(All Fields) OR ‘renals’(All Fields)) AND (‘cyst s’(All
Fields) OR ‘cystes’(All Fields) OR ‘cysts’(MeSH Terms) OR
‘cysts’(All Fields)).
Inclusion and exclusion criteria
All study data were extracted independently by two
researchers (Jianguo Gao and Meng Zhang) from the included studies.
Data could be input only after the agreement of two people.
Inclusion criteria were: i) Comparison of surgical methods,
ureteroscopic fenestration and drainage and laparoscopic renal cyst
decompression; ii) existing direct reports or computable sufficient
data (such as length of hospital stay, duration of surgery and
complications) in the study. The main exclusion criteria were: i)
no analysis of the above two surgical techniques, operation time
and complications; ii) case reports, abstracts of meetings,
summaries, letters to the editor, comments, editorials and other
articles from which sufficient data cannot be extracted; iii) a
polycystic kidney or Bosniak classification of CT imaging grades
III and IV; iv) renal mass or benign and malignant tumor; and v)
data of republished papers.
Study selection
Data retrieval was in two languages (English and
Chinese). The references of the retrieved papers were also
evaluated and considered for inclusion following research. A total
of three reviewers (Jianguo Gao, Meng Zhang and Huan Zhong)
conducted a comprehensive review of all studies according to
inclusion criteria. Each of the two reviewers (Jianguo Gao and Meng
Zhang) included eligible studies in the present review. Rongjiang
Wang identified each of these studies individually. In the
screening of this study, differences among several authors were
reached through negotiation.
Next, two authors (Jianer Tang and Zhihai Fang)
separately extracted data from the included studies. Huan Zhong
reviewed the data extracted by the two authors to ensure the
quality of the data and the consistency of the data extraction. The
extracted data were analyzed by two authors (Gao Jianguo and Zhang
Meng) and were grouped according to different treatment methods for
meta-analysis. The data included demographic cohort (age and sex),
cyst size, surgical method, intraoperative bleeding, postoperative
recovery and postoperative complications in both groups.
Data extraction
Jianguo Gao and Meng Zhang extracted a great deal of
data from the included studies: Study design, sample size, age,
sex, cyst type, cyst diameter, intervention type, intraoperative
bleeding, postoperative intestinal recovery, postoperative
complications, radiological success and symptom success.
Furthermore, the authors Jianguo Gao and Meng Zhang collected
information on the incidence of postoperative complications,
duration of intraoperative treatment and length of hospital stay
after treatment. The differences among the authors Jianguo Gao and
Meng Zhang were resolved through negotiation with the help of Yu
Chen. Yu Chen played a facilitative role in the consultation and
assisted in the judgment of disagreements arising from the data
analysis of the two authors.
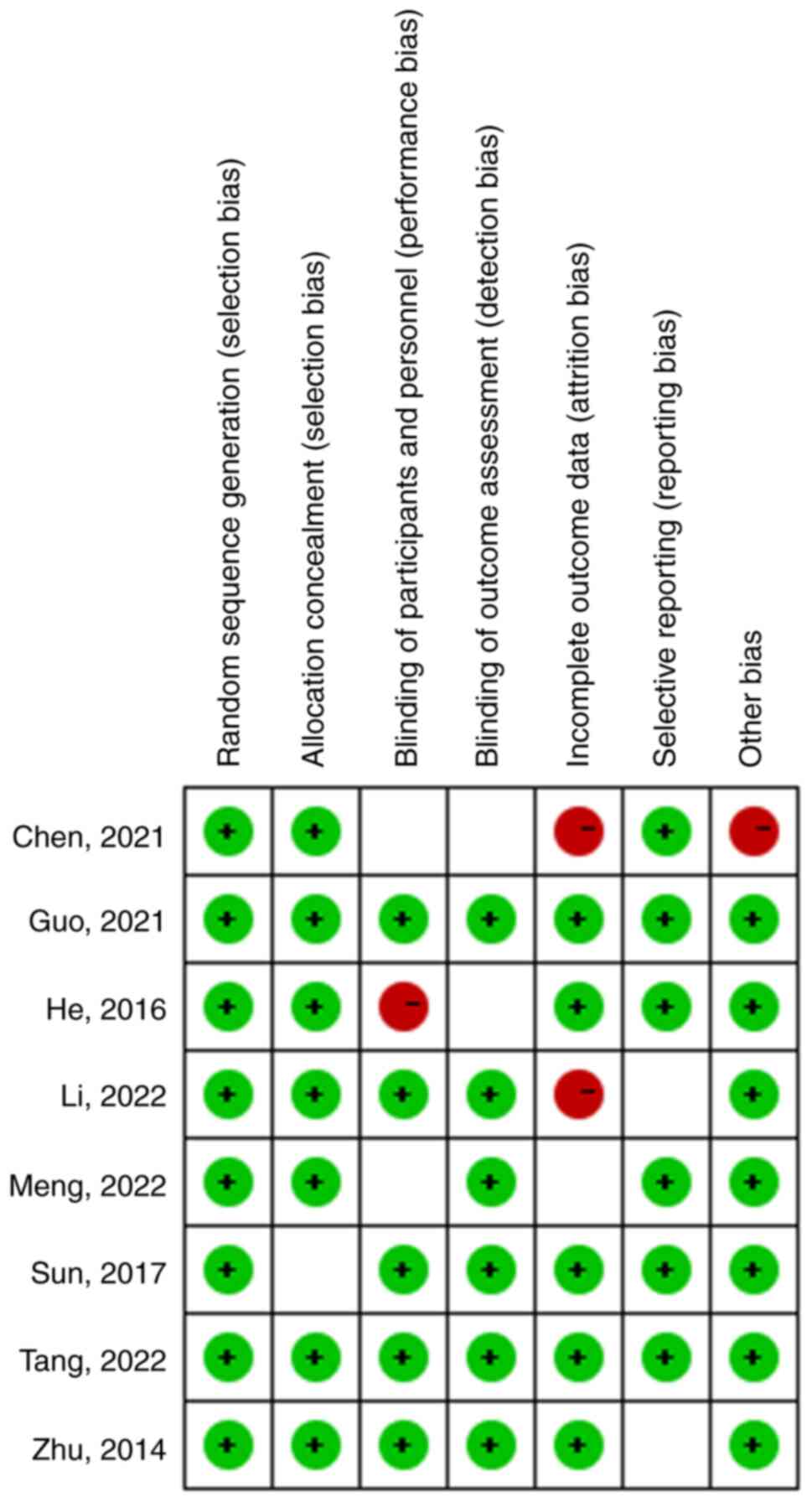
Evaluation of literature quality
The risk of bias was assessed according to the
guidelines outlined in the Manual for Systematic Review of Cochrane
Interventions (https://training.cochrane.org/handbook) Two reviewers
carefully read the full text of the included study and rated it as
‘high’, ‘low’ or ‘unclear’; whether participants and staff were
double-blind; whether the sequence generation followed the random
principle; whether there was hidden allocation made explicit in the
article; whether the results were evaluated blind; whether the
resulting data was complete; whether selective reporting existed;
and whether there were other biases.
Statistical analysis
Review Manager 5.4.1 software was used for the
statistical analysis. The data were analyzed following the overall
statistics and the results outputted with the overall percentage.
The Q statistic and I2 index were used to test the heterogeneity
among the studies. If no significant heterogeneity was identified,
the fixed effect model was used. The meta-analyzed effect sizes
were reported as the relative risk (RR) and 95% confidence interval
(95% CI) of treatment failure in the flexible ureteroscopic group
compared with laparoscopic resection. Alternatively, in case of
significant heterogeneity existing between the studies (Q statistic
<0.1 and I2 >50%), then a random effects model
using a reduced maximum likelihood (REML) approach was employed.
The overall statistics of the data were analyzed, and the results
were outputted in terms of the overall percentages. The results are
shown either as the mean ± SD or as percentages of cumulative
data.
Results
Study selection and
characteristics
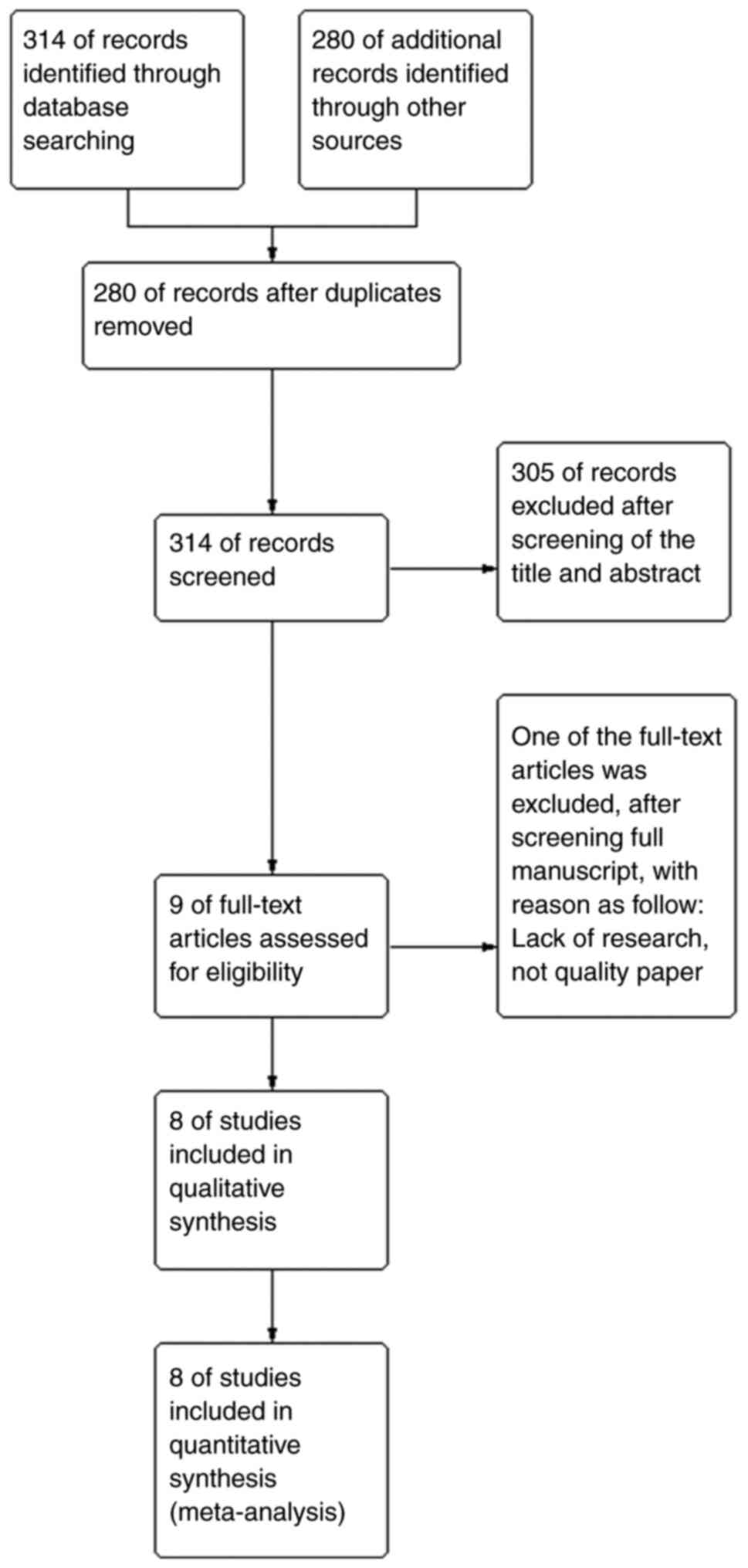
A PRISMA flow chart was used to express the
selection results in the present study (Fig. 1). Through literature search and
database search, it was found that there were 594 possible related
studies. After removing the duplicated studies, the remaining 314
studies needed to be analyzed in the next step. A total of 305 of
the studies were excluded after screening the title of the paper
and the content of the abstract, nine full-text articles were
assessed as qualified and one article was excluded after screening
the full manuscript for lack of research results. Finally, eight
studies met the inclusion criteria and were included in the
meta-analysis (Fig. 1) (6-13).
All data in Table I are from eight
studies, including not only the basic patient age and cyst size,
but more importantly, the relevant surgical data and postoperative
recovery results. All the selected studies date from 1980 onwards
and 4 of them were non-randomized trials (7,9,10,13),
the other 4 studies were randomized trials (6,8,11,12).
After evaluation, the bias was acceptable; a risk of bias summary
is in Fig. 2. The risk of
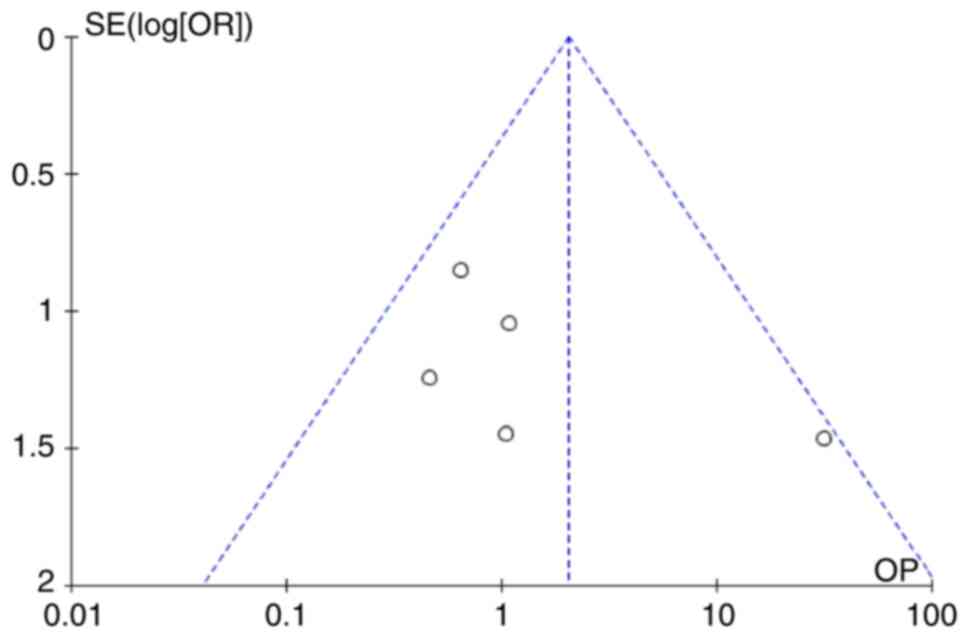
publication bias assessment of the included studies showed that the
majority of the studies had a low risk of bias from radiological
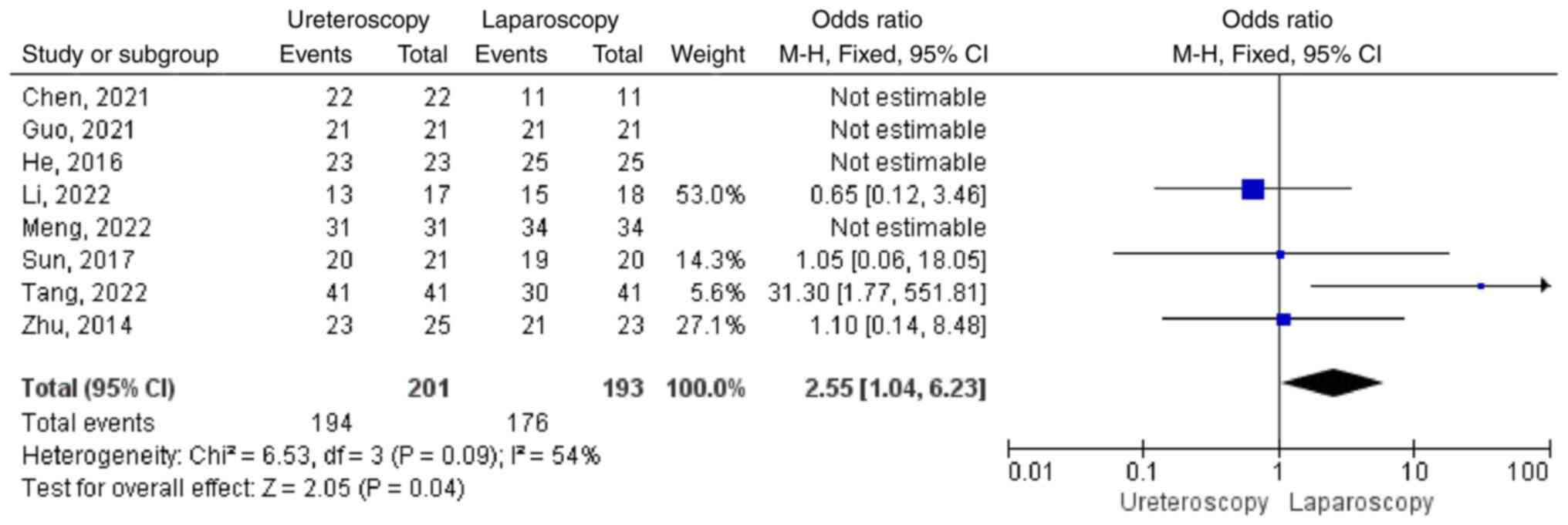
success (Figs. 3 and 4). In the treatment of peripelvic cysts,
holmium laser incision and internal drainage were used in most
patients under ureteroscopy, while incision and drainage were used
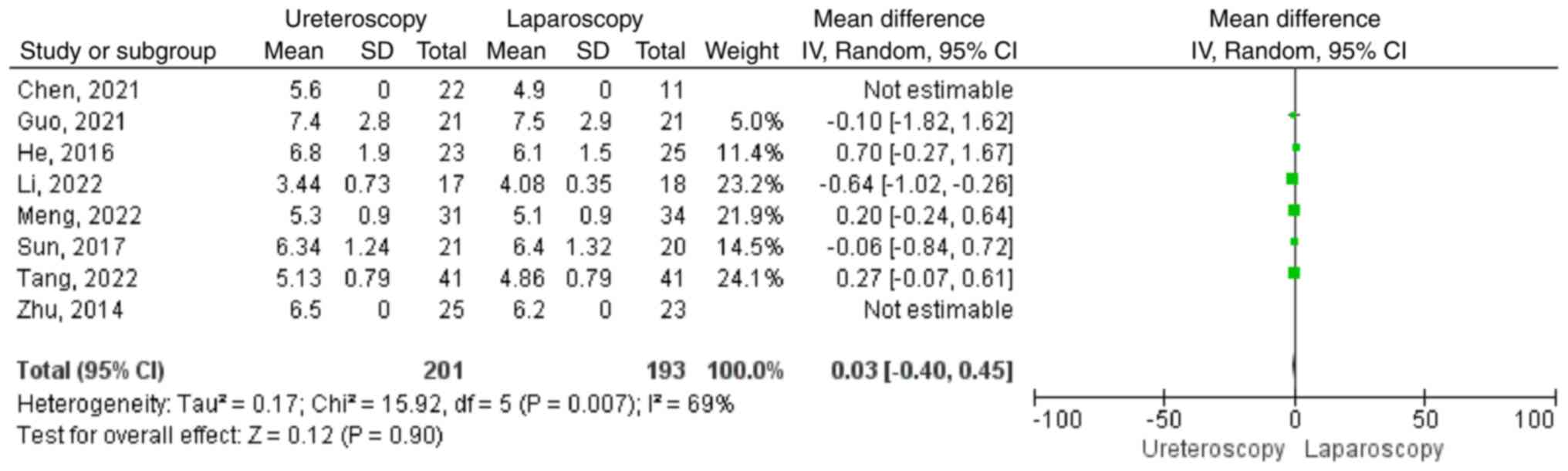
in most patients under laparoscopy. Of the patients 201 underwent
ureteroscopy and 193 underwent laparoscopy. The outcome of
meta-analysis showed us the cyst size of patients in the flexible
ureteroscopy group had no statistical differences compared with
that in the retroperitoneal laparoscopic group, with statistical
significance [mean difference (MD)=0.03, 95%confidence interval
(CI)-0.40,0.45; P=0.90; Fig. 5)].
Follow-up ranged from 6-35 months.
 | Table ICharacteristic for included
studies. |
Table I
Characteristic for included
studies.
| First author,
year | Design | | Age, years, mean
(range) | Sample (male:
female) | Cyst size, cm, mean
(range) | Operation time
(min) | Intra-operative
bleeding, ml | Postoperative
intestinal peristalsis time, h, mean | Postoperative
hospital stay, days, mean (range) | Pelvis perforated
during operation, n | Infect or fever,
n | Recurrence
occurring 6 months after operation | (Refs) |
|---|
| He, 2016 | Prospective
randomized study | Laparoscopy
ureteroscopy | 42 (32-62) | 25 (19:6) | 6.1±1.5 | 65.9±16.1 | 100.6±16.7 | | 6.0±0.6 | | | | (8) |
| | | | 47 (29-65) | 23 (15:8) | 6.8±1.9 | 40.9±14.6 | 18.3±7.2 | | 5.0±1.4 | | | | |
| Chen, 2021 | Retrospective
study | Laparoscopy
ureteroscopy | 58 (53-64) | 11 (6:5) | 4.9 (4-5.8) | 80 (70-95) | | | 4 (3-7) | | 1 | | (10) |
| | | | 54 (45-63) | 22 (12:10) | 5.6 (4.8-7) | 45 (28.8-56.3) | | | 2 (1.8-3) | | 2 | | |
| Guo, 2021 | Prospective
randomized study | Laparoscopy
ureteroscopy | 57.28±6.17 | 21 (12:9) | 7.5±2.9 | 50.91±15.28 | 37.92±10.26 | 19.29±5.77 | 6.52±1.37 | | 2 | | (12) |
| | | | 56.85±6.3 | 21 (13:8) | 7.4±2.8 | 40.88±14.37 | 30.19±11.68 | 15.38±4.15 | 5.79±1.18 | | 1 | | |
| Tang, 2022 | Prospective
randomized study | Laparoscopy
ureteroscopy | 57.65±5.12 | 41 (21:20) | 4.86±0.79 | 65.78±16.32 | 100.34±16.33 | | 5.18±1.03 | | | 11 | (11) |
| | | | 57.61±5.03 | 41 (22:19) | 5.13±0.79 | 40.36±14.57 | 18.32±7.21 | | 4.21±1.02 | | | | |
| Zhu, 2014 | Prospective
randomized study | Laparoscopy
ureteroscopy | 52 (35-66) | 23 (13:10) | 6.2 (5-10.5) | 69.48±14.21 | 49.35±12.18 | 31.43±6.99 | 6.04±1.29 | 1 | | 2 | (6) |
| | | | 53 (34-67) | 25 (14:11) | 6.5 (5.2-10) | 24.12±4.51 | 10.24±3.38 | 13.24±2.39 | 3.24±1.42 | | | 2 | |
| Li, 2022 | Retrospective
study | Laparoscopy
ureteroscopy | 43.24±8.46 | 18 (8:10) | 4.08±0.35 | 37.53±14.32 | | | 2.45±0.62 | | | | (7) |
| | | | 49.85±9.33 | 17 (8:9) | 3.44±0.73 | 35.26±13.31 | | | 2.04±0.32 | | 1 | | |
| Sun, 2017 | Retrospective
study | Laparoscopy
ureteroscopy | 53.86±8.14 | 20 (10:10) | 6.4±1.32 | 63.23±12.54 | 45.13±10.25 | 30.51±6.48 | 6.55±1.36 | | | | (9) |
| | | | 54.52±8.66 | 21 (11:10) | 6.34±1.24 | 27.16±5.24 | 12.41±3.66 | 12.54±2.52 | 3.36±1.38 | | 1 | | |
| Meng, 2022 | Retrospective
study | Laparoscopy
ureteroscopy | 46.8±7.8 | 34 (15:19) | 5.1±0.9 | 54.4±6.4 | 59±9.9 | | 5.6±0.9 | | 1 | | (13) |
| | | | 47.6±7.8 | 31 (15:16) | 5.3±0.9 | 30.1±4.3 | 5.5±1.7 | | 4.5±0.8 | | | | |
Operation time
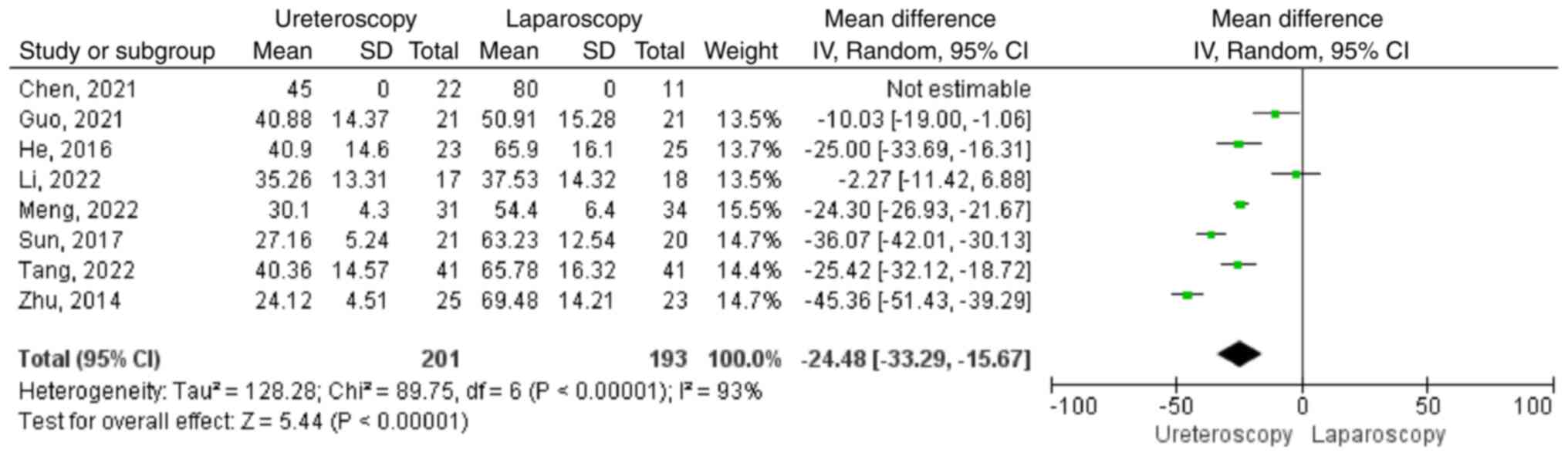
Operation time were reported in eight studies
(6-13).
In a total of 394 patients flexible ureteroscopy were compared with
retroperitoneal laparoscopy for the treatment of pelvic cyst in
surgery time consumption. They were included in two groups; 201
cases in flexible ureteroscopy group, 193 cases of retroperitoneal
laparoscopy group. The results showed that there was significant
heterogeneity in the studies (P<0.00001; I2=96%,).
Thus, a random effects model was applied. The results showed that
the operative time in the flexible ureteroscopy group was shorter
compared with that in the retroperitoneal laparoscopic group, with
statistical significance (MD=-24.48; 95%CI -33.29,-15.67;
P<0.00001; Fig. 6).
Intraoperative blood loss
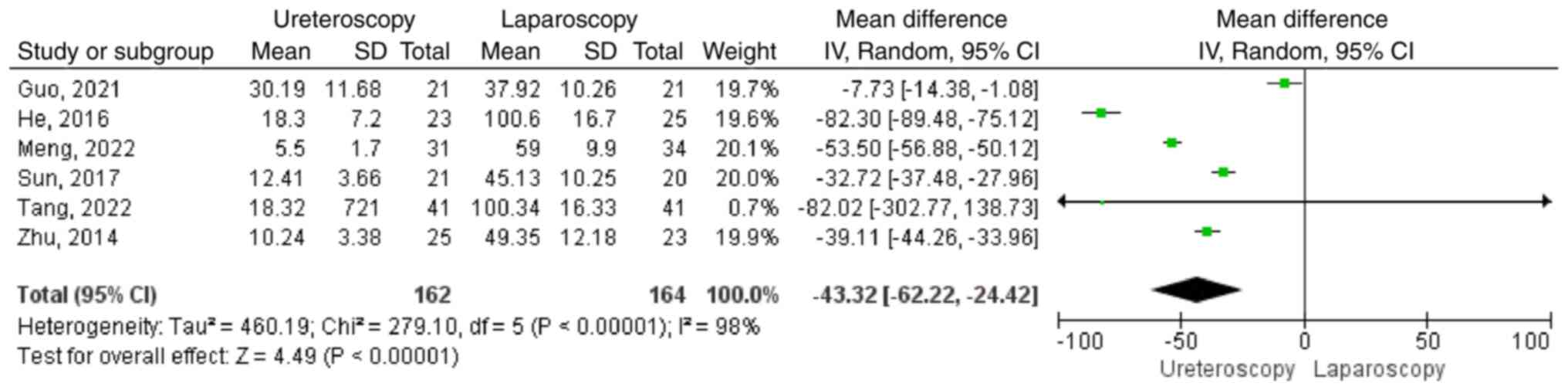
Intraoperative blood loss for treatment of
parapelvic cysts was compared between ureteroscopy and laparoscopy
in six studies (6,8,9,11-13).
There were 326 patients, including 162 in ureteroscopy group and
164 in laparoscopy group. The results showed obvious heterogeneity
in the studies (P<0.00001; I2=98%,), Meta-analysis
showed that intraoperative blood loss of patients in ureteroscope
group was significantly less than that in laparoscopic group, with
statistical significance (MD=-43.32; 95%CI -62.22,-24.42;
P<0.00001; Fig. 7).
Postoperative anal exhaust time
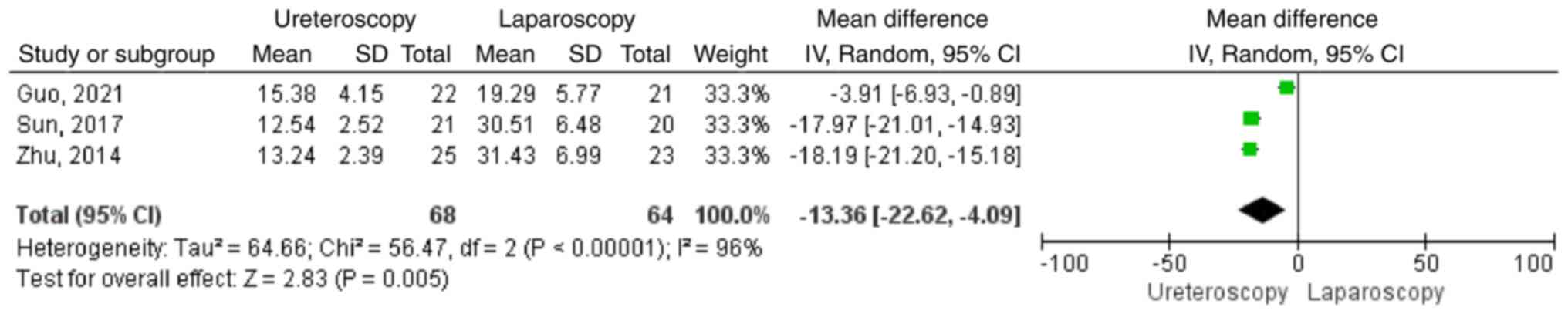
Calculation of anal exhaust time (h) following
surgery for parapelvic cysts compared ureteroscopy and laparoscopy
in three studies (6,9,12).
There were 132 patients, including 68 in the ureteroscopy group and
64 in laparoscopy group. The results showed obvious heterogeneity
in the studies (P<0.00001; I2=96%) and that the anal
exhaust time following surgery in ureteroscope group was
significantly less than that in laparoscopic group, with
statistical significance (MD=-13.36; 95%CI -22.62,-4.09; P=0.005;
Fig. 8).
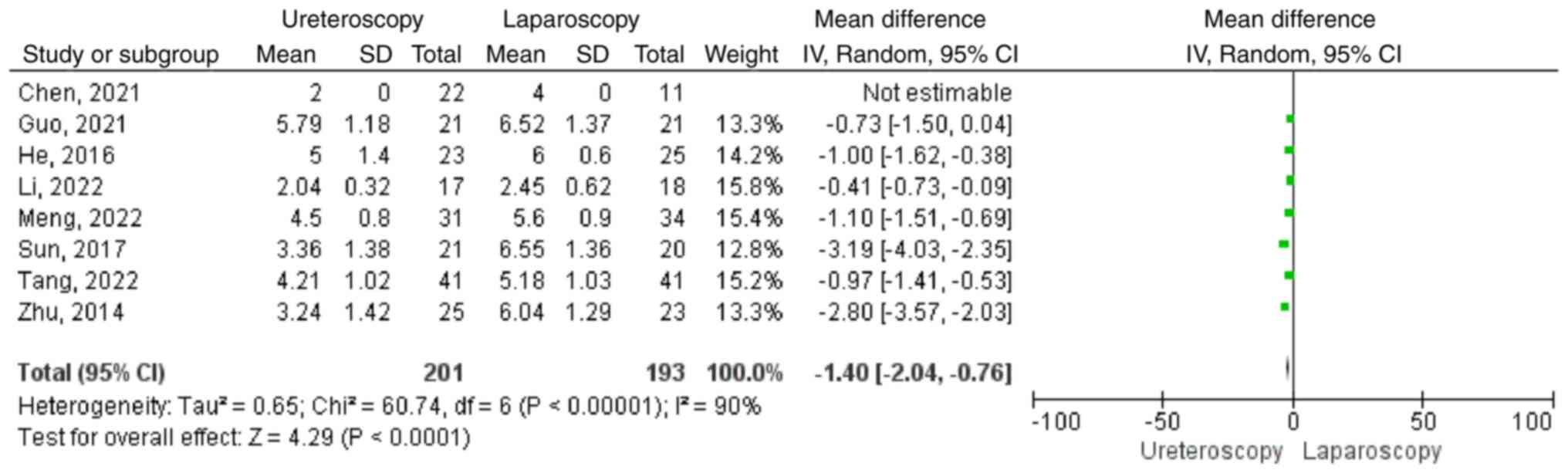
Postoperative hospital stay
In these eight studies, postoperative hospital stay
(days) was compared in the treatment of parapelvic cysts by
ureteroscopy or laparoscopy, including 394 patients, 201 in
flexible ureteroscopy group and 193 in retroperitoneal laparoscopy.
The results displayed significant heterogeneity among the studies
(P<0.00001; I2=93%). The random effects model was
used. The results of meta-analysis showed that the postoperative
hospital stay of patients in the ureteroscopy group was
significantly shorter than that in the laparoscopic group and the
difference was statistically significant (MD=-1.40; 95%CI
-2.04,-0.76; P<0.0001; Fig.
9).
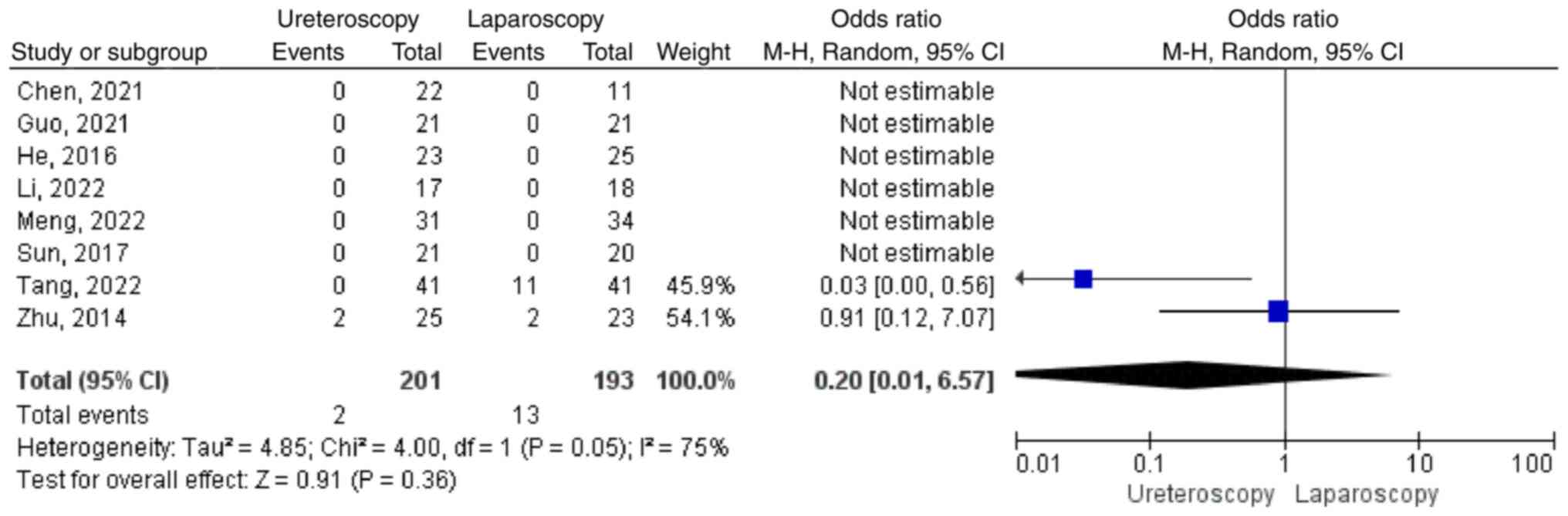
Recurrence after 6 months
Postoperative follow-up as the complete treatment of
parapelvic cysts by ureteroscopy and laparoscopy was searched for
in eight studies (6-13)
including 394 patients; 201 in the flexible ureteroscopy group and
193 in the retroperitoneal laparoscopy group. There was significant
heterogeneity in the studies (P=0.05; I2=75%). The
results of meta-analysis showed that postoperative recurrence after
6 months in the ureteroscopy group was not significant compared
with the laparoscopic group (MD=0.20; 95%CI 0.01,6.57; P=0.36;
Fig. 10).
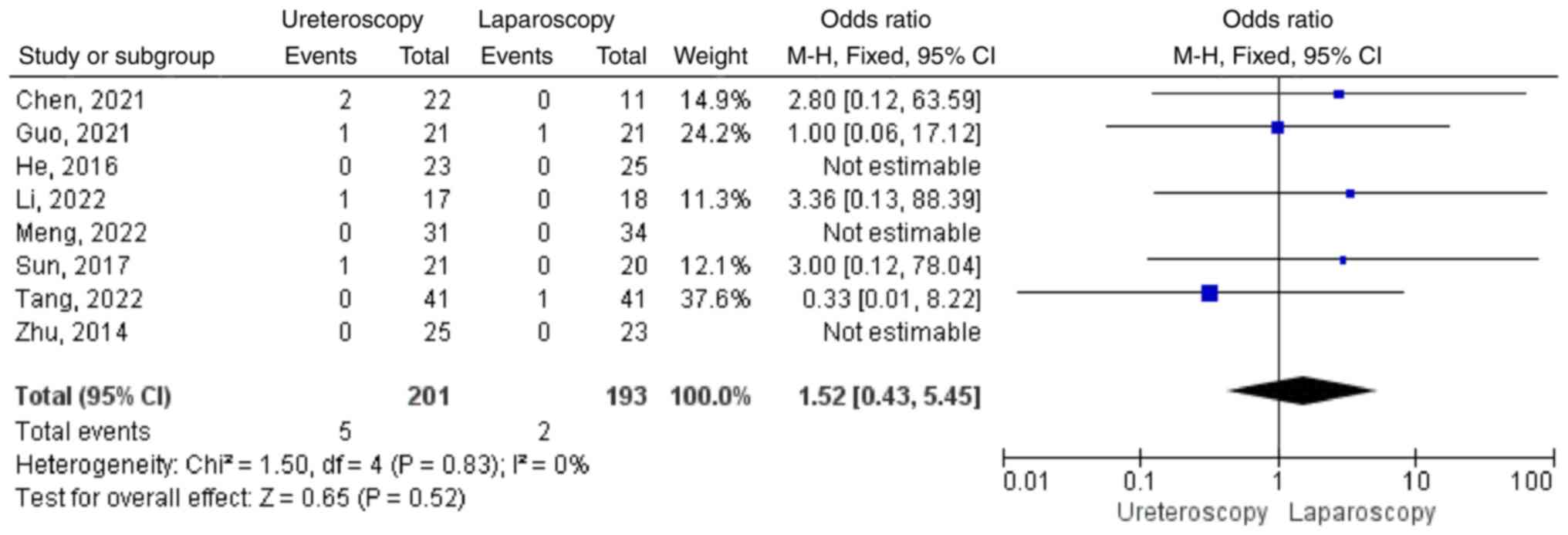
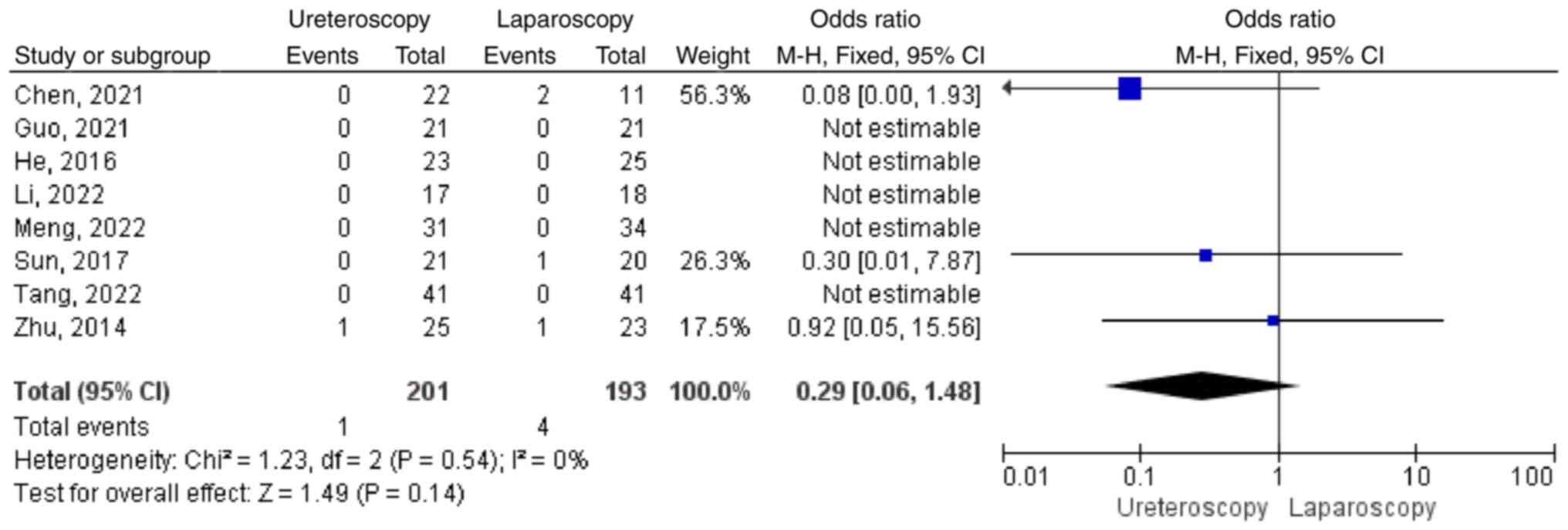
Complications
The eight studies also reported complications by
study and by group (see Table I).
Specifically, Tang et al (11) documented 11 cases of recurrence in
41 patients with laparoscopic deroofing and zero recurrence in 41
patients in the ureteroscopy group. Zhu et al (6) recorded two cases of recurrence in the
laparoscopic and ureteroscopic groups, respectively. Guo et
al (12) reported that one
case of infection occurred in the laparoscopic group following
surgery. In two studies, Chen et al (10) and Tang et al (11) found that there was one patient with
fever in the laparoscopic group respectively, while there were six
patients with fever following ureteroscopy from Chen et al
(10), Guo et al (12), Li and Lin (7) and Sun et al (9), respectively (Fig. 11). In three studies, Chen et
al (10), Zhu et al
(6) and Sun et al (9) found that there was four patients with
urine leakage after surgery in the laparoscopic group, compared
with one in Zhu et al (6)
in ureteroscopic group (Fig.
12).
Discussion
Parapelvic cysts are a common type in cystic lesions
of the kidney (14). Due to the
anatomical structure of parapelvic cysts close to the renal
pedicle, cysts located in the pelvis have a greater effect on the
patient than those in the parenchyma and on the surface of the
kidney; patients with small cysts may have waist discomfort,
hematuria, elevated blood pressure and other manifestations and
further development may lead to renal insufficiency and in severe
cases may lead to kidney failure (15). In general, parapelvic cysts with a
diameter of <4 cm and no symptoms are considered medically and
generally no special treatment is needed and only regular follow-up
is required. For the cyst diameter of >4 cm and obvious lumbago,
compression of renal parenchyma and other manifestations, the
doctor will recommend surgical treatment measures. For the
treatment of paraparenal cysts, traditional open surgery leads to
large incisions, a number of complications and long postoperative
recovery time. Therefore, most clinicians now prefer minimally
invasive surgical methods, such as laparoscopy and ureteroscope,
rather than open surgery with large incisions.
The treatment of renal cysts by laparoscopy was
first reported in 1992 and laparoscopy for parapelvic cyst is a
common treatment lasting a long time (16-19).
Relatively speaking, retrolaparoscopy can effectively reduce the
damage to abdominal organs, but the retroperitoneal space is small
and intraoperative cysts are not easy to be exposed, which
increases the difficulty of the operation. If the operation is not
properly performed, it is easy to cause complications. At the same
time, it should be noted that in patients undergoing laparoscopic
treatment it should be determined whether the cyst is communicating
with the renal pelvis and calices before and during the operation.
The objective lens of the laparoscope can be used to explore the
bottom of the cyst by using the magnification effect of laparoscopy
before the operation. During the operation, methylene blue can be
injected through the ureteral catheter after the cyst is uncapped
and then the blue liquid can be observed at the bottom of the sac.
Although Tang et al (11)
documented 11 cases of recurrence in 41 patients with laparoscopic
deroofing and zero recurrence in 41 patients in the ureteroscopy
group. Tang et al (11) did
not analyze the reasons why the recurrence rate was so high in the
laparoscopic group. The reason for such high heterogeneity in his
article may be the difference in surgical proficiency and
experience of clinicians, or it may be that different surgeons
performed laparoscopic surgery. For patients with intraoperative
cysts connected to the collection system, 4-0 absorbable line was
used for repair, fat backfilling was given in the cystic cavity and
double J tubes were indwelled after surgery. The implementation of
these measures in the operation will also directly lead to the
prolongation of the operation time. This meta-analysis found that
there was no significant difference in the recurrence rate 6 months
after operation between the ureteroscopy group and the laparoscopic
group.
In terms of efficacy, laparoscopy has a higher
success rate of cyst disappearance in postoperative imaging review.
The advantage of ureteroscopy is that it can shorten the operation
time, intraoperative blood loss, postoperative anal exhaust time,
postoperative hospital stay and costs. There was no significant
difference in postoperative recurrence and complications between
the two surgical methods (Fig. 4,
Fig. 5, Fig. 6, Fig.
7 and Fig. 8). The flexible
ureteroscopy is operated through the retrograde urinary tract path,
which is more direct to the peripelvic renal cyst than laparoscopic
surgery (20). Therefore, it is
very important to obtain the exact location of the cyst during the
incision and internal drainage of the peripelvic renal cyst using a
flexible ureteroscope. A number of studies have found that
computerized tomography (CT) urogram, CT plain scan, retrograde
urography, transvenous urography and Doppler ultrasound are
recommended to determine accurate position of cysts before surgery
(20-26).
Intraoperative localization of renal cysts. A
randomized controlled trial study in China found that injection of
methylene blue into pelvic para-renal cysts could significantly
reduce the time to find and identify cysts under flexible
ureteroscopy and shorten the operative time (27). Some studies (3,28)
consider that preoperative multiplanar reconstruction-CT urogram
and intraoperative ultrasound guidance can make the flexible
ureteroscope easily to find the cyst wall, so as to obtain an
improved therapeutic effect (accurate finding of cysts, reducing
bleeding and urinary fistula), compared with the simple use of
flexible ureteroscope technology. To the best of the authors'
knowledge, Chen et al (29)
attempted to treat peripelvic renal cysts using a 1,470 nm laser.
This is a near-infrared laser and the wavelength of 1,470 nm can be
absorbed by both water and hemoglobin at the same time. It has the
advantages of high cutting efficiency, complete hemostasis and
little thermal damage to tissues, which meets the requirements of
precision surgery. Compared with holmium laser treatment, the 1,470
nm laser showed more concentrated heat and tissue penetration of
2-3 mm (30). The 1,470 nm laser
is able to reduce intraoperative bleeding, open the cyst opening
and the outflow of cyst fluid, so as to achieve improved surgical
results; a good development direction for flexible ureteroscopic
surgery.
The present meta-analysis compared the two
treatments for parapelvic cysts from different aspects. Each has
its advantages and disadvantages (Table I). It is important for treatment
decisions to focus on patient selection and the expertise of the
surgeon. As most parapelvic cysts have a certain compression on the
collection system and are separated from the collection system by
only a thin wall, cysts can be found in the natural passages of the
human body, retrograde urinary system, incision and internal
drainage of cysts by holmium laser through ureteroscope and there
are generally fewer blood vessels in the cyst wall on the side of
the collection system, so the blood loss during holmium laser
incision is less and the damage to patients is mild.
Gastrointestinal function recovered more quickly and hospital stay
is shorter after surgery.
By analyzing these considerations, the present
meta-analysis compared the advantages and disadvantages of two
common surgical regimens for the treatment of parapelvic renal
cysts. Of course, if more randomized studies can be added in the
future to obtain larger sample sizes, more comprehensive
information and more standardized protocols, we will get more
in-depth comparison results.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by Huzhou Science and
Technology Bureau Project (grant no. 2022GYB36).
Availability of data and materials
Not applicable.
Authors' contributions
JG and MZ extracted the data from selected studies
for inclusion. RW made substantial contributionsto conception and
design. JT and ZF analyzed and interpreted data. HZ conducted a
strict audit of the extracted data to ensure its quality. JG and MZ
extracted the information from all the included studies. YC
collected and analyzed information and JG wrote the manuscript. All
authors read and approved the final manuscript. Data authentication
is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Basiri A, Hosseini SR, Tousi VN and
Sichani MM: Ureteroscopic management of symptomatic, simple
parapelvic renal cyst. J Endourol. 24:537–540. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Taguchi K, Harper JD, Stoller ML, Duty BD,
Sorensen MD, Sur RL, Usawachintachit M, Tzou DT, Wenzler DL,
Isaacson D, et al: Identifying factors associated with need for
flexible ureteroscope repair: A Western Endourology STone (WEST)
research consortium prospective cohort study. Urolithiasis.
46:559–566. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang R, Wang N, Tang J, Chen Y and Gao J:
The safety and efficacy of MPR-CTU combined with precise
intraoperative ultrasonography guided flexible ureteroscope in the
treatment of renal cystic disease. Exp Ther Med. 15:283–287.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Liu Z, Zhao Y, Wang X, Song M and Shi B:
Critical reviews of 1470-nm laser vaporization on benign prostatic
hyperplasia. Laser Med Sci. 33:323–327. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Higgins JPT and Green S: Cochrane handbook
for systematic review of interventions. Version 5.1.0, The Cochrane
Collaboration, 2011.
|
|
6
|
Zhu W, Zhu Q, Zeng F, Gao X and He Y:
Comparison of holmium laser ureteroscopic intrapelvic drainage vs.
retroperitoneal laparoscopy for the treatment of peripelvic cyst.
Chin J Exp Surg. 31(2)2014.(In Chinese).
|
|
7
|
Li X and Lin C: A comparative study of
three different methods in the treatment of parapelvic cysts. J
Chin Phys. 1726–1728. 2022.(In Chinese).
|
|
8
|
He H, Li L, Tao Z and Wang W: Flexible
ureteroscopy versus laparoscopy in treatment of parapelvic cyst. J
Mod Clin Med. 42:417–419. 2016.
|
|
9
|
Sun Y, Du D and Wu Y: To compare the
effect of flexible ureteroscopy holmium laser incision and internal
drainage and retroperitoneal laparoscopic cyst unroofing in the
treatment of parapelvic cyst. Henan Med Res. 26:1570–1571. 2017.(In
Chinese).
|
|
10
|
Chen H, Chen G, Pan Y and Jin X: Minimally
invasive surgeries in the management of renal parapelvic cysts: A
retrospective comparative study. Urol J. 18:389–394.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tang R, Yang J, Wan L and Yang Z: Clinical
effect of flexible ureteroscope and laparoscope in the treatment of
parapelvic cyst. Biomed Res Int. 2022(5718923)2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Guo H, Liu C, Sun J and Zhang X:
Comparison of holmium laser incision and internal drainage under
flexible ureteroscope and retroperitoneal laparoscopic
decompression to stress response in patients with parapelvic cyst.
J Third Mil Med Univ. 43:1258–1262. 2021.
|
|
13
|
Meng X and Mi Q: Transurethral flexible
ureteroscopic incision and drainage with holmium laser in the
treatment of parapelvic renal cysts: A retrospective study. INT
BRAZ Journal of Urology. 48:842–849. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Meola M, Samoni S and Petrucci I: Clinical
scenarios in chronic kidney disease: cystic renal diseases. Contrib
Nephrol. 188:120–130. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ishida K, Yuhara K and Kanimoto Y: A case
of acute renal failure due to parapelvic cyst in a solitary kidney.
Hinyokika Kiyo. 51:261–263. 2005.PubMed/NCBI(In Japanese).
|
|
16
|
Camargo AHLA, Cooperberg MR, Ershoff BD,
Rubenstein JN, Meng MV and Stoller ML: Laparoscopic management of
peripelvic renal cysts: University of California, San Francisco,
experience and review of literature. Urology. 65:882–887.
2005.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hoenig DM, McDougall EM, Shalhav AL,
Elbahnasy AM and Clayman RV: Laparoscopic ablation of peripelvic
renal cysts. J Urol. 158:1345–1348. 1997.PubMed/NCBI
|
|
18
|
Yoder BM and Wolf JS Jr: Long-term outcome
of laparoscopic decortication of peripheral and peripelvic renal
and adrenal cysts. J Urol. 171:583–587. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Morgan C Jr and Rader D: Laparoscopic
unroofing of a renal cyst. J Urol. 148:1835–1836. 1992.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yu W, Zhang D, He X, Zhang Y, Liao G, Deng
G and Jin B: Flexible ureteroscopic management of symptomatic renal
cystic diseases. J Surg Res. 196:118–123. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Mancini V, Cormio L, d'Altilia N,
Benedetto G, Ferrarese P, Balzarro M, Defidio L and Carrieri G:
Retrograde intrarenal surgery for symptomatic renal sinus cysts:
Long-term results and literature review. Urol Int. 101:150–155.
2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhao Q, Huang S, Li Q, Xu L, Wei X, Huang
S, Li S and Liu Z: Treatment of parapelvic cyst by internal
drainage technology using ureteroscope and holmium laser. West
Indian Med J. 64:230–235. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Li EC, Hou JQ, Yang LB, Yuan HX, Hang LH,
Alagirisamy KK, Li DP and Wang XP: Pure natural orifice
translumenal endoscopic surgery management of simple renal cysts:
2-Year follow-up results. J Endourol. 25:75–80. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Liaconis H, Pautler SE and Razvi HA:
Ureteroscopic decompression of an unusual uroepithelial cyst using
the holmium: YAG laser. J Endourol. 15:295–297. 2001.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Luo Q, Zhang X, Chen H, Liu Z, Chen X, Dai
Y and Zhao Z: Treatment of renal parapelvic cysts with a flexible
ureteroscope. Int Urol Nephrol. 46:1903–1908. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mao X, Xu G, Wu H and Xiao J:
Ureteroscopic management of asymptomatic and symptomatic simple
parapelvic renal cysts. BMC Urol. 15(48)2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang Z, Zeng X, Chen C, Wang T, Chen R and
Liu J: Methylene blue injection via percutaneous renal cyst
puncture used in flexible ureteroscope for treatment of parapelvic
cysts: A modified method for easily locating cystic wall. Urology.
125:243–247. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shen J, Chen Y and Wang R: Efficacy and
complication of flexible ureteroscopic holmium laser incision for
simple renal cysts: A retrospective study. J Endourol. 33:881–886.
2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Chen Y, Wang R, Shen X, Tang J, Shen J,
Fang Z, Shi Z and Jin X: Ultrasonography-assisted flexible
ureteroscope for the treatment of parapelvic renal cysts: A
comparison between the 1470-nm diode laser and the holmium laser.
Exp Ther Med. 21(172)2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhao Y, Liu C, Zhou G, Yu C, Zhang Y and
Ouyang Y: A retrospective evaluation of benign prostatic
hyperplasia treatment by transurethral vaporization using a 1470 nm
laser. Photomed Laser Surg. 31:626–629. 2013.PubMed/NCBI View Article : Google Scholar
|