Introduction
Ischemic fasciitis (IF) is a rare, benign
fibroblastic/myofibroblastic proliferation that mimics a
soft-tissue sarcoma both clinically and histologically. The
majority of patients with IF are elderly and a number of them are
debilitated or immobilized, bedridden or wheelchair-bound (1-3).
Its favored locations are trunk regions over bony prominences, such
as the shoulder, sacrum or greater trochanter (1-3).
Most patients show a painless mass of short duration, usually <6
months (3). IF tend to be poorly
circumscribed and multinodular, and typically involves subcutaneous
tissue (3). Proliferating cells in
IF may be cytologically atypical features with hyperchromatic
swollen nuclei and prominent nucleoli (3). From the therapeutic point of view, an
accurate diagnosis is needed because most IF cases are cured by
conservative therapy alone (3). We
encountered an elderly, mobile patient with IF that was clinically
suspected of being an aggressive sarcoma. We herein describe the
clinicopathological features of the present case to share our
experience of such self-limiting, pseudosarcomatous lesions.
Case report
A 76-year-old man, in good health and
self-supporting as regards activities of daily living (ADL), except
for medication for hypertension, was admitted to the National
Defense Medical College Hospital (Tokorozawa, Japan). His chief
complaint was a slowly growing, painless soft-tissue mass that had
been evident on his right back for two months. He was relatively
thin, and the mass was located above a rib bone. This mass was
chicken-egg-sized, elastic hard, and immobile without skin
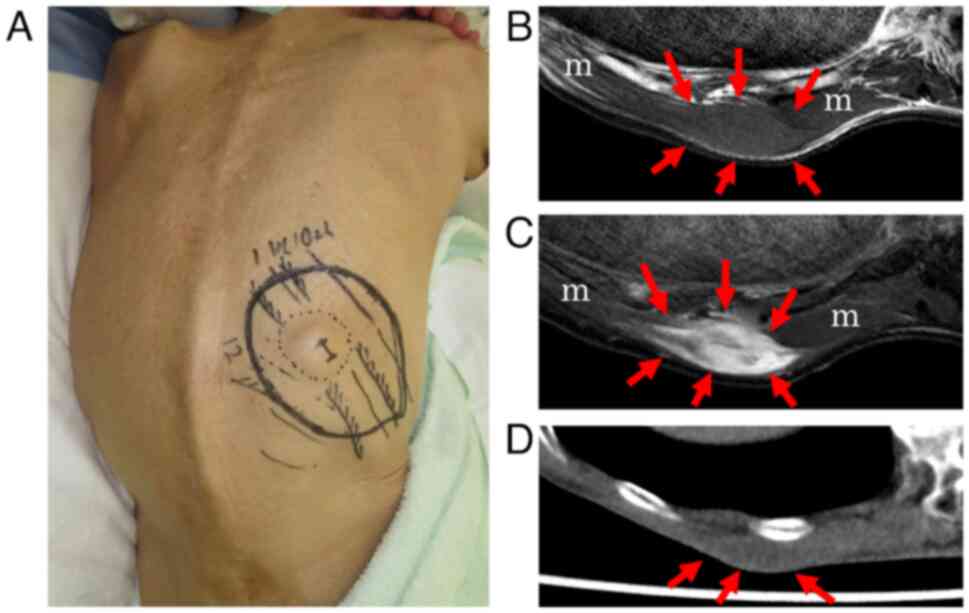
ulceration (Fig. 1A). An
ultrasound examination showed a mass with an acoustic shadow and
highly echogenic capsule. Magnetic resonance imaging (MRI) revealed
a 33-mm subcutaneous mass focally involving the latissimus dorsi
muscle. T1-weighted (T1W) images showed a signal that was slightly
hyperintense versus skeletal muscle (Fig. 1B), while T2-weighted (T2W) and
diffusion-weighted imaging (DWI) showed hyperintense signal mixed
with heterogeneous low-intensity areas (Fig. 1C). Tail-like signs were observed
from this tumor. X-ray computed tomography (CT) showed no bony
involvement (Fig. 1D). These
imaging features indicated a possible diagnosis of myxofibrosarcoma
or other myxoid sarcoma. Extensive surgical resection was planned,
and a preoperative incisional biopsy was performed. Based on the
resulting pathological diagnosis, the scheduled surgery was
canceled, and the patient was placed under conservative
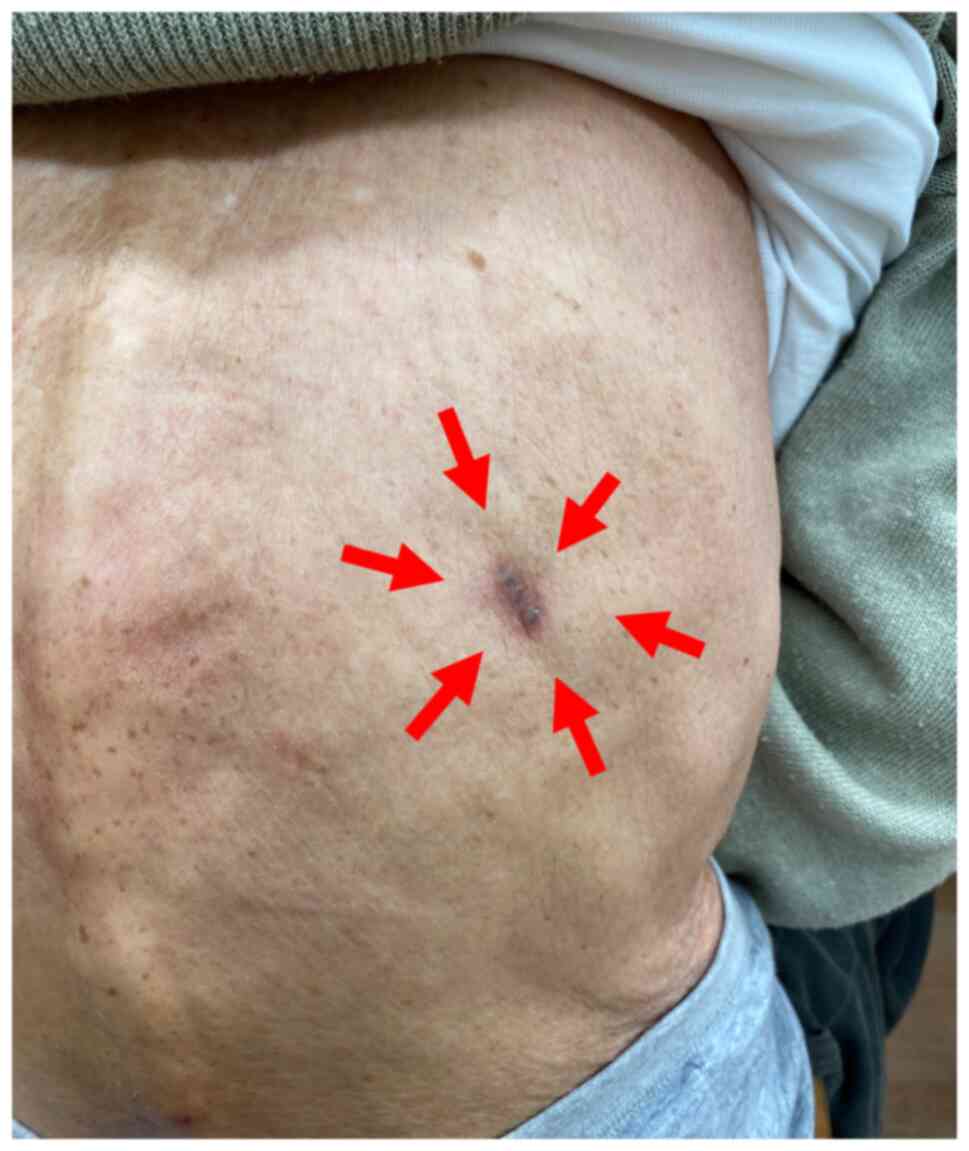
observation. This tumor gradually shrank in size, and had
completely disappeared after ~5 months (Fig. 2). One year after the biopsy
procedure, the patient is alive, and remains well with no
recurrence.
Pathological findings
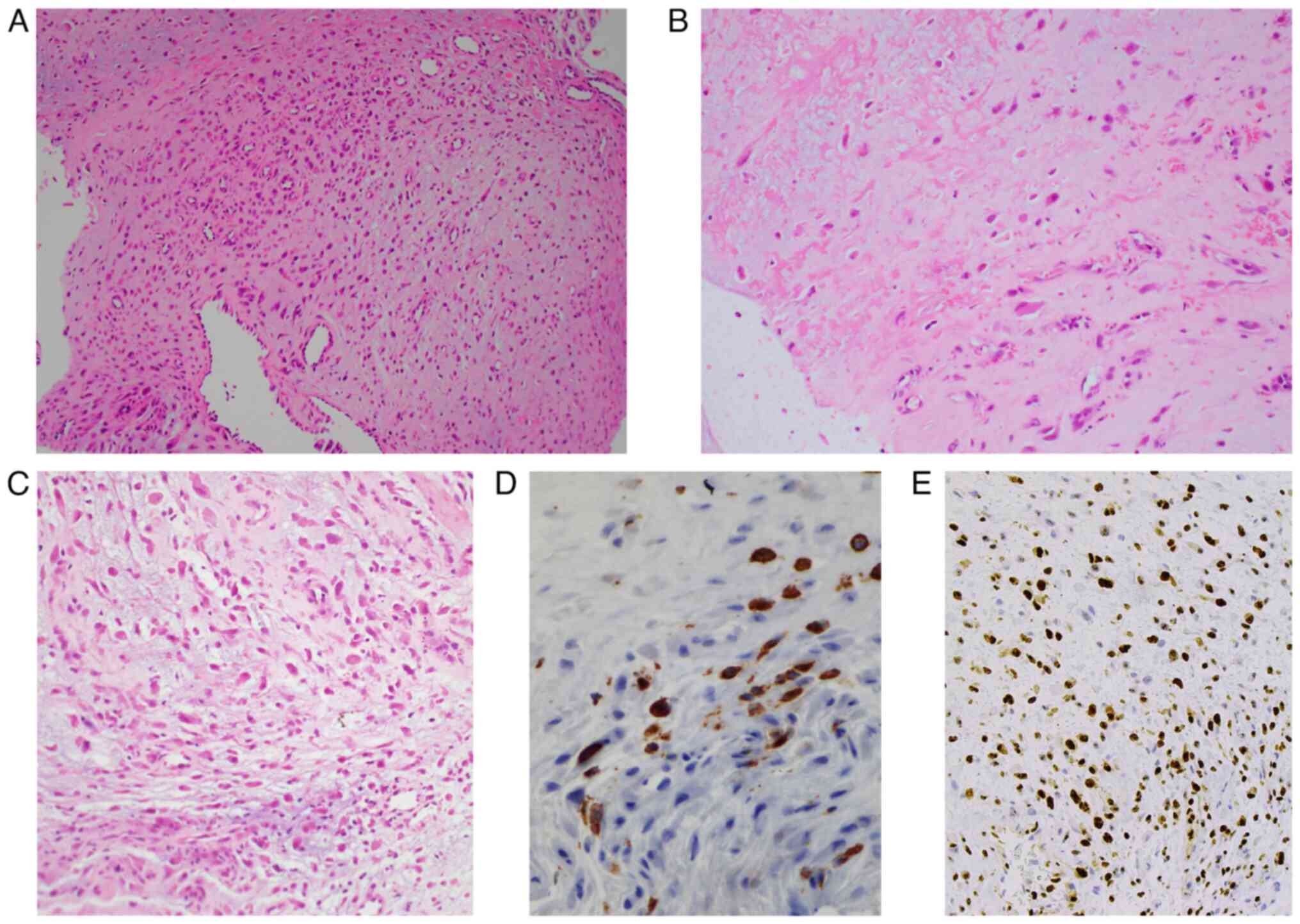
The biopsy specimens were composed of fragmented
soft tissues, and showed spindle or stellate cells, sometimes with
swollen round-to-oval nuclei, proliferating within the myxoid
fibrous tissues (Fig. 3A).
Fibrin-like material deposits were also present in the myxoid
stroma (Fig. 3B). Cellularity was
relatively low, but focal cellular areas composed of short spindle
cells with hyperchromatic nuclei were found. Some proliferating
cells had conspicuous nucleoli. No abnormal mitoses were observed.
Granulation tissue-like neovascularization containing enlarged
endothelial cells was focally recognized (Fig. 3C). Necrotizing vasculitis was not
observed. Immunohistochemically, proliferating spindle/stellate
cells were focally positive for CD68 (PGM1) (Fig. 3D) and negative for keratin
(AE1/AE3), alpha-smooth muscle actin, S-100 protein, myogenin,
desmin, and CD34. The Ki-67 index was ~25% in hot spots (Fig. 3E). These findings suggested a
diagnosis of IF.
Discussion
IF was first described as ‘atypical decubital
fibroplasia’ by Montgomery et al in 1992(1), and similar lesions were reported by
Perosio et al as ‘ischemic fasciitis’ in 1993(2). IF is a pseudosarcomatous
proliferative disease of reactive fibroblasts/myofibroblasts
associated with repair or healing of tissues that are necrotic or
destructed, possibly due to intermittent ischemia (1-3).
IF commonly occurs at sites of chronic mechanical pressure and
abrasion, such as bony prominences during prolonged bed rest,
immobilized postures, and wheelchair or orthotic use, particularly
in debilitated elderly patients (1-10).
IF uncommonly arises in young or middle-aged patients, and in
almost all such cases it is associated with physical pressure or
trauma (1,2,4-8).
In the present case, the patient was elderly, but mobile and
independent in ADL with no traumatic or decubital episodes.
Therefore, making a clinical diagnosis of IF was challenging. The
back was also considered not to be a favored location for IF.
Retrospectively considered, however, the patient was relatively
thin, suggesting that ischemia could occur just above the rib
bone.
IF is a benign disease that is expected to resolve
spontaneously in some cases (11).
However, as in our case, IF sometimes shows cellular atypia, a
variable frequency of mitosis, or myxoid changes in the stroma, and
may mimic sarcomatous lesions, such as myxofibrosarcoma, myxoid
chondrosarcoma, undifferentiated pleomorphic sarcoma, and
epithelioid sarcoma (1,2,4-6).
In excisional specimens, ‘zonal features’, which consist of a
central necrotic area and peripheral proliferation of
fibroblasts/myofibroblasts with granulation-like reactive vascular
hyperplasia and inflammatory cells, are useful for diagnosis as
they are not seen in sarcomas (1-4,6,7,11-14).
There is a high risk of misdiagnosis due to the likelihood of zonal
features being unclear in the fine-needle aspiration specimens
(6,15) and probably in other small
specimens. In the present case, the biopsy specimens were small and
fragmented, and zonal features were indistinct. However, the
detailed histology revealed fibrinoid necrosis/fibrin-like deposits
and myxofibrous stroma with focal neovascularization, findings that
were suggestive of the central and peripheral parts of zonal
features. In addition, degenerative and reactive changes are
helpful for diagnosis, such as myxoid degeneration, fat necrosis,
erythrocyte extravasation, and hemosiderin deposition (1,2,4).
An accurate diagnosis of IF is important to avoid
unnecessary extensive surgery. In fact, in the present case, the
tumor disappeared within several months after cancelation of the
planned surgery. Even in piecemeal specimens where the zonal
structure is unclear, in our experience the findings of a necrotic
lesion with fibrous stroma and degenerative/reactive changes, such
as myxoid changes, may provide us with clues to the correct
diagnosis. A diagnosis of IF should be kept in mind and should be
within lists employed for differential diagnosis when the patient
is elderly, even if not bedridden or immobile.
In conclusion, the diagnosis of IF is challenging in
patients with independent ADLs. The presence of fibrin-like
deposits and myxofibrous stroma may be hallmarks for its correct
diagnosis.
Acknowledgements
The authors thank Dr Robert Timms of English
Language Editing in Biomedical Sciences (Birmingham, UK) for his
skillful English-editing. The abstract was presented at the 111th
Annual Meeting of the Japanese Society of Pathology Apr 14-16 2022
in Kobe, Japan and published as abstract no. P-176 in Proc Jpn Soc
Pathol 111(1): 2022.
Funding
Funding: No funding was received.
Availability of data and materials
Data sharing is not applicable to this article as no
datasets were generated or analyzed during the study.
Authors' contributions
AM and SM conceived and designed the study. AM and
SM confirm the authenticity of all the raw data. AM, YS and SK
provided examined materials. AM, YS, SO and SM performed the
histopathological examination. SK and MS were involved in the
patient's clinical management and analyzed patient data. AM, SO and
YS collected appropriate references. AM wrote the paper. SM, SO and
MS reviewed and edited the manuscript. All authors read and
approved the final manuscript and agree to be accountable for all
aspects of the research in ensuring that the accuracy of integrity
of any part of the work are appropriately investigated and
resolved.
Ethics approval and consent to
participate
Ethical committee approval was provided from the
Faculty of Medicine, National Defense Medical College board
(approval no. 4480).
Patient consent for publication
Written consent for publication of the case report
and any accompanying images, without any potentially identifying
information, was provided by the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Montgomery EA, Meis JM, Mitchell M and
Enzinger F: Atypical decubital fibroplasia. A distinctive
fibroblastic pseudotumor occurring in debilitated patients. Am J
Surg Pathol. 16:708–715. 1992.PubMed/NCBI
|
|
2
|
Perosio PM and Weiss SW: Ischemic
fasciitis: A juxta-skeletal fibroblastic proliferation with a
predilection for elderly patients. Mod Pathol. 6:69–72.
1993.PubMed/NCBI
|
|
3
|
Goldblum JR, Folpe AL and Weiss SW:
Enzinger and Weiss's Soft tissue tumors. 7th edition. Elsevier
Health Sciences, Philadelphia, PA, 2020.
|
|
4
|
Liegl B and Fletcher C: Ischemic
fasciitis: Analysis of 44 cases indicating an inconsistent
association with immobility or debilitation. Am J Surg Pathol.
32:1546–1552. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yamamoto M, Ishida T and Machinami R:
Atypical decubital fibroplasia in a young patient with
melorheostosis. Pathol Int. 48:160–163. 1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Washing D and Zaher A: Pathologic quiz
case: A 76-year-old debilitated woman with a right thigh mass.
Ischemic fasciitis (atypical decubital fibroplasia). Arch Pathol
Lab Med. 128:e139–e140. 2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sakamoto A, Arai R, Okamoto T, Yamada Y,
Yamakado H and Matsuda S: Ischemic fasciitis of the left buttock in
a 40-year-old woman with beta-propeller protein-associated
neurodegeneration (BPAN). Am J Case Rep. 19:1249–1252.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Baldassano MF, Rosenberg AE and Flotte TJ:
Atypical decubital fibroplasia: A series of three cases. J Cutan
Pathol. 25:149–152. 1998.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wader J, Gajbi N and Kumbhar S: Ischaemic
fasciitis: A very rare entity with unusual presentation. J Clin
Diagn Res. 7:2952–2953. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Padmanaban D, Rangasami R, Chandrasekharan
A and Swaminathan R: Decubital ischemic fasciitis presenting in an
unusual location. Radiol Case Rep. 6(590)2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lehmer LM, Moore JB and Ragsdale BD:
Ischemic fasciitis: enhanced diagnostic resolution through
clinical, histopathologic and radiologic correlation in 17 cases. J
Cutan Pathol. 43:740–748. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ulus OS, Karaarslan E, Saglican Y and
Yakupoglu A: Case report: MRI of decubital ischemic fasciitis.
Indian J Radiol Imaging. 21:111–112. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Gavin M, Sharp L, Atkins R and Tarbox M:
Ischemic fasciitis in a debilitated older man. Proc (Bayl Univ Med
Cent). 32:429–430. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ilaslan H, Joyce M, Bauer T and Sundaram
M: Decubital ischemic fasciitis: Clinical, pathologic, and MRI
features of pseudosarcoma. AJR Am J Roentgenol. 187:1338–1341.
2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chatura KR, Katyal A and Hiremath SS:
Fine-needle aspiration cytology in soft tissue tumors: How far did
we go? J Adv Clin Res Insights. 2:107–111. 2015.
|