1. Introduction
As reported from the Hellenic Classical Era,
hematidrosis is a rare medical cutaneous condition (International
Classification of Diseases/ICD-10: L 74.8) which has rarely been
noted throughout the ages. It is regarded as an eccrine sweat
disorder, which is defined as the spontaneous dermatological
excretion of a mixture of blood and sweat directly from
non-traumatized skin. The pathological mechanism of blood oozing
from the skin and mucosa remains unclear. However, it is
hypothesized that dermal deficiencies can lead to blood-filled
spaces, which may be exuded into follicular canals, or directly to
the skin surface, demonstrating this peculiar phenomenon (1,2). As
a medical term, it is composed of two Greek words ‘hema’ (blood)
and ‘idrosis’ (sweating), while certain other associated terms used
in the English medical literature include the words stigmata (also
of Greek origin, hysterical stigmata), diapedesis (also of Greek
origin, meaning jumping through), vicarious menstruation,
ephidrosis cruenta (Greco-Latin origin), sudor cruentus and sudor
sanguineus (Latin terms) (3).
Hematidrosis, is classed as a somatic symptom disorder, almost
always related to psychic imbalance, ranging from acute or chronic
anxiety to fear (rivalry, scolding, punishment, bullying). Reports
exist of extensive unnecessary investigations, which at times, have
led towards risky therapeutic interventions (1,2,4).
Thomas K. Chambers in 1861, suggested that this strange experience
had triggered a ‘need to publish’ trend of case reports that
otherwise may have been neglected. Nevertheless, the majority of
available articles on the subject have appeared over the past
decades. In Christianity, its notorious appearance was connected to
the agony in the biblical historical reference on the ‘bloody
tears’ of Jesus Christ in the Garden of Gethsemane (1,5).
The present study, inspired by the nature of
hematidrosis itself, aimed to highlight both the hallmarks in the
history of medicine, as well as the currently available scientific
evidence. By searching through the archives of the literature in
the past and simultaneously conducting a narrative review of the
recent research, the present study aimed to provide a clearer
picture and a thesaurus for this ‘marvel’ entity in
dermatology.
2. Literature search strategy
A research strategy was developed to identify
relevant literature. This included selecting key search terms and
deciding on the criteria of inclusion and exclusion. Moreover,
certain conditions were set that are critical to the quality and
breadth of the present scoping review, framed by historical and
epistemological sources, starting from their compatibility and
retrospective consistency in the clinical context. The Preferred
Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)
guidelines were used consultatively to avoid a major quality
deficit regarding the studies included (6). The key words which were used to
render and describe this clinical entity were verbally similar
diagnostic terms concerning their syllabic pronunciation to provide
access to appropriate articles, chapters and books and various
references, thus explaining the intended dual search. Key words
included hemaditrosis, haematidrosis, hemathidrosis, αίµα and
ιδρώτας (blood and sweat for the Greek texts), diapedesis, stigmata
hysterica, sudor cruentus and sudor sanguineus (bleeding sweat and
bloody sweat for the Latin texts). All terms are considered
directly related to the research question. The present narrative
review was based on original studies, clinical case reports and
series, opinion articles, letters to the editor and review articles
to investigate recent knowledge. A thorough survey was conducted in
the online medical database PubMed/Medline for studies published
over the past two decades until December 1, 2022. To limit the
search and to set criteria, full-text articles published in the
English language were only included. The eligibility of each
citation was based on the title, abstract and full content of the
articles considered and retrieved, taking into account the
predefined admission criteria, such as methodological excellence,
authorship, the relevance of the responsible correspondence author,
and the quality and visibility characteristics of the biomedical
journal hosting the publication. The factors that were evaluated
covered the frequency of recording the clinical entity, management
parameters, the time course of clinical manifestations, coexisting
pathologic conditions and the socio-demographic and clinical
characteristics of the patients. For the historical investigation,
a bibliographic review was conducted using a documentary research
methodology, applying the same key words as aforementioned. The
year 1900 marked the end of the historical research. The survey
included the following: i) Texts of antiquity within the online
database Thesaurus Linguae Graecae (TLG) in Latin and Greek
language; ii) works within Gallica Digital Library (Gallica-BnF) in
the French language; and iii) books within online Google Digital
Book Index (Google Books) in the English, French, German, Italian
and Latin languages. Full-text availability was set as a criterion.
Cases associated with religion and religious books were excluded
for possible bigotry and deisidaimonía (superstition) to be
avoided. On the other hand, this exclusion criterion may provoke a
bias concerning cases with true hematidrosis. Thus, cases
presenting hematidrosis during stigmata phenomenon were excluded
from the main review; however, as they were partly connected to the
symptom in study, they are being historically perused, discussed
and registered independently.
3. Results of the literature search
Historical records unveiled relevant fragments of
treatises during Greek antiquity, the case of Jesus Christ in early
Christianity and 64 works with case references from the Renaissance
until 1900. A summary of nine works had been included from within
TLG, seven from Gallica-BnF and 57 form Google Books. Of the cases
referred, 29 were in English, 13 in French, 13 in Latin, eight in
German and one in Italian. Among the 64 works, 70 hematidrosis
incidents were revealed. The mean age of those who suffered was
25.6 years. The time expanse for case reports was 426 years
(Table I). The female sex was
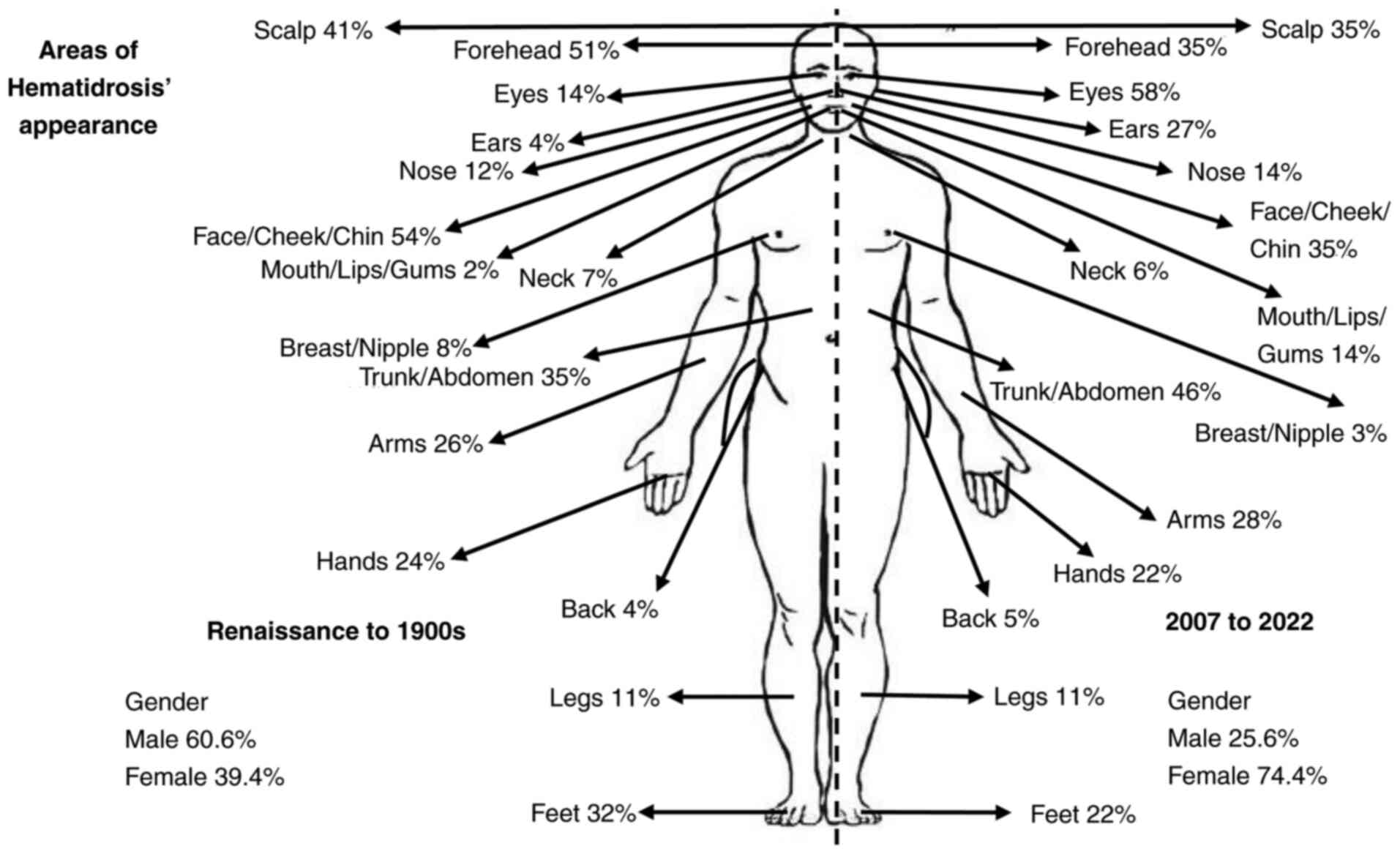
recorded in 39.7% of the affected individuals (Fig. 1). Articles in other languages (one
in Russian, one in Czech and two in Spanish) were excluded, as well
as some cases with no full texts (five works). A systematic search
of the current medical literature of the past two decades retrieved
56 articles, 37 of which were eligible for all data requirements to
have been included in the present review. Non-English articles,
nine in total, five publications with no abstract or text
available, and five overlapping publications were isolated and
excluded. Among the 37 articles identified, a total of 44 cases
were recorded. The mean age of the affected individuals was 15.8
years. The female sex exhibited a 74.4% dominance. The total time
span was 15 years (2008-2022) (Table
II). The number of articles on hematidrosis presents with a
peak during the second half of the 19th century and after 2007.
Until the end of 19th century, articles had appeared in Latin,
Italian, German, French and English languages, with English
language encompassing the majority of articles, followed by French
and Latin. Over past two decades, all articles are written in
English. A comparison of the bodily areas of the appearance of
hematidrosis between the two eras in question is demonstrated in
Fig. 1. Cases of famous
individuals, 26 in total, experiencing hematidrosis under stigmata
exposure are registered separately (Table III).
 | Table IWorks with references to hematidrosis
cases from the Renaissance until 1900. |
Table I
Works with references to hematidrosis
cases from the Renaissance until 1900.
| No. | Original
authora | Case | Body locations of
hematidrosis | Work and year of
publication |
|---|
| 1 | Johannes Müller von
Königsberg (32)
(Regiomontanus) | Young boy accused
for a crime | Whole body | Ephemerides,
1474 |
| 2 | Leonardo da Vinci
(98) | Soldier departing
for battle | Forehead, whole
body | Ca 1503, La
Battaglia di Anghiari era (Malvin Pilato, The Memoirs of Dr.
Michael Arthur Creed, 2010) |
| 3 | Jacques Auguste de
Thou (17) | Italian officer of
Monte Maro fortress proposed to surrender or die | Whole body | Historia sui
temporis, 1560-1584, (French translation of 1711) |
| 4 | Jacques Auguste de
Thou (17) | Young Florentine
sentenced to death by Pope Sixtus V | Whole body and
tears | Historia sui
temporis, 1560-1584, (French translation of 1711) |
| 5 | Wilhelm Fabricius
von Hilden (23) | 12-year-old child
after drinking red wine | Gums, every part of
integuments, nose | Observationem et
curationem chirurgicam centuriae sex, 1606 |
| 6 | Wilhelm Fabricius
von Hilden (23) | 45-year-old widow
losing her only son | Upper part of the
body, back of the head, temples, eyes, nose breast, tips of the
fingers | Observationem et
curationem chirurgicam centuriae sex, 1606 |
| 7 | Henricus ab Heer
(23) | Man | Bloody sweat with
worm like coagulation | Observo
Medicinalis, ca 1600-1636 |
| 8 | Georg Spörlin
(24) | 12-year-old boy
with high fever | Whole body | Letter in Wilhelm
Fabricius Hildanus. In: Opera quæ extant omni, 1627 |
| 9 | Paolo Zacchia
(22) | Young man condemned
to die in flames | Whole body | 1628 (Quaestiones
medico-legales, 1621-1651) |
| 10 | François Eudes de
Mézeray (17) | Charles IX King of
France | Whole body (pores
and conduits) | Histoire de France
depuis Faramond jusqu'au règne de Louis le juste, 1643-1651 |
| 11 | François Eudes de
Mézeray (17) | Mayor of a town
destroyed by a heavy storm and condemned to die | Whole body | Histoire de France
depuis Faramond jusqu'au règne de Louis le juste, 1643-1651 |
| 12 | James Henry Pooley
(14) | Sailor during a
storm | Whole body | Memoirs of the
Society of Arts of Haarlem (Popular Science Monthly, 1884) |
| 13 | Thomas Bartholinus
(22) | Various cases after
vehement terror agonies of torture | Whole body | De nivis usu medico
observationes variae Chapter XXII, 1661 |
| 14 | Du Gard (32) | 3-month-old child
dying | Nose, ears, hinder
part of the head, fingers, toes | Philosophical
Transactions, 1674 |
| 15 | S. Ledelius
(25) | Woman nursing | Breasts | Sudor sanguineus.
Misc Curiosa, Sive, Ephemaridum MedicoPhysicarum Germanicarum,
1683 |
| 16 | Herman Boerhaave
(19) | Girl suffering from
cold finger syndrome | Whole body | Ca 1688-1720
(Index-catalogue of the Library of the Surgeon-General’s Office,
United States Army, 1889) |
| 17 | Johannes Franciscus
Vicarius (32) | Newborn boy | Right arm | De sudore cruento
frequentiore, Misc. Acad. Nat. Curios., 1694 (Magnet JJ.
Bibliotheca medico-pratica sive rerum medicarum thesaurus
Cumulatissimus, 1698) |
| 18 | S. Ledelius
(25) | Man with
scurvy | Whole body | Manget JJ.
Bibliotheca medico-practica sive rerum medicinarum thesaurus,
1697 |
| 19 | Ido Wolf (32) | 43-year-old man,
cranial trauma | Cranium | Observationum
chirurgico-medicarum libri II, cum scholiis & variis
interspersis historiis medicis, 1704 |
| 20 | J.C. Schilling
(32) | Boy in coma and
convulsive disorder | Whole body | Case of Bloody
Sweat, 1747 (Popular Science Monthly, 1884) |
| 21 | Antonii Mesaporiti
(32) | Young lady | Whole body | Epistola D. Antonii
Mesaporiti, M. C. Genuensis ad Cl. Antonium Vallesnerium, 1753 |
| 22 | Christiani
Ehrenfried Eschenbach (32) | Girl | Whole body | Sudor sanguineus;
urina sudore et vomitu rejecta, Observata
anatomico-chirurgico-medica rariora, 1769 |
| 23 | Albrecht Von Haller
(32) | Woman, uterus
cancer | Whole body | Anfangsgruende der
Phisiologie des menschlichen Koerpers, 1772 (Schneider in Fulda.
Medicinisch-chirurgische Bemerkungen uber verschiedne Gegenstande
ans der Heilkunde, 1848) |
| 24 | Gallandat (32) | 31-year-old boatman
with fatigue | Whole body | Sueur de sang. Soc.
Scient. Harlemensis, 1773 (Dictionnaire abrégé des sciences
médicales, 1822) |
| 25 | Josephi Lanzoni
(32) | Young woman
suffering from cholera morbus | Whole body | Case of Bloody
Sweat, Ephemerid. Acad. Natur. Curios., 1788 |
| 26 | John Mason Good
(32) | Various cases in
general regardless of age | Whole body | A History of
Medicine, 1795 |
| 27 | Boivin (33) | 45-year-old man
with depression and burn out syndrome | Whole body | Observation sur une
diapédèse, Journ. de Méd., Chir., Pharm, 1807 |
| 28 | F.C. Câizergues
(33) | Young lady | Face, neck, chest,
armpit | Sueur de sang
survenue quatre fois pendant la plus grande vivacité des douleurs
d’une colique néphritique. J. de Méd., Chir., Pharm., 1814 |
| 29 | James Johnson
(editor) (33) | 21-year-old woman
with irregular menstruation | Cheeks and
epigastrium | Transactions
Médicales, 1830 (The Medico-chirurgical Review, and Journal of
Practical Medicine, 1831) |
| 30 | Chauffard M.
(33) | 21-year-old woman
after a parental clash due to religious issues | Cheeks and
abdomen | Transactions
Médicales, 1830 |
| 31 | Maur Hoffmann
(22) | Man ~50 years of
age, fatigue | Arms and feet | Ca 1836, Misc Nat
Curios Dec II Ann III Obs 27 (Wochenschrift für die gesammte
Heilkunde: 1848) |
| 32 | Kaminsky (31) | Young girl | Feet | Tertianfieber mit
Ausschwitzung von Blut aus den Füssen. Med. Ztg., Berl., 1837
(Schmidt’s Jahrbuecher, 1838) |
| 33 | John Gideon
Millingen (15) | Catherine Merlin of
Chamberg, 46 years of age, received a kick from a bullock in the
epigastrium | Scalp and various
parts of the body | Curiosities of
Medical Experience, 1839 |
| 34 | C.A.W. Schneider
(31) | 50-year-old man,
fatigue 30-year-old male, fear | Feet Forehead,
cheek | Blutschwitzen.
Wochenschrift für die gesammte Heilkunde: 1848 |
| 35 | Durius (16) | Student placed in
prison | Hands, chest,
arms | (Misscel. cur.
Ephemerid.) The Cyclopædia of Biblical Literature, 1851 |
| 36 | Auguste Nicolas
Gendrin (33) | Young lady | Whole body | Des Sueurs de Sang,
1856 |
| 37 | Huss (31) | 23-year-old woman,
emotional stress | Whole body | Allg Med Cent
Zeitung Nr 97-98, 1856 |
| 38 | Erasmus Wilson
(41) | Women Woman | Forehead, chin,
cheeks | On the Diseases of
the skin, 1857 |
| 39 | Julles Parrot
(33) | 37-year-old woman
with hysteria | Face and various
parts of the body | Bulletin De
l’Enseignement Médiclae, 1859 |
| 40 | Thomas K. Chambers
(30) | 27-year-old
woman | Whole body,
nose | Case of Bloody
Sweat, Lancet, 1861 |
| 41 | F. Servaes
(31) | Man, dementia
paralytica Man, dementia paralytica | Face Face, scalp,
ear | Ueber Blutschwitzen
am Kopfe de Dementia paralytica. Centralblatt fur die Medicinischen
Wissenschaften, 1863 |
| 42 | A. von Franque
(21) | 45-year-old woman,
into pregnancy after a previous abortion | Forehead, back |
Medicinisch-chirurgische Monatshefte:
kritisches Sammeljournal für praktische Heilkunde. 1863 |
| 43 | G. Sous (36) | 9-year-old
girl | Right eye | 1866 (Annales
d’oculistique, Sueur sanguinolente, Tircher, 1869) |
| 44 | Ferdinand Ritter
von Hebra (21) | Female Female
Male | Caruncula
lachrymalis Nipples Lower limps | On Diseases of the
Skin, Including the Exanthemata, 1866 |
| 45 | McCall Anderson
(18) | 15-year-old girl
with defective and irregular menstruation | Face, chest, arms
and legs | Journal Cutan. M.,
Lond. (British Medical Journal), 1867 |
| 46 | Messedaglia &
Lombroso (84) | 23-year-old
man | Whole body | Giornale Italiano
delle Malattie Veneree e delle Malattie della Pelle, Volume 2,
1869 |
| 47 | W.T.P. Douglas
(84) | 35-year-old woman,
fatigue, tetanus | Forehead | Hematidrosis with
tetanus, 1870 (Sammuel Wilks, Hematidrosis or Bloody sweat
complicating tetanus, Guy’s Hospital Reports, 1872) |
| 48 | Schneider (16) | Sailors during a
storm | Whole body | The biblical
museum, 1871 |
| 49 | Samuel Wilks
(84) | Woman with
tetanus | Whole body | A case of
hæmatidrosis, or bloody sweat, complicating tetanus. Guy’s Hosp.
Rep., 1872 |
| 50 | Rudolf Ludwig Carl
Virchow (28) | Louise Lateau, | Forehead, dorsal
surface of the hands and feet | Professor Virchow
on Louise Lateau, The Medical Times and Gazette: A Journal of
Medical Science, Literature, Criticism, and News, 1874 |
| 51 | W.P. Hart (18) | 24-year-old young
man | Whole body | Richmond and
Louisville Medical Journal, 1875 |
| 52 | M. Tittel (29) | 20-year-old man
with fatigue | Face | A case of
Hematidrosis, Medical record: a monthly journal of medicine and
surgery, 1876 |
| 53 | McCall Anderson
(41) | 15-year-old young
lady with early menstruation | Face, arms, chest,
legs | Lectures on
Clinical Medicine, 1877 |
| 54 | R.G. Hill (42) | 4-year-old boy,
malaria | Face and neck | Case of bloody
sweat. Virginia M. Month., Richmond, 1879-80 (The Ohio Medical
Recorder, Volume 5, 1881) |
| 55 | George William
Pollard (42) | 4-year-old boy
patient of Dr Hill R.G. suffering from malaria | Whole body | Virginia Medical
Monthly, 1880 |
| 56 | W. T. Mitchell
(42) | Woman, irregular
menstruation | Whole body | Case of
Hematidrosis. Ohio Med Recorder, 1881 |
| 57 | Juan De Maldonato
(13) | Man from Paris
sentenced to death | Whole body | A commentary on the
Holy Gospels, 1888 |
| 58 | Hehir (93) | 16-year-old
girl | Head, axillae | Indian Medical
Record (The Medical News, 1893) |
| 59 | Friedrich Albin
Hoffman (22) | Man | Feet | Lehrbuch der
Constitutionskrankheiten, 1893 |
| 60 | James Craven Wood
(27) | 6-year-old girl
with cicatrized fingers after strumous ulcers on the right hand
when 7 months old | Fingers, knees,
thighs, chest and grooves of the lower eyelids | A Text-book of
Gynecology, 1894 |
| 61 | Isadore Dyer
(26) | 26-year-old
American rubber in a local Turkish bath, fatigue | Shoulders | A Case of
Hematidrosis Combined with Chromidrosis, The Medical News,
1895 |
| 62 | R. Reynolds
(38) | Various cases
suffering from smallpox | Face | Report of the
Department of Health of the City of Chicago, 1895 |
| 63 | Henri Fournier
(32) | Magistrate after
any excitement | Whole body | Journal des
maladies cutanées et syphilitiques, 1896 |
| 64 | Alma L. Rowe
(5) | Pregnant woman | Whole body | Purpura
Hemorrhagica Attended with Hematidrosis Complicating Pregnancy,
Journal of the American Medical Association, 1900 |
 | Table IIWorks with references to hematidrosis
cases from 2002 until 2022. |
Table II
Works with references to hematidrosis
cases from 2002 until 2022.
| No. | Author(s) | Person | Body locations of
hematidrosis | (Refs.) |
|---|
| 1 | Manonukul et
al | 14 years old
girl | Scalp, palms, and
occasionally from trunk, soles, and legs | (2) |
| 2 | Carvalho et
al | 9-year-old girl
after strenuous exercise or prolonged exposure to heat | Around the
mouth | (49) |
| 3 | Mishra | 13-year-old girl
with platelet factor 3 dysfunction | Eyes | (72) |
| 4 | Jerajani et
al | 72-year-old male,
suffered from continuous mental stress | Area confined to
the abdomen | (56) |
| 5 | Bhagwat et
al | 12-year-old girl,
horrifying incident with psychological stress | Forehead | (51) |
| 6 | Patel and
Mahajan | 13-year-old boy
with no underlying disease | Face, arm and
trunk | (74) |
| 7 | Wang et
al | 13-year-old girl,
emotional excitement | Subungual area,
palms, feet, thighs, and trunk | (59) |
| 8 | Praveen and
Vincent | 10-year-old girl,
severe headache lasting for few hours on facing stressful
situations | Forehead, ear
canal, nasal bridge, neck, umbilicus, wrists and legs,
hemolacria | (50) |
| 9 | Mora and Lucas | 18-year-old girl,
high stress | Nose, lacrimal
ducts, forehead, hands, nails, and navel | (48) |
| 10 | Bhattacharya et
al | 12-year-old girl
with no underlying disease | Face, limb, palm
and sole | (46) |
| 11 | Biswas et
al | 12-year-old healthy
girl with low intelligent quotient and loss of insight | Forehead, face and
body | (77) |
| 12 | Khalid et
al | Female crying as a
result of emotional outburst or even sometimes voluntarily | Eyes and ears | (82) |
| 13 | Tshifularo | 30-year-old woman,
stress 26-year-old woman with no underlying disease 34-year-old
woman, stress 18-year-old woman, stress | Bloody
otorrhea | (63) |
| 14 | Deshpande et
al | 10-year-old boy,
behavioral interventions for the child and counseling and
psychoeducation to the parents | Navel, eyes, ear
lobules and nose | (76) |
| 15 | Shen et
al | 9-year-old girl
with no underlying disease | Various parts of
the skin on her body, canthi, tongue, nails or Umbilicus | (69) |
| 16 | Varalakshmi et
al | 10-year-old girl,
significant psychological stressors, temperamental difficulties and
conflicts with mother | Eyes | (52) |
| 17 | Jafar and Ahmad
al | 12-year-old girl
with no underlying disease | Face, eye and tear
duct | (60) |
| 18 | Techasatian et
al | 9-year-old boy
after a novice monk summer retreat | Scalp, cheeks,
palms, arms and legs | (57) |
| 19 | Yeşilova et
al | 11-year-old girl
when returning from outside cold air into a warm Environment | Forehead | (61) |
| 20 | Maglie and
Caproni | 21-year-old woman,
depression and anxiety disorder | Palms and face | (65) |
| 21 | Gião Antunes et
al | 66-year-old male
with Henoch-Schönlein Purpura | Hemolacria (bloody
tears), hematidrosis and appearance of a palpable purpura on the
lower limbs, abdomen, and trunk | (55) |
| 22 | Jayaraman et
al | 10-year-old girl,
intense fear secondary to psychosocial stressor,mixed anxiety and
depressive disorder | Scalp | (68) |
| 23 | Shahgholi | 11-year-old girl
with no underlying disease 11-year-old boy with no underlying
disease 9-year-old girl | Forehead, eyes,
ears, nails, arm, umbilical area, back, vagina, and
gastrointestinal tract Hand and feet Ears lobules, nose and
eyes | (58) |
| 24 | Alsermani et
al | 9-year-old girl,
bullying at school | Scalp, ear, mouth,
and eyes | (4) |
| 25 | Meyer et
al | 10-year-old girl,
post-traumatic | Forehead | (62) |
| 26 | Hansson et
al | 9-year-old boy,
migraine | Forehead, neck,
knee and mouth | (54) |
| 27 | Pari | 10-year-old girl
with no underlying disease | Forehead and
chest | (73) |
| 28 | Ricci et
al | 15-year-old girl,
major stressful event | Eyelids and
body | (79) |
| 29 | Murota et
al | 6-year-old girl
with no underlying disease | Palms | (64) |
| 30 | Dast et
al | 15-year-old girl
following a head injury 13-year-old girl, anxiety | Ears, nose and eyes
Face, eyes, shoulders and forearm | (78) |
| 31 | Matsuoka and
Tanaka | 11-year-old girl
presenting dissociative disor ders from the age of 7 and
self-harming from 9 | Scalp, forehead,
hands and feet | (80) |
| 32 | Shafique et
al | 10-year-old girl,
experiencing significant psychosocial stress due to the recent
separation of her parents | Eyelids, ears,
scalp, axillae, vagina, rectum, abdomen, chest, neck, and
trunk | (47) |
| 33 | Hoover et
al | 9-year-old boy,
possible genetic predisposition 6-month-old girl | Ears, eyes, scalp
and other sites Ears, eyes, scalp and other sites | (89) |
| 34 | Talwar et
al | 12-year-old boy,
separated from relatives, maladaptive response to a psychosocial
stressor | Eyes, ear,
mouth | (53) |
| 35 | Tirthani et
al | 13-year-old girl,
orphan girl living with her paternal uncle and cousins | Mid face and
hands | (81) |
| 36 | Zheng et
al | 8-year-old girl,
single parent (mother) | Mouth, eyes,
forehead, oral, arms and legs and intestine | (44) |
| 37 | Alasfoor et
al | 20-year-old woman,
retinoblastoma of the left eye with enucleation and artificial eye
placement, prolonged and heavy menstrual cycles and neurological
symptoms | Eye | (45) |
 | Table IIISome cases of famous people bearing
stigmata with hematidrosis. |
Table III
Some cases of famous people bearing
stigmata with hematidrosis.
| No. | Person | Canonized |
|---|
| 1 | Marie d'Oignies (ca
1177-1213) (100) | No |
| 2 | Saint Francois
d'Assise (1181-1226) (97) | Yes |
| 3 | Helen of Hungary
(d. ca 1241) (100) | No |
| 4 | Cistercian nun
Lutgard of Aywiéres (1182-1246) (100) | No |
| 5 | Clare of Montefalco
(ca 1268-1308) (100) | No |
| 6 | Margaret Ebnerin
(d. ca 1351) (100) | No |
| 7 | Gertrude D'Oosten
(d. ca 1358) (100) | No |
| 8 | Sainte Catherine de
Sienne (1347-1380) (97) | Yes |
| 9 | Saint Liduina of
Schiedam (1380-1433) (100) | Yes |
| 10 | Sainte Rita de
Cascia (1381-1457) (97) | Yes |
| 11 | Bienheureuse Lucie
de Narni (1476-1544) (97) | No |
| 12 | Sainte Catherine de
Ricci (1522-1590) (97) | Yes |
| 13 | Hieronyme Carvaglio
(d. ca 1604) (100) | No |
| 14 | Sainte Véronique
Giuliani (1660-1727) (97) | Yes |
| 15 | Bienheureuse Anne
Catherine Emmerick (1774-1824) (97) | No |
| 16 | Maria Theresia von
Mörl (1812-1868) (97) | No |
| 17 | Maria Domenica
Lazzeri (1815-1848) (97) | No |
| 18 | Maria Beatrix
Schuhmann (1823-1887) (97) | No |
| 19 | Juliana Weiskircher
(1824-1862) (97) | No |
| 20 | Sainte Mariam
Baouardy (1846-1878) (100) | Yes |
| 21 | Louise Lateaua
(1850-1883) (97) | No |
| 22 | Madeleine Lebouca
(1853-1918) (100) | No |
| 23 | Sainte Gemma
Galgani (1878-1903) (97) | Yes |
| 24 | Saint Pio de
Pietrelcinaa (1887-1968) (97) | Yes |
| 25 | Thérèse Neumanna
(1898-1962) (97) | No |
| 26 | Marie Rose Ferron
(1902-1936) (97) | No |
4. Hallmarks in history
The phenomenon of sweat which resembles blood was
coined to the observations noted in medicine by the ancient Greeks.
Hematidrosis appeared as an affliction from the unbroken surface of
the skin and greatly attracted the interest of scholars,
medico-philosophers and theologians of antiquity. Aristotle was the
first to mention bloody sweat in two fragments of his works, ‘if
blood gets too wet people get very weak. It becomes like ichor
(pus, coagulation disorders) and appears so that many have seen
bloody sweat’ (7), and ‘Instances,
indeed, are not unknown of persons who in consequence of a
cachectic state have secreted sweat that resembled blood’ (8). Theophrastus the philosopher, the
successor of Aristotle in the Peripatetic School also mentioned
that ‘sometimes with sweat blood appears’ (9). The Greek historian, Diodorus Siculus,
in his masterpiece entitled Bibliotheca Historica reported cases of
individuals bitten by snakes tormented with pain and seized with a
bloody sweat (10). The
Pseudo-Gallenic collection of works mentioned sweat with blood into
two books, ‘De Utilitate Respirationi’ (Latin text, paraphrasing
the reports of Aristotle) and ‘De Humoribus Liber’ (Greek text,
sweats in spring and summer produced by having blood and bile)
(11). Marcus Annaeus Lucanus
noted that the human body could emit humor, such as blood from
various areas such as the limbs and nostrils (12). Hematidrosis was connected with
acute anxiety in the case of Jesus Christ prior to his arrest and
crucifixion inside the gospel of the physician and evangelist Luke,
where Christ is reported to sweat large drops of blood when he was
praying with agony in the garden of Gethsemane (Luke 22:44)
(13). This report further
enhanced curiosity as opposed to the phenomenon itself, resulting
in numerous references by scholars throughout the next centuries
and fanatic religious to state that they also similarly suffer.
Kings, state officials, military officers and common individuals in
agony under fear or hysteria were reported as cases of hematidrosis
until the 19th century (14-31).
A. Westphal wrote one of the first post-medieval dissertations on
the subject, entitled De Sudore Sanguineo in 1775(32). The article of Jules Parrot's
entitled ‘Study of bloody sweat and neuropathic hemorrhage’ in 1859
was considered in its era the most essential work on the subject.
This original work attracted attention to the appearance of
cutaneous hemorrhages and hematidrosis during paroxysms of a
neuralgia, which was extremely severe and variously located
(17,33). For some researchers, hematidrosis
was classified as an entity related to hemophilia (Greek term
meaning friendship for blood) (34), characterized by the suddenness of
appearance with various outbreak patterns, connected sometime with
the vicarious menstruation (35).
It was also closely related to the central nervous paralysis and
hysteria, to ecstasy, to agony, to convulsion (spasms), to
hallucinations and in general in neurology disorders, reported as a
rare symptom (36,37). According to the beliefs of the
epoch, blood pure, or mingled with sweat could appear on the
surface of the skin in the form of drops or issues from the
glandurar openings (pilo-sebaceous, Meibomian, ceruminous) in tiny
jets. Moreover, dermatorrhagia (bleeding from the sub-epidermic
vascular network) could occur simultaneously and the condition have
also been considered as a form of hyperhidrosis with fatal
symptomatology (weakness, anemia, syncope and death) (38).
The most prolific complete treatise on the subject
of hematidrosis was this of Ernst Ziegler in 1895, naming
hematidrosis as diapedesis. Diapedesis of the blood through
uninjured walls of vessels was considered as something peculiar and
a different form the hemorrhage produced by ruptured ones when a
rhexis (Greek term for rupture) occurs. This occasional spontaneous
oozing of arterial blood from the sweat glands was studied by
microscopy and was attributed to the rise of pressure in the
capillaries and small veins combined with increased permeability of
the vessel walls. As for the hemorrhagic diathesis (Greek term,
meaning temper), this had been divided into congenital or
hereditary and acquired. A large cluster of diseases could enact
the provocation of hematidrosis, named scurvy, morbus maculosus
Werlhof, purpura simples, purpura rheumatic, purpura haemorrhagica,
melena neonatorum, septicemia, endocarditis, malignant pustule,
spotted typhus, cholera, smallpox, plague, acute yellow atrophy of
the liver, yellow fever, nephritis, phosphorus poisoning,
snake-bites, malnutrition, irritation or paralysis of the
vaso-mottor nerves, moral shock, terror, thrombosis or embolism or
ligation of a vessel complicated with stagnation and many more. The
female sex was most vulnerable against diapedesis. Psycho-therapy
and palliative interventions were suggested (39). Geranium, a genus of 422 species of
plants, was proposed to help confront hematidrosis (40). The treatise of Ziegler was
published the same year with Moriz Kapozi's masterpiece Pathology
and Treatment of the Disease of the Skin. However, Kapozi only
mentioned the occasional spontaneous oozing of arterial blood from
the sweat glands, named hematidrosis, considering it as the rarest
case of cutaneous hemorrhage (41).
The terrifying nature of the hematidrosis phenomenon
impressed the mind of medical observers and conquered the souls of
the uneducated population to assume an almost miraculous character.
Diapedesis on the forehead, hands and feet was stated to occur in
religious bigots considered by fanatics as a gift of holy marks and
bloody sweat of the Christ named stigmata. Those cases, following
careful scientific examination, had proven to be, at least most of
them, in the sphere of religion and faith or somehow fictitious.
Religion enthusiasts bearing hematidrosis made their appearance
from time to time mostly in the area of the Catholic church,
stating the ability to reveal and confess the real work of God.
Even publications were encountered in the form of Letters (famous
type of text in religion). Hyperboles, such as for public
demonstrations of hysteric or cataleptic poor peasant girls being
visited by hundreds of wondering spectators ready to worship them
and references of persons that had not slept or eaten for 8 years,
compelled scientists to refer to them as simply impostors (14).
Charles T. Scott was the first to publish in PubMed
in 1918 under the term haematidrosis, reporting the case of
abnormal perspiration of a pink fluid on the forehead of an
11-year-old girl with a nervous temperament (42). Almost a century later, Joe E.
Holoubek and Alice B. Holoubek in 1916, two devoted catholic
physicians, performed an extensive literature review based upon a
selection of 76 cases of Pooley's review ranging from the 17th
century to 1980. They had classified all cases under subgroups
according to the etiology: Systemic disease (e.g., scurvy and
lupus), vicarious menstruation, physical exertion, psychological
stress (repeated or unique), religious stigmatics and idiopathy
(43). Moreover, 2 cases were
reported during 2022 in the PubMed/MedLine database (44,45).
5. Findings in the modern literature
Hematidrosis depicts an eccrine sweat disorder,
strongly characterized by one or more transient, yet recurring
episodes of a spontaneously mixed fluid of sweat and blood from the
intact epidermis. Although it presents a notoriously rare and
fascinating condition, the prevalence and incidence of this
condition remain unknown, as illustrated by the small number of
cases published and the almost complete absence of case series.
However, over the past two decades the number of cases and studies
has increased, despite the fact that most of the cases which have
been reviewed displayed a stereotypical presentation of bleeding
pattern, background etiogenesis and therapeutic approach (1,4).
Female patients presented the majority of the cases, mainly young
between the ages of 9 to 15 years (46-52).
Male patients have been less frequently reported, but are usually
also at a young age (53,54) with a small number of exceptions of
patients >65 years of age (55,56).
The geographic distribution testifies a tendency towards the Asian
region (India and Pakistan) as one of the two cases of those
reported refers to the Indian population. A genetic predisposition
was proposed to explain this geographic predilection (1,4).
The most common areas of appearance of the
phenomenon, without being limited to these, are namely the
forehead, scalp, face, eyes and ears, and secondary trunk and
limbs. The majority of the cases were clinically examined and
interdisciplinary observed by more than one specialized physician,
as in numerous reports, there were suspicions that the symptom may
be factitious (5). Moreover, in
some reports, the diagnosis was based only on clinical criteria
with insufficient laboratory examinations, accompanied by a
misdiagnosed hypothesis of self-traumatism. However, fully
clinically examined patients, undergoing histopathological
examinations, is the trend observed over the past decade (57). Psychiatric disorders and severe
stress have been proposed (1,58-60),
while a post-traumatic appearance has been reported by 61. Yeşilova
et al (61) and Mejer
(62). Various areas of appearance
may be noted in a multiple concurrent emergence. Οtorrhea,
hematuria, epistaxis, bleeding from the intestines the oral cavity
and the eyelids have also been mentioned (1,41,59,60,63).
Pathology usually reveals a free medical history, and records have
demonstrated no family incidents; laboratory tests of complete
blood count, coagulation, immunology, renal and liver function have
yielded inconclusive results (60). Dermatological evaluation have
disclosed no cutaneous lesions. Histological findings following
skin biopsy have ranged from congested blood vessel capillaries,
extravasation of erythrocytes within the follicular lumen, leakage
of red blood cells in dermis, or even just normal skin layers
(1,2,43).
In a case where an increased number of CD34-positive cells were
observed around the eccrine sweat glands in a young female with
palmar hematidrosis, the authors suggested that high pressure
applied in the plantar surface of the hand (horizontal bar
exercise) subsequently damaged the balance of her small blood
cells, thus increasing the CD34-positive cells (64). As regards diagnosis, the following
criteria have been suggested: i) testified bleeding by medical
personnel; ii) red blood cell detection in the examination
exudates; iii) the absence of trauma, self-injury, telangiectasias,
purpura and no evidence of oozing after wiping of the area
(65). Differential diagnosis
included self-injury, vasculitis, connective tissue disorders
(increased vascular fragility and secondary bleeding), Munchausen's
by proxy syndrome, scurvy, hematomas, petechial, purpuric lesions,
pseudochromhidrosis, and chromhidrosis and psychogenic purpura
(5,62,66).
To avoid confusion, it must be noted that chromhidrosis is
characterized by the excretion of colored sweat from eccrine sweat
glands, while pseudochromhidrosis sweat is colorless, later
acquiring color due to its contact with chromogenic chemicals of
the skin (66,67).
The patho-physiolgical mechanisms involved in the
development of hematidrosis are not completely clarified. It has
been calculated that half of the cases of hematidrosis remained
with an undetermined causative etiology. The rupture of the small
capillaries that supply sweat glands has been suggested to be the
key factor of blood seepage (1).
Physical fatigue and emotional stress, fear of death, school
examinations, interfamily conflict and orphanage are being
indicated as the most frequent triggers of this condition (1,68).
Tonic seizures resolved with anti-epileptic medication may cause
hematidrosis, as recorded in a 9-year-old girl by Shen et al
(69) in 2015. It has been
hypothesized that the hyper-reactivity of the sympathetic nervous
system following a major or acute stressful event, may result in
vessel vasoconstriction, altering the blood supply to the eccrine
glands. In the post-stress phase as vasodilatation occurs, tinny
ruptures of the nutritional vessels of the sweat glands occur and
the secretion of bloody sweat droplets to the skin is implemented.
A distinctive vasculitis with intra-dermal bleeding and obstructed
capillaries has also been reported as the pathological basis of
hematidrosis cases (70,71). Platelet factor-3 dysfunction has
been also implicated (72).
Currently, there is no available treatment of
choice. The benign and transient nature of the disease should be
explained to the family and caregivers. Convincing the parents
about the nature of the disease is mandatory for the successful
management of any case. Moreover, holistic emotional support of all
implicated appears to be of paramount importance (72-76).
Personalized therapy and individualized interventions based on the
needs of patients and caregivers are strongly recommended. The
reduction of anxiety followed by the administration of
benzodiazepines, such as lorazepam and diazepam has been proven
efficacious (1,60). Hemostatic drugs and vitamin C are
being used without any notable results. Some cases have responded
to atropine transdermal patches (77), while others to adrenaline gauze
wipes (73,75). The administration of β-adrenoceptor
antagonists has been reported to be an effective treatment for
hematidrosis by regulating sympathetic nervous system activation
and reducing intense psychological excitement (4,47,78-80).
Wang et al (59) in 2010
reported a complete resolution and recovery of the bleeding
episodes in a 13-year old girl treated with propranolol.
Oxybutynin, an anticholinergic drug, was successfully used in a
13-year-old patient (81). There
are cases reporting that apart from medical personnel, patients
were searching for various spiritual treatments, homeopathy and
quackery (personas who fraudulently sell a product or service to
supposedly cure a patient) (82).
6. Summary and deliberation of
hematidrosis
Diapedesis from the plexus of the vessels
surrounding the sweat glands has intrigued scholars and scientists;
this has led to the appearance of records in medical and historical
books. Shallow skepticism of the medical community denied the
phenomenon for centuries, until only when it was directly observed.
Apart from plausibility, failure to evolve a comprehensive
explanation contributed further to its delayed acceptance.
Disbelief strengthened by the fact that recorded cases were being
described sporadically and in a number of cases, by completely
unrelated authors (83).
A plethora of studies refer to Aristotle as the
first to describe hematidrosis. That is not entirely accurate.
Aristotle in his work ‘On the Parts of Animals’, truly described
bloody sweat, but as a peculiarity observed in the animal kingdom,
but not in humans. He only noted that it is known to exist. Some
animals exude reddish fluids from the surface of the skin. This
blood-colored exudation is due to color globules, and not merely to
blood in the case of the hippopotamus. Flamingos secrete red fluids
by their stomachs (84). The
observation of domestic animals, horses and cattle reveals more
representations of livestock manifesting incidents of real bloody
sweat (85). There is also some
confusion as regards the referrak to Galen as the pioneer to
understand hematidrosis. There was an old treatise titled ‘De
utilitate respiration’ bearing the same name given by Galen to one
of his works. It was paraphrased by the physician, Richard Mead, in
his 1749 publication on the bloody sweat of Jesus Christ. Since
then, it was globally celebrated as a true work of Galen's
Collection. Nevertheless, the remark was noted by some other
scholars who wanted to draw additional attention by falsifying the
name of the Greek majesty. Nevertheless, references for bloody
sweat exist only in the pseudogalenic texts (43). To verify this fact, the authors
analyzed and made a translation of 3,054 of Galens' references to
blood (αίµα) and 78 to sweat (ιδρώτας) by accessing TLG, resulting
in no possible much for such a case.
The Latin terms, sudor cruentus and sudor
sanguineus, first appeared in 18th century medical dictionaries and
indexes of the era. Hellenic-derived spellings of h[a]e
[o]mat[oh/h]idrosis appeared at a later date, during 1854(43). Apart from the name of the disease,
hematidrosis itself, various terms of Hellenic origin are connected
to its pathology, such as H[a]emorrhage (blood outflow), hemolacria
(blood in tears), otorrhea (outflow from the ears), otorrhagia
(blood outflow from the ears) and epistaxis (blood drip from the
nose) (86,87). Terminology only implies for an
emotive entity in skin pathology. Otorrhagia appears in more
articles in PubMed Central than hematidrosis. Authors worldwide
have only heard about rare bleeding disorders, and yet, they
believe their existence. However, this is not valid concerning
cases of hematidrosis, as for many, it depicts a rather
controversial theme. This, raises the question of who to choose for
reader or reviewer for such an article (88). Cases such as the one reported by
Hoover et al (89), of two
siblings presenting hematidrosis, apart from witnessing genetic
predisposition, further complicates emotions and beliefs.
In both eras investigated, during the 15th-19th
century and the past 20 years, the female sex has been registered
as the dominant inside scientific texts. However, the numbers of
reported cases prior to 1900 are markedly lower when comparing with
those reported over the past two decades. Masculine restrictions,
deficiency in physical strength and limitations to intellectual
developmental activities had undermined the education and
intelligence of the female sex and particularly that of younger
females of the humbler social casts (90). In many cases, young girls
presenting hematidrosis were peregrinated for religion and profit
reasons being considered as stigmatics gathering pilgrims and coin.
Although a bleeding episode of a young girl may cause
embarrassment, social isolation, panic and depression, the majority
of those girls never attended a physician or registered as an
official case (14). This fact may
also explain the following: i) The difference in mean age, which
was 25.6 years until 1990 and 15.8 years over the past two decades,
when presumably all cases were examined by health professionals;
and ii) the female sex percentage recorded until 1900 was 39.4%,
while that over the past two decades increased into 74.4%. The
analogy report of the anatomical areas of bloody sweat oozing
through the skin demonstrates that in both eras, the scalp,
forehead, face, arms, trunk and feet are the most commonly recorded
regions, while the ears, eyes and mouth demonstrated considerably
higher numbers in later years. The time period of the past 15 years
presents the highest peak of all time concerning papers on
hematidrosis, with the second half of the 19th century to follow
(5,43). The second industrial revolution
marked the second half of the 19th century, provoking acute social
changes, while nowadays, the excessive and harmful use of
technology, such as cell phones, video games, personal computers,
the internet and in general, the modern way of life, greatly
aggravate psychological side-effects such as anxiety, stress and
depression, while the youth are often associated with emotional and
behavioral issues. Increased psychic disorders increase all
diseases associated, perhaps explaining the increase in the
incidence of hematidrosis (91,92).
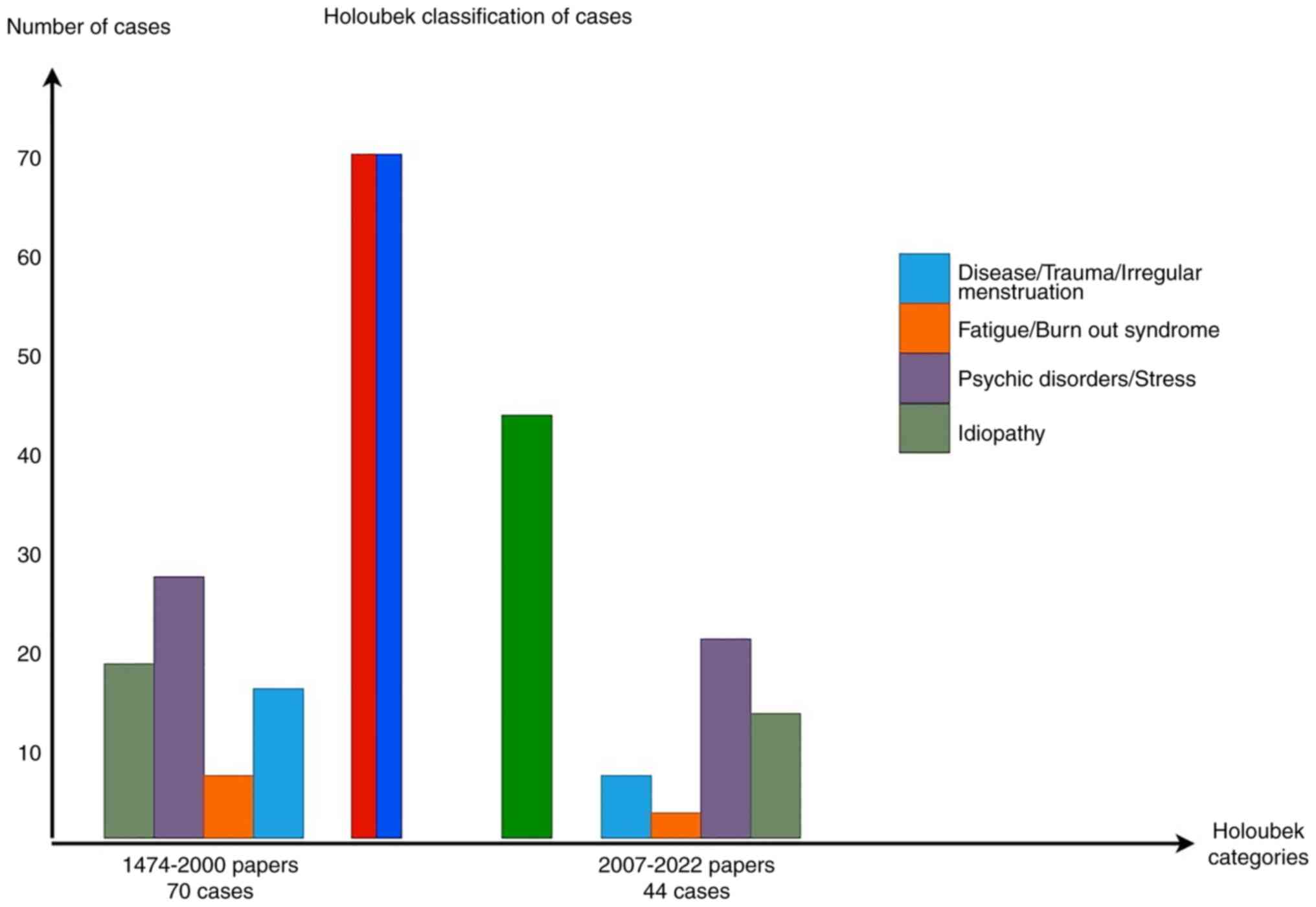
Articles categorized according to the classification of
hematidrosis by Holoubek and Holoubek (43) are demonstrated in Fig. 2, where psychotic
disorders/stressful events constitute the main trigger factor in
both eras. With the exception of the case described by Dr Hehir in
India, all other references until 1900 were reported from areas of
the European continent, while in the modern literature, the
majority of cases are recorded in India, or in Asia. The geographic
limitation of reports from Europe may be explained by the medical
achievements and progress mainly due to Western European
intellectual evolution through the ages, rendering this region as
the major point of quotation (93). English works until 1900 comprised
45.3%, while this number increased to 80.4% over the past two 2
decades. To support geography and language results, English was
cited as a universal language and globalization of the medical
references.
Jesus Christ when reacting to his future and known
to him torturous death, he had experienced a passionate agony, an
intensified stressful juncture of emphatic emotions, which flared
up as epistaxis. A number of medical writers still insist that
blood fell to the ground. Richard Mead in his 1749 work was the
first to notice and record that actually it was thromboi (clots of
blood) which touched the earth. The reddish fluid was thick and
viscous and rapidly coagulated (94,95).
The Hellenic term stigma was used to reproduce the optical
portraiture of the agony bleeding, crucifixion nails, thorny crown,
vinegar sponge, lash and spear wounds, which had been inflicted to
the palms, soles, head, chest, lips and back of Christ. Stigma in
Greek antiquity indicated a bloody wound or a sign marked on a
slave, while during the cultural spread of Christianity, it
acquired a more mystical meaning. Nuns, priests, saints, common
frauds and deep believers all experienced among other painful
effects, hematidrosis. Stigmata have never been studied under the
prism of a medical scientific approach until the review by
Kechichian et al (96) in
2018. A cluster of symptoms received by God is reported, including
painful purpura, erosions, blisters, scars and bleeding through the
epidermis with intact skin layers. Hematidrosis, the symptom of
interest, presents an obvious interaction between skin and psyche.
In a state of ecstasy, a pure believer may endure the agony felt by
his God, triggering the over-activation of the sympathetic nervous
system. An acute induce of a sympathetic response of the autonomic
nervous system may be held responsible for the vascular mechanisms
behind hematidrosis (96).
Although the conscious and voluntary fabrication or exaggeration of
physical and psychological symptoms for personal gain of frauds do
exist, physicians must have in mind the case of an almost ‘pure in
life’ true believer who may experience in the reality of his mind,
the passion of the Christ and in some cases, being canonized.
Hematidrosis is a condition which remains one of gruesome
fascination, but of great psychological suffering for the victim.
Neurology, psychiatry, dermatology, angiology and religion must
interact to explain some aspects (96-100).
7. Conclusions
Throughout the ages, a rarity in daily practice, a
sporadic reference in textbooks, an enigma in medicine, a malady
that may lead to extensive unnecessary laboratory tests and to
hazardous therapeutic interventions, hematidrosis is a spectacular
manifestation in skin pathology. It depicts a field where science,
the unknown and religion intertwine. The derma, psyche and faith
create a triad to explain diapedesis. For some medical personnel,
the condition appears to be an inconceivable phenomenon. For others
it is merely an ailment. For the Catholic church, hematidrosis in
stigmata constitutes an almost divine phenomenon. As medicine
without religion is a science disabled, to paraphrase the words of
Einstein, the present review highlights the pathology and
illustrates the necessity to believe in both, in order to
comprehend the peculiarities of nature. Nevertheless, blurred
etiopathogenesis, transdiagnostic variables, interdisciplinary
teams of health professionals, symptomatic and inconclusive therapy
and blood cells mixed with sweat are the only data that may be
presumed as certain.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
GT, DA and ES were involved in the intellectual
content of the review. GT, DA, AK and NP were involved in the
literature search. GT, DA and ES were involved in the acquisition
of data from the literature. GT, ES and KK were involved in the
analysis from the literature for inclusion in the review. GT and ES
were involved in the preparation and editing of the manuscript. ES,
KK and DAS were involved in the reviewing of the manuscript. All
authors have read and approved the final manuscript. Data
authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Kluger N: Hematidrosis (bloody sweat): A
review of the recent literature (1996-2016). Acta Dermatovenerol
Alp Pannonica Adriat. 27:85–90. 2018.PubMed/NCBI
|
|
2
|
Manonukul J, Wisuthsarewong W, Chantorn R,
Vongirad A and Omeapinyan P: Hematidrosis: A pathologic process or
stigmata. A case report with comprehensive histopathologic and
immunoperoxidase studies. Am J Dermatopathol. 30:135–139.
2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Whitney DW (ed): The Century Dictionary
and Cyclopedia. The Century Co., New York, NY, 1889.
|
|
4
|
Alsermani M, Alzahrani H and El Fakih R:
Hematidrosis: A fascinating phenomenon-case study and overview of
the literature. Semin Thromb Hemost. 44:293–295. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Duffin J: Sweating blood: History and
review. CMAJ. 189:E1315–E1317. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 29(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Aristotle: Animal History [Historia
animalium, ed. P. Louis, Aristote. Histoire des animaux], vols.
1-3. Les Belles Lettres, Paris, 1:1964; 2:1968; 3:1969: 1:1-157;
2:1-155; 3:1-145, 156-175. Lib. 1-4 (486a5-538b23): vol. 1. Lib.
5-7 (538b28-588a12): vol. 2. Lib. 8-10 (588a16-633b8,
633b12-638b36): vol. 3, 1876.
|
|
8
|
Louis P (ed): Aristotle: On the Animal
Parts [De partibus animalium. Les parties des animaux]. Les Belles
Lettres, Paris, pp1-166, 1956.
|
|
9
|
Wimmer F (ed): Theophrastus Phil:
Fragments [Fragmenta, Theophrasti Eresii opera, quae supersunt,
omnia]. Didot, Paris, pp364-410, pp417-462, 1866.
|
|
10
|
Diodorus Siculus: Library [Bibliotheca
Historica]. Georgiadis, Athens, 2010.
|
|
11
|
Kühn CG (ed): Pseudo-Galenus: Works [De
utilitate respiration & De humoribus liber]. Vol 19. Knobloch,
Liepzig, pp485-496, 1830.
|
|
12
|
Marcus Annaeus Lucanus: Pharsalia [M.
Annaei Lucani Pharsalia]. Bell, London, p348, 1827.
|
|
13
|
Luce: The Gospel of Luce by Howard
Marshall. Wm. B. Eerdmans Publishing, Grand Rabids, 1978.
|
|
14
|
Pooley JH: Bloody Sweat. The Popular
Science Monthly, Appleton and Company, New York, NY, 1885.
|
|
15
|
Millingen JG: Curiosities of Medical
Experience Revised and Considerably Augmented. Richard Bentley,
London, 1839.
|
|
16
|
Gray CJ: The Biblical Museum. Elliot
Stock, London, 1871.
|
|
17
|
Parrot J: Study on blood sweat and
neuropathic hemorrhages [Étude sur la sueur de sang et les
hémorrhagies névro-pathiqués]. Bulletin De l'Enseignement Médicale,
pp633-635, 1859.
|
|
18
|
Hart WP: On Bloody Sweat. The London
Medical Record: A Review of the Progress of Medicine, Surgery,
Obstetrics and the Allied Sciences. Smith, London, 1875.
|
|
19
|
Moore J: Index-catalogue of the library of
the surgeon-general's office. United States Army. U.S. Government
Printing Office, Washington, DC, 1889.
|
|
20
|
Banberger H, Foerster A and von Scanzoni
F: Stahel's book and art negotiation [Wurzburger Medichinische
Zeitschrift]. Stahelschen Buch und Kunstverhandlung, Wurzburg,
1864.
|
|
21
|
Casper JL: Weekly Medical Magazine,
Editorial [Wochenschrift fur die gesammte Heilkunde]. August
Hirschwald, Berlin, 1848.
|
|
22
|
Hoffmann FA: Textbook of Constitutional
Diseases [Lehrbuch der Constitutionkrankheiten]. Von Ferdinand
Enke, Stuttgart, 1893.
|
|
23
|
Von Franque O and Geigel A:
Medical-Surgical Monas Booklets [Medicinisch-chirurgische
Monashefte]. Kritisches Sammeljournal fur praktische Heilkunde. Von
Ferdinand Enke, Jahrgang, 1863.
|
|
24
|
Spörlin G: Letter [1627], in Wilhelm
Fabricius Hildanus. In: Works [Opera quæ extant omni]. Johannis
Beyeri, Frankfurt, p601, 1646.
|
|
25
|
Ledelius S: Library of the Medical
Treasure of Practice [Bibliotheca medico-practica sive rerum
medicinarum thesaurus etc.]. Manget JJ (ed). Vol 4. Chouet and
Ritter, Geneva, p592, 1697.
|
|
26
|
Dyer I: A Case of Hematidrosis Combined
with Chromidrosis. The Medical News, Brighton, pp702-703, 1895.
|
|
27
|
Wood JC: A text-book of gynecology.
Boericke and Tafel, Philadelphia, 1894.
|
|
28
|
Virchow RLC: Professor Virchow on Louise
Lateau. The Medical Times and Gazette: A Journal of Medical
Science, Literature, Criticism, and News, p507, 1874.
|
|
29
|
Tittel M: A Case of Hematidrosis. The
Medical Record: A Monthly Journal of Medicine and Surgery, p142,
1876.
|
|
30
|
Chambers TK: A case of bloody sweat.
Lancet. 1:205–209. 1861.
|
|
31
|
Servaes F: About blood sweating on the
head in Dementia paralytica [Ueber Blutschwitzen am Kopfe de
Dementia paralytica]. Centralblatt fur die Medicinischen
Wissenschaften. August Hirschwald, Berlin, 1863.
|
|
32
|
Westphal A: Bloody Sweat [De Sudore
Sanguineo] (Baldinger sylloge t. II). Gryphisw, 1775.
|
|
33
|
Fabre A: Pathogenesis of the
Neuro-Diseases [Les relations pathogéniques des troubles nerveux].
Delahaye, Paris, 1880.
|
|
34
|
Nevis Hyde J: A Practical Treatise On the
Diseases of the Skin. Leo Brothers, Philadelphia, PA, 1893.
|
|
35
|
Anderson M: Lectures on Clinical Medicine.
MacMillan and Co, London, 1877.
|
|
36
|
Berheim S and Laurent E: Practical
Treatise on Clinical and Therapeutic Medicine [Traité Pratique de
Médecine Clinique et Thérapeudique]. Maloine, Paris, 1895.
|
|
37
|
Dechambre A: Encyclopedic Dictionary of
Medical Sciences [Dictionnaire Encyclopédique des Sciences
Médicales]. Asselin & Masson, Paris, 1871.
|
|
38
|
Van Harlingen A: Haematidrosis (Bloody
Sweat). International clinics volume II. Lippincott, Philadelphia,
PA, 1896.
|
|
39
|
Ziegler E: General pathology, The science
of the causes, nature and course of the pathological disturbances
which occur in the living subject. W. Wood and Company, New York,
NY, 1895.
|
|
40
|
Shoemaker JV: Geranium Maculatum in Nelson
E.M. Saint Louis Courier of Medicine Volume XIX. Chambers,
Mississippi, MS, 1888.
|
|
41
|
Kapozi M: Pathology and Treatment of
Diseases of the Skin. W. Wood & Company, New York, NY,
1895.
|
|
42
|
Scott CT: A case of Haematidrosis. Br Med
J. 2993:532–533. 1918.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Holoubek JE and Holoubek AB: Blood, sweat
and fear. A classification of hematidrosis. J Med. 27:115–133.
1996.PubMed/NCBI
|
|
44
|
Zheng J, Bian MR, Wu XQ, Xiao Y, Chen YH,
Shen R, Feng C and Gao KB: Hematidrosis: A case report. Dermatol
Ther. 35(e15462)2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Alasfoor S, Albashari M, Alsermani A,
Bakir M, Alsermani M and Almustanyir S: A strange occurrence of
hematohidrosis: A case report from Saudi Arabia. Cureus.
14(e21682)2022.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Bhattacharya S, Das MK, Sarkar S and De A:
Hematidrosis. Indian Pediatr. 50:703–704. 2013.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Shafique DA, Hickman AW, Thorne A, Elwood
HR and Zlotoff BJ: Pediatric hematidrosis-A case report and review
of the literature and pathogenesis. Pediatr Dermatol. 38:994–1003.
2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Mora E and Lucas J: Hematidrosis: Blood
sweat. Blood. 121(1493)2013.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Carvalho AC, Machado-Pinto J, Nogueira GC,
Almeida LM and Nunes MB: Hematidrosis: A case report and review of
the literature. Int J Dermatol. 47:1058–1059. 2008.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Praveen BK and Vincent J: Hematidrosis and
hemolacria: A case report. Indian J Pediatr. 79:109–111.
2012.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Bhagwat PV, Tophakhane RS, Rathod RM,
Shashikumar BM and Naidu V: Hematohidrosis. Indian J Dermatol
Venereol Leprol. 75:317–318. 2009.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Varalakshmi B, Doshi VV, Sivalingam D and
Nambi S: The story of a girl with weeping blood: Childhood
depression with a rare presentation. Indian J Psychiatry. 57:88–90.
2015.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Talwar M, Chidambaram AC, Mekala S,
Parameswaran N and Delhikumar CG: Haematohidrosis in a 12-year-old
boy: Blood, sweat and tears. Paediatr Int Child Health. 41:300–302.
2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Hansson K, Johansson EK, Albåge M and
Ballardini N: Paediatric haematohidrosis: An overview of a rare but
clinically distinct condition. Acta Paediatr. 108:1023–1027.
2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Antunes AS, Peixe B and Guerreiro H:
Hematidrosis, hemolacria, and gastrointestinal bleeding. GE Port J
Gastroenterol. 24:301–304. 2017.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Jerajani HR, Jaju B, Phiske MM and Lade N:
Hematohidrosis-a rare clinical phenomenon. Indian J Dermatol.
54:290–292. 2009.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Techasatian L, Waraasawapati S,
Jetsrisuparb C and Jetsrisuparb A: Hematidrosis: A report with
histological and biochemical documents. Int J Dermatol. 55:916–918.
2016.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Shahgholi E: A case series of
hematohidrosis: A puzzling medical phenomenon. Turk J Pediatr.
60:757–761. 2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Wang Z, Yu Z, Su J, Cao L, Zhao X, Bai X,
Zhan S, Wu T, Jin L, Zhou P and Ruan C: A case of hematidrosis
successfully treated with propranolol. Am J Clin Dermatol.
11:440–443. 2010.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Jafar A and Ahmad A: Child who presented
with facial hematohidrosis compared with published cases. Case Rep
Dermatol Med. 2016(5095781)2016.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Yeşilova Y, Turan E and Aksoy M:
Hematidrosis on the forehead following trauma: A case report. Int J
Dermatol. 56:212–214. 2017.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Meyer J, Spacil K, Stehr M, Hinrichs W,
Haller S and Schäfer FM: Hematidrosis after head injury-a case
report. Klin Padiatr. 231:326–327. 2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Tshifularo M: Blood otorrhea: Blood
stained sweaty ear discharges: Hematohidrosis; four case series
(2001-2013). Am J Otolaryngol. 35:271–273. 2014.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Murota H, Kotobuki Y, Yamaga K and
Yoshioka Y: Female child with hematidrosis of the palm: Case report
and published work review. J Dermatol. 47:166–168. 2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Maglie R and Caproni M: A case of blood
sweating: Hematohidrosis syndrome. CMAJ. 189(E1314)2017.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Barankin B, Alanen K, Ting PT and
Sapijaszko MJA: Bilateral facial apocrine chromhidrosis. J Drugs
Dermatol. 3:184–186. 2004.PubMed/NCBI
|
|
67
|
Nair PA, Kota RKS, Surti NK, Diwan NG and
Gandhi SS: Yellow pseudochromhidrosis in a young female. Indian
Dermatol Online J. 8:42–44. 2017.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Jayaraman AR, Kannan P and Jayanthini V:
An interesting case report of hematohidrosis. Indian J Psychol Med.
39:83–85. 2017.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Shen H, Wang Z, Wu T, Wang J, Ren C, Chen
H, Yu Z and Don W: Haematidrosis associated with epilepsy in a girl
successfully treated with oxcarbazepine: Case report. J Int Med
Res. 43:263–269. 2015.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Uber M, Robl R, Abagge KT, Carvalho VO,
Ehlke PP, Antoniuk SA and Werner B: Hematohidrosis: Insights in the
pathophysiology. Int J Dermatol. 54:e542–e543. 2015.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Zhang FK, Zheng YL, Liu JH, Chen HS, Liu
SH, Xu MQ, Nie N and Hao YS: Clinical and laboratory study of a
case of hematidrosis. Zhonghua Xue Ye Xue Za Zhi. 25:147–150.
2004.PubMed/NCBI(In Chinese).
|
|
72
|
Mishra KL: Bloody tears and hematohidrosis
in a patient of PF3 dysfunction: A case report. Cases J.
2(9029)2009.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Pari T: Hematohidrosis-A rare case. Indian
Dermatol Online J. 10:334–335. 2019.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Patel RM and Mahajan S: Hematohidrosis: A
rare clinical entity. Indian Dermatol Online J. 1:30–32.
2010.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Favaloro EJ and Lippi G: Commentary:
Controversies in thrombosis and hemostasis part 1-hematidrosis:
‘Blood, Sweat and Fears’ or A ‘Pigment of fertile imaginations?’.
Semin Thromb Hemost. 44:296–297. 2018.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Deshpande M, Indla V, Kumar V and Reddy
IR: Child who presented with hematohidrosis (sweating blood) with
oppositional defiant disorder. Indian J Psychiatry. 56:289–291.
2014.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Biswas S, Surana T, De A and Nag F: A
curious case of sweating blood. Indian J Dermatol. 58:478–480.
2013.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Das D, Kumari P, Poddar A and Laha T:
Bleeding to life: A case series of hematohidrosis and hemolacria.
Indian J Pediatr. 87(84)2020.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Ricci F, Oranges T, Novembre E, Della Bona
ML, la Marca G, de Martino M and Filippi L: Haematohidrosis treated
with propranolol: A case report. Arch Dis Child.
104(171)2019.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Matsuoka R and Tanaka M: Hematidrosis in a
Japanese girl: Treatment with propranolol and psychotherapy.
Pediatr Int. 62:1001–1002. 2020.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Tirthani K, Sardana K and Mathachan SR:
Hematohidrosis of the mid-face and hands treated with oral
oxybutynin. Pediatr Dermatol. 38:962–963. 2021.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Khalid SR, Maqbool S, Raza N, Mukhtar T,
Ikram A and Qureshi S: Ghost spell or hematohidrosis. J Coll
Physicians Surg Pak. 23:293–294. 2013.PubMed/NCBI
|
|
83
|
Buck AH: A Reference Handbook of the
Medical Sciences Embracing the Entire Range of Scientific and
Allied Sciences. Vol 3. Wood and Company, New York, NY, 1886.
|
|
84
|
Wilks S: Hematidrosis or Bloody Sweat
Complicating Tetanus in Guy's Hospital Reports. Samuel Highley,
London, 1872.
|
|
85
|
Kral F and Novak BJ: Veterinary
Dermatology. Lippincott, Philadelphia, PA, 1953.
|
|
86
|
Liddel Η and Scott R: Grand Lexicon of the
Hellenic Language. Konstantinides, Athens, 1904.
|
|
87
|
Babiniotis G: Lexicon of the New Hellenic
Language, 2nd edition. Lexicology Center, Athens, 2002.
|
|
88
|
Favaloro EJ and Lippi G: Commentary:
Controversies in thrombosis and hemostasis part 1-hematidrosis:
Blood, sweat and fears or a pigment of fertile imaginations? Semin
Thromb Hemost. 44:296–297. 2018.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Hoover A, Fustino N, Sparks AO and Rokes
C: Sweating blood: A case series of 2 siblings with hematohidrosis.
J Pediatr Hematol Oncol. 43:70–72. 2021.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Milne JD: Industrial and Social Position
of Women in the Middle and Lower Ranks. Chapman and Hall, London,
1857.
|
|
91
|
Hou CY, Rutherford R, Chang H, Chang FC,
Shumei L, Chiu CH, Chen PH, Chiang JT, Miao NF, Chuang HY and Tseng
CC: Children's mobile-gaming preferences, online risks, and mental
health. PLoS One. 17(e0278290)2021.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Hashemi S, Ghazanfari F, Ebrahimzadeh F,
Ghavi S and Badrizadeh A: Investigate the relationship between
cell-phone over-use scale with depression, anxiety and stress among
university students. BMC Psychiatry. 22(755)2022.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Conrad LI, Neve M, Nutton V, Porter R and
Wear A: The Western Medical Tradition: 800 BC to AD 1800. Cambridge
University Press, Cambridge, 1995.
|
|
94
|
Valpy E: The new testament with english
notes, critical, philological and explanatory. Vol 3. 4th edition.
Longman, Baldwin, Whittaker, Rivington and Simpkin, London,
1836.
|
|
95
|
Hesychius: Hesychii Alexandrini Lexicon.
Sumptibus Frederici Maukii, Ienae, 1868.
|
|
96
|
Kechichian E, Khoury E, Richa S and Tomb
R: Religious stigmata: A dermato-psychiatric approach and
differential diagnosis. Int J Dermatol. 57:885–893. 2018.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Del Forno C: Stigmata: From Saint Francis
of Assisi to idiopathic. Ann Dermatol Venereol. 141:529–530.
2014.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
98
|
Pilato MM: The memoirs of Dr. Michael
Arthur Creed. Xlibris Corporation, 2010.
|
|
99
|
Jestice PG: Holy People of the World: A
Cross-Cultural Encyclopedia. ABC-CLIO, Santa Barbara & Denver
& Oxford, 2004.
|
|
100
|
Von Gorres JJ: The Stigmata a History of
Various Cases. Richardson, London, 1883.
|