Introduction
Superior mesenteric artery embolism (SMAE) is a
disease that is caused by the obstruction of the superior
mesenteric artery (SMA) due to the entry of emboli. The diameter of
the SMA varies among individuals and typically ranges 0.5-1.0 cm
(1). The SMA frequently has an
acute angle, where it originates from the abdominal aorta. This
anatomical feature makes blood flow into the SMA prone to eddies
and turbulence, which can increase the risk of emboli entering and
blocking blood vessels (2,3). Therefore, SMAE is common in clinical
practice and is present in 40-50% acute mesenteric vascular
ischemia cases (4). Emboli
typically originate from wall-attached thrombi in the heart.
Therefore, they are more common in patients with rheumatic heart
disease, coronary heart disease, infective endocarditis and recent
myocardial infarction (5). In
addition, this disease has both an insidious onset and rapid
development, which can cause extensive necrosis of the small
intestine and right hemicolon within a short period of time. Its
mortality rate can reach up to 90% (6). However, even with surgical
intervention, the mortality rate remains as high as 70%; the main
reasons include the following two aspects: First, SMAE can cause
extensive intestinal necrosis and even after surgery to remove a
large number of necrotic intestinal tubes, patients may face
serious problems such as infection and short bowel syndrome,
increasing the risk of mortality; second, following surgery,
patients may experience complications such as reperfusion injury,
anastomotic leakage and abdominal infection, which can also
threaten their lives (7). It is
difficult to diagnose this disease and specific clinical symptoms
are lacking (8). The patient in
this case was admitted due to acute abdominal pain and the clinical
manifestations lacked specificity. Laboratory tests only showed
elevated white blood cell count and D-dimer levels. SMAE is similar
to other acute abdominal diseases, including gastrointestinal
perforation, acute appendicitis and acute pancreatitis, with a
misdiagnosis rate of up to 75-90% (9). Therefore, rapid diagnosis and timely
intervention are crucial for lowering its mortality rate. The
present case report detailed the diagnosis and treatment processes
of a patient with SMAE, who recovered well following timely and
effective intervention.
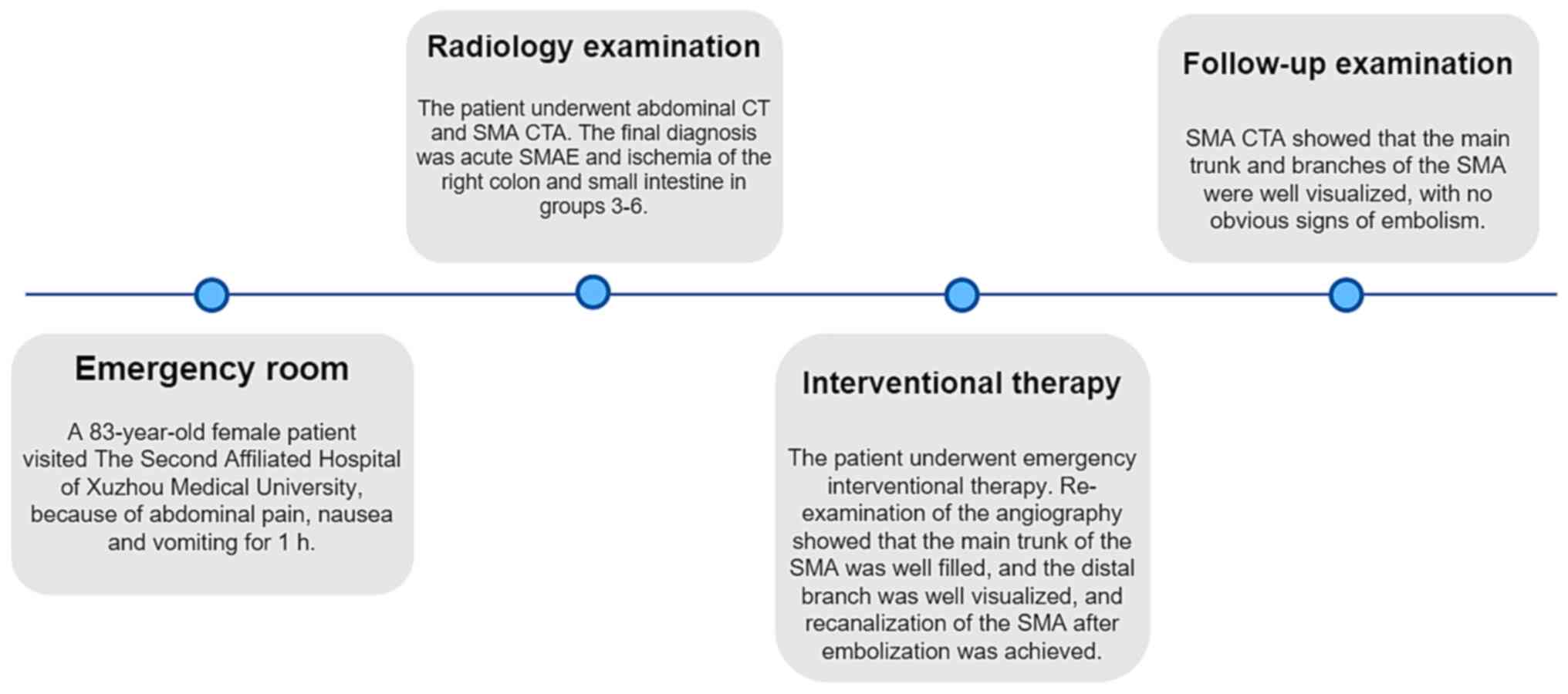
Case report
A female patient aged 83 years was admitted to The
Second Affiliated Hospital of Xuzhou Medical University (Jiangsu,
China) in September 2023 as a result of abdominal pain, nausea and
vomiting for 1 h. The health condition of the patient was poor. The
patient had a history of hypertension for >20 years and received
self-administer antihypertensive medication that was prescribed by
a doctor (Valsartan, 80 mg, s.i.d, taken orally), but had poor
blood pressure level control. The patient also had a history of
type 2 diabetes for >20 years and received self-administer
hypoglycemic medication that was prescribed by a doctor (Metformin
Hydrochloride Tablets, 0.5 g, b.i.d, taken orally), but had poor
blood glucose level control. In addition, the patient had a history
of coronary heart disease and atrial fibrillation for >10
years.
A physical examination of the patient showed the
following: i) Body temperature, 36.5˚C; ii) pulse, 113 beats/min;
iii) respiration, 24 breaths/min; iv) blood pressure, 149/72 mmHg;
v) slow response; vi) apparent distress; and vii) passive body
posture.
Laboratory test results showed the following: i)
white blood cell count, 12.56x109/l (reference range,
4-10); ii) D-dimer, 738 ng/ml (reference range, 0-500); iii)
platelet count, 162x109/l (reference range, 100-300);
iv) aspartate aminotransferase, 21 U/l (reference range, 7-50); v)
alanine transaminase, 15 U/l (reference range, 0-50); vi) lactate
dehydrogenase, 176 U/l (reference range, 109-245); vii) creatinine,
71 µmol/l (reference range, 40-110); viii) urea nitrogen, 5.4
mmol/l (reference range, 1.7-8.3); ix) blood amylase, 37 U/l
(reference range, 28-100); and x) urine amylase, 102 U/l (reference
range, 0-500). An electrocardiogram demonstrated fast ventricular
rate atrial fibrillation.
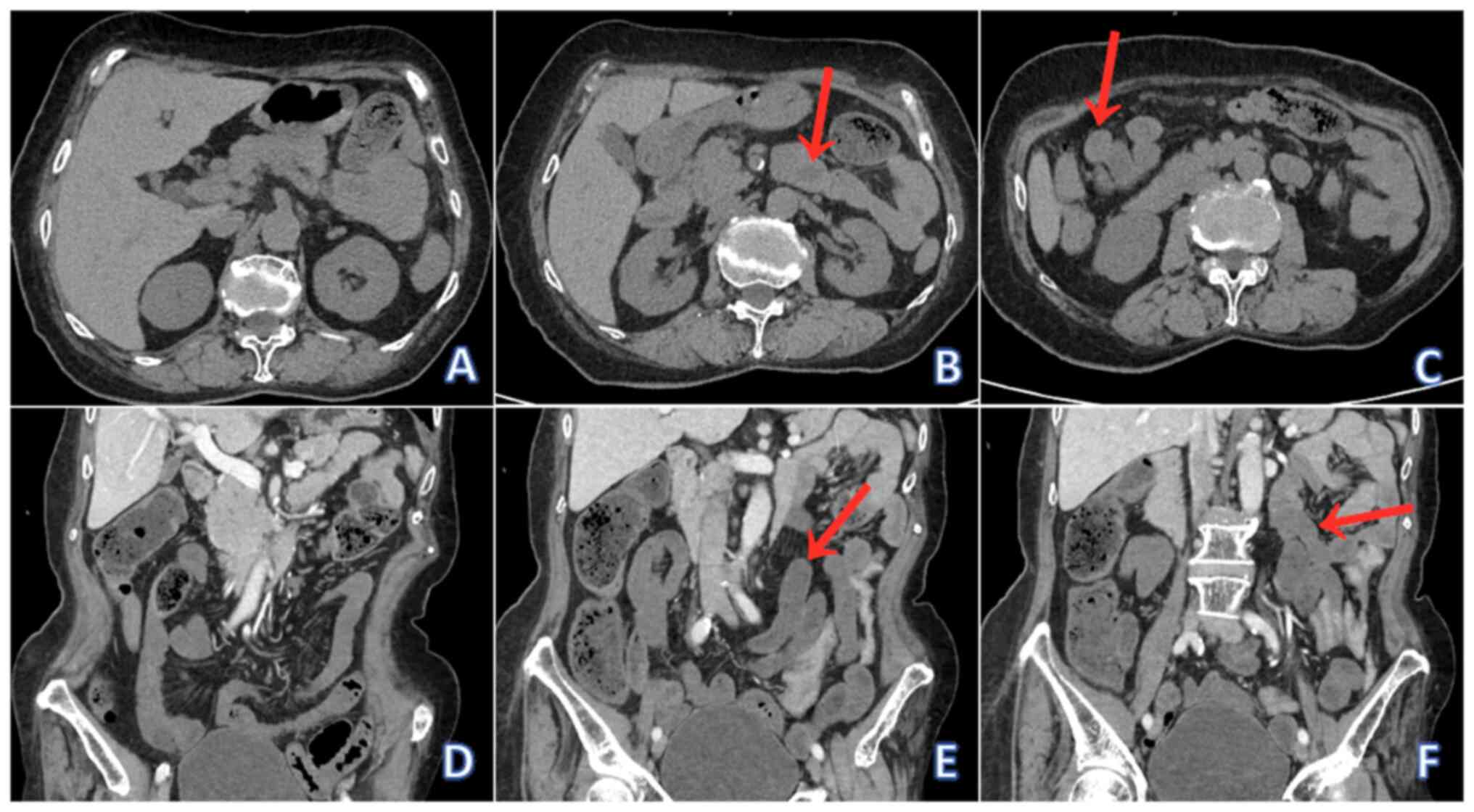
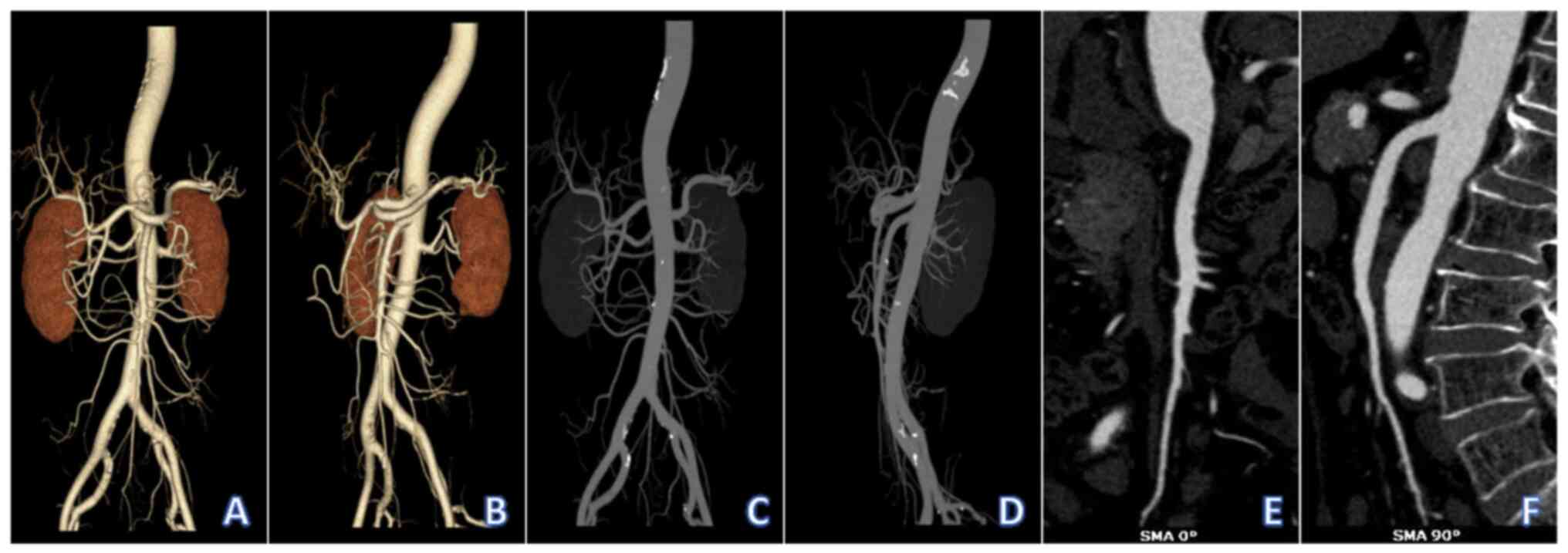
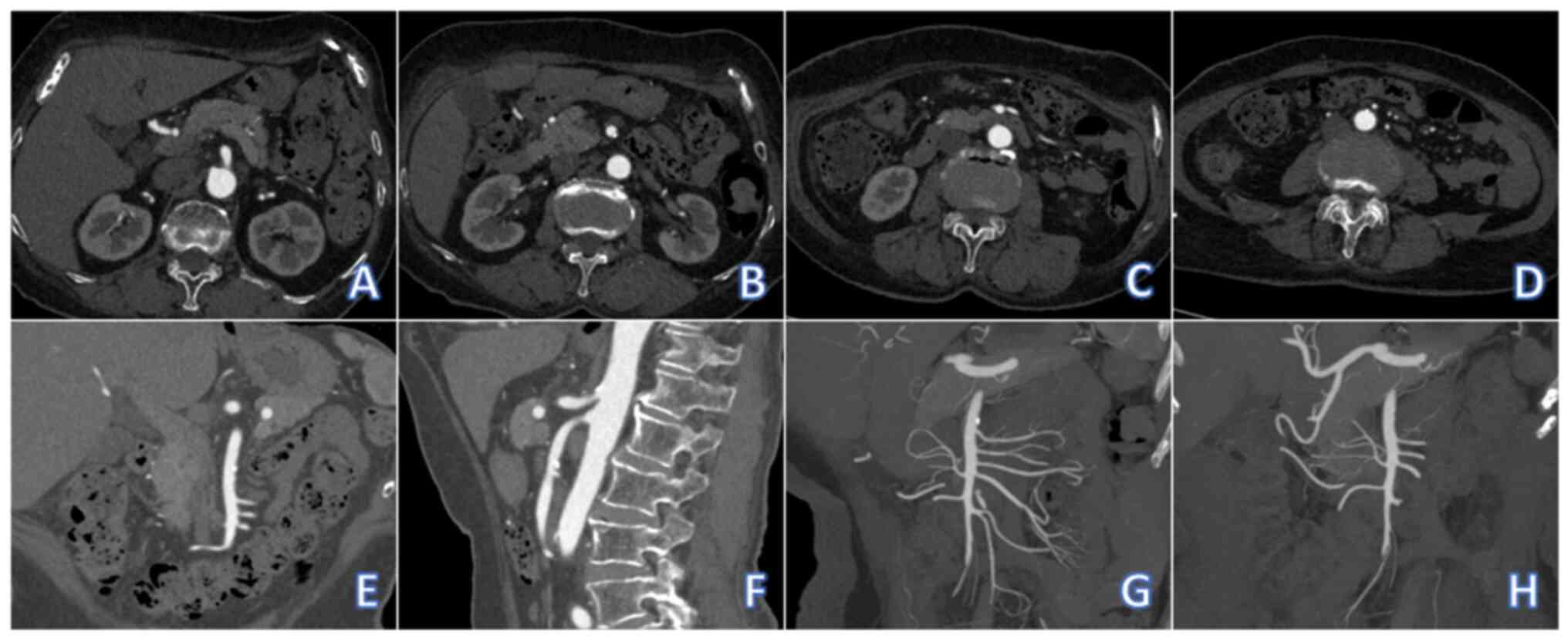
Radiological examination using a non-contrast
abdominal computed tomography (CT) showed there was no thickening
of the intestinal wall and the mesenteric space was clear (Fig. 1A), with partial effusion in the
small intestine (Fig. 1B) and no
evidence of exudation or fluid accumulation in the abdominal cavity
(Fig. 1C). Contrast-enhanced
abdominal CT showed decreased enhancement of the intestinal wall of
the lower jejunum and the upper ileum (Fig. 1D), the middle ileum and the lower
ileum (Fig. 1E), and the right
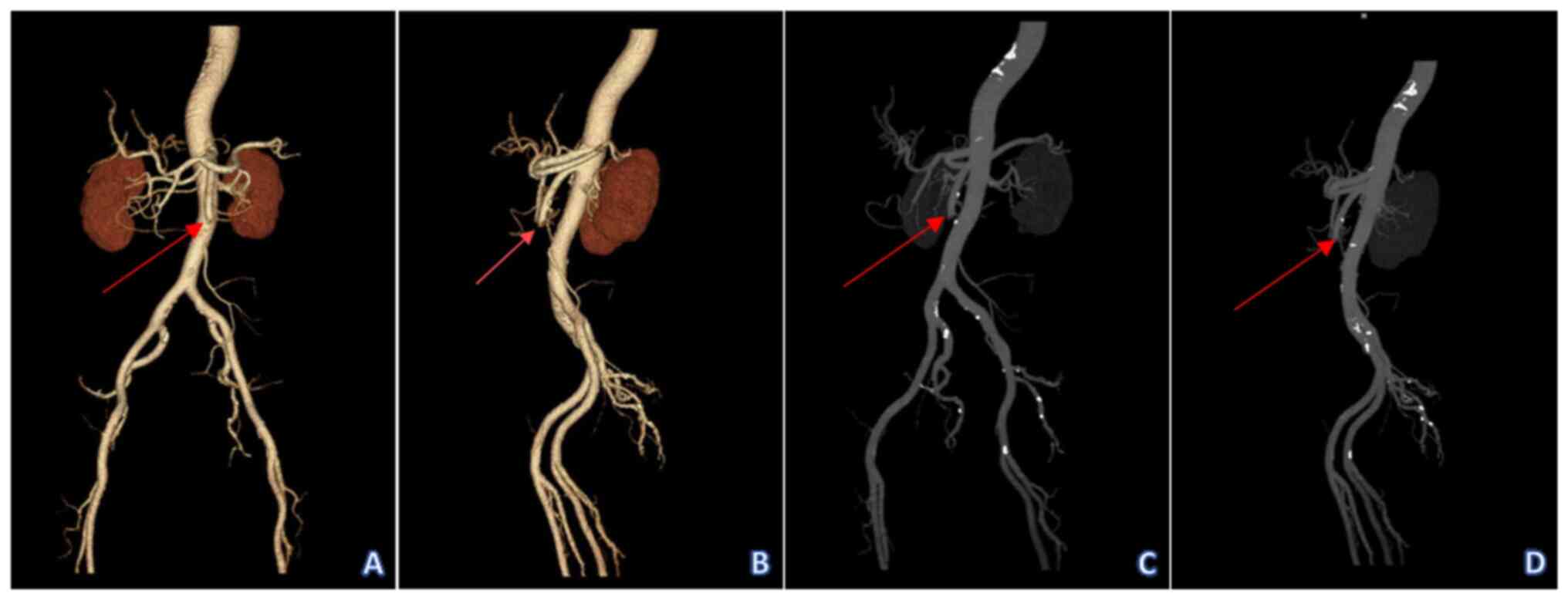
colon (Fig. 1F). SMA CT
angiography (CTA) showed a filling defect in the lumen at a
distance of 6.5 cm from the origin of the SMA below the opening of
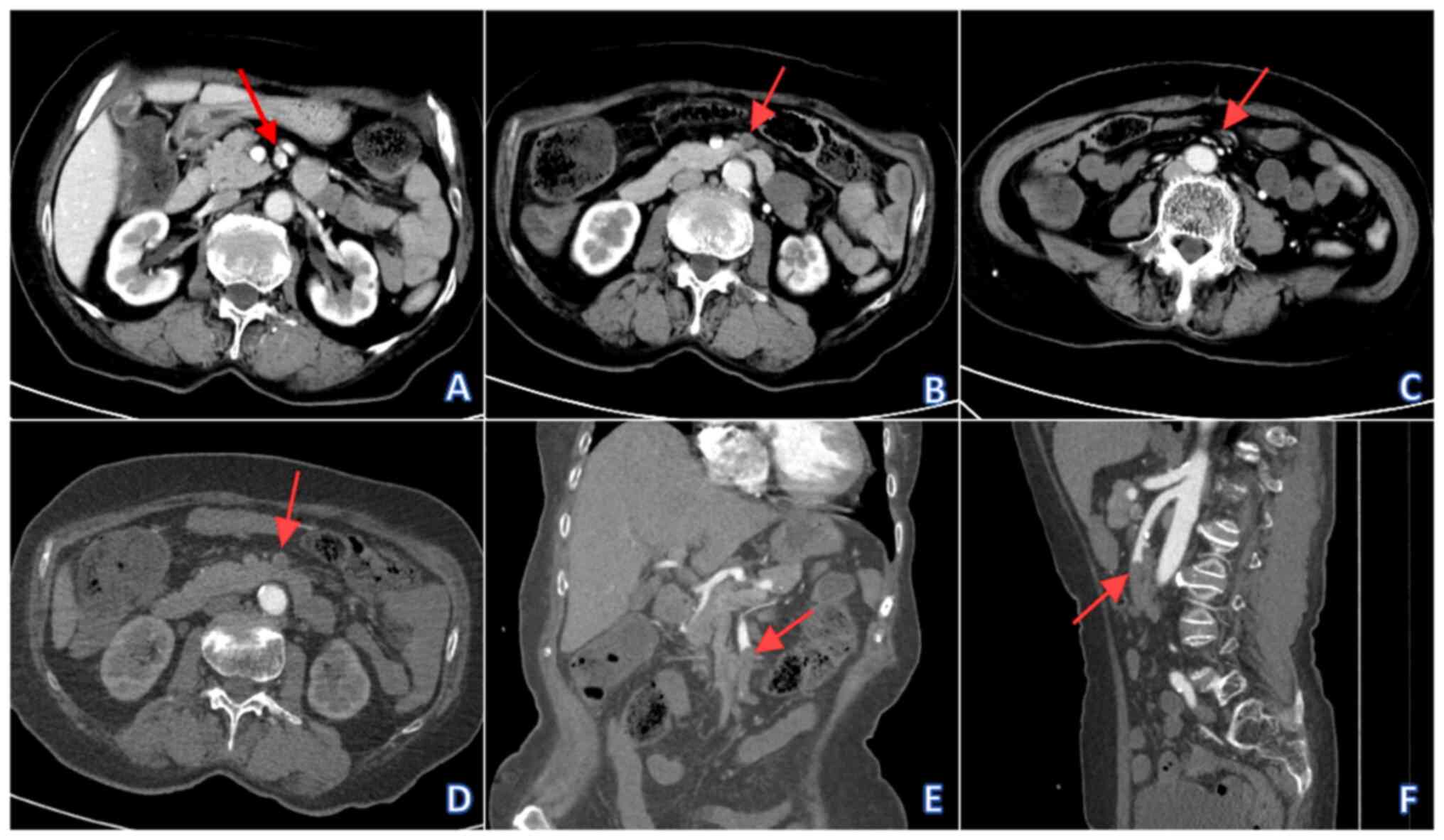
the inferior pancreaticoduodenal artery (Fig. 2). The distal end of the SMA, middle
colon artery, right colon artery, ileocolonic artery, multiple
jejunal arteries and ileal arteries were not visualized due to
thrombus blockage in the SMA (Fig.
3). Abdominal CT did not show any free gas in the abdominal
cavity, therefore ruling out gastrointestinal perforation.
Abdominal CT did not show thickening of the appendix or changes in
surrounding exudate, therefore appendicitis was ruled out.
Abdominal CT showed no abnormalities in pancreatic morphology and
density and no exudate around it, therefore acute pancreatitis was
ruled out. The final radiological diagnoses were acute SMAE and
ischemia of the right colon and small intestine in groups 3-6.
After excluding relevant contraindications,
including: i) Hypersensitivity to iodinated contrast media; ii)
severe coagulation dysfunction; iii) severe hepatic and renal
dysfunction, the patient underwent emergency surgical treatment for
a thrombectomy and thrombolysis of the SMA under general
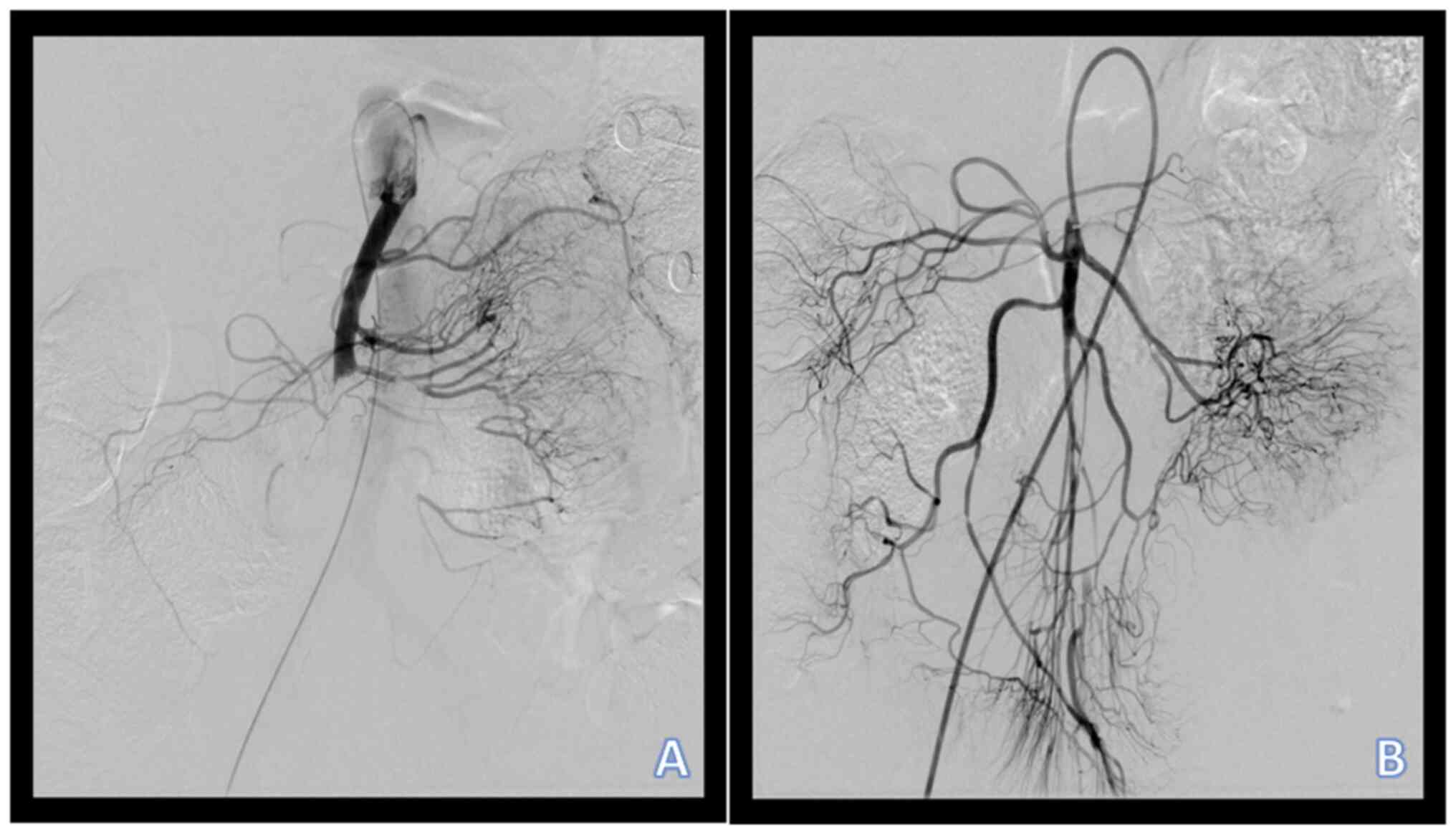
anesthesia. Additionally, angiography of the patient showed
truncation at the proximal end of the SMA, whilst the distal branch
was not visualized due to thrombus blockage in the SMA (Fig. 4A). Urokinase (urokinase for
injection, 60,000 U) and urokinase precursor (recombinant human
prourokinase for injection, 50 mg) were injected through a
catheter, following which after 10 min a peripheral thrombus
aspiration catheter was introduced to repeatedly aspirate the
thrombus in the main trunk and branches of the SMA. Following
treatment, the angiography indicated that the main trunk of the SMA
was well filled, the distal branch was well visualized and
recanalization of the SMA after embolization was achieved (Fig. 4B). After surgery, the patient was
returned to the ICU and received treatments including
electrocardiographic monitoring, assisted ventilation,
anticoagulation, fluid replacement, control of ventricular rate,
analgesia and maintenance of blood pressure.
On postoperative day 1, the patient's condition was
stabilized and the patient was then transferred to a regular ward
for continued symptomatic treatments, including anticoagulants
(Dabigatran etexilate, 150 mg, b.i.d, taken orally), antibiotics
(Cefixime, 0.1 g, b.i.d, taken orally), treatments to prevent
vasospasm vasospasm (Isosorbide Dinitrate SR Tablets, 30 mg, s.i.d,
taken orally), fluid replacement (compound sodium chloride
injection, 250 ml, b.i.d, intravenous injection), blood sugar
reduction (Gliclazide, 80 mg, b.i.d, taken orally) and control of
ventricular rate (Metoprolol Tartrate tablets, 50 mg, b.i.d, taken
orally). At 1 week after surgery, the patient's condition was
stable, resulting in discharge from hospital. The patient was
advised to take medication regularly (Aspirin Enteric-coated
Tablets, 100 mg, b.i.d, taken orally; Gliclazide, 80 mg, b.i.d,
taken orally; Metoprolol Tartrate tablets, 50 mg, b.i.d, taken
orally), consume a low-salt and low-fat diet, avoid excessive
fatigue and perform moderate exercise. At 1 week after discharge,
the patient was followed up by phone and the family of the patient
reported that the patient exhibited no significant discomfort or
further issues.
After 6 months, the patient visited The Second
Affiliated Hospital of Xuzhou Medical University for a follow-up
examination. SMA CTA showed that the main trunk and branches of the
SMA were well visualized, with no obvious sign of embolism
(Figs. 5 and 6). The timeline for the diagnosis and
treatment of the patient from the present case report was displayed
in Fig. 7. Recently, a telephone
follow-up was conducted with the patient, who was living normally
without any discomfort.
Discussion
SMAE is a type of mesenteric ischemic disease that
is caused by the entry of emboli into the mesenteric artery,
leading to acute complete vascular occlusion ischemia, before
finally necrosis of the intestinal wall and smooth muscle
dysfunction (10). SMAE has an
insidious onset and rapid development, which can cause extensive
necrosis of the small intestine and right hemicolon over a short
timeframe (11). The mortality
rate of SMAE can reach up to 90% (5). Therefore, rapid diagnosis and timely
treatment interventions serve a crucial role in reducing the
mortality rate of this disease.
SMAE typically originates from the left atrium and
is frequently associated with various types of arrhythmias, such as
atrial fibrillation (12). In
addition, it may be caused by endocarditis, leading to valve
dysfunction and thrombus detachment (13). Emboli typically exist in anatomical
stenoses and are located 3-10 cm away from the start of the SMA.
Notably, a history of atrial fibrillation and the anatomical
structure of the mesenteric artery are primary risk factors for
SMAE (14,15). The SMA frequently has an acute
angle, where it originates from the abdominal aorta. This
anatomical feature makes blood flow into the SMA prone to eddies
and turbulence, which can increase the risk of emboli entering and
blocking blood vessels (2,3). It has been previously reported that
the tolerance time for intestinal ischemic necrosis is 12 h,
whereby intestinal ischemia lasting for 4-6 h can lead to severe
intestinal damage (16).
The patient in the present case had a number of risk
factors for thromboembolism, including atrial fibrillation and
diabetes mellitus. Patients with atrial fibrillation may experience
a series of hemodynamic changes, changes in atrial structure
(atrial enlargement and myocardial fibrosis) and activation of the
coagulation system, all of which are associated with thrombus
formation (17). Furthermore,
patients with diabetes mellitus are in a chronic state of
hyperglycemia and inflammation, which is accompanied by insulin
resistance and metabolic disorders (protein metabolism disorder and
dyslipidemia), further increasing the risk of thrombosis (18). The anticoagulant and T2DM
controlled in this patient were not satisfactory. Therefore,
anticoagulant control for atrial fibrillation-related thrombosis
and control for diabetes mellitus were recommended for the patient
in the present case.
The main method used for the early diagnosis of SMAE
is severe upper abdominal and periumbilical pain without
corresponding signs (persistent, non-focal abdominal pain or
periumbilical colic), a history of heart disease (in particular
atrial fibrillation) and gastrointestinal symptoms (such as
vomiting and diarrhea), known as the ‘Bergan triad’ (19). Currently, no specific laboratory
test indicators are available for the diagnosis of SMAE. A previous
study reported that elevated D-dimer levels are an independent risk
factor for intestinal ischemia, though its validity requires
further investigation (20). In
clinical practice, an increase in the D-dimer level typically
indicates the presence of thrombosis or thrombolytic processes in
the body, which may be induced by various factors, such as
malignant tumors, infection, fever, myocardial infarction and
atrial fibrillation (21).
Therefore, the detection of D-dimer levels would be of benefit for
the early detection of hypercoagulability and prevention of
thrombosis (22). This patient's
D-dimer level was mildly elevated, which gave some hints to rule
out the possibility of embolism. In this regard, the detection of
D-dimer levels may also be useful for the diagnosis of patients
with suspected SMAE (23).
Abdominal X-rays lack specificity for the diagnosis
of SMAE, where >25% patients with mesenteric ischemia have
yielded false negative results (24). In this case, the patient's
abdominal X-ray result was negative. Observation of intestinal
obstruction, wall thickening and inflation may contribute to the
successful diagnosis of SMAE, but these clinical manifestations
typically occur during the latter stages of the disease (25). CTA therefore confers diagnostic
advantages compared with other tests, since it typically has a
shorter examination time, higher accuracy and the capability of
observing the location and range of SMAE, making it the preferred
radiological examination for SMAE (26).
According to the clinical and radiological
manifestations of the patient from the present case, SMAE should be
differentiated from a number of conditions, namely isolated SMA
dissection, SMA vasculitis, SMA aneurysm and non-occlusive
mesenteric ischemia (NOMI).
Isolated SMA dissection involves damage and rupture
of the intima and media of the SMA due to endogenous or exogenous
factors, causing blood to rush into the arterial wall and a
dissection to occur (27). On CTA
images, SMA appears as a double lumen shadow, which is specific to
SMA dissection, whilst the false lumen surrounds the true lumen in
a crescent shape. The density of the true lumen is different from
that of the false counterpart, where endometrial patches can be
found between them. The true lumen can be compressed to varying
degrees and either become thinner or occluded. In some patients,
the entrance and exit of the false lumen can be observed (28).
SMA vasculitis is inflammation of the SMA wall,
which can be caused by a number of factors, such as autoimmune
disease, bacterial infection and hypertension (29). On CTA images, circular thickening
of the arterial wall, luminal narrowing and microaneurysms can be
observed during SMA vasculitis. The long segment lumen gradually
narrows and multiple aneurysms can mimic the bead-like appearance
of SMA (30).
SMA aneurysm typically occurs 5 cm proximal to SMA
(31). SMA aneurysms can be
classified as either a true aneurysm or a pseudo-aneurysm. A true
aneurysm results from the dilation of the arterial wall, which is
at ≥1.5 times the normal diameter. On CTA images, this typically
appears as spindle-shaped or cystic SMA dilation, with continuous
wall calcification. A pseudo-aneurysm is caused by vascular injury,
where blood flows out from a rupture and is enveloped by the
surrounding connective tissue. On the CTA images of
pseudo-aneurysms, adjacent hematomas, extensive wall thrombi and
discontinuous wall calcification can be observed (32).
NOMI is an acute mesenteric circulatory system
disease without organic obstruction of the main mesenteric artery
or vein, which has a high mortality rate (30-70%) (33). Its pathogenesis is typically
characterized by intestinal microcirculatory dysfunction with
systemic circulatory disorders (34). NOMI does not exhibit obvious
thrombosis compared with SMAE, where angiography may have
differential diagnostic significance for this disease.
Once a diagnosis of acute SMAE is confirmed, fluid
resuscitation should be started immediately, regardless of the
presence of shock symptoms, aiming to increase visceral perfusion,
actively improve heart function, prevent infection, correct
acidosis and electrolyte imbalance (35). If the patient's condition permits,
early intravascular intervention therapy should be performed to
achieve an improved prognosis. In the case of an irreversible
embolism of the intestinal vessels or irreversible intestinal
necrosis, surgical intervention should be performed urgently to
avoid the absorption of toxins (36,37).
If absorption of toxins happens, it may lead to systemic
inflammatory response syndrome, multiple organ dysfunction, septic
shock and coagulation dysfunction (38). The goals of surgical intervention
should be to re-establish the blood supply to the ischemic site,
remove all non-functional areas of the intestine, preserve all
functional areas of the intestine and enlarge the scope of
intestinal resection to ≥15 cm above and below the necrotic
intestine to avoid anastomotic leakage after surgery. Meanwhile,
the occluded mesentery should be removed (39).
In the present case, the patient experienced
intestinal ischemia for a relatively short period of time, which
lasted ~3 h from the onset of the disease and definitive diagnosis,
to thrombectomy and thrombolysis of the SMA, which achieved
vascular recanalization. A rapid diagnosis and timely and effective
interventions enabled the patient to achieve a good prognosis,
avoiding possible postoperative complications, including short
bowel syndrome.
In conclusion, for patients with unexplained acute
abdominal pain, particularly those with concomitant heart disease,
such as atrial fibrillation and elevated D-dimer levels, the
possibility of SMAE should be taken into consideration by
clinicians. In addition, to achieve a good prognosis, appropriate
examination methods, such as CTA, should be utilized to achieve
early diagnosis and treatment, where patients should adhere to
anticoagulation (drug anticoagulation and physical anticoagulation)
and anti-shock treatments (complement of blood volume and improving
microcirculation) following surgery.
Acknowledgements
Not applicable.
Funding
Funding: The present case report was supported by the Key
Research & Development Project of Xuzhou Science and Technology
Bureau (grant no. KC23208) and the Development Fund Project of
Xuzhou Medical University Affiliated Hospital (grant no.
XYFY202460).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YW and PD were responsible for the conception and
design of the study, collection and assembly of data, the writing
and revision of the manuscript. All authors read and approved the
final version of the manuscript. YW and PD confirm the authenticity
of all the raw data.
Ethics approval and consent to
participate
The present case report was reviewed and approved by
Ethics Committee of The Second Affiliated Hospital of Xuzhou
Medical University (approval no. KY-20241317). The patient provided
written informed consent to participate in the present study.
Patient consent for publication
The patient provided written consent for the
publication of their information and associated clinical
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Xu R, Tang L, Qin S, Zhang S and Wang M:
Percutaneous mechanical thrombectomy using the AcoStream thrombus
aspiration system for acute superior mesenteric artery embolism.
Ann Vasc Surg. 106:264–272. 2024.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kerdiles T and Gras J: Superior mesenteric
artery syndrome. N Engl J Med. 389(359)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Balcerzak A, Tubbs RS,
Waśniewska-Włodarczyk A, Rapacka E and Olewnik Ł: Classification of
the superior mesenteric artery. Clin Anat. 35:501–511.
2022.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Jing Y, Xu J, Chen B, Xia D, Xia D, Tian
Y, Xia W, Lu C and Wu Y: Superior mesenteric artery embolism after
radiofrequency ablation in regularly anticoagulated patients with
paroxysmal atrial fibrillation: A case report. BMC Cardiovasc
Disord. 23(56)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang Z, Chen X, Li C, Feng H, Yu H and
Zhu R: Percutaneous mechanical thrombectomy for acute superior
mesenteric artery embolism: Preliminary experience in five cases.
Ann Vasc Surg. 63:186–192. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Du R, Zhang J, Chang Y and Liu Y: A case
of acute superior mesenteric artery embolism caused by constipation
after hemorrhoid surgery. Asian J Surg. 45:2420–2422.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yun WS, Lee KK, Cho J, Kim HK and Huh S:
Treatment outcome in patients with acute superior mesenteric artery
embolism. Ann Vasc Surg. 27:613–620. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yang JS, Xu ZY, Chen FX, Wang MR, Cong RC,
Fan XL, He BS and Xing W: Role of clinical data and multidetector
computed tomography findings in acute superior mesenteric artery
embolism. World J Clin Cases. 10:4020–4032. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yu Z, Hu J and Lang D: Pseudoaneurysm as a
rare complication in the treatment of superior mesenteric artery
embolism via percutaneous mechanical thrombectomy: A case report. J
Int Med Res. 49(3000605211022941)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Barakate MS, Cappe I, Curtin A, Engel KD,
Li-Kim-Moy J, Poon MS and Sandeman MD: Management of acute superior
mesenteric artery occlusion. ANZ J Surg. 72:25–29. 2002.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhang YR, Li ZY, Liang J, Bai S and Zhang
ZF: Diagnostic value of mesenteric CTA combined with D-dimer level
and inflammatory factor changes in severity of mesenteric artery
embolism. Pak J Med Sci. 39:1321–1325. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liao G, Chen S, Cao H, Wang W and Gao Q:
Review: Acute superior mesenteric artery embolism: A vascular
emergency cannot be ignored by physicians. Medicine (Baltimore).
98(e14446)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chinsakchai K, Wongwanit C, Ruangsetakit C
and Mutirangura P: Successful treatment in superior mesenteric
artery embolism: A case report and literature review. J Med Assoc
Thai. 93:739–744. 2010.PubMed/NCBI
|
|
14
|
Wang B, Sun R, Chen W and Li T:
Enlightenment and lesson from the successful treatment of acute
superior mesenteric artery embolism. Cell Mol Biol
(Noisy-le-grand). 63:23–27. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sato O, Okamoto H and Matsumoto H:
Emergency CT scan for the diagnosis of superior mesenteric artery
embolism. Report of 2 cases. Int Angiol. 22:438–440.
2003.PubMed/NCBI
|
|
16
|
Tsuda M, Nakamura M, Yamada Y, Saito H,
Ishibashi T and Takahashi S: Acute superior mesenteric artery
embolism: Rapid reperfusion with hydrodynamic thrombectomy and
pharmacological thrombolysis. J Endovasc Ther. 10:1015–1018.
2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sagris M, Vardas EP, Theofilis P,
Antonopoulos AS, Oikonomou E and Tousoulis D: Atrial fibrillation:
Pathogenesis, predisposing factors, and genetics. Int J Mol Sci.
23(6)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cloete L: Diabetes mellitus: An overview
of the types, symptoms, complications and management. Nurs Stand.
37:61–66. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang H, Xiao X, Zhang W, Ma Z, Zhang JL,
Tang L and Yang X: Imaging of acute superior mesenteric artery
embolus using spectral CT in a canine model. Br J Radiol.
88(20150296)2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Simó G, Echenagusia AJ, Camúñez F,
Turégano F, Cabrera A and Urbano J: Superior mesenteric arterial
embolism: Local fibrinolytic treatment with urokinase. Radiology.
204:775–779. 1997.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wang G, Lu W, Xia Q, Mao B, Wang L, Li T
and Jiang L: Superior mesenteric arterial embolism: A retrospective
study of local thrombolytic treatment with urokinase in West China.
Int J Clin Pract. 57:588–591. 2003.PubMed/NCBI
|
|
22
|
Franchini M, Focosi D, Pezzo MP and
Mannucci PM: How we manage a high D-dimer. Haematologica.
109:1035–1045. 2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Halaby R, Popma CJ, Cohen A, Chi G,
Zacarkim MR, Romero G, Goldhaber SZ, Hull R, Hernandez A, Mentz R,
et al: D-Dimer elevation and adverse outcomes. J Thromb
Thrombolysis. 39:55–59. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sinha D, Kale S, Kundaragi NG and Sharma
S: Mesenteric ischemia: A radiologic perspective. Abdom Radiol
(NY). 47:1514–1528. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sugiyama C, Akai A, Yamakita N, Yasuda K
and Ihara N: Rupture of pancreaticoduodenal artery aneurysm caused
by superior mesenteric artery embolism. Am J Gastroenterol.
103:1841–1842. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Heiss P, Loewenhardt B, Manke C, Hellinger
A, Dietl KH, Schlitt HJ, Scheibl K, Feuerbach S and Paetzel C:
Primary percutaneous aspiration and thrombolysis for the treatment
of acute embolic superior mesenteric artery occlusion. Eur Radiol.
20:2948–2958. 2010.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Luan JY, Guan X, Li X, Wang CM, Li TR,
Zhang L and Han JT: Isolated superior mesenteric artery dissection
in China. J Vasc Surg. 63:530–536. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Anil G, Wee-Thong N and Ashley Robless P:
Short bowel syndrome after endovascular recanalization of superior
mesenteric artery embolic occlusion: A rare event. J Vasc Interv
Radiol. 23:1709–1711. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Alkhader A, Saleh N, Mansour MM, Hussein O
and Saad B: Expect the unexpected: A rare case of isolated superior
mesenteric artery vasculitis. Cureus. 15(e40106)2023.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Haymet AB, Lee D, Ho-Shon K and Waugh R:
When the conventional treatment fails: A rare approach to superior
mesenteric arterial embolization. Vasc Endovascular Surg.
54:169–171. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Xu X, Eubanks AL, Wladis A, Veldhuis P and
Eubanks S: Mycotic superior mesenteric artery aneurysm: Case report
and literature review. Surg Innov. 26:260–264. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Calin GA, Calin S, Ionescu R, Croitoru M,
Diculescu M and Oproiu A: Successful local fibrinolytic treatment
and balloon angioplasty in superior mesenteric arterial embolism: A
case report and literature review. Hepatogastroenterology.
50:732–734. 2003.PubMed/NCBI
|
|
33
|
Ikeda A, Yamada S, Ishizaka R, Sakurai K,
Takatsuka D, Takaichi M, Fujiwara K and Noguchi M: Non-obstructive
mesenteric ischaemia during drug therapy for maxillary cancer: A
case report. Biomed Rep. 21(172)2024.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Bourcier S, Klug J and Nguyen LS:
Non-occlusive mesenteric ischemia: Diagnostic challenges and
perspectives in the era of artificial intelligence. World J
Gastroenterol. 27:4088–4103. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kim YW, Choi HC, Yang WJ, Koo BJ, Ahn JK,
Lee JP, Na JB, Jo SH, Park SE and Won JH: Microcatheter-directed
thrombolysis using recombinant tissue plasminogen activator for the
treatment of acute superior mesenteric artery embolism: A case
report. Medicina (Kaunas). 59(1889)2023.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Blessing E, Rottbauer W, Mereles D, Hosch
W, Benz A, Friess H, Autschbach F, Müller M, Stremmel W and Katus
H: Isolated left ventricular noncompaction of the myocardium as a
cause of embolic superior mesenteric artery occlusion. J Am Soc
Echocardiogr. 18(693)2005.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Nakayama T, Nakamura Y, Niitsuma K,
Ushijima M, Yasumoto Y, Kuroda M, Nakamae K, Minamidate N, Hayashi
Y, Tsuruta R, et al: Totally thoracoscopic atrial fibrillation
surgery following massive small bowel resection due to superior
mesenteric artery embolization: Report of two cases. Surg Case Rep.
10(141)2024.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ahue KHN, Goho KM, Adon AA, Coulibaly NA,
Kpan KJ and Keita M: Bifocal bowel obstruction by synchronous
transverse and sigmoid colon volvulus: A case report and
qualitative review of the literature. Int J Surg Case Rep.
123(110312)2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Xu Q, Wang Y, Xu B, Lang D and Lin Z:
Efficacy and safety analysis of AcoStream thrombus aspiration
device in the treatment of acute superior mesenteric artery
embolism. Vascular. (17085381241240865)2024.PubMed/NCBI View Article : Google Scholar : (Epub ahead of
print).
|