Introduction
The 2019 novel coronavirus (2019-ncov, named SARS-CoV-2 by the International Committee on Classification of Viruses) emerged in 2019 and has rapidly spread throughout the world. The pathogen responsible for the outbreak has been identified as a newly discovered enveloped RNA beta-coronavirus. It belongs to the same family as the SARS-CoV virus, which caused the severe acute respiratory syndrome (SARS) outbreak in 2002-2003 (1,2). As of March 2022, over 600 million individuals have been infected, and tragically, >6.5 million lives have been lost due to the severe impact of the virus (3,4), which resulted in high rates of hospitalization and intensive care unit admissions (5). This global pandemic has not only posed a significant threat to human life safety but has also caused profound disruptions to international economic development. SARS-CoV-2 infection is not limited to the respiratory system; it can affect multiple organs, including the lungs, liver, heart and kidneys. Additionally, as proposed by Lechien et al (6), olfactory dysfunction appears to be an important underestimated symptom of mild-to-moderate COVID-19 infection. In severe cases, patients may develop acute respiratory distress syndrome, experience multiple organ failure, and even succumb to the infection. Notably, it has been observed that individuals with chronic kidney disease (CKD) are at an increased risk of contracting SARS-CoV-2 and have a higher likelihood of mortality after infection (4,7). In a study by Popov et al (8), older men with underlying hypertension, cardiovascular, malignant, and chronic kidney diseases with signs of dyspnea and nausea were at higher risk for severe clinical form. Patients with maintenance hemodialysis (MHD) along with end-stage renal disease (ESRD) complications and immunosuppression are more susceptible to severe infection (9). There is still a significant lack of knowledge regarding the occurrence of COVID-19 infections and the risk factors. Extensive research conducted in China, Italy and England, has reported a wide range of COVID-19 incidence rates spanning from 2 to 30%, among outpatient hemodialysis centers. Moreover, the mortality rate associated with COVID-19 infections in these centers has been reported to reach as high as 30% (10). Recent research has shed light on the crucial role of vitamin D in the immune system, establishing it as a hormone with various extra-skeletal effects (11). Drechsler et al (12) revealed that for each unit decrease in 25-hydroxyvitamin D [25(OH)D] levels below 20 ng/ml, the risk of death from infection increased. In addition, clinical trials and meta-analyses have suggested that supplementation with cholecalciferol or ergocalciferol (forms of vitamin D) may help prevent acute respiratory infections (13). Observational studies have revealed that low serum 25(OH)D levels are associated with an increased risk of SARS-CoV2 infection (14,15). Given these observations, the aim of the present study was to investigate the various risk factors that contribute to the occurrence of co-infection with COVID-19 among patients with MHD, and to analyze the relationship between 25(OH)D levels and COVID-19, as well as to assess the risk factors associated with COVID-19 and mortality, which could provide valuable insights into the potential role of vitamin D in preventing or mitigating COVID-19 among patients with MHD.
Patients and methods
Diagnosis of cases
The COVID-19 diagnosis of the patients was confirmed after conducting a real-time PCR test from a throat swab sample at the laboratory of the People's Hospital of Ningxia Hui Autonomous Region (Yinchuan, China). Chest computed tomography (CT) scans were further used to assist in diagnosing and evaluating the condition of the patients.
Inclusion and exclusion criteria
The present retrospective study included 171 patients with MHD who received treatment at the hemodialysis center of the People's Hospital of Ningxia Hui Autonomous Region (Yinchuan, China) from January 2022 to January 2023. The mean age of the patients was 55.18±14.01 years and 69.01% were male. The inclusion criteria were as follows: Patients with MHD receiving regular hemodialysis treatment for >3 months, undergoing at least two dialysis sessions per week, and having complete medical records. The exclusion criteria were as follows: Patients who had undergone hemodialysis (HD) treatment for a duration of <3 months, and <2 times per week. In addition, research data from individuals with treatment incompatibilities, such as allergic reactions or adverse side effects, were not included in the present study.
Data collection and participants
The general information included age, sex, body mass index, dialysis duration, dialysis frequency, cause of end-stage kidney disease, hypertension, diabetes mellitus and coronary heart disease.
Laboratory data included the following parameters: White blood cell count, hemoglobin, lymphocyte count, platelet count, urea, creatinine, sodium, potassium, calcium, phosphorus, parathyroid hormone (PTH), prealbumin, albumin, C-reactive protein (CRP), Kt/V, 25(OH)D, folic acid, Vitamin B12, serum iron and serum ferritin.
RT-PCR assay
All patients were sampled with nasopharyngeal/oropharyngeal swabs, and these samples underwent real-time reverse-transcription-polymerase-chain-reaction (RT-PCR) assay. RT-PCR was performed using the Novel Coronavirus 2019-nCoV Nucleic Acid Test Kit (cat. no. DA0990; PCR-Fluorescence Method; Daan Gene Co., Ltd.). The primers for RT-PCR for the detection of the ORF1ab gene: ORF1ab forward, 5'-CCCTGTGGGTTTTACACTTAA-3' and reverse, 5'-ACGATTGTGCATCAGCTGA-3'. The primers for RT-PCR for the detection of the N gene were: N gene forward, 5'-GGGGAACTTCTCCTGCTAGAAT-3' and reverse, 5'-CAGACATTTTGCTCTCAAGCTG-3'. RNase P was used as the housekeeping gene, and the primers were: RNase P forward, 5'-TGAATGTCGTCTCTCAACTAGCC-3' and reverse, 5'-CTCCGTCTTAGCATGTGCTTC-3'. According to the protocol of the kit (Dan Gene Co., Ltd.), the nucleic acid was extracted from the clinical samples and blended with the Master mix provided in the kit before running. PC reactions were run in a 20-µl final volume. The mixture was placed into a real-time PCR thermocycler for PCR amplification: First step, enzyme activation at 95˚C for 2 min; second step, amplification at 95˚C for 5 sec and 60˚C for 15 sec, for 42 cycles. Relative fold changes of genes expression were calculated by the 2-ΔΔCq method (16).
Imaging and invasive procedures
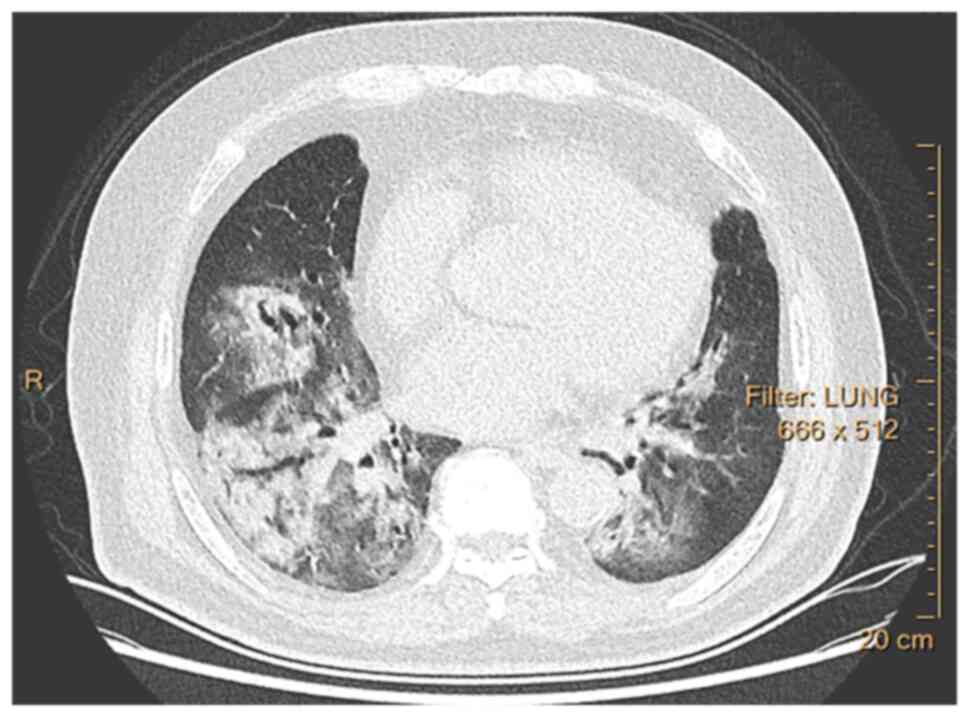
Lung tomography was performed in patients with symptoms suspected to be caused by COVID-19. Multiple small patchy shadows or ground-glass opacities and consolidation in the peripheral distribution of the lungs are related to pulmonary involvement in COVID-19. PCR positive or typical CT findings were used for the diagnosis of COVID-19 disease.
Statistical analysis
Data was analyzed using the IBM SPSS version 23.0 statistical software. Categorical variables were analyzed using Chi square test of independence. Measurement data with normal distribution were expressed as the mean ± standard deviation, and comparison between groups was analyzed by independent sample t-test. Count data were described by constituent ratio. Additionally, to investigate the factors affecting the binary response variable, logistic regression with binomial link function was implemented. Finally, P<0.05 was considered to indicate a statistically significant difference.
Ethical considerations
The present study was a single-center, retrospective, observational study. The Medical Ethics Committee of the People's Hospital of Ningxia Hui Autonomous Region (Yinchuan, China) approved [approval no. (2023)-LL-045] the protocol of the present study on September 7, 2023. The present study adhered to the principles of the Declaration of Helsinki. The patients provided written informed consent for the publication of any associated data and accompanying images.
Results
The demographic and clinical parameters of all patients with MHD are presented in Table I. The mean age of the patients was (55.18±14.01) years, and 69.01% were male. The most common cause of ESRD was chronic glomerulonephritis (60.23%). The average dialysis vintage was 63.45±42.75 months, and the average dialysis frequency was 2.91±0.27 times per week. The most common comorbidities of the 171 patients with MHD were hypertension (100%), followed by coronary heart disease (31.58%) and diabetes (28.07%). In total, 89 patients (52.05%) were infected with COVID-19, of which 11 patients (6.43%) succumbed to the disease. The lung CT scans of patients who were infected with COVID-19 exhibited the presence of distinctive and characteristic lesions, such as ground-glass opacity and concurrent areas of consolidation (Figs. 1 and 2).
 |
Figure 1
Chest computed tomography findings of COVID-19 pneumonia on a transaxial image, revealing bilateral, patchy ground-glass parenchymal opacities with prevalent peripheral and mid-lower lobe distribution. All images have the same window level of -600 and window width of 1,600.
|
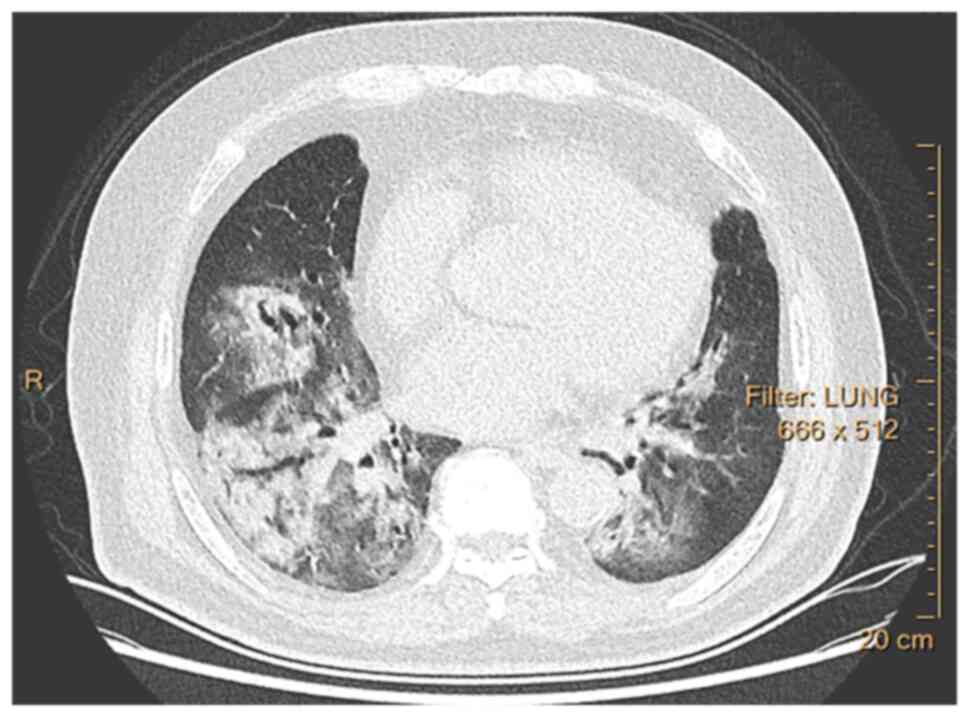 |
Figure 2
Chest computed tomography findings of COVID-19 pneumonia on a transaxial image, revealing bilateral patchy ground-glass opacities associated with small areas of consolidation. All images have the same window level of -600 and window width of 1,600.
|
 |
Table I
Demographic and clinical characteristics of patients with maintenance hemodialysis pre-COVID-19 infection.
|
Table I
Demographic and clinical characteristics of patients with maintenance hemodialysis pre-COVID-19 infection.
| Parameter |
Value |
| Age, years |
55.18±14.01 |
| Male sex, n (%) |
118 (69.01) |
| BMI, kg/m2 |
22.36±3.82 |
| Dialysis vintage, months |
63.45±42.75 |
| Dialysis frequency, times/week |
2.91±0.27 |
| Primary kidney disease |
|
| Glomerulonephritis |
103 (60.23) |
| Diabetic nephropathy |
46 (26.90) |
| Hypertensive nephropathy |
5 (2.92) |
| Polycystic kidney |
6 (3.51) |
| Obstructive nephropathy |
3 (1.76) |
| Lupus nephritis |
5 (2.92) |
| AAV |
3 (1.76) |
| Kt/v ≥1.2 |
110 (64.33) |
| Kt/v ≥1.4 |
56 (32.75) |
| Comorbidity |
|
| Hypertension |
171(100) |
| Diabetes |
48 (28.07) |
| Coronary heart disease |
54 (31.58) |
| WBC, 109/l |
6.34±2.02 |
| Lym, 109/l |
1.29±0.43 |
| Hb, g/l |
115.97±20.08 |
| Plt, 1012/l |
171.76±62.74 |
| BUN, mmol/l |
23.82±6.48 |
| SCR, µmol/l |
923.68±239.56 |
| Ca, mmol/l |
2.22±0.22 |
| P, mmol/l |
1.70±0.49 |
| iPTH, pg/ml |
400.30±0.49 |
| CRP, mg/l |
6.90±10.51 |
| 25(OH)D, ng/ml |
22.3±11.28 |
| SI, µmol/l |
11.21±5.18 |
| SF, ng/ml |
420.13±398.15 |
| Alb, g/l |
38.67±2.91 |
| PA, mg/l |
294.29±71.94 |
| COVID-19-infected patients |
89 (52.05) |
| Mortality related to COVID-19 |
11 (6.43) |
Comparison of the clinical parameters at baseline between patients who contracted COVID-19 and those who did not, is shown in Table II. The findings revealed that infected patients had lower levels of iPTH and folic acid, as well as a lower proportion of taking Vitamin D analogues compared with non-infected patients, and these results were found to be statistically significant (P<0.05). Conversely, the infected patients had higher levels of CRP and serum ferritin compared with the non-infected patients, emphasizing the presence of inflammation and iron overload in the infected group. These differences were also found to be statistically significant (P<0.05). Notably, there was no significant difference observed in the levels of 25(OH)D between the two groups.
 |
Table II
Comparison of baseline characteristics between patients with maintenance hemodialysis infected and uninfected with COVID-19.
|
Table II
Comparison of baseline characteristics between patients with maintenance hemodialysis infected and uninfected with COVID-19.
| Parameter |
COVID-19 (-) (n=82) |
COVID-19 (+) (n=89) |
P-value |
| Age, years |
55±14.62 |
55.35±13.51 |
0.872a |
| Male sex |
54 (67.07) |
64 (71.91) |
0.395b |
| BMI, kg/m2 |
22.59±3.19 |
22.16±4.34 |
0.459a |
| Dialysis vintage, months |
63.93±40.98 |
63.01±44.54 |
0.889a |
| Dialysis frequency (times/week) |
2.92±0.28 |
2.90±0.27 |
0.699a |
| Diabetic nephropathy |
23 (28.05) |
25 (28.09) |
0.995b |
| Coronary heart disease |
27 (32.93) |
27 (30.34) |
0.718b |
| WBC, 109/l |
6.39±2.03 |
6.29±2.02 |
0.742a |
| Lym, 109/l |
1.33±0.45 |
1.25±0.41 |
0.200a |
| Hb, g/l |
117.74±18.76 |
114.34±21.21 |
0.269a |
| Plt, 1012/l |
173.99±62.74 |
169.71±63.02 |
0.657a |
| BUN, mmol/l |
23.50±6.57 |
24.13±6.41 |
0.528a |
| SCR, µmol/l |
924.22±237.40 |
922.98±242.88 |
0.968a |
| Ca, mmol/l |
2.25±0.22 |
2.20±0.22 |
0.218a |
| P, mmol/l |
1.70±0.51 |
1.69±0.47 |
0.880a |
| iPTH, pg/ml, |
462.39±397.02 |
343.09±271.74 |
0.022a,c |
| CRP, mg/l |
5.15±5.47 |
8.52±13.43 |
0.036a,c |
| 25(OH)D, ng/ml |
22.83±11.74 |
21.81±10.88 |
0.557a |
| Vitamin B12, pg/ml |
553.44±304.77 |
490.11±236.30 |
0.129a |
| Folic acid, ng/ml |
11.94±7.99 |
9.63±6.92 |
0.045a,c |
| SI, µmol/l |
11.52±5.38 |
10.91±5.00 |
0.443a |
| SF, ng/ml |
357.67±339.43 |
477.69±439.55 |
0.049a,c |
| Alb, g/l |
38.51±2.71 |
38.82±3.08 |
0.497a |
| PA, mg/l |
298.77±70.40 |
290.16±73.48 |
0.435a |
| Intake of vitamin D analogues |
71 (86.59) |
66 (74.16) |
0.049a,c |
Based on the independent variables presented in Table II, logistic regression analysis was performed to examine their relationship with COVID-19 in patients with MHD. The analysis revealed that both iPTH and serum ferritin levels were identified as risk factors for COVID-19 in patients with MHD, as indicated in Table III.
 |
Table III
Logisitic regression analysis of COVID-19-infected patients with maintenance hemodialysis.
|
Table III
Logisitic regression analysis of COVID-19-infected patients with maintenance hemodialysis.
| Parameter |
B |
SE |
Wald |
P-value |
OR |
95% CI |
| Lym |
-0.766 |
0.421 |
3.309 |
0.069 |
0.465 |
0.204-1.061 |
| iPTH |
-0.001 |
0.001 |
5.913 |
0.015a |
0.999 |
0.998-1 |
| Vitamin B12 |
-0.001 |
0.001 |
2.054 |
0.152 |
0.999 |
0.998-1 |
| Folic acid |
-0.036 |
0.023 |
2.473 |
0.116 |
0.965 |
0.923-1.009 |
| SI |
-0.024 |
0.036 |
0.442 |
0.506 |
0.977 |
0.911-1.047 |
| SF |
0.001 |
0.000 |
6.030 |
0.014a |
1.001 |
1-1.002 |
| Alb |
0.111 |
0.071 |
2.426 |
0.119 |
1.118 |
0.972-1.285 |
| PA |
0.000 |
0.003 |
0.006 |
0.937 |
1 |
0.994-1.005 |
| CRP |
0.031 |
0.024 |
1.624 |
0.202 |
1.031 |
0.984-1.081 |
The clinical indicators of COVID-19-infected patients with MHD were compared with those of uninfected patients with MHD during the same period (Table IV). The results revealed some notable differences. Firstly, the lymphocyte count in infected patients was found to be lower than that in uninfected patients. Additionally, infected patients displayed lower levels of blood urea nitrogen, vitamin B12, and prealbumin when compared with uninfected individuals. Furthermore, the present study found that infected patients had higher levels of CRP and serum ferritin compared with uninfected patients. These findings point towards an enhanced inflammatory response in COVID-19 patients as indicated by elevated CRP levels. However, there was no significant difference in the 25(OH)D level between the two groups. Overall, the comparison of clinical indicators between COVID-19 patients and uninfected individuals highlights several important differences, including immune system dysfunction, altered nutrient metabolism, and an exaggerated inflammatory response in infected patients.
 |
Table IV
Comparison of clinical characteristics between patients with maintenance hemodialysis infected and uninfected with COVID-19 during the same period of COVID-19 infection.
|
Table IV
Comparison of clinical characteristics between patients with maintenance hemodialysis infected and uninfected with COVID-19 during the same period of COVID-19 infection.
| Parameter |
COVID-19 (-) (n=82) |
COVID-19 (+) (n=89) |
P-value |
| WBC, 109/l |
9.33±30.26 |
6.08±3.73 |
0.315a |
| Lym, 109/l |
1.21±0.42 |
0.90±0.48 |
0.001a,b |
| Hb, g/l |
114.18±17.50 |
114.55±20.70 |
0.901a |
| Plt, 1012/l |
179.41±60.17 |
161.28±60.23 |
0.051a |
| BUN, mmol/l |
25.00±6.50 |
22.78±6.99 |
0.034a,b |
| Scr, µmol/l |
957.97±218.23 |
907.58±287.20 |
0.201a |
| Ca, mmol/l |
2.18±0.19 |
2.15±0.22 |
0.365a |
| P, mmol/l |
1.73±0.56 |
1.68±0.54 |
0.480a |
| iPTH, pg/ml |
512.60±419.69 |
417.06±361.40 |
0.112a |
| CRP, mg/l |
6.59±10.93 |
33.62±66.36 |
0.001a,b |
| 25(OH)D, ng/ml |
16.95±6.60 |
15.85±7.77 |
0.321a |
| Vitamin B12, pg/ml |
605.29±339.07 |
491.51±227.90 |
0.011a,b |
| Folic acid, ng/ml |
8.02±5.85 |
8.25±6.27 |
0.806a |
| SI, µmol/l |
11.31±4.36 |
11.74±5.17 |
0.576a |
| SF, ng/ml |
390.78±380.56 |
597.95±553.25 |
0.006a,b |
| Alb, g/l |
38.60±2.68 |
38.24±4.38 |
0.524a |
| PA, mg/l |
316.58±81.68 |
279.23±91.22 |
0.006a,b |
Comparison of baseline characteristics was performed between patients with MHD infected with COVID-19 who had succumbed and those who survived (Table V). The findings revealed that out of the total patients studied (n=89), 11 individuals succumbed to the infection while 78 managed to survive. Upon further analysis, it was evident that the deceased patients tended to be significantly older in age compared with the survivors. Additionally, the ferritin levels were found to be significantly higher in the patients who did not survive. Moreover, in comparison, the levels of 25(OH)D and albumin were both significantly lower in the fatal cases. It is important to note that these differences were found to have statistical significance.
 |
Table V
Comparison of baseline characteristics between patients with maintenance hemodialysis infected with COVID-19 who succumbed to disease and those who survived.
|
Table V
Comparison of baseline characteristics between patients with maintenance hemodialysis infected with COVID-19 who succumbed to disease and those who survived.
| Parameter |
Patients who succumbed (n=11) |
Patients who survived (n=78) |
P-value |
| Age, years |
65.55±11.60 |
53.50±14.39 |
0.009a,b |
| Male sex |
9 (81.82) |
55 (70.51) |
0.441c |
| BMI, kg/m2 |
22.31±4.73 |
22.13±4.31 |
0.902a |
| Dialysis vintage, months |
69.00±55.45 |
62.17±43.15 |
0.636a |
| Dialysis frequency, times/week |
2.82±0.40 |
2.92±0.25 |
0.261a |
| Diabetic nephropathy |
9 (81.82) |
16 (20.51) |
0.001c |
| Coronary heart disease |
6 (54.55) |
21 (26.92) |
0.063c |
| WBC, 109/l |
7.17±2.21 |
6.16±1.97 |
0.121a |
| Lym, 109/l |
1.24±0.44 |
1.25±0.41 |
0.951a |
| Hb, g/l |
110.91±15.12 |
114.82±21.96 |
0.570a |
| Plt, 1012/l |
177.82±68.58 |
168.56±62.59 |
0.651a |
| BUN, mmol/l |
23.81±6.85 |
24.17±6.39 |
0.865a |
| Scr, µmol/l |
822.24±227.59 |
937.18±242.98 |
0.143a |
| Ca, mmol/l |
2.11±0.20 |
2.21±0.22 |
0.113a |
| P, mmol/l |
1.75±0.58 |
1.68±0.46 |
0.645a |
| iPTH, pg/ml |
208.08±184.71 |
362.12±277.47 |
0.078a |
| CRP, mg/l |
12.62±14.52 |
7.94±13.27 |
0.282a |
| 25(OH)D, ng/ml |
14.47±4.89 |
22.72±11.06 |
0.001a,b |
| Vitamin B12, pg/ml |
540.36±244.27 |
483.03±235.91 |
0.477a |
| Folic acid, ng/ml |
9.69±7.63 |
9.62±6.87 |
0.978a |
| SI, µmol/l |
12.32±5.00 |
10.71±5.00 |
0.338a |
| SF, ng/ml |
806.18±496.01 |
431.36±413.84 |
0.007a,b |
| Alb, g/l |
36.75±2.89 |
39.11±3.01 |
0.016a,b |
| PA, mg/l |
254.35±71.61 |
295.21±72.22 |
0.084a |
Based on the significant variables identified in Table V, comprehensive multivariate logistic regression analysis was conducted to examine the relationship between various factors and the risk of death in patients with MHD infected with COVID-19. The findings of this analysis revealed that 25(OH)D may be a risk factor for mortality in patients with MHD infected with COVID-19, as indicated in Table VI.
 |
Table VI
Logisitic regression analysis of deceased COVID-19-infected patients with maintenance hemodialysis.
|
Table VI
Logisitic regression analysis of deceased COVID-19-infected patients with maintenance hemodialysis.
| Parameters |
B |
SE |
Wald |
P-value |
OR |
95% CI |
| Age |
0.036 |
0.035 |
1.053 |
0.305 |
1.036 |
0.968-1.109 |
| 25(OH)D |
-0.175 |
0.085 |
4.202 |
0.040a |
0.84 |
0.711-0.992 |
| SF |
0.001 |
0.001 |
3.095 |
0.079 |
1.001 |
1.000-1.003 |
| Alb |
-0.204 |
0.146 |
1.958 |
0.162 |
0.816 |
0.613-1.085 |
Discussion
Epidemiological studies have revealed that the elderly or patients with chronic diseases are more susceptible to COVID-19 and have a higher risk of death (17). In CKD, expression of Toll-like receptors (TLRs) is increased, and phagocytosis is deficient. The number of dendritic cells is reduced, as is the expression of MHC Class I, Class II and costimulatory molecules, resulting in impaired ability to activate T cells (18). The number of naive B cells in patients with CKD is also reduced due to the increased apoptosis rate, leading to impaired humoral immune function (19). These alterations lead to impaired innate and adaptive immune responses in patients with CKD, rendering patients with MHD more susceptible to severe infections. Male sex, age, smoking habits, obesity, elevated D-dimer levels, diabetes, hypertension, chronic obstructive pulmonary disease, malignancies, cardiovascular disease, and CKD have been reported as risk factors associated with a fatal outcome of COVID-19(20).
A total of 171 patients with MHD were included in the present study. The results revealed that the incidence of COVID-19 in patients with MHD was 52.05% (89/171), and the mortality was 6.43% (11/171). The levels of iPTH and folate in the infected patients were significantly lower than those in the uninfected patients, while the levels of CRP and serum ferritin were significantly higher than those in the uninfected patients. Logistic regression analysis revealed that iPTH and serum ferritin were risk factors for COVID-19 in patients with MHD. Tentori et al (21) identified an association between abnormal PTH levels and adverse clinical outcomes. In a study by Hong et al (22), a low serum iPTH level was an independent risk factor for infection-related mortality in incident dialysis patients. However, the pathophysiological mechanisms were not well established. In the aforementioned study, possible mechanisms, such as PTH having a stimulatory function on T lymphocytes, and low iPTH, which may be associated with a decrease in cellular immunity, were suggested. In another study, a low serum iPTH level was associated with malnutrition-inflammation-complex syndrome (23). A low serum iPTH level reflects a state of malnutrition, which may increase infection risk (24). Folate deficiency may have adverse health effects, including suppression of immune function (25). The observation that folate deficiency was associated with a worse outcome in a group of patients with COVID-19 further supports the importance of adequate folate status for COVID-19 prognosis (26). The inflammation-related biomarkers CRP, serum ferritin were elevated in patients with MHD infected with COVID-19, which may reflect the aggravation of the inflammatory response, and although the immune defense of dialysis patients was impaired, they were able to mount an immune response to coronavirus.
The results of the present study revealed that the patients who succumbed to COVID-9 infection were significantly older than those who survived, and the levels of ferritin were significantly higher, while the levels of 25(OH)D and albumin were significantly lower. It was further revealed that 25(OH)D is a risk factor for mortality in patients with MHD infected with COVID-19. Vitamin D is a fat-soluble essential vitamin that plays an important role in the regulation of innate and adaptive immune responses (27). Vitamin D receptors and 1α-hydroxylase are present in a variety of immune cells, including neutrophils, macrophages, and dendritic cells, indicating the effects of vitamin D on the immune system beyond the musculoskeletal system (11). A previous study found that vitamin D reduced the risk of COVID-19 infection and death by regulating the renin-angiotensin system, cellular innate and adaptive immunity, and physical barriers (28). Vitamin D deficiency is common in patients with MHD (29), and low serum 25(OH)D levels are known to be associated with an increased risk of infection and death (30). Low serum albumin may suggest malnutrition, underlying disease, or an infectious process. Albumin can also be used as a reliable indicator for assessing the prognosis of patients with severe COVID-19(31). A previous study on patients with COVID-19 found that hypoalbuminemia was an independent risk factor for mortality, and the risk of death in patients with hypoalbuminemia was 6.394 times higher than that in patients with normal albumin (32).
Important limitations of the present study are that it was a single-center study with a relatively small sample size, and its retrospective design. Missing laboratory data for some patients may have led to bias in clinical characteristics. Therefore, further studies are warranted to better understand the risk factors and prognosis of COVID-19 in patients with MHD and ultimately help guide mortality reduction efforts.
In conclusion iPTH and serum ferritin were revealed to be risk factors for COVID-19 in patients with MHD, and 25(OH)D may be a risk factor for death in patients with MHD infected with COVID-19. According to the findings of the present study, vitamin D supplementation can be provided to patients with MHD who are at high risk of COVID-19 infection or who have been infected with COVID-19 if they have combined vitamin D deficiency or vitamin D insufficiency. However, it is important to note that there is no scientific evidence supporting the use of vitamin D supplementation as a preventive measure, prophylaxis, or to reduce the severity of the disease in individuals with normal blood vitamin D levels.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Natural Science Foundation of Ningxia Province (grant no. 2023AAC03458).
Availability of data and materials
The data generated in the present study are included in the tables of this article.
Authors' contributions
GZ and YZ designed the study. GZ performed the data curation, as well as the preparation and writing of the original draft. DM performed the data collection. BL analyzed and synthesized the data of the study. LB, HL and SC formulated the overarching research goals, reviewed and edited the manuscript and interpreted the data. YZ and DM confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was a single-center, retrospective, observational study. The Medical Ethics Committee of the People's Hospital of Ningxia Hui Autonomous Region approved the study protocol [approval no.(2023)-LL-045]. The present study adhered to the principles of the Declaration of Helsinki.
Patient consent for publication
The patients provided written informed consent for the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing interests.
References
|
1
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gudbjartsson DF, Helgason A, Jonsson H, Magnusson OT, Melsted P, Norddahl GL, Saemundsdottir J, Sigurdsson A, Sulem P, Agustsdottir AB, et al: Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 382:2302–2315. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Allan M, Lièvre M, Laurenson-Schafer H, de Barros S, Jinnai Y, Andrews S, Stricker T, Formigo JP, Schultz C, Perrocheau A and Fitzner J: The World Health Organization COVID-19 surceillance database. Int J Equity Health. 21 (Suppl 3)(S167)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ng JH, Hirsch JS, Wanchoo R, Sachdeva M, Sakhiya V, Hong S, Jhaveri KD and Fishbane S: Northwell COVID-19 Research Consortium and the Northwell Nephrology COVID-19 Research Consortium. Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int. 98:1530–1539. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, et al: Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 323:1574–1581. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, Huet K, Plzak J, Horoi M, Hans S, et al: Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 288:335–344. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hilbrands LB, Duivenvoorden R, Vart P, Franssen CFM, Hemmelder MH, Jager KJ, Kieneker LM, Noordzij M, Pena MJ, de Vries H, et al: COVID-19-related mortality in kidney transplant and dialysis patients: Results of the ERACODA collaboration. Nephrol Dial Transplant. 35:1973–1983. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Popov GT, Baymakova M, Vaseva V, Kundurzhiev T and Mutafchiyski V: Clinical characteristics of hospitalized patients with COVID-19 in Sofia, Bulgaria. Vector Borne Zoonotic Dis. 20:910–915. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Vaziri ND, Pahl MV, Crum A and Norris K: Effect of uremia on structure and function of immune system. J Ren Nutr. 22:149–156. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Khatri M, Islam S, Dutka P, Carson J, Drakakis J, Imbriano L, Jawaid I, Mehta T, Miyawaki N, Wu E, et al: COVID-19 antibodies and outcomes among outpatient maintenance hemodialysis patients. Kidney360. 2:263–269. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Peelen E, Knippenberg S, Muris AH, Thewissen M, Smolders J, Tervaert JW, Hupperts R and Damoiseaux J: Effects of vitamin D on the peripheral adaptive immune system: A review. Autoimmun Rev. 10:733–743. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Drechsler C, Pilz S, Obermayer-Pietsch B, Verduijn M, Tomaschitz A, Krane V, Espe K, Dekker F, Brandenburg V, März W, et al: Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur Heart J. 31:2253–2261. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, et al: Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 356(i6583)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kaufman HW, Niles JK, Kroll MH, Bi C and Holick MF: SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 15(e239252)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Meltzer DO, Best TJ, Zhang H, Vokes T, Arora V and Solway J: Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw Open. 3(e2019722)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Pfaffl MW: A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 29(e45)2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L and Zheng C: Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19). Radiology. 295:715–721. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chiang WF, Hsiao PJ and Chan JS: Vitamin D for recovery of COVID-19 in patients with chronic kidney disease. Front Nutr. 9(930176)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Meier P, Dayer E, Blanc E and Wauters JP: Early T cell activation correlates with expression of apoptosis markers in patients with end-stage renal disease. J Am Soc Nephrol. 13:204–212. 2002.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Barek MA, Aziz MA and Islam MS: Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: A meta-analysis with 55 studies and 10014 cases. Heliyon. 6(e5684)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tentori F, Wang M, Bieber BA, Karaboyas A, Li Y, Jacobson SH, Andreucci VE, Fukagawa M, Frimat L, Mendelssohn DC, et al: Recent changes in therapeutic approaches and association with outcomes among patients with secondary hyperparathyroidism on chronic hemodialysis: The DOPPS study. Clin J Am Soc Nephrol. 10:98–109. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hong YA, Kim JH, Kim YK, Chang YK, Park CW, Kim SY, Kim YS, Kang SW, Kim NH, Kim YL and Yang CW: Low parathyroid hormone level predicts infection-related mortality in incident dialysis patients: A prospective cohort study. Korean J Intern Med. 35:160–170. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dukkipati R, Kovesdy CP, Colman S, Budoff MJ, Nissenson AR, Sprague SM, Kopple JD and Kalantar-Zadeh K: Association of relatively low serum parathyroid hormone with malnutrition-inflammation complex and survival in maintenance hemodialysis patients. J Ren Nutr. 20:243–254. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Fukagawa M, Akizawa T and Kurokawa K: Is aplastic osteodystrophy a disease of malnutrition? Curr Opin Nephrol Hypertens. 9:363–367. 2000.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Topless R, Green R, Morgan SL, Robinson P, Merriman T and Gaffo AL: Folic acid and methotrexate use and their association with COVID-19 diagnosis and mortality: A case-control analysis from the UK Biobank. BMJ Open. 12(e62945)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Itelman E, Wasserstrum Y, Segev A, Avaky C, Negru L, Cohen D, Turpashvili N, Anani S, Zilber E, Lasman N, et al: Clinical characterization of 162 COVID-19 patients in Israel: Preliminary report from a large tertiary center. Isr Med Assoc J. 22:271–274. 2020.PubMed/NCBI
|
|
27
|
Aranow C: Vitamin D and the immune system. J Investig Med. 59:881–886. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Glinsky GV: Tripartite combination of candidate pandemic mitigation agents: Vitamin D, quercetin, and estradiol manifest properties of medicinal agents for targeted mitigation of the COVID-19 pandemic defined by genomics-guided tracing of SARS-CoV-2 targets in human cells. Biomedicines. 8(129)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bhan I, Burnett-Bowie SAM, Ye J, Tonelli M and Thadhani R: Clinical measures identify vitamin D deficiency in dialysis. Clin J Am Soc Nephrol. 5:460–467. 2010.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Nigwekar SU, Bhan I and Thadhani R: Nutritional vitamin D in dialysis patients: What to D-iscern? Nephrol Dial Transplant. 26:764–766. 2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Qin S, Li W, Shi X, Wu Y, Wang C, Shen J, Pang R, He B, Zhao J, Qiao Q, et al: 3044 cases reveal important prognosis signatures of COVID-19 patients. Comput Struct Biotechnol J. 19:1163–1175. 2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Huang J, Cheng A, Kumar R, Fang Y, Chen G, Zhu Y and Lin S: Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J Med Virol. 92:2152–2158. 2020.PubMed/NCBI View Article : Google Scholar
|