Introduction
Coronavirus disease-19 (COVID-19) is caused by
severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and
this disease originally emerged in Wuhan, China in December 2019,
as a cluster of patients with pneumonia (1). A global outbreak of the disease
occurred in the subsequent months, leading to the COVID-19 pandemic
in 2020(2).
Patients with COVID-19 present with a variety of
symptoms, including fever, cough, dyspnea, fatigue, myalgia,
headache, anosmia, nausea, vomiting and diarrhea. The most severe
complications of the disease include pneumonia, acute respiratory
distress syndrome, shock, acute kidney and liver injury,
myocarditis, thromboembolic events and neurological disorders
(3,4). Elderly patients and patients with
underlying conditions, such as hypertension, diabetes and
cardiovascular disease, exhibited an increased risk of developing
severe COVID-19 (3-5).
COVID-19 also exerted a significant effect on the
mental health of patients. During the early stages of the pandemic,
numerous affected countries implemented quarantine measures to
prevent viral spread. However, the subsequent reduction of physical
activity exerted a negative effect on the psychological well-being
of patients (6). Notably, results
of a previous study revealed that adapted physical activity
prevented COVID-19 disease progression and aided in rehabilitation
following the disease, leading to positive psychological outcomes
in patients (7).
During the first year of the pandemic, the number of
patients with COVID-19 that required hospitalization increased, due
to a lack of vaccinations and specific targeted therapies (3,5). As
a result, the COVID-19 pandemic exerted a significant effect on
healthcare systems worldwide (5,8).
Certain countries, such as Italy, were particularly affected by the
disease and the requirement for additional beds in hospitals and
intensive care units was increased (9).
Following the first year of the pandemic, bed
availability for patients with COVID-19 decreased, placing a burden
on healthcare systems. A high percentage of patients admitted to
hospital with COVID-19 exhibited underlying comorbidities that
required prolonged hospitalization and bed requirements continued
to increase until after the severe phase of the disease had passed.
Notably, these patients remained in COVID-19 hospital wards, as a
negative SARS-CoV-2 PCR test result was required for transferal to
a non-COVID-19 hospital ward. The incidence of hospital-acquired
SARS-CoV-2 infection also increased during this period and patients
undergoing surgery were transferred to COVID-19 wards, regardless
of symptom severity. This was also the case for patients with
COVID-19 who were transferred to hospital from other healthcare
locations, such as nursing homes, as they were unable to return to
these without a negative PCR test. Thus, the requirement for
hospital beds for patients with COVID-19 was crucial and the impact
on healthcare systems was evident.
According to Eurostat, Greece accounted for 418
available hospital beds per 10,0000 inhabitants in 2019(10). At the beginning of the COVID-19
pandemic, the Greek Government implemented several measures to
support healthcare systems. These measures included restrictions in
public movement, guidelines outlining the number of days in
quarantine required for patients with COVID-19 and the development
of COVID-19 units. The majority of these units included previous
medical and surgical hospital wards that were dedicated to patients
with COVID-19. Private hospitals were not involved in the care of
hospitalized patients with COVID-19; however, these hospitals
contributed to the care of patients without the disease, through
the provision of beds to support the increasing requirements of
public hospitals.
In the present study, data was obtained from a
middle-step COVID-19 Unit in a secondary care hospital in the
region of Western Attica, between October 2020 and June 2021. The
present study aimed to validate the role of a supportive department
when healthcare systems were under pressure of the COVID-19
pandemic. The present study also aimed to assess the effectiveness
of the middle-step unit, which may exhibit potential in future
pandemics. Thus, patient outcomes, including time to hospital
discharge, referral back to the referring hospital or death and the
length of hospital stay were evaluated. Patient demographics,
comorbidities and clinical characteristics were also examined in
the present study.
Materials and methods
In the region of Western Attica, five central
general hospitals provided wards exclusively for patients with
COVID-19 (Attikon General University Hospital of Athens, General
Hospital of Nikaia, Agios Panteleimon, Asklipieio Voulas General
Hospital, Thriasio General Hospital of Elefsina and Tzaneio General
Hospital of Piraeus). At baseline, 180 hospital beds were provided
and the number of available COVID-19-specific hospital beds was
adjusted according to the number of COVID-19 cases at each
timepoint. Notably, during peaks of the COVID-19 pandemic, a total
of ~420 hospital beds were available in the five reference
hospitals.
To overcome the limited number of COVID-19-specific
hospital beds, a novel middle-step COVID-19 Unit was created in a
secondary care hospital in the region of Western Attica. The
middle-step unit of the Agia Varvara hospital was founded in the
first year of the pandemic and patients with COVID-19 were accepted
and transferred to the Unit, following referrals from COVID-19
wards of the five general hospitals of the region. The rationale
was to support the referral hospitals, through the acceptance of
patients with non-severe COVID-19, patients who could not be
discharged until a quarantine period was completed, or patients
with underlying diseases that could not be transferred to medical
or surgical wards prior to a negative PCR test. Notably, the unit
included new hospital beds and did not include previously existing
wards that had been converted to COVID-19-specific wards. In total,
the unit had a capacity of 35 beds, which increased to 55 during
the peaks of the pandemic. Medical staff working in the unit
consisted of three Consultant Respiratory Physicians, three
Consultant General Internal Medicine Physicians, one Consultant
Cardiologist, one Consultant Surgeon, one Consultant Anesthetist
and three General Internal Medicine Registrars.
Inclusion criteria was as follows: Confirmed
COVID-19 via a SARS-CoV-2 PCR test; at least two days of
hospitalization prior to unit transfer; no signs of progressive
severe COVID-19; and hemodynamic stability with oxygen requirements
of ≤40% fraction of inhaled oxygen (FiO2). Patients with
concomitant underlying conditions that required prolonged
hospitalization following the acute phase of COVID-19 infection,
who also exhibited a positive SARS-CoV-2 PCR test, were also
accepted to the unit. Deteriorating patients that could not be
managed at the unit or in secondary care were referred back to the
original referring hospital.
The protocol of the present study was approved by
the Ethics Committee of Attikon University Hospital (ethics
approval no. 121/03-03-2021) and complied with the guidelines of
the Declaration of Helsinki.
In the current study descriptive statistical
analysis was performed. Categorical variables are presented as n
(%), whereas numerical variables are presented as mean ± standard
deviation or median [interquartile ranges (IQR)] for normally
distributed and skewed data, respectively. In this way data were
present on the median number of days between admission and
discharge from the unit and the number of patients that were
discharged home, returned to the referring hospital or succumbed.
Furthermore, a random sample of 401 patients were examined
regarding Charlson Comorbidity Index (11), frequency of hypertension, diabetes
mellitus, background of coronary artery disease, heart failure,
history of atrial fibrillation, cancer, history of connective
tissue disease, dementia, chronic obstructive pulmonary disease,
asthma and idiopathic pulmonary fibrosis. The present study also
analyzed the prevalence of fever, anosmia, anorexia, cough,
dyspnea, fatigue, headache, diarrhea or other gastrointestinal
symptoms and partial arterial pressure for oxygen/FiO2
on admission in this random sample. Finally, it examined the
incidence of new-onset infection, pulmonary embolism, deep vein
thrombosis, new cardiovascular events, acute kidney injury and
acute liver injury during hospitalization. Data were analyzed using
SPSS 17.0 for Windows (SPSS Inc.).
Results
Between October 2020 and June 2021, the mean weekly
admissions for the five general hospitals in the Western Attica
region was 225 and the mean weekly discharges was 197. The mean
number of admissions per hospital was 98 for the Attikon General
University Hospital of Athens; 51 for the General Hospital of
Nikaia, Agios Panteleimon; 34 for the Asklipieio Voulas General
Hospital; 27 for the Thriasio General Hospital of Elefsina; and 46
for the Tzaneio General Hospital of Piraeus.
In addition, the COVID-19 Unit of the Agia Varvara
Hospital had a total of 631 admissions. The median age of patients
was 69 years (IQR, 56-81) and 316 (50.1%) patients were male. In
total, 83 (13.15%) patients were nursing home residents prior to
hospital admission. All patients were managed and treated according
to the guidelines of the National Public Health Organization
(12). The median number of days
between admission and discharge from the unit was 6 (IQR, 4-13). In
total, 539/631 patients (85.4%) were discharged, 57 patients (9%)
were referred back to the referring hospitals for further
management and 35 patients (5.6%) succumbed (Table I).
 | Table IOverall patient admissions,
discharges, repatriations and deaths at the middle-step COVID-19
Unit in different time periods. |
Table I
Overall patient admissions,
discharges, repatriations and deaths at the middle-step COVID-19
Unit in different time periods.
| Period | Admissions Agia
Varvara Covid-19 Unit | Discharges Agia
Varvara Covid-19 Unit | Repatriations Agia
Varvara Covid-19 Unit | Deaths Agia Varvara
Covid-19 Unit |
|---|
| 10/2020-12/2020 | 146 | 106 | 10 | 14 |
| 01/2021-03/2021 | 293 | 235 | 30 | 11 |
| 04/2021-5/2021 | 192 | 198 | 17 | 10 |
| Total, n (%) | 631 (100.0) | 539 (85.4) | 57 (9.0) | 35 (5.6) |
Data was also obtained from a random sample of 401
patients with COVID-19. The median Charlson Comorbidity Index score
was 4 (IQR, 2-5). In addition, 196 patients (48.9%) had
hypertension, 103 patients (25.7%) had diabetes mellitus, 36
patients (9%) had a background of coronary artery disease, 36
patients (9%) had heart failure, 48 patients (12%) had a known
history of atrial fibrillation, 13 patients (3.2%) had cancer, 8
patients (2%) had a known history of connective tissue disease, 96
patients (23.9%) had dementia, 25 patients (6.2%) had chronic
obstructive pulmonary disease, 18 patients (4.5%) had asthma and
one patient (0.2%) had a known history of idiopathic pulmonary
fibrosis (Table II).
 | Table IIComorbidities of 401 study
participants. |
Table II
Comorbidities of 401 study
participants.
| Variable | Value |
|---|
| Charlson Comorbidity
Indexa | 4 (2-5) |
| Hypertension, n
(%) | 196 (48.9) |
| Diabetes mellitus, n
(%) | 103 (25.7) |
| Coronary artery
disease, n (%) | 36 (9.0) |
| Heart failure, n
(%) | 36 (9.0) |
| Atrial fibrillation,
n (%) | 48 (12.0) |
| Malignancy, n
(%) | 13 (3.2) |
| Connective tissue
disease, n (%) | 8 (2.0) |
| Dementia, n (%) | 96 (23.9) |
| Chronic Obstructive
Pulmonary Disease (COPD), n (%) | 25 (6.2) |
| Asthma, n (%) | 18 (4.5) |
| Idiopathic pulmonary
fibrosis, n (%) | 1 (0.2) |
In addition, 302 patients (75.3%) presented with
fever, nine patients (2.3%) presented with anosmia, 38 patients
(9.5%) presented with anorexia, 138 patients (34.4%) presented with
a cough, 140 patients (34.9%) presented with dyspnea, 109 patients
(27.3%) presented with fatigue, 33 patients (8.3%) presented with a
headache and 72 patients (18%) presented with diarrhea or other
gastrointestinal symptoms. The median
paO2/FiO2 on admission to the COVID-19 Unit
was 328 (IQR, 283-371; Table
III). During hospitalization, 75 patients (18.7%) experienced a
new-onset infection, three patients (0.7%) experienced pulmonary
embolism, two patients (0.5%) experienced deep vein thrombosis, 35
patients (8.7%) experienced new cardiovascular events, 36 patients
(9%) experienced acute kidney injury and three patients (0.7%)
experienced acute liver injury (Table
IV).
 | Table IIIPresenting symptoms of 401 study
participants. |
Table III
Presenting symptoms of 401 study
participants.
| Variable | Value |
|---|
| Fever, n (%) | 302 (75.3) |
| Anosmia, n (%) | 9 (2.3) |
| Anorexia, n (%) | 38 (9.5) |
| Cough, n (%) | 138 (34.4) |
| Dyspnea, n (%) | 140 (34.9) |
| Fatigue, n (%) | 109 (27.3) |
| Headache, n (%) | 33 (8.3) |
| Gastrointestinal
symptoms, n (%) | 72 (18.0) |
|
PaO2/FiO2a | 328 (283-371) |
 | Table IVEvents during hospitalization of 401
study participants. |
Table IV
Events during hospitalization of 401
study participants.
| Variable | Value |
|---|
| New onset infection,
n (%) | 75 (18.7) |
| Pulmonary embolism, n
(%) | 3 (0.7) |
| Deep vein thrombosis,
n (%) | 2 (0.5) |
| Cardiovascular
events, n (%) | 35 (8.7) |
| Acute kidney injury,
n (%) | 36 (9.0) |
| Acute liver injury, n
(%) | 3 (0.7) |
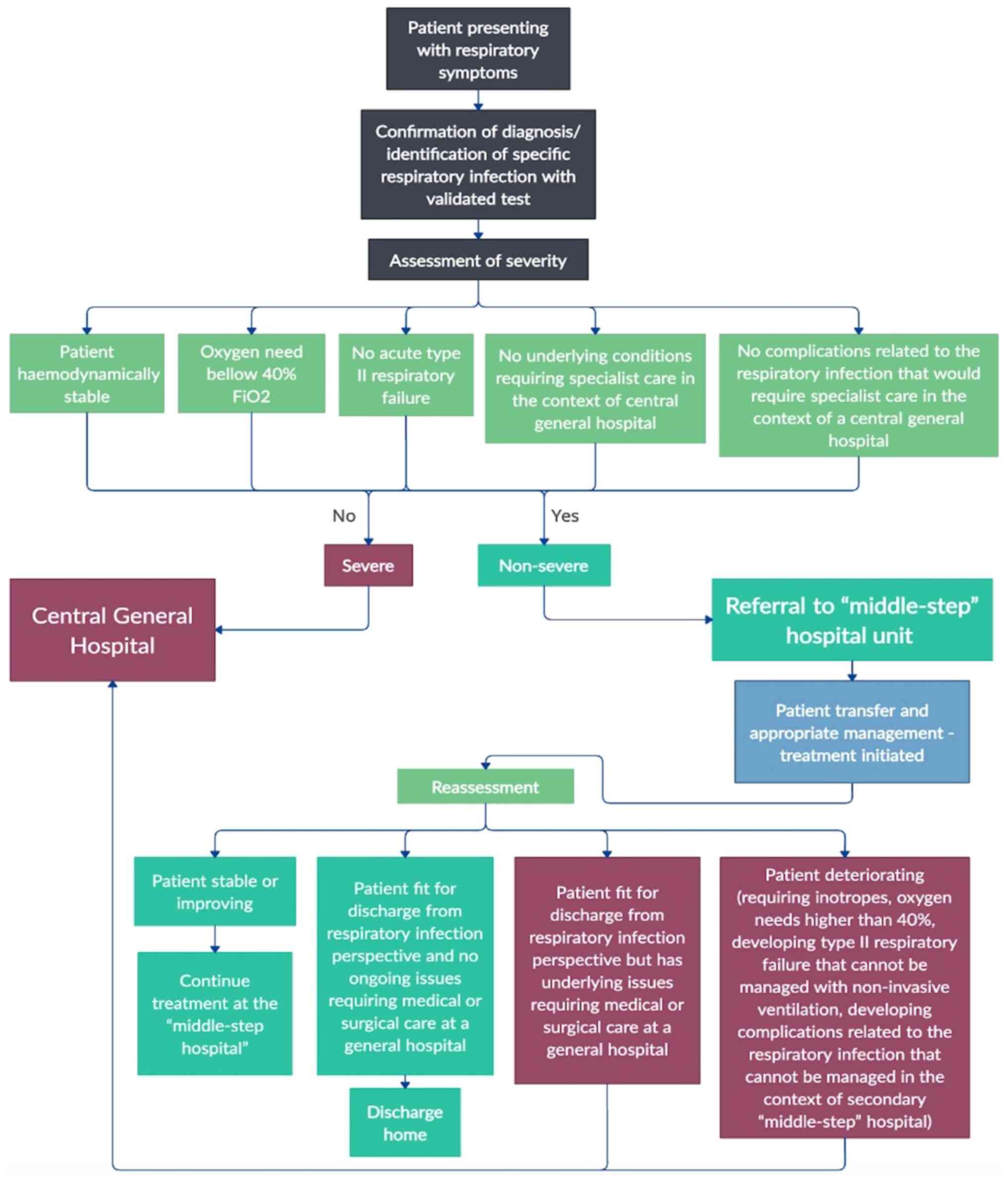
Based on observations of the COVID-19 unit of the
Agia Varvara Hospital during the pandemic, an algorithm for
implementing a middle-step unit was proposed. According to the
algorithm, patients presenting with respiratory symptoms at the
central general hospital should first undergo a validated test to
confirm the diagnosis of the specific respiratory infection.
Following confirmation of respiratory infection, disease severity
should be assessed. Notably, disease severity is assessed according
to hemodynamic stability; a requirement for oxygen of ≤40%
FiO2; acute type II respiratory failure; underlying
conditions requiring specialist care, in the context of a central
general hospital; and complications of respiratory infection that
required specialist care, in the context of a central general
hospital. According to the aforementioned assessment, patients with
severe disease should remain under the care of the central general
hospital. Patients with non-severe disease should be referred to
the middle-step unit. Following patient transferal to the
middle-step unit, appropriate management and treatment will be
initiated. Subsequently, a reassessment of patient status can take
place. If the patient is clinically stable or improving, they will
continue hospitalization in the middle-step unit. If the patient is
fit for discharge and there are no ongoing issues requiring medical
or surgical care at a central general hospital, they will be
discharged. If the patient fit for discharge presents with
underlying conditions that require medical or surgical care at a
central general hospital, they should be referred back to the
central general hospital. If the patient requires inotropes or
oxygen of >40% FiO2, has developed type II
respiratory failure that cannot be managed with non-invasive
ventilation, or has developed complications associated with
respiratory infection that cannot be managed in the context of a
middle-step unit, they will be referred back to the central general
hospital (Fig. 1).
Discussion
In the present study, incorporation of a specialized
middle-step unit contributed to a decrease in workload in the
central general hospitals observed. During peaks of the pandemic
between January and March 2021, the number of available beds and
the number of admissions to the COVID-19 Unit of the Agia Varvara
Hospital were increased by ~2-fold. This increased bed availability
for patients with and without COVID-19 in the central general
hospitals.
Results of the present study demonstrated that the
middle-step unit provided adequate care to patients with a variety
of different backgrounds, comorbidities and symptoms. They also
demonstrated that in patients with COVID-19, hypertension was the
most frequent comorbidity and fever, dyspnoea and cough were the
most frequent symptoms of disease. Notably, these results were
comparable with those observed in previous studies (13,14).
In addition, the length of hospital stay in the middle-step unit
was reduced, compared with results obtained from previous studies
(13,14). However, the acceptance of patients
from central hospitals after at least two days of hospitalization
in the referring hospital may have affected these results.
Notably, the middle-step unit was operating in the
early stages of the pandemic. In this period, specific targeted
treatment options and vaccines were yet to be developed (15,16).
Thus, patient outcomes may not be reflective of the entire duration
of the pandemic. However, results of the present study demonstrated
that incorporation of a middle-step unit may exhibit potential in
future pandemics, when no vaccines or specific targeted treatments
are available.
A previous study discussed proposals for future
pandemics, based on the outcomes of the COVID-19 pandemic, focusing
on therapeutic strategies (17).
An additional previous study examined the efficacy of mobile cabin
hospitals that were opened in public in the early stages of the
pandemic (18). By contrast, the
present study introduced a middle-step unit within secondary care,
with resources, staff and medical supplies readily available. In
addition, mobile cabin hospitals excluded elderly patients and
patients with pre-existing conditions (18). However, the middle-step unit
described in the present study accepted elderly patients and
patients with comorbidities and the proposed algorithm may improve
patient outcomes. Thus, the middle-step unit exhibited potential in
future pandemics.
The present study possessed limitations. Notably,
bed management was observed in the healthcare system of a specific
region, while each healthcare system may possess different dynamics
and resources. However, limited bed availability is often observed
during pandemics. Therefore, the middle-step unit proposed in the
present study exhibited potential as a viable solution to reduce
workload within healthcare systems. In addition, the number of
available beds and daily patient transfers to the unit fluctuated
during different time periods, in accordance with the overall
admissions to hospitals in the region. Notably, the number of
available beds and staff recruitment was adjusted in the unit
during peaks of the pandemic. Patients were also transferred from
central hospitals to the unit using ambulance services. Despite the
requirement for additional resources, the increase in bed
availability for patients with severe infection at the central
hospitals was beneficial.
In conclusion, the middle-step unit exhibited
potential in increasing bed availability and reducing workload
within the healthcare system during peaks of the COVID-19 pandemic.
Thus, the proposed model exhibits potential in reducing healthcare
system workload, supporting specialist management and optimizing
patient outcomes during future pandemics.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Author's contributions
GV, AP, VA, DK, DB, SP, EM and SL contributed to the
conception, drafting and critical revisions of the manuscript. GV,
AP, VA and SL contributed to the acquisition, analysis and
interpretation of data. GV, VA and SL confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of Attikon University Hospital (approval no.
121/03-03-2021) and complied with the guidelines of the Declaration
of Helsinki. Written informed consent was obtained from all
patients included in the present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhu N, Zhang D, Wang W, Li X, Yang B, Song
J, Zhao X, Huang B, Shi W, Lu R, et al: A Novel Coronavirus from
Patients with Pneumonia in China, 2019. N Engl J Med. 382:727–733.
2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sohrabi C, Alsafi Z, O'Neill N, Khan M,
Kerwan A, Al-Jabir A, Iosifidis C and Agha R: World Health
Organization declares global emergency: A review of the 2019 novel
coronavirus (COVID-19). Int J Surg. 76:71–76. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wiersinga WJ, Rhodes A, Cheng AC, Peacock
SJ and Prescott HC: Pathophysiology, transmission, diagnosis, and
treatment of coronavirus disease 2019 (COVID-19): A review. JAMA.
324:782–793. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chams N, Chams S, Badran R, Shams A, Araji
A, Raad M, Mukhopadhyay S, Stroberg E, Duval EJ, Barton LM and Hajj
Hussein I: COVID-19: A multidisciplinary review. Front Public
Health. 8(383)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Maugeri G, Castrogiovanni P, Battaglia G,
Pippi R, D'Agata V, Palma A, Di Rosa M and Musumeci G: The impact
of physical activity on psychological health during Covid-19
pandemic in Italy. Heliyon. 6(e04315)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Maugeri G and Musumeci G: Adapted Physical
Activity to Ensure the Physical and Psychological Well-Being of
COVID-19 Patients. J Funct Morphol Kinesiol. 6(13)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hick JL and Biddinger PD: Novel
coronavirus and old lessons-preparing the health system for the
pandemic. N Engl J Med. 382(e55)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Remuzzi A and Remuzzi G: COVID-19 and
Italy: What next? Lancet. 395:1225–1228. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Eurostat: Hospital beds. https://ec.europa.eu/eurostat/databrowser/product/page/TPS00046.
Last Update July 12, 2020.
|
|
11
|
Charlson ME, Pompei P, Ales KL and
MacKenzie CR: A new method of classifying prognostic comorbidity in
longitudinal studies: Development and validation. J Chronic Dis.
40:373–83. 1987.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chalmers JD, Crichton ML, Goeminne PC, Cao
B, Humbert M, Shteinberg M, Antoniou KM, Ulrik CS, Parks H, Wang C,
et al: Management of hospitalised adults with coronavirus disease
2019 (COVID-19): a European Respiratory Society living guideline.
Eur Respir J. 57:2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Karageorgou V, Papaioannou AI, Kallieri M,
Blizou M, Lampadakis S, Sfika M, Krouskos A, Papavasileiou V,
Strakosha F, Vandorou KT, et al: Patients hospitalised for COVID-19
in periods of Delta and Omicron variant dominance in Greece:
Determinants of severity and mortality. J Clin Med.
12(5904)2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pappas AG, Panagopoulos A, Rodopoulou A,
Alexandrou M, Chaliasou AL, Skianis K, Kranidioti E, Chaini E,
Papanikolaou I and Kalomenidis I: Moderate COVD-19: Clinical
trajectories and Predictors of Progression and Outcomes. J Pers
Med. 12(1472)2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Paraskevis D, Gkova M, Mellou K,
Gerolymatos G, Psalida N, Gkolfinopoulou K, Kostaki EG, Loukides S,
Kotanidou A, Skoutelis A, et al: Real-world Effectiveness of
Molnupiravir and Nirmatrelvir/Ritonavir as Treatments for COVID-19
in patients at high risk. J Infect Dis. 228:1667–1674.
2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Maltezou HC, Basoulis D, Bonelis K,
Gamaletsou MN, Giannouchos TV, Karantoni E, Karapanou A, Kounouklas
K, Livanou ME, Zotou M, et al: Effectiveness of full (booster)
COVID-19 vaccination against severe outcomes and work absenteeism
in hospitalized patients with COVID-19 during the Delta and Omicron
waves in Greece. Vaccine. 41:2343–2348. 2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Li G, Hilgenfeld R, Whitley R and De
Clercq E: Therapeutic strategies for COVID-19: Progress and lessons
learned. Nat Rev Drug Discov. 22:449–475. 2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Shi F, Li H, Liu R, Liu Y, Liu X, Wen H
and Yu C: Emergency Preparedness and Management of Mobile Cabin
Hospitals in China During the COVID-19 Pandemic. Front Public
Health. 9(763723)2022.PubMed/NCBI View Article : Google Scholar
|