Introduction
Anthrax is a statutory class B infectious disease,
an acute zoonotic infectious disease caused by infection with
Bacillus anthracis (1).
Humans are also susceptible and the main sources of infection are
infected animals and their products, as well as contaminated
environments. Bacillus anthracis infection can occur through
multiple routes, such as the respiratory tract, digestive tract,
skin and mucous membranes (2). The
main clinical type is cutaneous anthrax, while other types include
intestinal anthrax and pulmonary anthrax, which can be secondary to
sepsis and meningitis (3). The
case fatality rate associated with cutaneous anthrax is low;
however, the case fatality rate associated with all other types of
anthrax is high (4). The reported
incidence of anthrax in the Shandong province of China remains low
with 1 case of cutaneous anthrax reported in 2010 and 1 case in
2014. In 2021, there were two cases, and there was a common
exposure history of slaughtering sick cattle. The other epidemic
consisted of 13 cases. The source of infection was sick cattle, and
the route of transmission was slaughtering sick cattle, and being
in contact with contaminated equipment and related cattle products.
The patients were mainly engaged in cattle slaughtering or cattle
product collection and sale-related occupations (5). The present study describes one case
of anthrax meningitis admitted to the Second People's Hospital of
Liaocheng (Linqing, China), and the investigative and treatment
strategies applied are also reported.
Case report
In January 2024, a 55-year-old man was admitted to
The Second People's Hospital of Liaocheng (Linqing, China). The
patient presented with a fever, rapid heart rate, rapid breathing,
high blood pressure, fully unconsciousness, and a tense and painful
facial expression. The patient experienced numb limbs and a stiff
neck. According to the laboratory results and MRI examination
results, the initial diagnosis was encephalitis (considering
bacterial or viral infection), and it was necessary to investigate
the cause of coma and hypertension. Following admission, the
patient received treatment with the dehydration drug mannitol at
0.5 g/kg once every 8 h, an acyclovir injection (5 mg/kg, once
every 12 h) against the cold virus, piperacillin sodium/tazobactam
sodium injection (75 mg/kg, once every 6 h) as resistance against
bacterial infection in the central nervous system (according to
clinical experience), dexamethasone injection (10 mg, once a day)
to reduce brain edema, and tracheal intubation, mechanical
ventilation and sputum aspiration; however, the condition of the
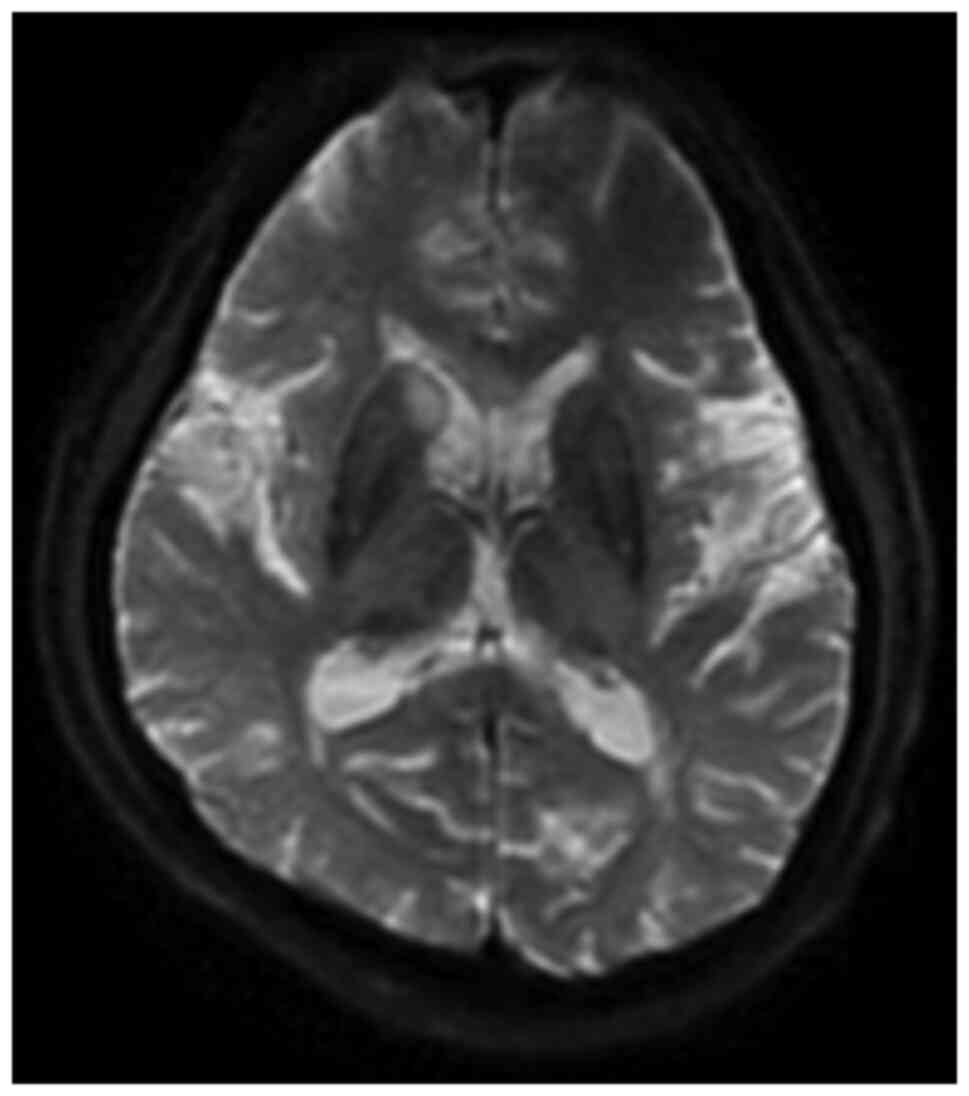
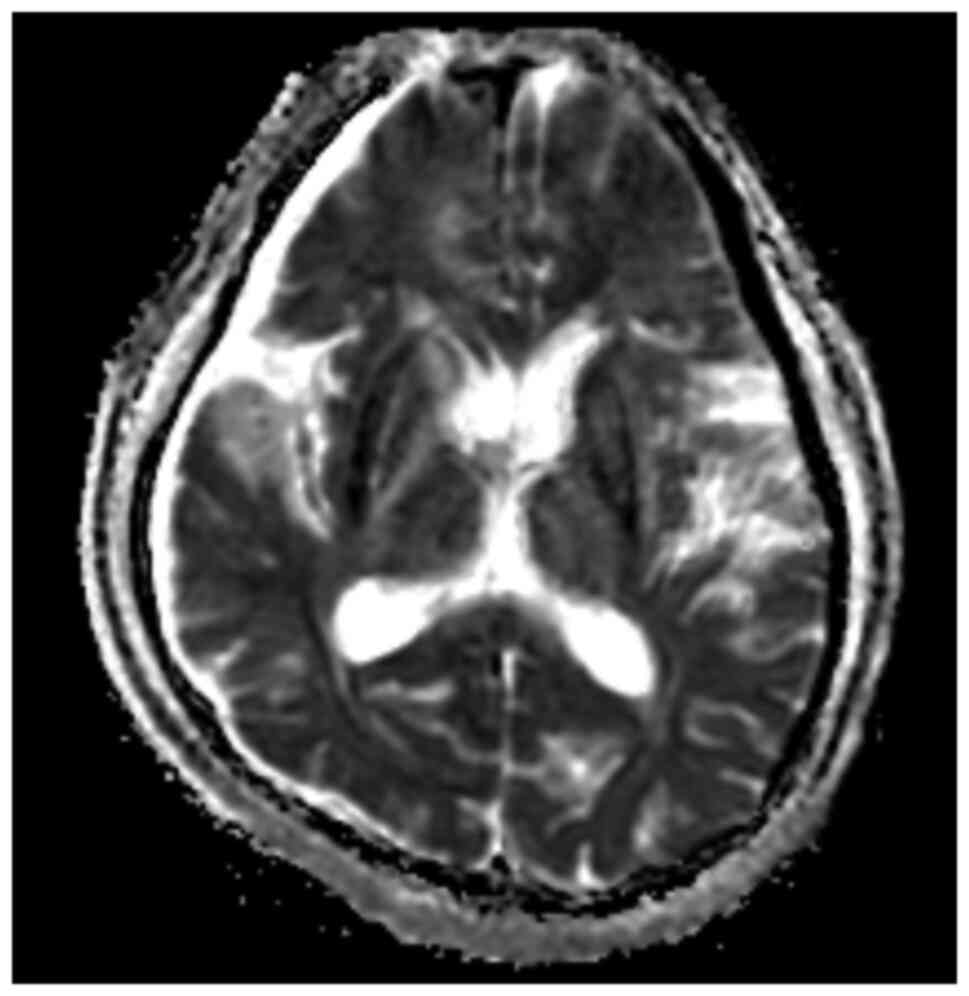
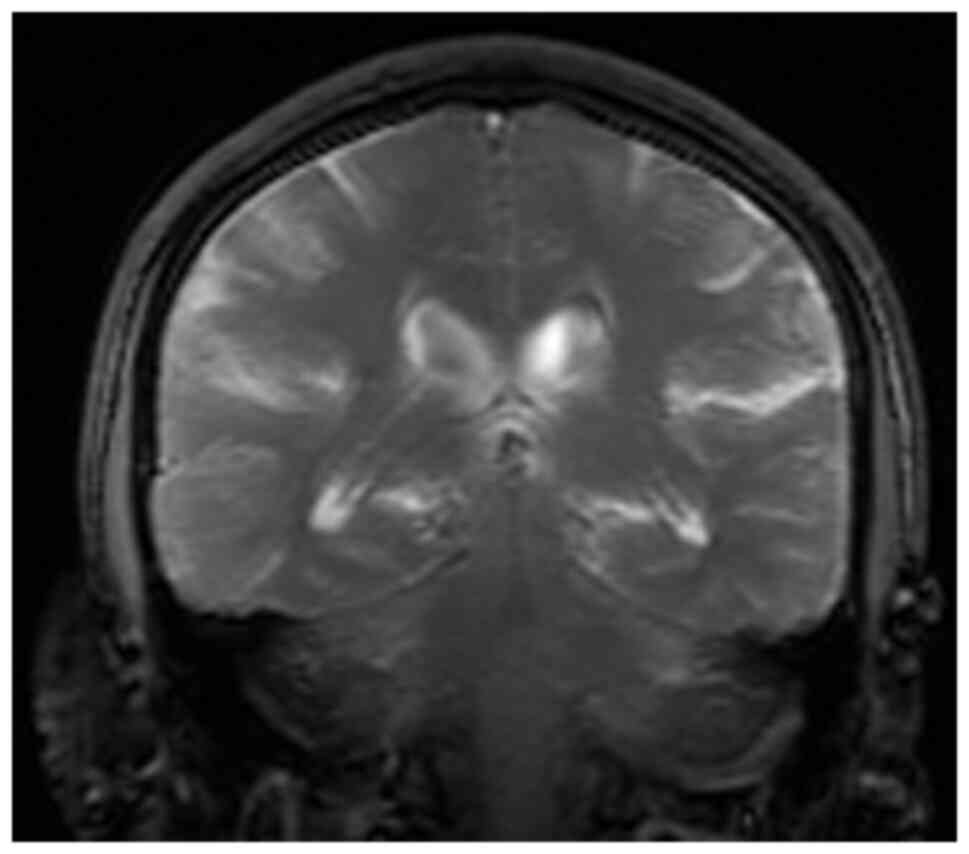
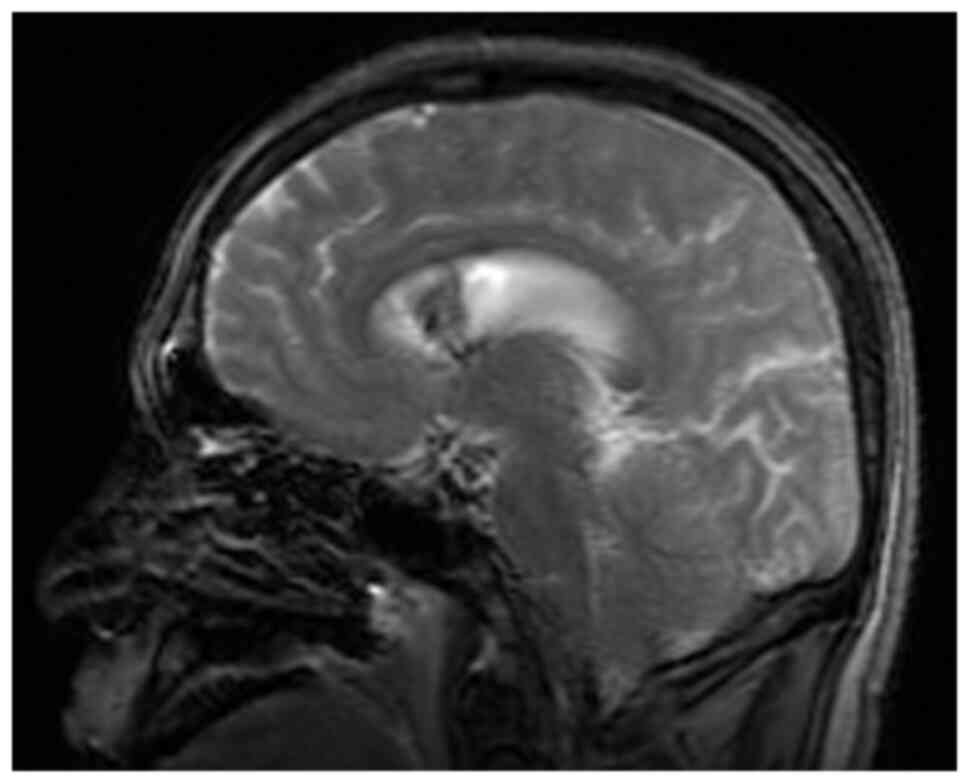
patient did not improve (6). Head
MRI revealed an abnormal signal in the right caudate nucleus and
bilateral hippocampus, indicating encephalitis (Fig. 1, Fig.
2, Fig. 3 and Fig. 4). A brain computed tomography (CT)
scan revealed lacunar infarction (Fig.
5). The MRI findings were consistent with mild cerebral
arteriosclerosis and localized cerebral artery stenosis (7). For ‘bacterial encephalitis’, the
treatment with piperacillin sodium/tazobactam sodium and acyclovir
was terminated, and the more sensitive vancomycin combined with
meropenem was used for anti-infection treatment according to
clinical experience (8).
Cerebrospinal fluid analysis and next generation
sequencing (NGS) of the blood metagenome was performed by Yinfeng
Gene Technology Co., Ltd. A pPathogenic microorganism targeted gene
detection kit was used to prepare DNA/RNA sequencing samples (cat.
no. PT001; Nanjing Practical Medical Inspection Co., Ltd.). The
concentration and purity of DNA and RNA nucleic acids were
determined by Nano-300 micro spectrophotometer (Hangzhou Aosheng
Instrument Co., Ltd.), and the integrity of genomic DNA and genomic
RNA fragments were analyzed by Agilent 2100 biological analyzer
(Agilent Technologies, Inc.). The sequence length was 75 bp and the
direction of sequencing was ‘single end’. The FASTASeq 300
sequencing kit V1.0 (FCH-D SE075-D) (100 cycles; cat. no. S000191;
Shenzhen Zhenmai Biotechnology Co., Ltd.) was used. The final
concentration of the library was 3.6 pM. The data were analyzed by
SJ-tNGS software (version 240829; Nanjing Practical Medical
Inspection Co., Ltd.). The results showed Bacillus anthracis
infection. The number of gene detection sequences in the
cerebrospinal fluid was 83,942, and that in the blood was 41. The
diagnosis of anthrax meningitis and anthracemia was made.
In the patient of the present study, anthrax
meningitis was diagnosed and the patient was immediately isolated
in a separate room without contact. At the same time, the
Department of Infectious Diseases and the Center for Disease
Control and Prevention (Liaocheng, China) were contacted to guide
the treatment, and antibiotic treatment was adjusted to vancomycin
+ meropenem + moxifloxacin combined antibacterial therapy,
according to the 2023 version of the anthrax diagnosis and
treatment plan (9), and the
patient was continued to be treated with dehydration, intracranial
pressure reduction, epilepsy prevention and treatment and brain
protection. Tracing the route of infection, the patient went to a
cattle and sheep butcher's shop 12 days ago to buy mutton to eat
himself. Anthrax was detected on the chopping board of the
butcher's shop. The patient had a history of cerebrospinal fluid
rhinorrhea 5 years ago, a recent history of a cold, sneezing and
nasal discharge, and a high possibility of cerebrospinal fluid
rhinorrhea prior to infection. Following combined antibacterial
therapy, the symptoms were alleviated and combined with the
monitoring of blood, cerebrospinal fluid and sputum bacteria, it
was considered that the patient had meningitis directly caused by
anthrax, and meningitis was the main focus. Considering that the
penetration of vancomycin through the blood-brain barrier is poor
(10), treatment was changed to
the protein synthesis inhibitor linezolid, 600 mg by injection,
every 12 h (11), and the
infection indicators of the treated patient exhibited a downward
trend 3 days later. However, it is not necessary to change the
antibacterial drug to linezolid for the treatment of non-meningitis
anthrax. The anthrax test was weakly positive, and the meropenem
treatment was stopped and downgraded to an intravenous drip of
penicillin at 4 million units twice a day. Combined with linezolid,
at 600 mg by injection every 12 h, and moxifloxacin, at 400 mg by
injection, for antibacterial treatment every day, the condition of
the patient markedly improved and the antimicrobial drug was
gradually downgraded in the later 14 days, and the results of the
cerebrospinal fluid analysis were negative. The biochemical results
of the cerebrospinal fluid 33 days after admission showed the
following: Cerebrospinal fluid protein, 682 mg/l (normal range,
150-450 mg/l); cerebrospinal fluid sugar, 3.68 mmol/l (normal
range, 2.5-4.4 mmol/l) and leukocytes, 29x106/l (normal range,
<5x106/l). The results of routine blood tests showed
white blood cell levels of 8.29x109/l (normal range,
4-10x109/l) and a neutrophil ratio of 66.3% (normal
range, 50-70%). Isolation of the patient was terminated following
multidisciplinary consultation. Subsequently, the antibiotic
infusion was gradually discontinued and the treatment was switched
to single oral moxifloxacin tablets. Following standardized
treatment at the hospital, the symptoms of the patient were
markedly alleviated and they were discharged. Follow-up was
performed once every 2 months after discharge, and the patient is
now left with encephalitis sequela, is occasionally fidgety, has
had a seizure once and occasionally has vague consciousness.
Discussion
Anthrax is persistent and after entering the 21st
century, with the development of animal husbandry and the
acceleration of trade circulation, the disease has exhibited an
upward trend in a number of areas, endangering animals and
threatening human health (10). At
present, the diagnosis and treatment of anthrax meningitis still
encounters significant challenges (11). Early detection, diagnosis and
treatment, as well as the prevention of complications can improve
the prognosis of affected patients (12).
With regard to early detection, the anthrax
infection in the present patient may have been caused by a contact
infection from buying mutton. Patients are exposed to lamb meat
with Bacillus anthracis, which may enter the skull through
the nose or external auditory canal and cause encephalitis. In the
patient described herein, although Bacillus anthracis was
not detected in the nasal cavity or external auditory canal of the
patient, the patient's history of cerebrospinal fluid rhinorrhea
and a history of a ‘cold’ suggest that intracranial infection
through the nasal cavity is highly possible. In this case, anthrax
was detected in the cerebrospinal fluid and through blood genetic
monitoring, and the content of Bacillus anthracis in the
cerebrospinal fluid was ample, which led to the diagnosis of
anthrax meningitis. The patient had been examined at the village
clinic in the early stages of infection and had not received a
clear diagnosis, indicating that the local clinicians did not have
sufficient knowledge of anthrax, which led to the worsening
condition of the patient. Therefore, the local government needs to
formulate an intervention plan to carry out comprehensive
intervention measures focusing on health education for animal
husbandry and animal husbandry workers in the county. In addition,
measures are needed to strengthen the training of medical personnel
at all levels in the identification, diagnosis and treatment of
anthrax on the premise of training in the prevention and control of
emerging infectious diseases, so as to improve the ability of early
identification and diagnosis of infectious diseases. Joint
prevention and control mechanisms are required in order to
strengthen the information exchange between health and agriculture
departments, animal husbandry, market supervision and public
security in order to jointly and effectively prevent and control
zoonotic infectious diseases (13). The next step should be to further
strengthen the construction of laboratories and improve the ability
of case diagnoses and environmental monitoring at the grassroots
level.
Early diagnosis and treatment are mandatory. Anthrax
meningitis has a rapid onset, mainly with sudden fever, fatigue,
dizziness, nausea, vomiting, agitation, seizures, delirium and
meningeal irritation (13). The
normal white blood cell count in adult peripheral blood is
4-10x109/l, while that of anthrax patients is increased,
usually at 10-20x109/l, but reaching as high as
60-80x109/l, and is mainly composed of neutrophils
(14). Certain patients have
thrombocytopenia. For an etiological and serological examination,
specimens of blister fluid, blood, cerebrospinal fluid, pleural
effusion and secretions can be collected for testing: i) Bacterial
smear: Under the microscope, gram-positive crude bacilli were
arranged in series (15); ii)
bacterial culture: The collected specimens are inoculated in
nutrient agar medium and Bacillus anthracis can be cultured;
iii) nucleic acid detection: PCR or quantitative PCR detect the
specific nucleic acid of Bacillus anthracis and the results
are positive; iv) antigen detection: Bacillus anthracis
antigen detection can be performed by immunochromatography;
however, a negative result cannot rule out anthrax; v) antibody
detection: ELISA and immunochromatography can detect antibodies to
blood anthrax toxin antigens and capsular antibodies.
The differential diagnosis of anthrax meningitis
includes subarachnoid or intracerebral hemorrhage, bacterial or
aseptic meningitis and viral encephalitis; MRI, which was applied
in the present case, can easily identify hemorrhagic
meningoencephalitis and subarachnoid or intracerebral hemorrhages
(16). To distinguish between
other hemorrhagic or non-hemorrhagic meningoencephalitis, Gram
staining and cultures of the cerebrospinal fluid (17), which were applied in the present
case, need to be performed. In cases of subarachnoid hemorrhages,
headaches, nausea and vomiting may occur, and meningeal irritation
may be present. Cranial CT scans (18), which were applied in the present
case, or MRI may indicate subarachnoid hemorrhage, and the lumbar
puncture examination of cerebrospinal fluid (19), which was applied in the present
case, may reveal homogeneous bloody cerebrospinal fluid. Epidemic
meningitis is acute purulent meningitis caused by meningococcal
bacteria, and its clinical presentation and cerebrospinal fluid
characteristics are similar to those of anthrax meningitis;
however, it can be distinguished by etiological testing (20). For instance, common bacteria, such
as Staphylococcus aureus and Escherichia coli can
also cause bacteremia, and the culture and identification of these
bacteria are essential for the differential diagnosis (21). In addition, knowledge of the
medical and epidemiological history of the patient is also a key
reference for the differential diagnosis. Anthracemia is usually
secondary to severe infections, such as cutaneous, enteral or
pulmonary anthrax; thus, an investigation to identify any possible
history of exposure or medical history can aid doctors in
determining whether a person may be infected with Bacillus
anthracis (22).
Anthrax meningitis should also be differentiated
from rhinosinusal aspergilloma: Common complaints are nasal
congestion, a runny nose and olfactory dysfunction. Unilateral and
persistent headache, trigeminal neuralgia and unilateral scabs are
strong clinical indicators. An endoscopic examination reveals
obvious edema or middle nasal polyps. Imaging reveals unilateral
maxillary-ethmoidal sinus injury with hyperosteogeny, calcification
in the maxillary sinus wall and sinus and obstruction of
bone-phlegm complex. The imaging lesions of aspergilloma include
the dissolution of aspergilloma and the bone wall of the maxillary
sinus, particularly the bone wall of the medial wall, orbital floor
and bone septum. A high-resolution CT scan can emphasize erosion.
An MRI can also be used to describe tumor obstruction secondary to
fluid retention in the sinus cavity. The most common eye and orbit
complications are accompanied by orange peel-like tissue in the
orbital sinus, particularly severe nosebleeds, severe headaches,
possible fever and systemic damage (23).
For anthrax, general treatment includes the
following: Strict isolation, bed rest, appropriate fluid
replacement to maintain water and electrolyte balance in patients
with vomiting, diarrhea and difficulty eating, the appropriate
management of hemorrhage, shock and neurological symptoms, and
hormonal therapy in patients with severe edema or meningitis
(24).
Regarding the treatment of pathogens, Bacillus
anthracis is susceptible to β-lactams (penicillin,
carbapenems), aminoglycosides, macrolides, fluoroquinolones,
tetracyclines, glycopeptides, lincosamides, rifamycins and
oxazolidinones, but not to cephalosporins and sulfonamides
(25). For anthrax with sepsis and
with severe edema, two or more antimicrobial agents active against
Bacillus anthracis should be administered, at least one of
which has bactericidal activity (26). The first-line regimen is
ciprofloxacin and alternative options are levofloxacin,
moxifloxacin, meropenem, imipenem, vancomycin, penicillin G and
ampicillin (27). At least one
other agent is a protein synthesis inhibitor (clindamycin or
linezolid as a first-line regimen; doxycycline or rifampicin as
alternatives) (28). Anthrax
meningitis is treated with at least three antimicrobial agents
active against Bacillus anthracis (29). At least one of them is a fungicide
(fluoroquinolone or β-lactam) and at least one is a protein
synthesis inhibitor; all antimicrobials should have good central
nervous system penetration (30).
Fluoroquinolone antimicrobials include ciprofloxacin [400 mg
intravenously (i.v.) every 8 h] as a first-line option;
levofloxacin (750 mg i.v. once a day) or moxifloxacin (400 mg i.v.
once a day) as alternatives (31).
β-lactam antimicrobials include meropenem (2 g i.v. every 8 h) as a
first-line option; penicillin G (4 million units i.v. every 4 h)
and ampicillin (3 g i.v. every 6 h) are alternatives (32). Protein synthesis inhibitors include
linezolid (600 mg i.v. every 12 h) as a first-line option and
clindamycin (900 mg i.v. every 8 h), vancomycin [60 mg/(kg d),
administered in three divided doses, maintain serum trough
concentration 15-20 mg/l], rifampicin (600 mg i.v. every 12 h) and
chloramphenicol (1 g i.v. every 8-6 h) (33). Due to poor central nervous system
permeability, doxycycline should not be used as a protein synthesis
inhibitor in patients with meningitis (34).
Patients can be discharged after the clinical
symptoms have subsided and their secretions or excretions are
negative for two consecutive bacterial cultures or nucleic acid
tests (24 h apart). Anthrax meningitis has a mortality rate of
almost 100% and is a complication of anthrax exposure. Meningitis
can be primary (i.e., no obvious route of transmission) or
secondary (i.e., complications of any other form of anthrax).
Meningitis occurs in 14-37% of patients infected with anthrax via
injection, ingestion, the systemic cutaneous route or via
inhalation, depending on the route of transmission (3). Therefore, all patients with signs or
symptoms of systemic disease need to be evaluated for meningitis.
In the clinical diagnosis and treatment, the positive rate of
traditional cerebrospinal fluid culture is not high, and the
special flora is not easy to culture, while cerebrospinal fluid
gene detection covers a wide range. In the case of the present
study, no bacteria were detected in the cerebrospinal fluid culture
and the results of cerebrospinal fluid and blood metagenomic
sequencing (NGS) in the early stage revealed infection with
Bacillus anthracis, and pathogen-specific treatment was
administered: Fluoroquinolone antimicrobials, β-lactam
antimicrobials and protein synthesis inhibitors were combined for
antibacterial therapy. The treatment effect was satisfactory and
the anthrax culture was negative; thus, the antimicrobial drug was
gradually tapered and the condition of the patient improved and he
was discharged from the hospital.
In terms of the prevention of epidemics, studies
have shown that the public's awareness of epidemic prevention may
determine the probability of an anthrax epidemic in humans;
strengthening the conveyance of anthrax knowledge may be the key
measure to prevent and control an epidemic (35). It has been suggested that the
health education of farmers and herdsmen on anthrax prevention and
control should be strengthened as soon as possible, so that
herdsmen can develop the hygienic concept and behavior of ‘not
slaughtering, dissecting and not eating sick and dead livestock’
(36). Animal husbandry and
veterinary departments shall strengthen grassroots technical forces
and legal publicity measures, and strengthen the monitoring of
epidemic situations among animals. Immediately following an
outbreak of inter-livestock anthrax, the trading market should be
closed. The dead livestock should be properly handled, such as the
incineration or deep burial of livestock that have died of the
disease, so as to control the spread of the inter-livestock
epidemic as soon as possible, and fundamentally cut off the
transmission route, in order to avoid the occurrence of human
epidemics (37). In this outbreak,
due to the fact that the patient described herein and his family
did not understand the dangers of anthrax and the village doctor
was not highly vigilant, it was not possible to make a positive
diagnosis and perform treatment at an early stage. Therefore,
strengthening the professional knowledge training of county,
township (town) health centers and village doctors, and improving
their clinical diagnosis and treatment capabilities should be the
focus of medical and health work in agricultural and pastoral areas
in the future.
The present case report has certain limitations,
which should be mentioned. First, it only describes one case, and
this disease is known to appear in a number of forms. In addition,
the patient came to the hospital for reexamination regularly, but
the follow-up period after discharge was only 7 months.
In conclusion, anthrax meningoencephalitis is a rare
central nervous system complication of anthrax, which progresses
rapidly following the onset of the disease; timely treatment needs
to be administered in order to prevent the high disability and
mortality rates associated with his type of infection. Early
detection, early diagnosis and early treatment are of particular
importance for patients with anthrax meningoencephalitis and
strengthening epidemic prevention is also a key task. The present
study shares the diagnosis and treatment of a case of anthrax
meningitis with an aim to provide experience and advice regarding
anthrax prevention and treatment.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
KL and LZ conceived and designed the study. ZC and
XY analyzed and summarized the data and wrote the manuscript. KL,
ZC and LZ collected the laboratory examination data and MRI images
of the case. XY critically revised the manuscript. KL and LZ
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was conducted in accordance with the
principles expressed in the Declaration of Helsinki.
Patient consent for publication
The patient involved in the present study was
subjected to standard clinical practice and provided written
informed consent for the publication of medical data and
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tschopp R and Kidanu AG:
Knowledge-attitude and practice of Anthrax and brucellosis:
Implications for zoonotic disease surveillance and control in
pastoral communities of Afar and Somali region, Ethiopia. PLoS Negl
Trop Dis. 18(e0012067)2024.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Nana SD, Caffin JH, Duboz R,
Antoine-Moussiaux N, Binot A, Diagbouga PS, Hendrikx P and Bordier
M: Towards an integrated surveillance of zoonotic diseases in
Burkina Faso: The case of anthrax. BMC Public Health.
22(1535)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bradley JS, Bulitta JB, Cook R, Yu PA,
Iwamoto C, Hesse EM, Chaney D, Yu Y, Kennedy JL, Sue D, et al:
Central nervous system antimicrobial exposure and proposed dosing
for anthrax meningitis. Clin Infect Dis. 78:1451–1457.
2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Blackburn JK, Kenu E, Asiedu-Bekoe F,
Sarkodie B, Kracalik IT, Bower WA, Stoddard RA and Traxler RM: High
case-fatality rate for human anthrax, Northern Ghana, 2005-2016.
Emerg Infect Dis. 27:1216–1219. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang EM, Zhang HJ, He JR, Li W and Wei
JC: Analysis of epidemic characteristics of anthrax in China from
2017 to 2019 and molecular typing of Bacillus anthracis. Zhonghua
Yu Fang Yi Xue Za Zhi. 56:422–426. 2022.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
6
|
Caffes N, Hendricks K, Bradley JS,
Twenhafel NA and Simard JM: Anthrax meningoencephalitis and
intracranial hemorrhage. Clin Infect Dis. 75 (Suppl 3):S451–S458.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhou G, Wang H, Zhang X, Yu L, Yao F, Li B
and Fang Q: Cerebral arteriosclerosis stenosis predicts poor
short-term prognosis in non-valvular atrial fibrillation related
cardioembolic stroke treated by reperfusion therapy. Clin Neurol
Neurosurg. 207(106738)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gozdas HT, Dogan A, Wright H and Fox-Lewis
A: Laboratory findings in acute bacterial meningitis and acute
viral encephalitis. N Z Med J. 137:103–104. 2024.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bhattacharya D, Kshatri JS, Choudhary HR,
Parai D, Shandilya J, Mansingh A, Pattnaik M, Mishra K, Padhi SP,
Padhi A and Pati S: One Health approach for elimination of human
anthrax in a tribal district of Odisha: Study protocol. PLoS One.
16(e0251041)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zhang H, Zhang E, Guo M, He J, Li W and
Wei J: Epidemiological characteristics of human Anthrax - China,
2018-2021. China CDC Wkly. 4:783–787. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kutmanova A, Zholdoshev S, Roguski KM,
Sholpanbay Uulu M, Person MK, Cook R, Bugrysheva J, Nadol P,
Buranchieva A, Imanbaeva L, et al: Risk factors for severe
cutaneous anthrax in a retrospective case series and use of a
clinical algorithm to identify likely meningitis and evaluate
treatment outcomes, kyrgyz republic, 2005-2012. Clin Infect Dis. 75
(Suppl 3):S478–S486. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Thompson JM, Cook R, Person MK, Negrón ME,
Traxler RM, Bower WA and Hendricks K: Risk factors for death or
meningitis in adults hospitalized for cutaneous anthrax, 1950-2018:
A systematic review. Clin Infect Dis. 75 (Suppl 3):S459–S467.
2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sidwa T, Salzer JS, Traxler R, Swaney E,
Sims ML, Bradshaw P, O'Sullivan BJ, Parker K, Waldrup KA, Bower WA
and Hendricks K: Control and Prevention of Anthrax, Texas, USA,
2019. Emerg Infect Dis. 26:2815–2824. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ben-Shmuel A, Glinert I, Sittner A,
Bar-David E, Schlomovitz J, Levy H and Weiss S: Doxycycline,
levofloxacin, and moxifloxacin are superior to ciprofloxacin in
treating anthrax meningitis in rabbits and NHP. Antimicrob Agents
Chemother: Apr 30, 2024 (Epub ahead of print).
|
|
15
|
Wicky PH, Poiraud J, Alves M, Patrier J,
d'Humières C, Lê M, Kramer L, de Montmollin É, Massias L,
Armand-Lefèvre L and Timsit JF: Cefiderocol treatment for severe
infections due to difficult-to-treat-resistant non-fermentative
Gram-Negative Bacilli in ICU patients: A case series and narrative
literature review. Antibiotics (Basel). 12(991)2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhou ZM, Gu LL, Zhou ZY and Liang QL:
Recent Advance of S100B proteins in spontaneous intracerebral
hemorrhage and aneurysmal subarachnoid hemorrhage. Front Biosci
(Landmark Ed). 29(37)2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bobinger T, Roeder SS, Spruegel MI,
Froehlich K, Beuscher VD, Hoelter P, Lücking H, Corbeil D and
Huttner HB: Variation of membrane particle-bound CD133 in
cerebrospinal fluid of patients with subarachnoid and intracerebral
hemorrhage. J Neurosurg. 134:600–607. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhao X, Zhou B, Luo Y, Chen L, Zhu L,
Chang S, Fang X and Yao Z: CT-based deep learning model for
predicting hospital discharge outcome in spontaneous intracerebral
hemorrhage. Eur Radiol. 34:4417–4426. 2024.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Conklin J and Lev MH: Beyond the AJR:
Intracranial CTA versus lumbar puncture for suspected subarachnoid
hemorrhage with negative head CT. AJR Am J Roentgenol: Jul 17, 2024
(Epub ahead of print).
|
|
20
|
Li JH, Wu D, Yin ZD and Li YX: Analysis of
epidemic characteristics for meningococcal meningitis in China
during 2015-2017. Zhonghua Yu Fang Yi Xue Za Zhi. 53:159–163.
2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
21
|
Bita Fouda AA, Latt A, Sinayoko A,
Mboussou FFR, Pezzoli L, Fernandez K, Lingani C, Miwanda B, Bulemfu
D, Baelongandi F, et al: The bacterial meningitis epidemic in
banalia in the democratic republic of congo in 2021. Vaccines
(Basel). 12(461)2024.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhai LN, Zhao Y, Song XL, Qin TT, Zhang
ZJ, Wang JZ, Sui CY, Zhang LL, Lv M, Hu LF, et al: Inhalable
vaccine of bacterial culture supernatant extract mediates
protection against fatal pulmonary anthrax. Emerg Microbes Infect.
12(2191741)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vrinceanu D, Dumitru M, Patrascu OM,
Costache A, Papacocea T and Cergan R: Current diagnosis and
treatment of rhinosinusal aspergilloma (Review). Exp Ther Med.
22(1264)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Beliveau M, Rubets I, Bojan D, Hall C,
Toth D, Kodihalli S and Kammanadiminti S: Animal-to-Human dose
translation of ANTHRASIL for treatment of inhalational anthrax in
healthy adults, obese adults, and pediatric subjects. Clin
Pharmacol Ther. 115:248–255. 2024.PubMed/NCBI View
Article : Google Scholar
|
|
25
|
Doganay M, Dinc G, Kutmanova A and Baillie
L: Human Anthrax: Update of the diagnosis and treatment.
Diagnostics. 13(1056)2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Person MK, Cook R, Bradley JS, Hupert N,
Bower WA and Hendricks K: Systematic review of hospital treatment
outcomes for naturally acquired and bioterrorism-related anthrax,
1880-2018. Clin Infect Dis. 75 (Suppl 3):S392–S401. 2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Bower WA, Yu Y, Person MK, Parker CM,
Kennedy JL, Sue D, Hesse EM, Cook R, Bradley J, Bulitta JB, et al:
CDC guidelines for the prevention and treatment of anthrax, 2023.
MMWR Recomm Rep. 72:1–47. 2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Matharoo K, Chua J, Park JR, Ingavale S,
Jelacic TM, Jurkouich KM, Compton JR, Meinig JM, Chabot D,
Friedlander AM and Legler PM: Engineering an Fc-Fusion of a capsule
degrading enzyme for the treatment of anthrax. ACS Infect Dis.
8:2133–2148. 2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lin C, Dou X, Zhang D, Sun Y, Han H, Chen
C, Zhang X, Li S, Chen Y, Zhang H, et al: Epidemiological
Investigation of an Inhalational Anthrax Patient Traveling for
Medical Treatment in Beijing Municipality, China, August 2021.
China Cdc Wkly. 4:4–7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Hesse EM, Godfred-Cato S and Bower WA:
Antitoxin use in the prevention and treatment of anthrax disease: A
systematic review. Clin Infect Dis. 75 (Suppl 3):S432–S440.
2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Aktories K: Treatment of ovarian cancer
with modified anthrax toxin. Proc Natl Acad Sci USA.
119(e2210179119)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Martchenko Shilman M, Bartolo G, Alameh S,
Peterson JW, Lawrence WS, Peel JE, Sivasubramani SK, Beasley DWC,
Cote CK, Demons ST, et al: In vivo activity of repurposed
amodiaquine as a host-targeting therapy for the treatment of
anthrax. ACS Infect Dis. 7:2176–2191. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Legler PM, Little SF, Senft J, Schokman R,
Carra JH, Compton JR, Chabot D, Tobery S, Fetterer DP, Siegel JB,
et al: Treatment of experimental anthrax with pegylated circularly
permuted capsule depolymerase. Sci Transl Med.
13(eabh1682)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Jauro S, Ndumnego OC, Ellis C, Buys A,
Beyer W and Heerden HV: Immunogenicity and protective efficacy of a
non-living anthrax vaccine versus a live spore vaccine with
simultaneous penicillin-G treatment in cattle. Vaccines (Basel).
8(595)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Oh J, Jo H, Park J, Lee H, Kim HJ, Lee H,
Kang J, Hwang J, Woo S, Son Y, et al: Global burden of
vaccine-associated rheumatic diseases and their related vaccines,
1967-2023: A comprehensive analysis of the international
pharmacovigilance database. Int J Rheum Dis.
27(e15294)2024.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Schneider SN, Nguyen TQ, Hake KL,
Nightingale BS, Mangan TP, Rice AN and Carroll JC: Development of a
pharmacy point-of-dispensing toolkit for anthrax post-exposure
prophylaxis for allegheny county postal workers. J Public Health
Manag Pract. 30:231–239. 2024.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Li S, Ma Q, Chen H, Liu Y, Yao G, Tang G
and Wang D: Epidemiological investigation and etiological analysis
of a cutaneous anthrax epidemic caused by Butchering Sick Cattle in
Guizhou, China. Front Public Health. 8(65)2020.PubMed/NCBI View Article : Google Scholar
|