Introduction
Xanthogranulomatous endometritis (XE) is a rare,
histiocyte-rich and inflammatory disease that may affect the
endometrium, mimicking malignancy, with <25 cases reported to
date (1-3).
XE is a histopathologically benign entity characterized by
inflammatory cell infiltration and foamy macrophages (1). The mean age of presentation is 72
years and vaginal discharge is the most common presentation
(1). Malakoplakia (MP) rarely
involves the female genital tract with <40 reported cases up to
2021(4) and the vagina being the
most affected site (4). Although
the etiology of MP is generally considered to be non-specific,
immune suppression through conditions such as diabetes has been
documented to contribute in numerous reported cases (5-8).
The mean age of presentation is 66 years (2) and vaginal bleeding is reported as the
most common presentation (4).
However, histopathological samples are frequently positively
stained with von Kossa special stain and have pathognomonic
Michaelis-Gutmann bodies (4,5). MP
is rare and the knowledge remains limited, for which there are no
established treatment methods. Antibiotics and surgical resection
are considered to be optimal for the treatment of this disease
(4,5).
Rosai-Dorfman disease (RDD) is another non-common
benign idiopathic disease, with a prevalence of 1 in
200,000(9), that rarely involves
the female genital tract (10,11).
RDD commonly affects the lymph nodes but could be extranodal and
affect the skin, bones and orbital tissues as common sites
(11). The affected tissue is
typically positively stained with S100, CD68 and CD163, whilst
negatively staining for CD1a and Langerin (CD207) (10,11).
To the best of our knowledge, the co-existence of MD and RDD in the
same patient has never been reported. The present study reported
the unique existence of disease entities that could be mistaken for
malignancy and that a targeted histopathological diagnosis would
facilitate handling of unexpected outcomes.
Case report
A 66-year-old multiparous, with type 2 diabetes,
hypertensive woman who previously had no surgical operations,
presented to the Specialty Hospital (Amman, Jordan) in February
2023 with recurrent episodes of post-menopausal bleeding over a
1-year period. Physical examination revealed a normal body mass
index of 27 kg/m2 and lower abdominal tenderness. A
transvaginal ultrasound scan (images not captured) showed a bulky
uterus, an abnormal endometrial thickness of 8 mm and no adnexal
masses or free fluid in the pelvis. A cervical smear was collected
and the result was normal with no cytological indicators of
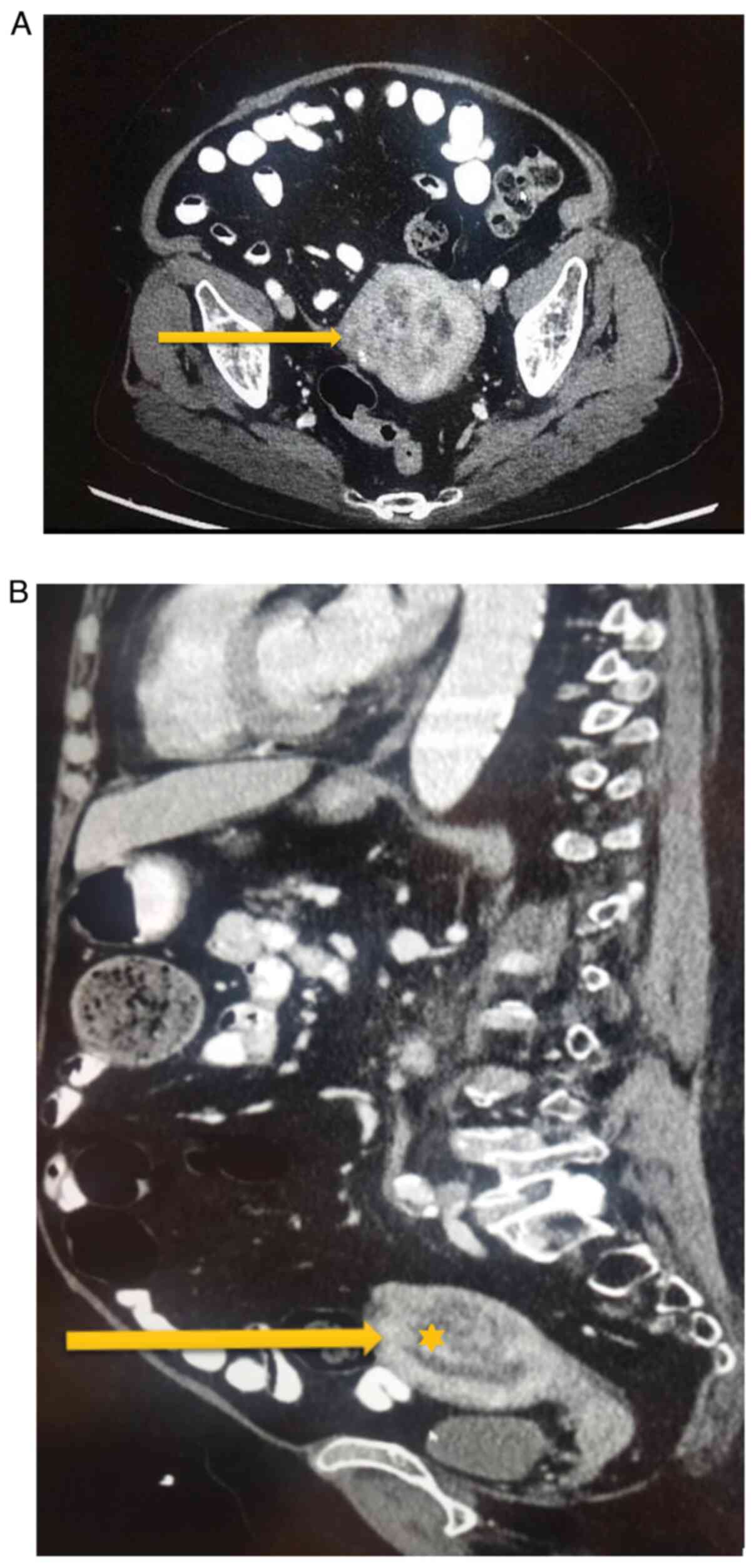
cancerous/pre-cancerous lesions. Furthermore, an abdominopelvic CT
scan was performed to identify any possible other types of lesions.
The results showed a heterogeneous lesion occupying the posterior
wall of the uterus involving two-thirds of the myometrium measuring
5.0x4.5x4.0 cm, compressing the endometrial cavity, with few
retroperitoneal lymph nodes and no pelvic free fluid (Fig. 1A and B).
An endometrial biopsy was collected by dilatation
and curettage and the tissue was processed for histological
analysis. The tissue was fixed in 10% formalin at room temperature
for 24 h, cut at a 5-µm thickness, stained with Harris H&E and
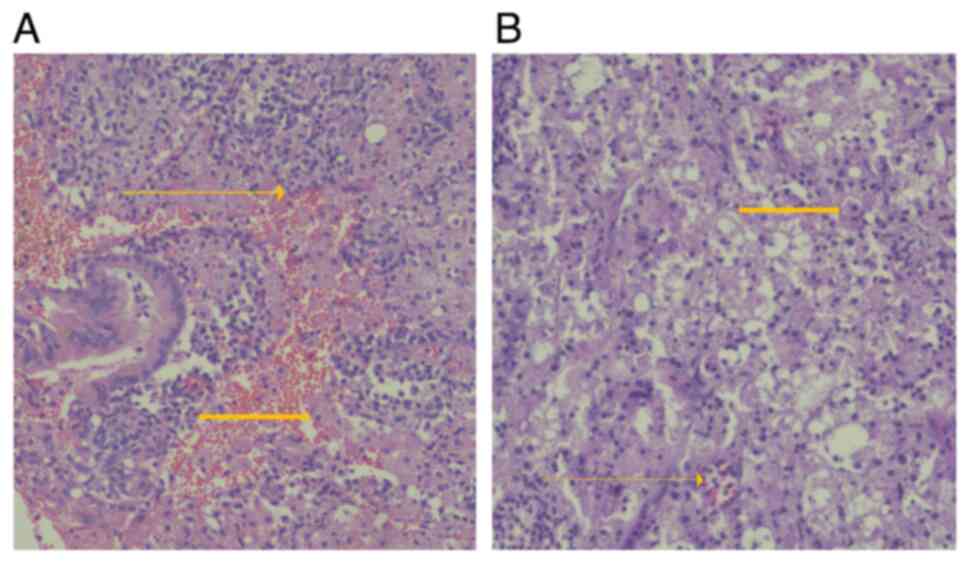
observed under a light microscope. The histopathology results
showed abundant inflammatory foamy histiocytes and chronic
inflammatory cells (multinucleated giant cells formed from
macrophage fusion), with no evidence of malignancy. The findings
were suggestive of XE (Fig.
2A).
Considering the recurrence of postmenopausal
bleeding and the results of histopathology being indicative of XE
mimicking malignancy in it's presentation, a total abdominal
hysterectomy and bilateral salpingo-oophorectomy (TAH + BSO) were
performed at the Specialty Hospital with the consent of the
patient. Intraoperative findings showed a 10-week size uterus (10
cm) and no evidence of uterine fibroids, whereas both ovaries and
Fallopian tubes were atrophic.
The results of histopathology using H&E
confirmed histiocytic-rich lesions in the endometrium but otherwise
an unremarkable cervix and ovaries (Fig. 2B). Histopathological differential
diagnoses included RDD, MP and histiocytosis X. Subsequently,
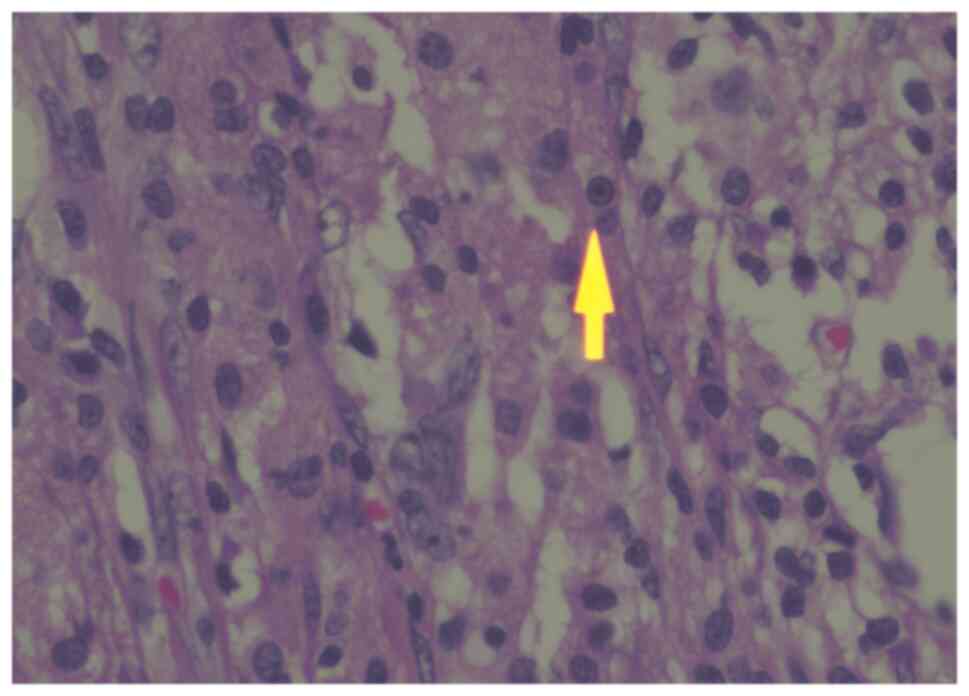
special stains were performed, which were suggestive of MP. The
tissue was positive for pathognomonic Michaelis-Gutmann bodies
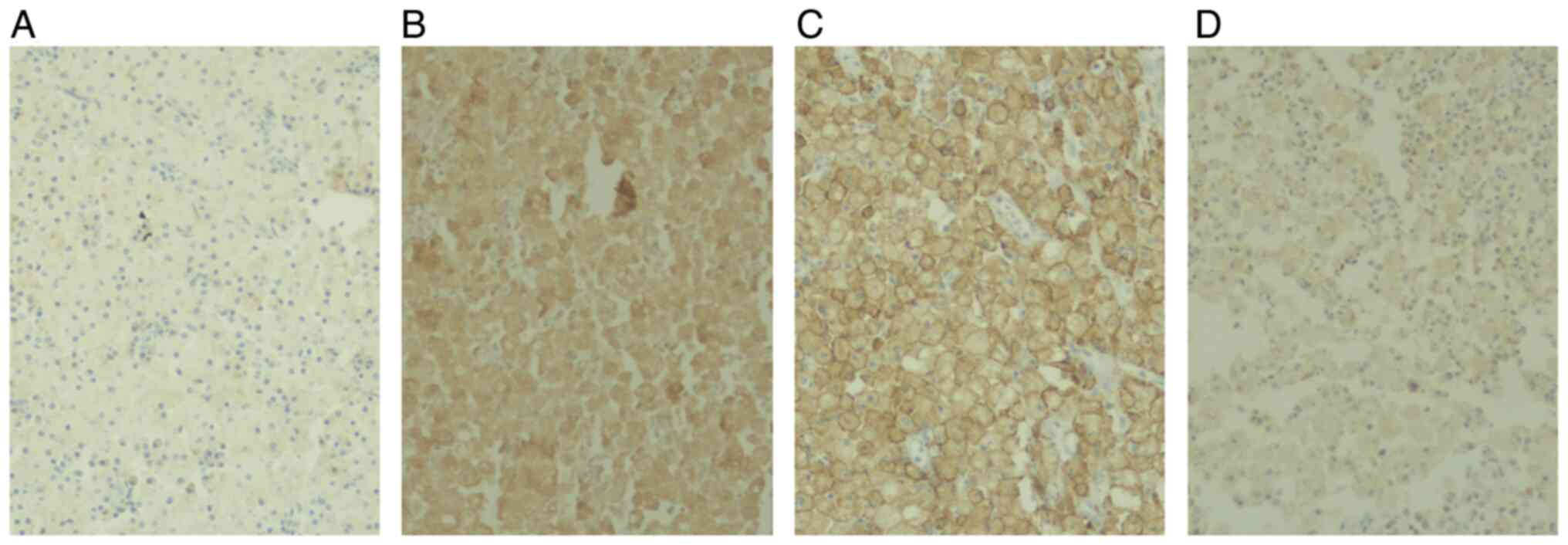
(H&E; Fig. 3). In addition,
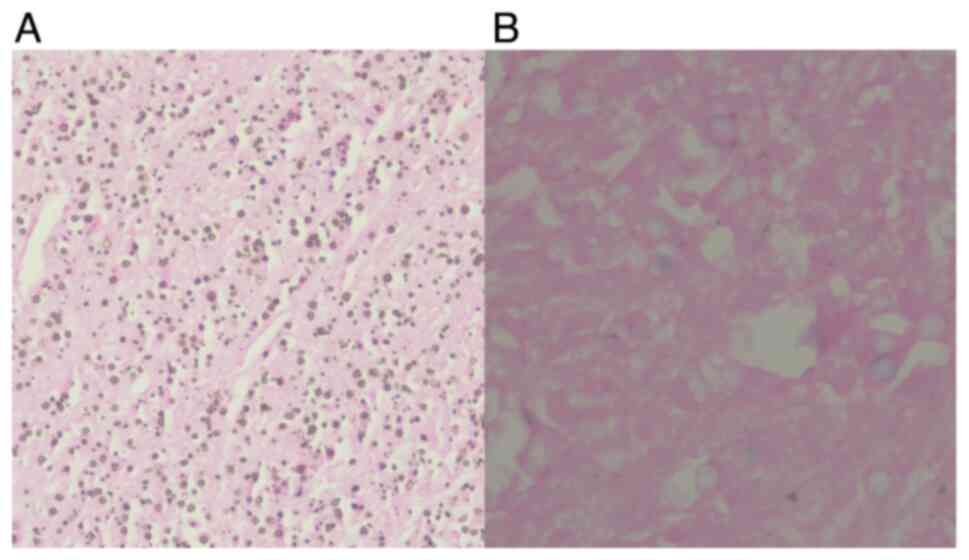
both van Kossa staining (Fig. 4A)
and iron staining (Fig. 4B)
revealed positive results. A second histopathological opinion was
sought, where further immunohistochemical staining was performed to
examine the potential presence of RDD. For immunohistochemistry, a
tissue sample was embedded in paraffin and cut at a thickness of 5
µm. The sections were incubated in H2O2
solution and a ready-to-use antibody kit was used. Detection was
performed using 3,3'-diaminobenzidine. The stained tissue sections
were observed under a light microscope. Finally, the presence of
RDD was confirmed in addition to MP through positive staining to
CD68, CD163 and S100 and negative staining to CD1a (Fig. 5). All staining was performed using
standard protocols on an automated machine with pre-prepared
antibodies (BenchMark GX; Roche Tissue Diagnostics).
Postoperatively, the patient had multiple admissions
to the same hospital (three times for 5-6 days each) due to
recurrent retroperitoneal abscesses, pneumonia and sepsis, but
eventually, the patient recovered completely. The blood and pus
cultures were positive for Escherichia coli. Broad-spectrum
antibiotics were administered (mainly meropenem 500 mg
intravenously twice daily and levofloxacin 500 mg intravenously
once daily for 10 days that were chosen according to blood and
abscess aspirate culture sensitivity) and a multiple CT-guided
drainage of the pelvic abscesses was performed.
Discussion
XE is a benign disease that most commonly involves
the kidney and gallbladder, but it rarely involves the female
genital tract (2). Whilst the
pathogenesis of XE remains clear, it may include obstruction of the
female genital tract, inflammation, ischemia and hemorrhage, which
may lead to the generation of free radicals and lipid peroxidation
as part of the inflammatory process (2). Furthermore, in the histopathological
diagnosis of XE, there is either focal or diffuse histiocyte
infiltration (3). In the present
case, XE involved the endometrium and two-thirds of the myometrium,
which may explain the posterior uterine wall lesion observed on the
CT scan.
The development of XE may involve both Langerhans
and non-Langerhans cell histiocytosis (12). The non-Langerhans cell
histiocytosis may encompass various diseases, such as RDD (12), which the patient in the present
case was also found to have.
The first reported case of XE was in 1978(1) with <30 reported cases worldwide to
date (3,13). The clinical interest of XE in
gynecology is that the clinical presentation, imaging and pathology
may mimic malignancy, thereby making management challenging and
necessitating a definitive histopathological diagnosis (1,2).
Since the endometrial biopsy in the present case indicated XE and
considering that endometrial adenocarcinoma and XE may co-exist
(2), the patient was advised to
undergo TAH + BSO.
Risk factors for the development of XE include being
postmenopausal, having diabetes mellitus and hypertension, which
the present patient had. The majority of cases of XE resolve after
antibiotic treatment (1,3,13).
However, if untreated, XE may result in systemic inflammation and
death; therefore, surgery forms the mainstay of the treatment
(1,3,13).
The patient in the present case had several
postoperative hospital admissions due to recurrent retroperitoneal
abscesses, pneumonia and sepsis. This postoperative course is not
uncommon in women who have XE and develop Escherichia coli
infections, similarly to the present case (14). The abscesses were drained under CT
guidance along with antibiotics treatment [mainly meropenem
(carbapenem) and levofloxacin (third generation fluoroquinolone)],
which were chosen according to the bacterial culture
sensitivity.
RDD is a rare inflammatory disease characterized by
non-Langerhans cell histiocytosis commonly affecting the lymph
nodes. Up to 2018, there have been only three reported cases of RDD
involving the female genital tract (10). Histologically, RDD is characterized
by positive staining of S100, CD68 and CD163 and negative staining
of CD1a and Langerin (CD207) (11).
Surgical excision of the affected tissue may be
indicated in a unifocal extranodal disease (11) as in the present case. Additionally,
systemic therapy may include corticosteroids, whereas
immunomodulators can be used for the treatment of a non-focal
disease. A recurrence is reported in 70% of untreated RDD cases
(10).
MP is another rare inflammatory disease that
frequently occurs in immunocompromised individuals (5). It commonly affects the urinary
system, but rarely involves the female genital tract (4). Up to 2021, a total of <40 cases of
MP involving the female genital tract have been reported, with the
vagina being the most commonly affected site (4). The etiology of MP is poorly
understood and is considered to be associated with the defective
bactericidal capacity of macrophages (5). Clinically, vaginal bleeding is the
most common presentation (83%) of MP (4). Histopathologically, pathognomonic
Michaelis-Gutmann bodies (calcified iron-containing
intracytoplasmic inclusions) are characteristic of MP, whilst
positive staining can also be observed with periodic acid-Schiff,
Perls' stain and von Kossa stain (5). Due to the limited cases reported, the
clinical management of this disease remains unclear. However,
general principles of treatment include the use of systemic
antibiotics, surgical excision and limiting the immunosuppression
process (5). These overlapping
inflammatory processes (XE, RDD and MP) can be misdiagnosed
clinicoradiologically as malignancy. However, clinicoradiological
methods are the primary methods for differential diagnosis until a
histopathological diagnosis is made (1,3).
Furthermore, immunostaining techniques are used to confirm the
inflammatory and disease-specific process over the neoplastic one
(1,3). Also, the presence of
Michaelis-Gutmann bodies is pathognomonic for MP, which are absent
in malignancy (1,3).
In conclusion, XE is a rare inflammatory disease,
which rarely involves the endometrium. It may be misdiagnosed as
cancer, where its presence may complicate a postoperative course
with repeated infections. Therefore, knowledge of the disease may
help in planning postoperative care. Surgical resection and
antibiotics administration are the primary treatment strategy for
this disease.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
WAE and MAA clinically managed the patient,
performed the surgery, and drafted and revised the manuscript. SS
and IAM collected clinical data, wrote and edited the manuscript,
and prepared the figures. AAM performed histopathological analyses
and drafted the manuscript. IAM and SS confirm the authenticity of
all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Malik V, Chatterjee D, Goel B and Takkar
N: Xanthogranulomatous endometritis: A benign uncommon masquerader
of malignancy. J Midlife Health. 10:206–208. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Makkar M, Gill M and Singh D:
Xanthogranulomatous endometritis: An unusual pathological entity
mimicking endometrial carcinoma. Ann Med Health Sci Res. 3
(Suppl1):S48–S49. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Merviel P, James P, Carlier M,
Thomas-Kergastel I, Guilloique M, Conan-Charlet V, Bastard C,
Marcorelles P, Jobic Y and Dupré PF: Xanthogranulomatous
endometritis: A case report and literature review. Clin Case Rep.
9(e04299)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Saco A, Rakislova N, Marimon L, Torne A,
Diaz-Feijoo B, Salvador R, Alos S, Jordao D, Hurtado JC and Ordi J:
Malacoplakia of the uterine cervix: A case report. Pathogens.
10(343)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kwan E, Riley CA and Robinson CA:
Malakoplakia. In StatPearls. StatPearls Publishing.
Malakoplakia-PubMed (nih.gov), 2022.
|
|
6
|
Leão CA, Duarte MI, Gamba C, Ramos JF,
Rossi F, Galvão MM, David-Neto E, Nahas W, Shikanai-Yasuda MA and
Pierrotti LC: Malakoplakia after renal transplantation in the
current era of immunosuppressive therapy: Case report and
literature review. Transpl Infect Dis. 14:E137–E141.
2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Medlicott S, Magi-Galluzzi C, Jimenez RE
and Trpkov K: Malakoplakia associated with prostatic
adenocarcinoma: Report of 4 cases and literature review. Ann Diagn
Pathol. 22:33–37. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kohl SK and Hans CP: Cutaneous
malakoplakia. Arch Pathol Lab Med. 132:113–117. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Werneck Rodrigues DO, Wolp Diniz R, Dentz
LC, Costa MA, Lopes RH, Suassuna LF, Cintra JRD and Domenge C: Case
study: Rosai-dorfman disease and its multifaceted aspects. J Blood
Med. 15:123–128. 2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Marie J, Alday M and Cortez AC. (n.d.):
Case report: Rosai-Dorfman disease: Pelvic
manifestation*.
|
|
11
|
Bruce-Brand C, Schneider JW and Schubert
P: Rosai-Dorfman disease: An overview. J Clin Pathol. 73:697–705.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bourm KS, Menias CO, Ali K, Alhalabi K and
Elsayes KM: Spectrum of xanthogranulomatous processes in the
abdomen and pelvis: A pictorial review of infectious, inflammatory,
and proliferative responses. AJR Am J Roentgenol. 208:475–484.
2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chandramouli R, Rajan N, Veerappan V,
Venkatesan D and Balasundaram P: Xanthogranulomatous endometritis:
A benign mimicker of malignancy. Int J Reprod Contracept Obstet
Gynecol. 13:1858–1861. 2024.
|
|
14
|
Silva-Rengifo C, Asencio A and Salirrosas
O: Xanthogranulo-matous endometritis: A report of two cases.
Cureus. 15(e38226)2023.PubMed/NCBI View Article : Google Scholar
|