Introduction
For a number of years, endoscopic retrograde
cholangiopancreatography (ERCP)-guided biliary drainage (ERCP-BD)
has been the first choice for the treatment of malignant biliary
obstruction (MBO). However, this drainage method can be difficult
when the duodenoscope cannot reach the Vater papilla because of
duodenal obstruction or if biliary cannulation is impossible.
Recently, endoscopic ultrasound-guided biliary drainage (EUS-BD) is
widely used as a second biliary drainage method for MBO in patients
for whom ERCP-BD fails (1). EUS-BD
methods include EUS-guided choledochoduodenostomy (EUS-CDS),
EUS-guided hepaticogastrostomy (EUS-HGS), EUS-guided antegrade
stenting (EUS-AGS), and combination of EUS-HGS and EUS-AGS. In
recent meta-analyses, the technical success and clinical success of
these EUS-BD techniques were reported to be comparable to those of
ERCP-BD (2,3). Therefore, EUS-BD has become the
first-line biliary endoscopic treatment. However, EUS-BD is a
skilled endoscopic treatment. Several severe adverse events, such
as bleeding, bile leakage, and dislocation (4,5),
which are sometimes fatal (6,7),
have been reported in previous reports and avoiding technical
failure is desirable. Despite the risk, EUS-BD can be performed by
endoscopists without sufficient experience. For these reasons,
ERCP-BD is successful in most cases, and EUS-BD is a relatively
novel treatment (8). On the other
hand, which EUS-BD procedures are appropriate for beginners is
unknown. In this study, we aimed to clarify the factors for
successful EUS-BD performed by beginners and to determine which
EUS-BD cases are suitable for beginners.
Materials and methods
Study design, patients, and
ethics
This was a retrospective study that investigated
methods for selecting MBO cases that are suitable for EUS-BD
beginners. This study was approved by the Institutional Review
Board of Fukushima Medical University (approval number: REC
2023-201). Patients with histologically diagnosed MBO who underwent
EUS-BD at Fukushima Medical University between March 2005 and June
2024 were enrolled in this study. The need to obtain informed
consent was waived because this was a retrospective study of
anonymized clinical data. The details of the study can be found on
the homepage of Fukushima Medical University.
Definition of EUS-BD beginners
All EUS-BD procedures were performed by
endoscopists, who have performed more than 300 cases of endoscopic
ultrasound-guided fine needle aspiration (EUS-FNA). EUS-BD
beginners were defined as endoscopists who had performed fewer than
20 procedures according to a previous report written by Hara et
al (9).
EUS-BD procedures
EUS-BD procedures were started after MBO patients
were sufficiently sedated by midazolam. EUS-BD was performed as
follows: the puncture point of the target bile duct was determined
via consultation with an expert. The common bile duct or
intrahepatic bile duct was punctured via the duodenal bulbus or
stomach via an EUS-FNA needle, and the biliary tract was enhanced
via the injection of contrast medium. After a sufficient length of
guidewire was placed in the biliary tract, fistula dilation was
performed via a dilation catheter. Finally, a biliary stent was
placed via the duodenum or stomach. When the puncture route or the
guidewire could not be observed on the monitor, the echo image was
modulated under expert guidance. If an EUS-BD beginner could not
complete the procedure, an expert completed the procedure.
The selection of an appropriate EUS-BD method was as
follows: For lower biliary strictures without duodenal bulb
obstruction, EUS-CDS was performed. For hilar biliary strictures or
long CBD strictures, EUS-HGS was performed. When a guidewire was
sufficiently inserted into the duodenum, EUS-AGS was combined with
EUS-HGS. EUS-HGS was also performed for patients who underwent
partial gastrectomy.
The echoendoscope used was a GF-UCT260,
GF-UC240P-AL5, or GF-UCT240-AL5 (Olympus Medical Systems, Tokyo,
Japan). The echo device used was an EU-ME1, an EU-ME2 (Olympus
Medical Systems), a Prosound SSD α10, or an SSD5500 (Hitachi Alocha
Medical, Tokyo, Japan). The FNA needles used were 19G SonoTip
(Medi-Grobe, Rosenheim, Germany), 19G Echotip Ultra (Cook Medical,
Tokyo, Japan), 19G NA-11J-KB (Olympus Medical Systems), 19 or 22G
Expect (Boston Scientific Japan, Tokyo, Japan), or 19 or 22G Ez
shot3 plus (Olympus Medical Systems) needles. The guidewire used
was a 0.018 Fielder 18, 0.025 VisiGlide, VisiGlide 2 (Olympus
Medical Systems), 0.025 or 0.035 Jagwire, or 0.025 EndoSelector
(Boston Scientific Japan). The dilator used was a 6-Fr
Cysto-Gastro-Set (Endo-Flex GmbH, Voerde, Germany), an ES dilator
(Zeon Medical Co., Tokyo, Japan), an MTW ERCP tapered catheter (MTW
endoskopie, Wesel, Germany), a Tornus ES (Olympus Medical Systems),
or a 4 mm Hurricane RX Biliary Balloon Dalation Catheter (Boston
Scientific Japan). The biliary plastic stent used was a 7 Fr
Flexima Plus (Boston Scientific), 7 Fr IT (Gadelius Medical Co.,
Ltd., Tokyo, Japan), or 7 Fr double pig-tail stent (Cook Medical).
The biliary self-expandable metallic stent (SEMS) used for EUS-CDS
or EUS-HGS was a 10 mm Niti-S COMVI, an 8 mm Niti-S covered Spring
Stopper (Taewoong Medical, Gyoenggi-do, Korea), or a 10 mm
partially covered WallFlex Biliary RX stent (Boston Scientific).
The biliary SEMS used for EUS-AGS was a 10 mm Zilver 635 (COOK
Medical), an 8-10 mm BileRush (PIOLAX, Kanagawa, Japan), or a 10 mm
Niti-S Large Cell slim delivery (Taewoong Medical).
Outcomes
The main aim of this study was to identify
predictive factors for successful EUS-BD performed by beginners.
The potential predictive factors were selected according to
previous reports (10-13).
The patient characteristics included age, sex, history of
gastrectomy, disease status (primary or metastatic), biliary
stricture location, and use of a duodenal stent before EUS-BD. The
factors related to EUS-BD procedures included the puncture length,
diameter of the punctured bile duct, use of an EUS-FNA needle (19 G
or 22 G), type of dilator used (cautery or mechanical), type of
EUS-BD (CDS or HGS, with or without AGS), and type of stent used
(plastic stent or metallic stent).
The puncture length and diameter of the punctured
bile duct were measured via echo imaging. When an appropriate echo
image was not available, these parameters were measured via X-ray
imaging. The definition of technical success was stent deployment
from the stomach or duodenum to the target bile duct. The
definition of clinical success was an improvement in alanine
transaminase or total bilirubin values to normal values or half of
the pretreatment values.
Sample size
The primary aim of this study was to clarify the
factors associated with successful EUS-BD performed by beginners.
To achieve this aim via multiple logistic regression, 10 events per
explanatory variable were needed. Two variables were evaluated in
the multivariate analysis; therefore, 20 patients with successful
EUS-BD were necessary. According to the results below, the expected
technical success for beginners is approximately 70%. Therefore, at
least 29 patients were included in this study.
Statistical analysis
Continuous variables that were normally distributed
are presented as the means ± standard deviations. Continuous
variables that were not normally distributed are reported as
medians (ranges). Nominal variables are reported as n or n (%). The
potential factors for successful EUS-BD performed by beginners were
determined via multiple logistic regression. The determined factors
were evaluated via receiver operating characteristic (ROC) curves.
A P value <0.05 was considered statistically significant. All
the statistical analyses were performed via EZR version 1.68
(Saitama Medical Center, Jichi Medical University, Saitama,
Japan).
Results
Participants
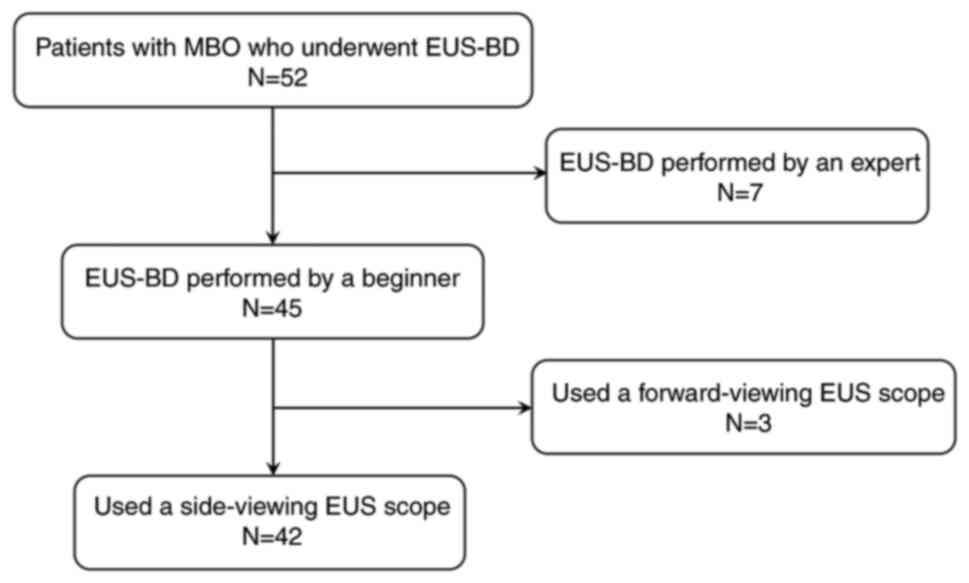
The flowchart of the participants is shown in
Fig. 1. EUS-BD was attempted in 52
patients with MBO. Among these patients, 45 underwent EUS-BD
performed by beginners. Three patients with a history of
pancreaticoduodenotectomy and biliojejunostomy were excluded from
this study because they underwent EUS-BD via a forward-viewing
echoendoscope. Overall, 42 patients who underwent EUS-BD performed
by beginners with the use of a side-view echoendoscope were
included in this study.
Summary of patient characteristics and
EUS-BD procedures
The patient characteristics and EUS-BD procedures
performed by beginners are shown in Table I. The mean age was 71.7±9.4 years.
Twenty-seven (64.3%) patients were male. Three patients underwent
gastrectomy (Billroth-I: 1 patient, Billroth-II: 2 patients), 38
MBO patients had primary disease, and 4 MBO patients had metastatic
disease. Distal biliary stricture was observed in 39 (92.9%)
patients. Fourteen (33.3%) MBO patients underwent EUS-CDS, and 28
(66.7%) patients underwent EUS-HGS. In 10 patients, EUS-AGS was
added to the procedure. The final technical success rate for the
experts was 95.2% (40 patients), and the technical success rate for
the beginners was 73.8% (31 patients). The reasons for technical
failure for beginners were puncture failure (n=9), dilation failure
(n=1), and stenting failure (n=1). The adverse events were bile
leakage (n=1) and bleeding (n=1).
 | Table ISummary of patient characteristics
(n=42) and EUS-BD performed by beginners. |
Table I
Summary of patient characteristics
(n=42) and EUS-BD performed by beginners.
| Parameters | Value |
|---|
| Mean age ± SD,
years | 71.7±9.4 |
| Sex, n (%) | |
|
Male | 27 (64.3) |
|
Female | 15 (35.7) |
| History of
gastrectomy, n (%) | 3 (7.1) |
|
Billroth-I,
n | 1 |
|
Billroth-II,
n | 2 |
| Diagnosis, n (%) | |
|
Primary
disease | 38 (90.5) |
|
Pancreatic
cancer | 29 |
|
Biliary
tract cancer | 9 |
|
Metastatic
disease | 4 (9.5) |
|
Bladder
cancer, n | 1 |
|
Urothelial
cancer, n | 1 |
|
Retroperitoneal
liposarcoma, n | 1 |
|
Lymph
node metastasis of unknown origin, n | 1 |
| Biliary stricture
location, n (%) | |
|
Distal | 39 (92.9) |
|
Hilar | 3 (7.1) |
| Duodenal stent before
EUS-BD, n (%) | 11 (26.2) |
| Mean puncture length
± SD, mm | 17.2±7.5 |
| Median diameter of
the punctured bile duct (range), mm | 7.3 (1.7-20.0) |
| Type of needle used,
n (%) | |
|
19 G | 25 (59.5) |
|
22 G | 17 (40.5) |
| Type of dilator used,
n (%) | |
|
Cautery
dilator | 6 (14.3) |
|
Mechanical
dilator | 36 (85.7) |
| EUS-CDS, n (%) | 14 (33.3) |
| EUS-HGS, n (%) | 28 (66.7) |
| Addition of EUS-AGS,
n (%) | 10 (23.8) |
| Type of stent used, n
(%) | |
|
Plastic | 30 (71.4) |
|
SEMS | 10 (2.4) |
|
Stent
placement failure | 2 (4.8) |
| Technical success, n
(%) | 40 (95.2) |
| Technical success for
beginners, n (%) | 31 (73.8) |
| Reasons for technical
failure of beginners, n | |
|
Puncture
failure | 9 |
|
Dilation
failure | 1 |
|
Stenting
failure | 1 |
| Clinical success, n
(%) | 40 (95.2) |
| Adverse events, n
(%) | 2 (4.8) |
|
Bile
leakage, n | 1 |
|
Bleeding,
n | 1 |
Predictive factors for successful
EUS-BD performed by beginners
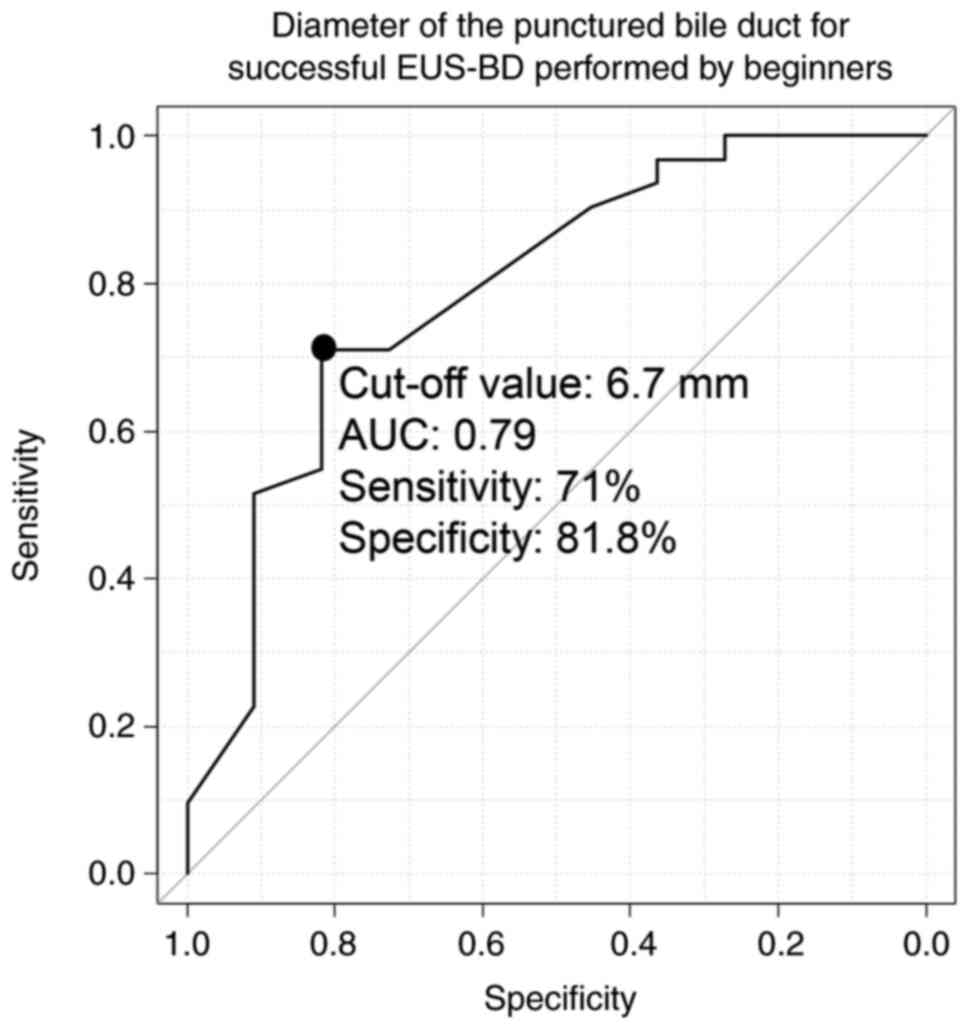
The results of the multivariate analysis are shown
in Table II. According to the
univariate analyses, the diameter of the punctured bile duct was
the only significant factor for successful EUS-BD performed by
beginners (odds ratio (OR): 1.35, 95% confidence interval (CI)
0.33-5.30, P value=0.026). According to the reasons for the
technical failure of beginners, puncture failure was the main cause
(Table I). According to previous
reports, the determination of the tumor position via EUS monitoring
is a risk factor for puncture failure (14). Therefore, the puncture length,
which is a factor affecting the tumor position, and the diameter of
the punctured bile duct were included in the multivariate analysis.
Finally, the diameter of the punctured bile duct was a significant
predictor of successful EUS-BD performed by beginners according to
multivariate analysis (OR: 1.34, 95% CI: 1.03-1.75; P value=0.031).
The cutoff value of the punctured bile duct diameter was 6.7 mm
(area under the ROC curve: 0.79; sensitivity: 71%; specificity:
81.8%), as shown in Fig. 2.
 | Table IIUnivariate and multivariate analyses
of predictive factors that might be associated with successful
EUS-BD performed by beginners. |
Table II
Univariate and multivariate analyses
of predictive factors that might be associated with successful
EUS-BD performed by beginners.
| | Univariate | Multivariate |
|---|
| Variable | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Age | 0.93 | 0.85-1.02 | 0.12 | | | |
| Sex, male | 2.93 | 0.71-12.10 | 0.14 | | | |
| History of
gastrectomy | 0.69 | 0.06-8.45 | 0.77 | | | |
| Primary disease | 0.93 | 0.09-10.00 | <0.96 | | | |
| Distal biliary duct
stricture | <0.01 | 0-infinity | <0.99 | | | |
| Duodenal stent
before EUS-BD | 0.93 | 0.20-4.38 | 0.92 | | | |
| Puncture
length | 0.95 | 0.87-1.04 | 0.29 | 0.99 | 0.89-1.11 | 0.89 |
| Diameter of the
punctured bile duct | 1.35 | 1.04-1.75 | 0.03 | 1.34 | 1.03-1.75 | 0.03 |
| 19 G needle
used | 1.32 | 0.33-5.30 | 0.70 | | | |
| Cautery dilator
used |
5.10x107 | 0-infinity | 0.99 | | | |
| EUS-HGS (vs.
CDS) | 0.31 | 0.057-1.67 | 0.17 | | | |
| Addition of
EUS-AGS | 1.57 | 0.28-8.83 | 0.61 | | | |
| Plastic stent
used | <0.01 | 0-infinity | 0.99 | | | |
Discussion
This study revealed that the diameter of the
punctured bile duct was associated with successful EUS-BD performed
by beginners. The recent meta-analysis by Barbosa et al
(15) included six randomized
controlled trials (577 patients) and compared the treatment
outcomes between patients who underwent EUS-BD and those who
underwent ERCP-BD. For EUS-BD, the technical success rate, clinical
success rate, and adverse event rate were 93.0% (95% CI:
89.3-95.5), 89.0% (95% CI: 80.9-93.9), and 8.33% (95% CI:
4.30-15.53), respectively. For ERCP-BD, the technical success rate,
clinical success rate, and adverse event rate were 88.0% (95% CI:
79.1-93.4), 88.0% (95% CI: 83.3-91.5), and 15.6% (95% CI:
10.9-21.9), respectively. These treatment outcomes are not
significantly different, and EUS-BD could be the first choice for
the endoscopic treatment of MBO. EUS-BD procedures are being
refined and are becoming more popular. However, the clear
conditions for EUS-BD that are appropriate for beginners are not
well known.
In previous reports, puncture and opacification,
guidewire manipulation, and fistula dilation emerged as
representative and definitive factors for predicting EUS-BD
failure. Vila et al (16)
reported the initial experience of EUS-BD and EUS-guided pancreatic
drainage for 125 patients in Spain. Puncture and opacification were
successful in 113 patients, and guidewire manipulation was
successful in 94 patients. Oh et al (10) reported failure in 129 patients who
underwent EUS-HGS. Among these patients, 46 experienced EUS-HGS
failure (puncture and opacification failure: 11 patients; guidewire
manipulation failure: 15 patients; fistula dilation failure: 20
patients). With respect to the steps after guidewire manipulation,
not only the technique of the endoscopist but also the technique of
the assistant is important. This report indicated that bile duct
puncture might be the most critical step of EUS-BD procedures for
beginners.
For EUS-BD to the thin bile duct, a procedure
involving the use of 22 G needles, a new 0.018 guidewire, and a
dedicated dilator was reported. According to the report written by
Iwashita et al (17), the
technical success rate was 100% (26/26) for the median 5
(interquartile 3-6) mm diameter bile duct. Ogura et al
(18) also performed EUS-BD using
22G needles in 18 patients. Although the diameter of the bile duct
was very thin, ranging from 0.5-1.3 mm, the technical success rate
was 88.9%. These new devices can contribute to overcoming the
difficulty of EUS-BD in patients with thin biliary ducts. However,
excellent results have been achieved by very skilled experts. In
this study, 22G needles, a 0.018 guidewire, and a dedicated dilator
were used for some patients. Therefore, the diameter of the bile
duct is still a factor affecting the difficulty of EUS-BD for
beginners.
There were several limitations in this study. First,
this was a retrospective study performed at a single institution.
In the future, a multicenter prospective study is needed to confirm
the findings of this study. Second, several types of EUS-BD
procedures were evaluated. However, the rates of technical success,
clinical success, and adverse events were comparable between the
EUS-HGS and EUS-CDS procedures in a recent meta-analysis. In this
study, the EUS method was not associated with EUS-BD failure among
beginners.
In conclusion, the diameter of the punctured bile
duct might be associated with successful EUS-BD procedures
performed by beginners. When a beginner performs EUS-BD, a diameter
of the targeted bile duct >6.7 mm might be desirable for
successful procedures.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
MS wrote the paper, and designed and performed the
study. TT and HO designed and oversaw the study. RS, HA, TH, JN,
MT, HS, KS, RO, TK, TY and MO performed analysis and interpretation
of data. MS and TT confirm the authenticity of all the raw data.
All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of Fukushima Medical University (approval no. REC
2023-201; Fukushima, Japan). The requirement for informed consent
was waived because this was a retrospective study of anonymized
clinical data.
Patient consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mukai S, Itoi T, Baron TH, Takada T,
Strasberg SM, Pitt HA, Ukai T, Shikata S, Teoh AYB, Kim MH, et al:
Indications and techniques of biliary drainage for acute
cholangitis in updated Tokyo Guidelines 2018. J Hepatobiliary
Pancreat Sci. 24:537–549. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Jin Z, Wei Y, Lin H, Yang J, Jin H, Shen S
and Zhang X: Endoscopic ultrasound-guided versus endoscopic
retrograde cholangiopancreatography-guided biliary drainage for
primary treatment of distal malignant biliary obstruction: A
systematic review and meta-analysis. Dig Endosc. 32:16–26.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kakked G, Salameh H, Cheesman AR, Kumta
NA, Nagula S and DiMaio CJ: Primary EUS-guided biliary drainage
versus ERCP drainage for the management of malignant biliary
obstruction: A systematic review and meta-analysis. Endosc
Ultrasound. 9:298–307. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hayat U, Bakker C, Dirweesh A, Khan MY,
Adler DG, Okut H, Leul N, Bilal M and Siddiqui AA: EUS-guided
versus percutaneous transhepatic cholangiography biliary drainage
for obstructed distal malignant biliary strictures in patients who
have failed endoscopic retrograde cholangiopancreatography: A
systematic review and meta-analysis. Endosc Ultrasound. 11:4–16.
2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Paik WH and Park DH: Outcomes and
limitations: EUS-guided hepaticogastrostomy. Endosc Ultrasound. 8
(Suppl 1):S44–S49. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Martins FP, Rossini LG and Ferrari AP:
Migration of a covered metallic stent following endoscopic
ultrasound-guided hepaticogastrostomy: Fatal complication.
Endoscopy. 42 (Suppl 2):E126–E127. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ramírez-Luna MA, Téllez-Ávila FI,
Giovannini M, Valdovinos-Andraca F, Guerrero-Hernández I and
Herrera-Esquivel J: Endoscopic ultrasound-guided biliodigestive
drainage is a good alternative in patients with unresectable
cancer. Endoscopy. 43:826–830. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tonozuka R, Itoi T, Tsuchiya T, Tanaka R
and Mukai S: EUS-guided biliary drainage is infrequently used even
in high-volume centers of interventional EUS. Gastrointest Endosc.
84:206–207. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hara K, Yamao K, Mizuno N, Hijioka S,
Imaoka H, Tajika M, Tanaka T, Ishihara M, Okuno N, Hieda N, et al:
Endoscopic ultrasonography-guided biliary drainage: Who, when,
which, and how? World J Gastroenterol. 22:1297–1303.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Oh D, Park DH, Song TJ, Lee SS, Seo DW,
Lee SK and Kim MH: Optimal biliary access point and learning curve
for endoscopic ultrasound-guided hepaticogastrostomy with
transmural stenting. Therap Adv Gastroenterol. 10:42–53.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sugimoto M, Takagi T, Suzuki R, Waragai Y,
Konno N, Asama H, Sato Y, Irie H, Nakamura J, Takasumi M, et al:
Factors associated with difficult endoscopic ultrasonography-guided
biliary drainage. J Clin Gastroenterol. 58:494–501. 2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Honjo M, Itoi T, Tsuchiya T, Tanaka R,
Tonozuka R, Mukai S, Sofuni A, Nagakawa Y, Iwasaki H and Kanai T:
Safety and efficacy of ultra-tapered mechanical dilator for
EUS-guided hepaticogastrostomy and pancreatic duct drainage
compared with electrocautery dilator (with video). Endosc
Ultrasound. 7:376–382. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kanno Y, Ito K, Koshita S, Ogawa T, Masu
K, Masaki Y and Noda Y: Efficacy of a newly developed dilator for
endoscopic ultrasound-guided biliary drainage. World J Gastrointest
Endosc. 9:304–309. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yasuda I, Iwashita T and Doi S: Tips for
endoscopic ultrasound-guided fine needle aspiration of various
pancreatic lesions. J Hepatobiliary Pancreat Sci. 21:E29–E33.
2014.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Barbosa EC, Santo PADE, Baraldo S, Nau AL
and Meine GC: EUS-versus ERCP-guided biliary drainage for malignant
biliary obstruction: A systematic review and meta-analysis of
randomized controlled trials. Gastrointest Endosc. 100:395–405.e8.
2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vila JJ, Pérez-Miranda M,
Vazquez-Sequeiros E, Abadia MA, Pérez-Millán A, González-Huix F,
Gornals J, Iglesias-Garcia J, De la Serna C, Aparicio JR, et al:
Initial experience with EUS-guided cholangiopancreatography for
biliary and pancreatic duct drainage: A Spanish national survey.
Gastrointest Endosc. 76:1133–1141. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Iwashita T, Ogura T, Ishiwatari H, Nakai
Y, Iwata K, Mukai T, Shimizu M, Isayama H, Yasuda I and Itoi T:
Utility of dedicated bougie dilator for a 0.018-inch guidewire
during EUS-guided biliary drainage: A multi-center retrospective
cohort study. J Hepatobiliary Pancreat Sci. 29:810–816.
2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ogura T, Okuda A, Ueno S, Nishioka N,
Miyano A, Ueshima K, Yamamoto Y and Higuchi K: Prospective
comparison study between 19-gauge needle with .025-inch guidewire
and 22-gauge needle with novel .018-inch guidewire during
EUS-guided transhepatic biliary drainage (with video). Gastrointest
Endosc. 96:262–268.e1. 2022.PubMed/NCBI View Article : Google Scholar
|