Introduction
A hemangioma is a benign vascular mass lesion that
can occur in various parts of the body, including the kidneys,
liver, head, bladder and neck. They are rare, isolated, small and
usually unilateral (1-3).
Hemangiomas can have sponge-like, capillary-like or fibrous shapes;
however, venous hemangioma is a rarer subtype with non-specific
clinical manifestations (4).
Certain patients seek medical attention for hematuria; however,
most patients are asymptomatic. Hemangiomas are typically
discovered incidentally during physical or surgical examinations.
Due to the rarity of venous hemangioma, its preoperative diagnosis
is challenging and can often lead to misdiagnosis. Enhanced
computed tomography (CT) cannot completely distinguish between
retroperitoneal and renal venous hemangioma (5,6).
Although diagnosis is challenging, these venous hemangiomas are
benign with a good prognosis. Most patients receive a definitive
diagnosis during surgery and ultimate confirmation through
pathological examination (7). The
present study reported the case of a patient with renal vein
hemangioma that was initially detected as a left retroperitoneal
mass on CT and confirmed via histopathological examination
postoperatively.
Case report
The present study reports on a 37-year-old man with
a left renal venous hemangioma. The patient presented with frequent
urination for 1 week, urgency for 1 week, urethral pain for 1 week
and hematuria for 1 day at Zhangye People's Hospital affiliated
with Hexi University (Zhangye, China). Physical examination
revealed no palpable lumps, vertebral tenderness or skin damage.
Upon admission, blood examination revealed normal levels of white
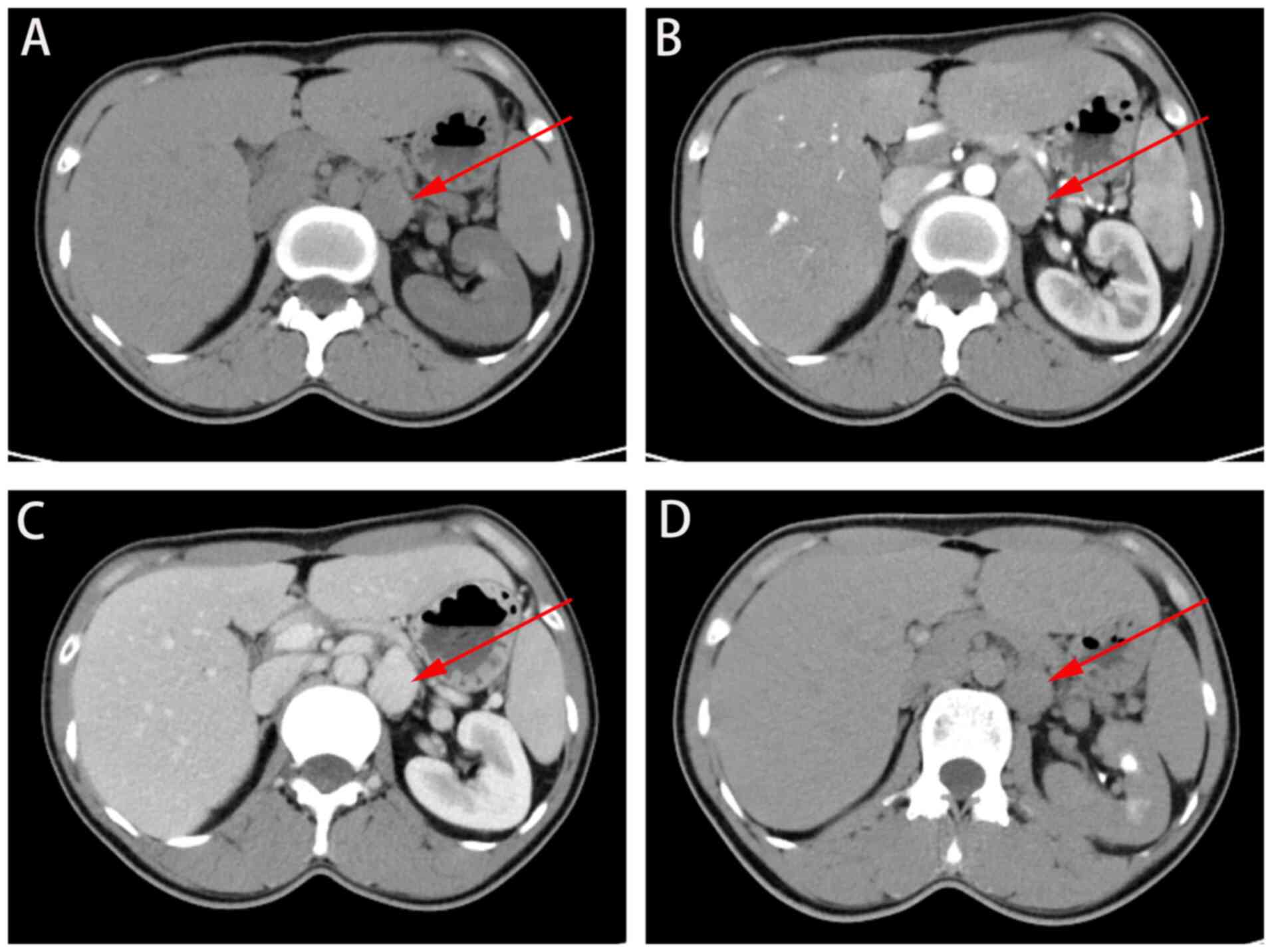
blood cells, red blood cells, platelets and coagulation. CT
revealed a left retroperitoneal mass, considered a left adrenal
tumor (Fig. 1). Surgical treatment
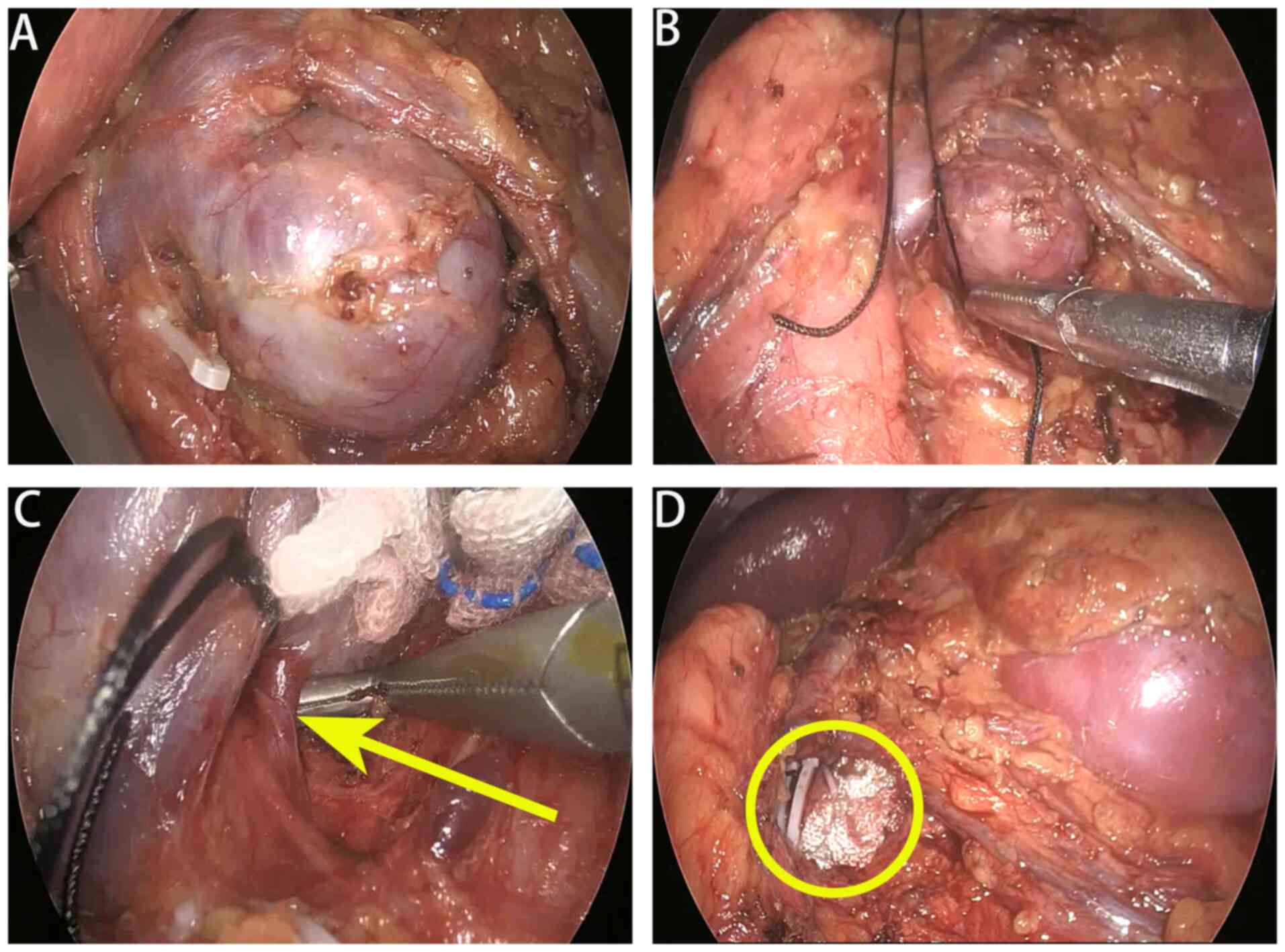
was performed, and a 3x2.6 cm, dark-purple soft mass was found next
to the left renal vein, which was compressed and deformed (Fig. 2A). A left renal venous hemangioma
was suspected (Fig. 2). Left renal
venous hemangioma resection was performed, resulting in the
disappearance of the patient's hematuria symptoms postoperatively.
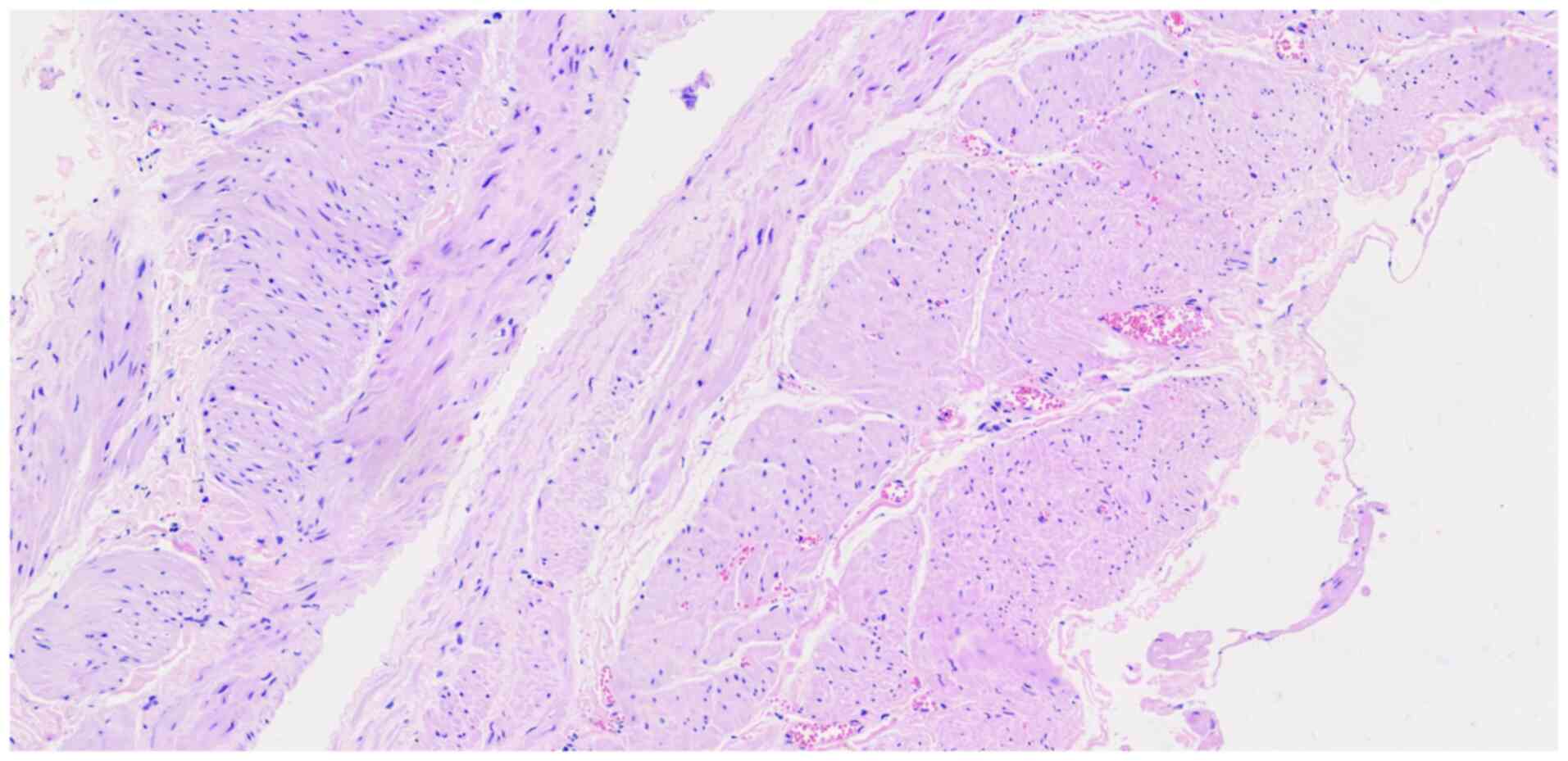
Pathological examination revealed a gray-red mass with smooth wall
and visible smooth muscle on hematoxylin-eosin staining; combined
with clinical findings, this confirmed the presence of a left renal
venous hemangioma (Fig. 3). The
patient was satisfied with the treatment and recovered well before
being discharged.
Discussion
Most renal hemangiomas are non-specific and
asymptomatic. The majority of renal hemangiomas are discovered
incidentally and occur in asymptomatic patients (8). A small percentage of patients may
experience clinical symptoms, including hematuria and lower back
pain. The current case report showcases that these diseases are
easily misdiagnosed preoperatively due to a lack of specific
clinical and imaging manifestations. Similar reports have been
published in the literature, and certain patients have undergone
nephrectomies. Hemangiomas and vascular sarcomas may at times
appear very similar (9). On CT,
their characteristic features include increased early peripheral
and delayed enhancement. Abdominal cavernous hemangioma typically
has distinct features on imaging, and ultrasound may be helpful in
its differentiation, showing peripheral enhancement accompanied by
a central hypoechoic area (10,11).
These features distinguish renal hemangiomas from renal aneurysms,
as well as renal tumors from adrenal tumors. However, these signs
are not unique to renal vein hemangiomas and relying solely on an
ultrasound diagnosis may be insufficient. Enhanced CT or magnetic
resonance imaging (MRI) is required for differential diagnosis.
Renal venous hemangiomas are benign and may be
associated with congenital diseases (5). The patient's family history has an
important role in the genetic diagnosis of any vascular
malformation; however, the patient of the present study had no
family history after consultation. The incidence of spontaneous
bleeding in patients with renal hemangiomas is low. However,
adverse events may occur due to diseases such as vascular
fragility, infarction, necrosis, cystic inflammation and increased
pressure from the blood vessels. It is crucial to increase
awareness of this rare disease. Preoperative imaging is essential
and enhanced CT and MRI examinations can be performed if needed
(6). However, mature and minimally
invasive kidney surgical techniques and professional knowledge are
crucial. Laparoscopic or robotic surgery at experienced medical
institutions is a safe and effective treatment method.
In conclusion, the preoperative diagnosis of renal
venous hemangioma is challenging because no imaging or clinical
standards exist for reference. The best treatment should be
tailored to a specific situation, even if the venous hemangioma is
accidentally discovered during surgery, requiring temporary
decision-making based on factors such as location, size and
symptoms. Based on our experience, a thorough preoperative impact
assessment and precise minimally invasive surgery are necessary for
ensuring a good patient prognosis at professional medical
institutions.
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by a grant from the Hexi
University 14th Science and Technology Innovation Project (grant
no. 164).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JL, YPL and JXY contributed to the drafting of the
manuscript and the design of the study. RY, LZ, XZ, JW, YQQ and JQ
contributed substantially to the conceptualization and design of
the study. JXY aided with the completion of the surgery. JQ and JXY
approved the final version of the manuscript for publication. JQ
and JY confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Hexi University affiliated Zhangye People's Hospital (approval
no. B2024-026; Zhangye, China).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the patient's data/images included
in this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torrence D and Antonescu CR: The genetics
of vascular tumours: An update. Histopathology. 80:19–32.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Garaz R, Stühler V, Stenzl A, Rottscholl R
and Amend B: Hemangioma of the urinary bladder: A brief narrative
review of their diagnosis, histology, and treatment options. Urol
Int. 108:83–88. 2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Iacobas I, Phung TL, Adams DM, Trenor CC
III, Blei F, Fishman DS, Hammill A, Masand PM and Fishman SJ:
Guidance document for hepatic hemangioma (infantile and congenital)
evaluation and monitoring. J Pediatr. 203:294–300.e2.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mansfield SA, Williams RF and Iacobas I:
Vascular tumors. Semin Pediatr Surg. 29(150975)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Montanaro F, Bertolo R, Costantino S, De
Maria N, Veccia A, Migliorini F, Caliò A, Brunelli M, Montemezzi S,
Cerruto MA and Antonelli A: Robot-assisted excision of hemangioma
of the right renal vein. Urol Case Rep. 53(102651)2024.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Elek A, Kwon JW, Ertugrul S and Oren NC:
Radiologic and pathologic correlation of a renal venous hemangioma.
Int Cancer Conf J. 12:227–232. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yoshino N, Okada D, Ujiie H, Akiyama H,
Nishimura Y, Koizumi K and Shimizu K: Venous hemangioma of the
posterior mediastinum. Ann Thorac Cardiovasc Surg. 18:247–250.
2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sternberg IA, Katz BF, Baldinger L, Mano
R, Paz GE, Bernstein M, Akin O, Russo P and Karlo C: Can renal
hemangiomas be diagnosed preoperatively? Isr Med Assoc J.
17:157–160. 2015.PubMed/NCBI
|
|
9
|
Subramaniam A, Giani C, Napolitano A, Ravi
V, Frezza AM and Jones RL: Management of vascular sarcoma. Surg
Oncol Clin N Am. 31:485–510. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Goncharuk RA, Rakhmonov ZA, Stegnii KV,
Krekoten AA, Shulga IV and Dvoinikova ER: Combined surgical
treatment of giant cavernous hepatic hemangioma: A case report. Int
J Surg Case Rep. 94(107012)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ferreira FG, Ribeiro MA, Abreu P, Ferreira
R, Assef MS, Park JH and Szutan LA: Endoscopic Ultrasound-guided
ethanol injection associated with Trans-arterial embolization of a
giant Intra-abdominal cavernous hemangioma: Case report and new
therapeutic option. J Gastrointest Cancer. 52:381–385.
2021.PubMed/NCBI View Article : Google Scholar
|