|
1
|
World Health Organization. Global
tuberculosis report 2020. Geneva, World Health Organization,
2020.
|
|
2
|
Peto HM, Pratt RH, Harrington TA, LoBue PA
and Armstrong LR: Epidemiology of extrapulmonary tuberculosis in
the United States, 1993-2006. Clin Infect Dis. 49:1350–1357.
2009.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Sandgren A, Hollo V and van der Werf MJ:
Extrapulmonary tuberculosis in the European Union and European
Economic Area, 2002 to 2011. Euro Surveill.
18(20431)2013.PubMed/NCBI
|
|
4
|
Wang X, Yang Z, Fu Y, Zhang G and Wang X,
Zhang Y and Wang X: Insight to the epidemiology and risk factors of
extrapulmonary tuberculosis in Tianjin, China during 2006-2011.
PLoS One. 9(e112213)2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nachiappan AC, Rahbar K, Shi X, Guy ES,
Mortani Barbosa EJ Jr, Shroff GS, Ocazionez D, Schlesinger AE, Katz
SI and Hammer MM: Pulmonary tuberculosis: Role of radiology in
diagnosis and management. Radiographics. 37:52–72. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bholla M, Kapalata N, Masika E, Chande H,
Jugheli L, Sasamalo M, Glass TR, Beck HP and Reither K: Evaluation
of Xpert® MTB/RIF and Ustar EasyNAT™ TB IAD for
diagnosis of tuberculous lymphadenitis of children in Tanzania: A
prospective descriptive study. BMC Infect Dis.
16(246)2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
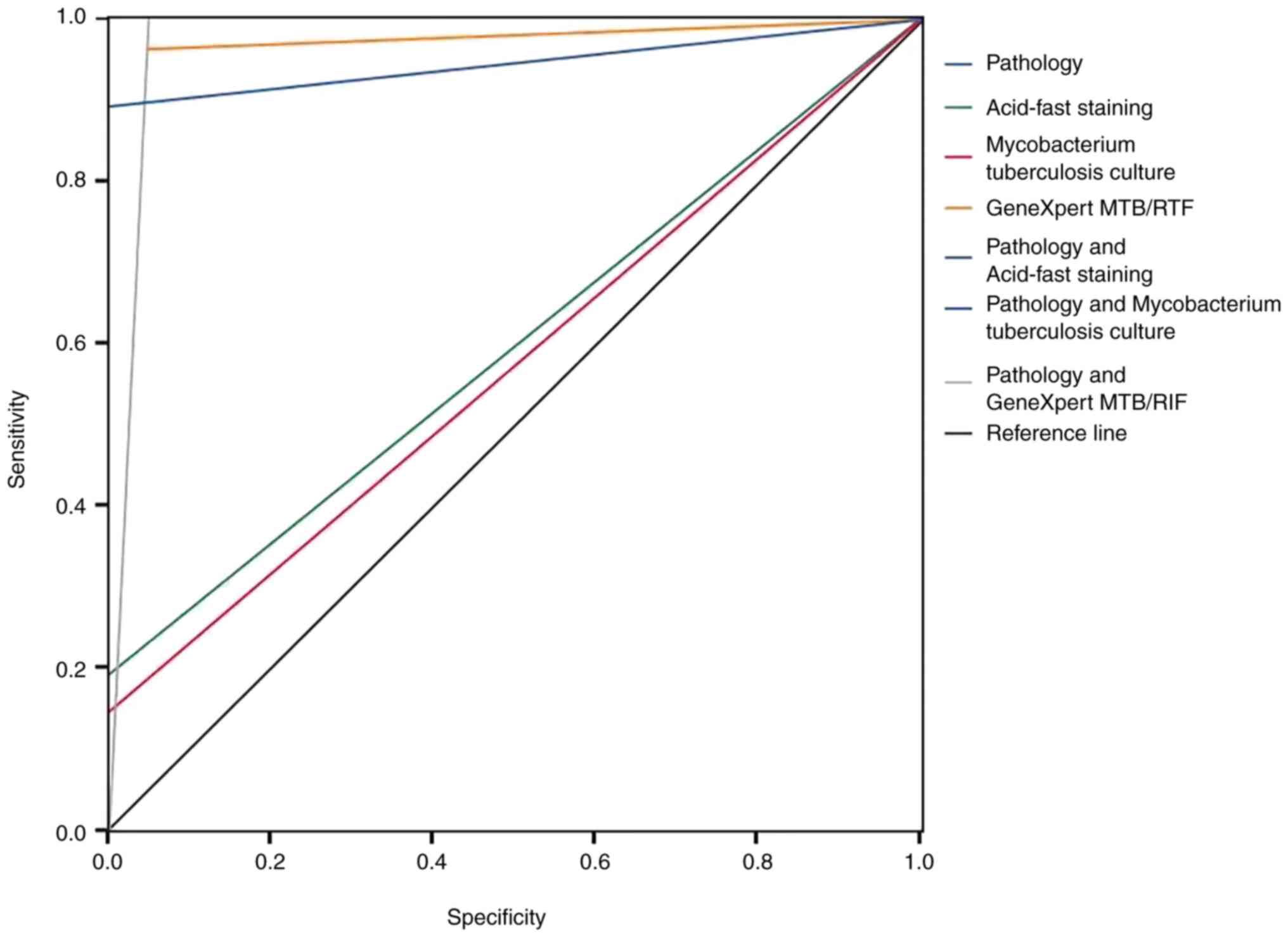
Sun W, Zhou Y, Li W, Wang Y, Xiong K,
Zhang Z and Fan L: Diagnostic yield of Xpert MTB/RIF on
contrast-enhanced ultrasound-guided pleural biopsy specimens for
pleural tuberculosis. Intl J Infect Dis. 108:89–95. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rice JP, Seifert M, Moser KS and Rodwell
TC: Performance of the Xpert MTB/RIF assay for the diagnosis of
pulmonary tuberculosis and rifampin resistance in a low-incidence,
high-resource setting. PLoS One. 12(e0186139)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chinese Medical Association. Clinical
diagnosis standardof TB for
clinicaltechnologyoperation(TBvol-umes). People's Medical
Publishing House, 2005.
|
|
10
|
Jian S, Rong ZL and Baohua S: Diagnostic
value of pleural histopathology and pleural effusion in tuberculous
pleurisy. Western Med. 27:27–28. 2015.
|
|
11
|
Hooper C, Lee YC and Maskell N: BTS
Pleural Guideline Group. Investigation of a unilateral pleural
effusion in adults: British Thoracic Society pleural disease
guideline 2010. Thorax. 65:4–17. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Barnes TW, Morgenthaler TI, Olson EJ,
Hesley GK, Decker PA and Ryu JH: Sonographically guided
thoracentesis and rate of pneumothorax. J Clin Ultrasound.
33:442–446. 2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Defrancis N, Klosk E and Albano E:
Needlebiopsy of theparietalpleura. N Engl J Med. 252:948–949.
1995.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Benamore RE, Scott K, Richards CJ and
Entwisle JJ: Image guided pleura biopsy: Diagnostic yield and
complications. Clin Radiol. 61:700–705. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Christopher DJ, Schumacher SG, Michael JS,
Luo R, Balamugesh T, Duraikannan P, Pollock NR, Pai M and Denkinger
CM: Performance of Xpert MTB/RIF on pleural tissue for the
diagnosis of pleural tuberculosis. Eur Respir J. 42:1427–1429.
2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Diacon AH, Van de Wal BW, Wyser C, Smedema
JP, Bezuidenhout J, Bolliger CT and Walzl G: Diagnostic tools in
tuberculous pleurisy: A direct comparative study. Eur Respir J.
22:589–591. 2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Steingart KR, Schiller I, Horne DJ, Pai M,
Boehme CC and Dendukuri N: Xpert® MTB/RIF assay for
pulmonary tuberculosis and rifampicin resistance in adults.
Cochrane Database Syst Rev. 2014(CD009593)2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Blakemore R, Story E, Helb D, Kop J,
Banada P, Owens MR, Chakravorty S, Jones M and Alland D: Evaluation
of the analytical performance of the Xpert MTB/RIF assay. J Clin
Microbiol. 48:2495–2501. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Denkinger CM, Schumacher SG, Boehme CC,
Dendukuri N, Pai M and Steingart KR: Xpert MTB/RIF assay for the
diagnosis of extrapulmonary tuberculosis: A systematic review and
meta-analysis. Eur Respir J. 44:435–446. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Koegelenberg CF, Irusen EM, von
Groote-Bidlingmaier F, Bruwer JW, Batubara EM and Diacon AH: The
utility of ultrasound-guided thoracentesis and pleural biopsy in
undiagnosed pleural exudates. Thorax. 70:995–997. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Saeed M, Ahmad M, Iram S, Riaz S, Akhtar M
and Aslam M: A breakthrough for the diagnosis of tuberculous
pericarditis and pleuritisin less than 2 hours. Saudi Med J.
38:699–705. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Haijing Z, Chengyong L and Dongqing Z:
Application value of GeneXpert MTB/RIF system in rapid diagnosis of
tuberculous pleurisy). Beijing Med J. 38:739–741. 2016.
|
|
23
|
Sun W, Gu J, Bi K, Zhang Y, Shen MJ, Wang
Y and Fan L: Clinical performance of Xpert MTB/RIF on
contrast-enhanced ultrasound-guided core biopsy specimens for rapid
diagnosis of superficial tuberculous lymphadenitis in high TB
burden settings. Infection. 49:653–660. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gu Y, Wang G, Dong W, Li Y, Ma Y, Shang Y,
Qin S and Huang H: Xpert MTB/RIF and GenoType MTBDRplus assays for
the rapid diagnosis of bone and joint tuberculosis. Infect Dis.
36:27–30. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Yu C, Xuhui L and Liang F: Diagnostic
value of genexp ERT m TB/RIF in HIV negative urinary tuberculosis.
Chin J Tuberculosis. 39:1100–1106. 2017.
|
|
26
|
Bahr NC, Marais S, Caws M, van Crevel R,
Wilkinson RJ, Tyagi JS, Thwaites GE and Boulware DR: Tuberculous
Meningitis International Research Consortium. GeneXpert MTB/Rif to
diagnose tuberculous meningitis: Perhaps the first test but not the
last. Clin Infect Dis. 62:1133–1135. 2016.PubMed/NCBI View Article : Google Scholar
|