1. Introduction
Hashimoto's thyroiditis (HT) is considered to be the
reason for autoimmune Graves' disease that may eventually progress
to hypothyroidism; HT causes inflammation that affects the thyroid
gland and can lead to hypothyroidism. The condition is known as an
autoimmune disease, which describes the complex interplay between
predisposition from genetics/genes, and environmental factors and
immune disorders which may also be the cause. In this case, the
immune system of the body fails to differentiate the actual tissue
of the thyroid, which it is supposed to be protective, but
perceivably considers it as a type of foreign object and thus
relentlessly keeps attacking its tissue (1). This results in the activation of an
immune response, eventually leading to abnormal thyroid tissue,
which causes inflammation of the thyroid cells, resulting in the
very slow secretion of thyroid hormones. Clinically, the symptoms
of HT appear to be the same as those of hypothyroidism, including
but not confined, to a constant feeling of tiredness, an inability
to tolerate cold and weight gain. The diagnosis will be based on
the outcomes of thyroid function tests and serological markers
detecting the association between thyroid gland carriers and
antithyroid antibodies (2).
Additionally, during the gestation period in females affected by
HT, hormone replacement therapy is administered, which relieves
symptoms and prevents possible related complications. However, HT
indeed has profound implications on the quality of life of
patients; patients are destined to outlive their pathology with
appropriate and effective management for the malignancy. On the one
hand, the intricate pathomechanism, which is the core of Chinese
medicine, provides ample investigative aspects for the researchers.
On the other hand, possible research outcomes stimulate the
development of the unique, European-based pharmacopeia that will
help people cure their autoimmune disorders (3).
The mechanisms through which these genetic and
epigenetic factors contribute to the development of HT have been
identified as key factors in these complex phenomena. In addition,
research that establishes the association between genetic
predisposition and HT may be of value for determining which
individuals are genetically susceptible, and may also determine the
process of the disease pathogenesis. Clinicians are searching for
the specific gene variant which triggers this genetic condition and
for the genes which may function as risk factors for the condition
(4). Consequently, HT may
experience epigenetic regulation which differs from the normal DNA
sequence, although the DNA does not change. Therefore, knowledge of
the effects and countermeasures of these factors is a key
prerequisite in building a solid genome-environment connection. The
factor that modifies gene expression in heritable thyroid disorders
is rich in epigenetic mechanisms, and it operates through a variety
of mechanisms, which may be significant in the modification of
immune responses and thyroid function. Furthermore, the scientific
understanding of the mechanisms functioning at the level of the
gene and at the epigenetic level may help identify other novel
therapeutic targets that can be used for more successful
personalized approaches. The latter specific genetic and epigenetic
pathways, may be critical for the pathogenesis (complication
processes) of HT and may guide the development of new intervention
strategies which can be used to better manage autoimmune
pathologies than what has previously been possible. Consequently,
as a result, it can be comprehended that education at this level is
necessary, not only for mankind, but also for influencing the
development of treatment strategies (5).
The present review on HT and its genetic and
epigenetic markers aimed to contribute to the scientific
understanding of this disease and to further improve clinical
management. The present review provides an overview of currently
existing evidence on the genetic and epigenetic mechanisms of HT
(6). The present review aimed to
not only provide explanations of the possible disease-causal
pathways of the disease, but also to enhance the understanding of
the pre-existing and causative factors of the disease. Similarly,
the present review provides an assessment of the strength and
weakness of research on HT, in an aim to enhance the quality of
evidence. The present review also identifies inconsistencies and
discontinuities that can be sought in the field of research based
on the review of the existing secondary sources, thereby presenting
an opportunity for further analysis and conclusions. It is also
important to highlight the fact that utilizing these genetic and
epigenetic markers of HT opens a line of clinical relevance that
can be used for more decisive risk assessments and for the better
prediction of disease outcomes, as adequate therapeutic
interventions can be developed. It is hoped that he information
presented herein may expand the available knowledge of the disease,
which in turn may help to improve clinical expertise. This may also
help to encourage further practice and may improve quality of
treatment of the patients with this complex autoimmune disease
(7).
2. Definition of Hashimoto's
thyroiditis
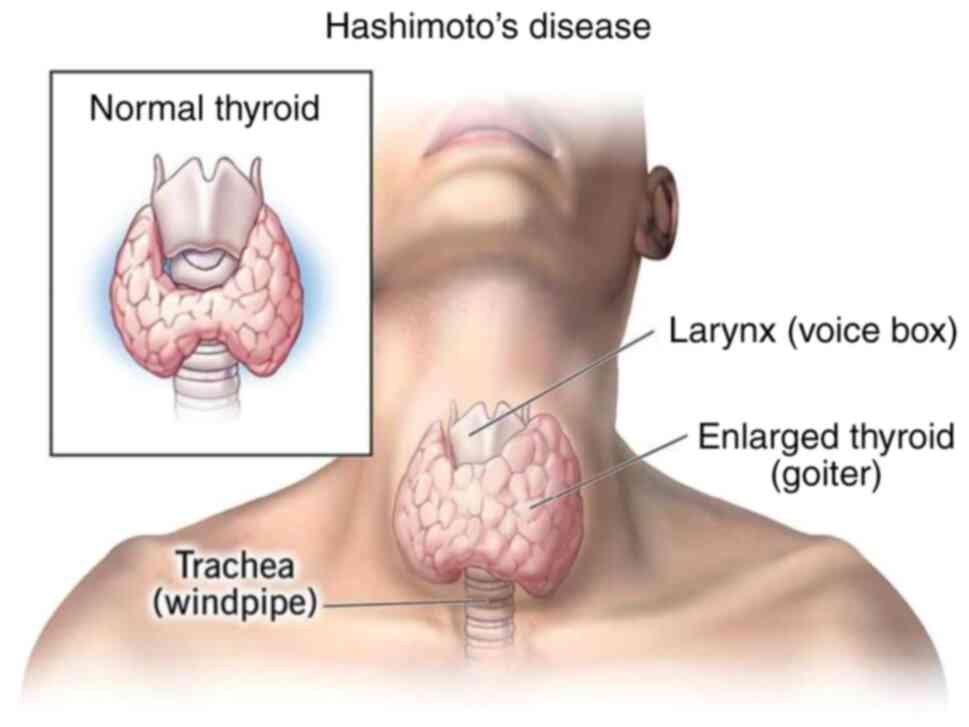
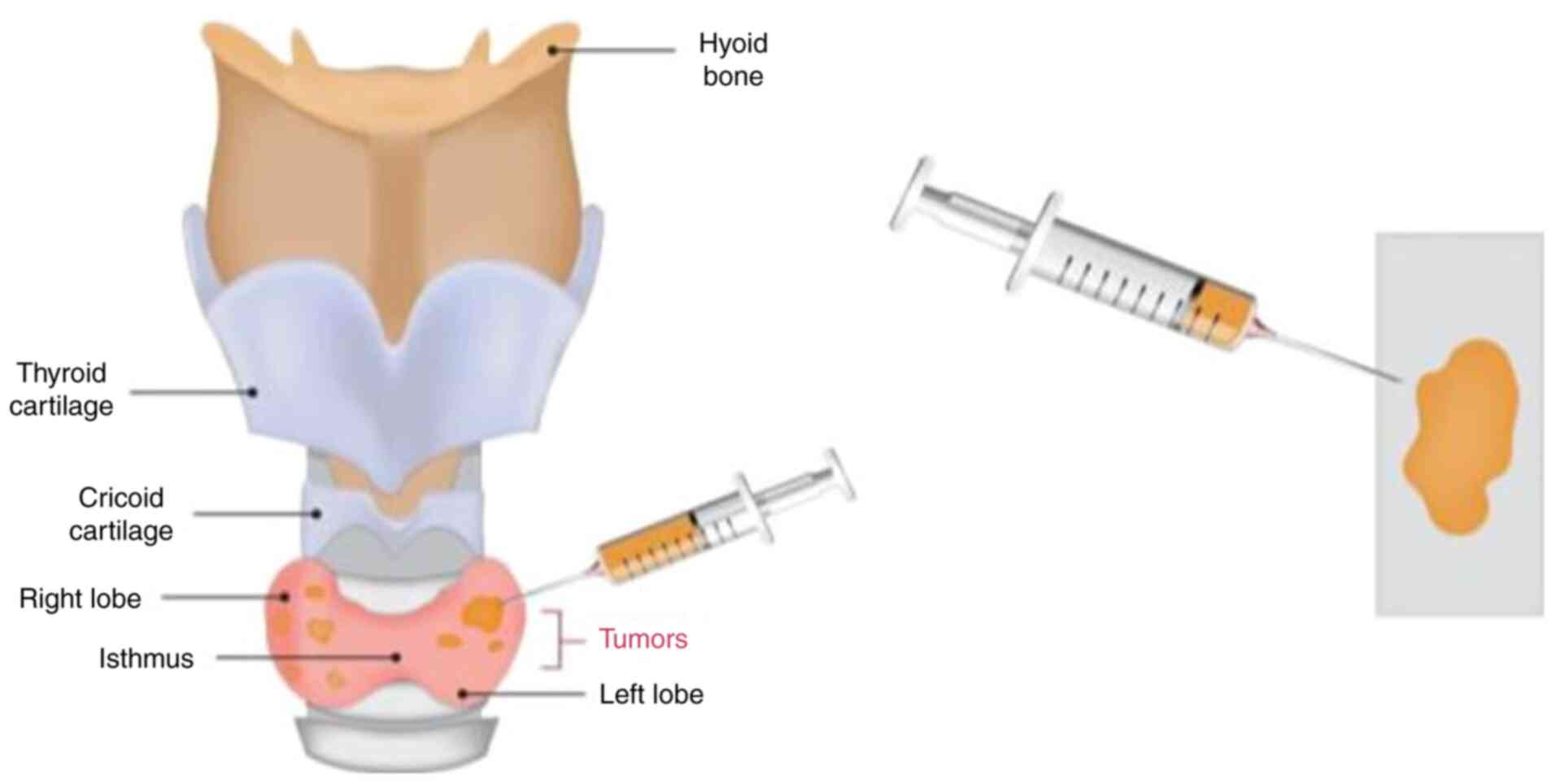
HT is the most frequent autoimmune disorder of the
thyroid gland and is the leading cause of hypothyroidism in
iodine-sufficient areas worldwide. Approximately 20-30% of patients
suffers from HT, the cause of which is considered to be a
combination of genetic susceptibility and environmental factors
that causes the loss of immunological tolerance. This leads to an
autoimmune attack of the thyroid tissue and the development of the
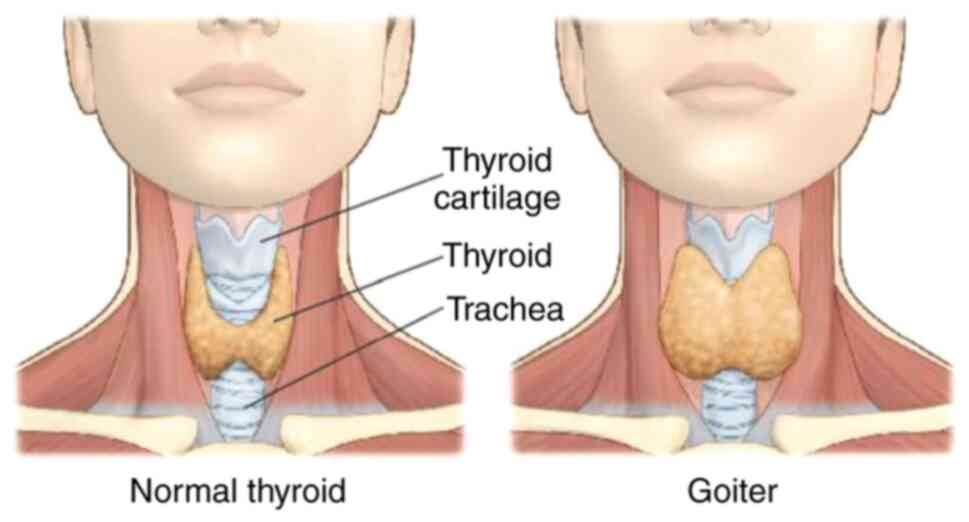
disease. The thyroid gland becomes inflamed in this type of
autoimmune disease. An image of the thyroid gland in both normal
conditions and in HT conditions is presented in Fig. 1 (8).
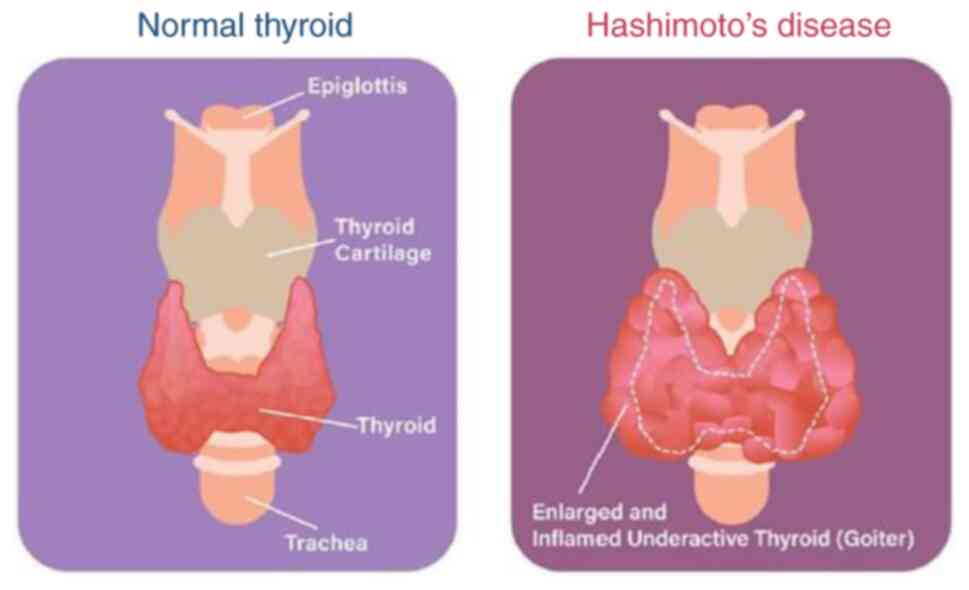
With this illness, it is not the gland that produces
the thyroid hormone whose production is damaged; the immune system
of the body targets the gland, attacking it gradually until it
reaches the stage of complete destruction over a course of time. An
image of the differences between the normal and affected thyroid
gland is presented in Fig. 2.
The inhibition of iodine influx deadlocks the
capability of the immune system and the consequence is a
hypofunction of the gland, directly related to the decrease of the
amount of produced hormones, the equilibrium of which is followed
by hypothyroidism, which is, in turn, leads to a deterioration of
health (9). HY may predispose to
goitrous hypothyroidism, which involves an adequate of iodine; this
condition mainly affects middle-aged females. However, it can also
occur in males and among the elderly of both sexes. The symptoms
mentioned above are instrumental in diagnosis of the disease via
clinical evaluation, testing for thyroid function, and the search
for autoimmune markers, such as anti-thyroid markers. Treatment
approaches involve strategies which lead to the secretion of normal
hormone levels and maintain the same clinical state via ongoing
substitute therapy throughout life (9). Despite the fact that the disease is
chronic and it requires proper medical attention for a life-long
period, it is possible to maintain a normal lifestyle, and numerous
patients with the disease live healthy lives (1).
3. Genetic and epigenetic markers in
autoimmune diseases
HT is a complex disease combining genetic and
epigenetic factors affecting autoimmunity development; it is well
known as a susceptibility factor for the development of other
autoimmune diseases (4).
Genetic markers. Genetic
predisposition
In the majority of autoimmune diseases, it is
considered that inheritance plays a crucial, including the
existence of genetic mutations. On the other hand, gene variation
is highly implicated in autoimmune diseases; subjects vulnerable to
such diseases carry increased levels of susceptibility genes
(9).
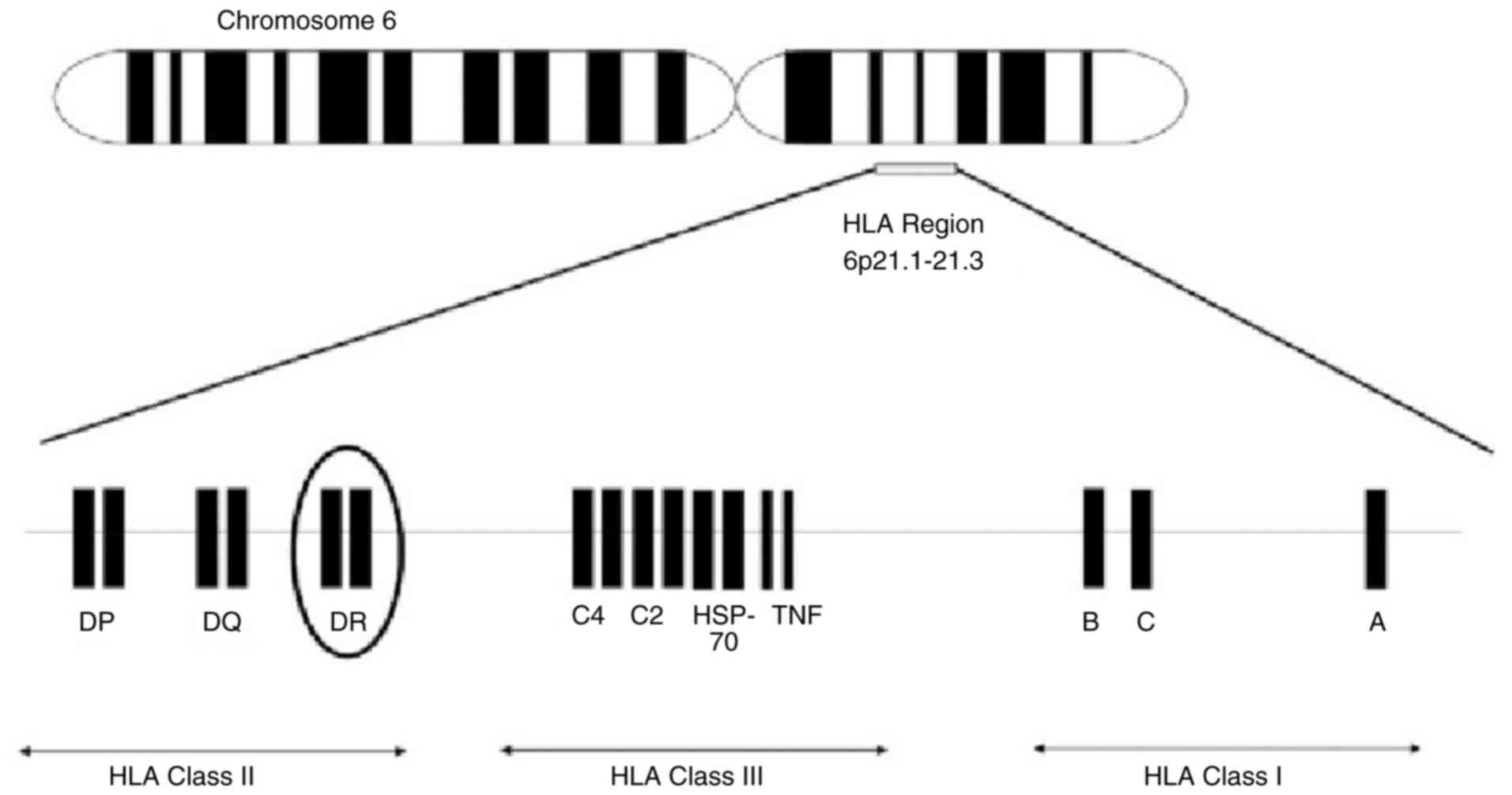
Human leukocyte antigen (HLA) genes. One of
the most powerful tools for fighting infectious diseases is,
without a doubt, the HLA gene located on the chromosome 6 (Fig. 3) (10); the HLA genes constitute the
strongest and the most common, if not the only common,
susceptibility factor for numerous autoimmune diseases, such as
type 1 diabetes, celiac disease and rheumatoid arthritis; they
continue to be the most extensively studied genes with relation to
immunity (10).
Non-HLA genes. In addition to the HLA genes,
the non-HLA genes, can be as essential as the HLA genes for the
analysis of the disease. Part of these analyses would be genetic
and these genes would mainly promote immune functioning, as well as
the regulation of inflammation involved in immunity. Some examples
of such genes are protein tyrosine phosphatase, non-receptor type
22, insulin gene, cytotoxic T-lymphocyte-associated protein 4,
nucleotide-binding oligomerization domain containing 2 and tumor
necrosis factor) (10).
Gene-environment interactions. It was after
the genealogy constituent was discovered that a new ecological base
was added to the risk of being predisposed to autoimmune diseases.
The environmental factors involved include diet and nutrition,
toxins and pollutants, stress and mental health, sun exposure and
physical activity. Gene-environment interactions produce elicitors,
which increase the risk of developing autoinflammatory diseases
(11).
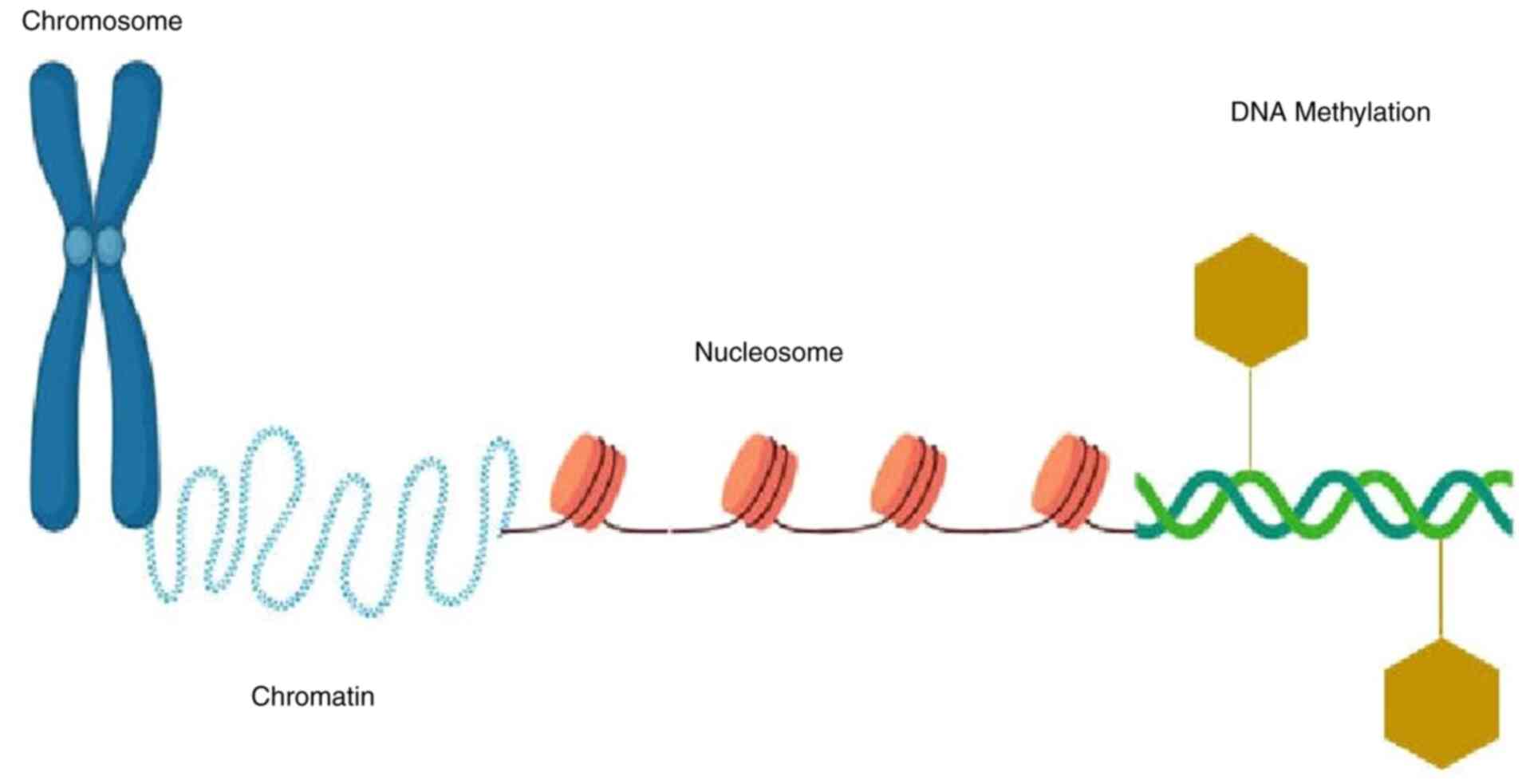
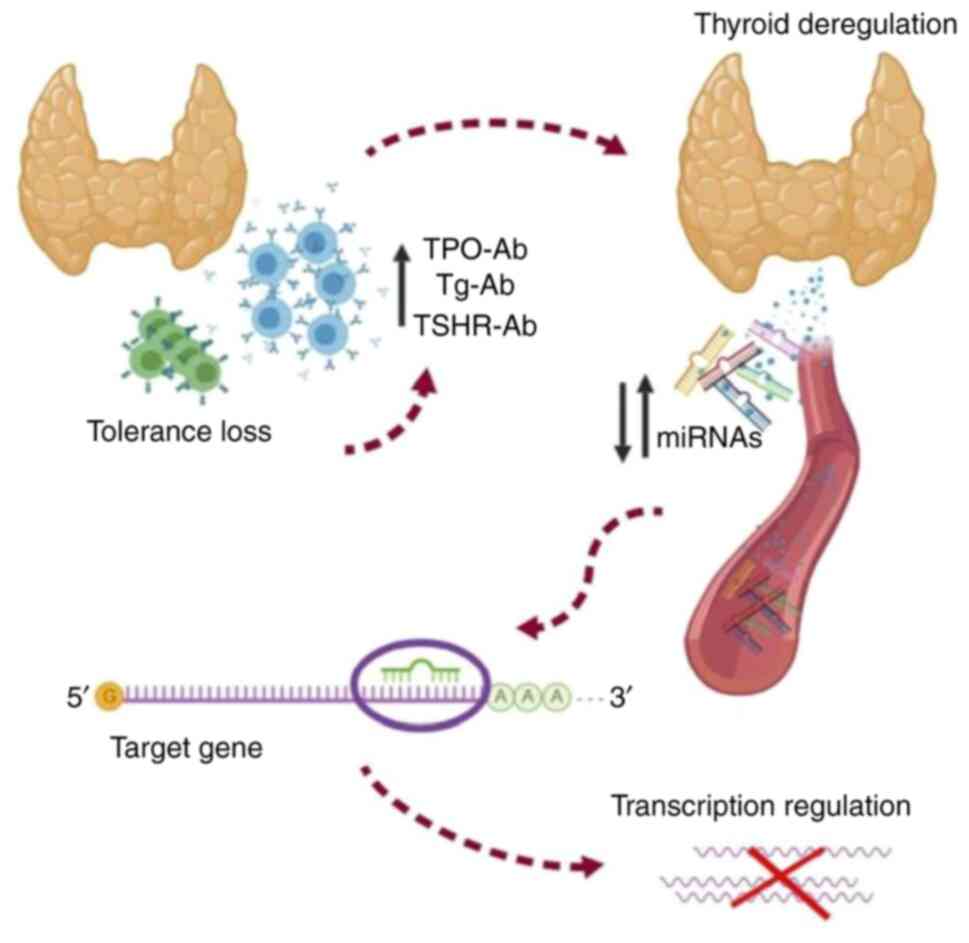
Epigenetic markers. DNA
methylation
DNA methylation, which adds a methyl group to the
DNA on the cytosine base primarily at cytosine-guanine (CpG)
dinucleotides (two nucleotides), is the fundamental building block
of epigenetic modification. HT-associated abnormal DNA methylation
was noted with the genes involved in the thyroid function and
immunity regulation involves the target genes of these epigenetic
changes (12). Hypermethylation of
the thyroid specific gene, including thyroid-stimulating hormone
(TSH) receptor and thyroid peroxidase may serve as a predisposing
cause to thyroid deficiency in patients with HT (13). A schematic illustration of DNA
methylation is presented in Fig.
4.
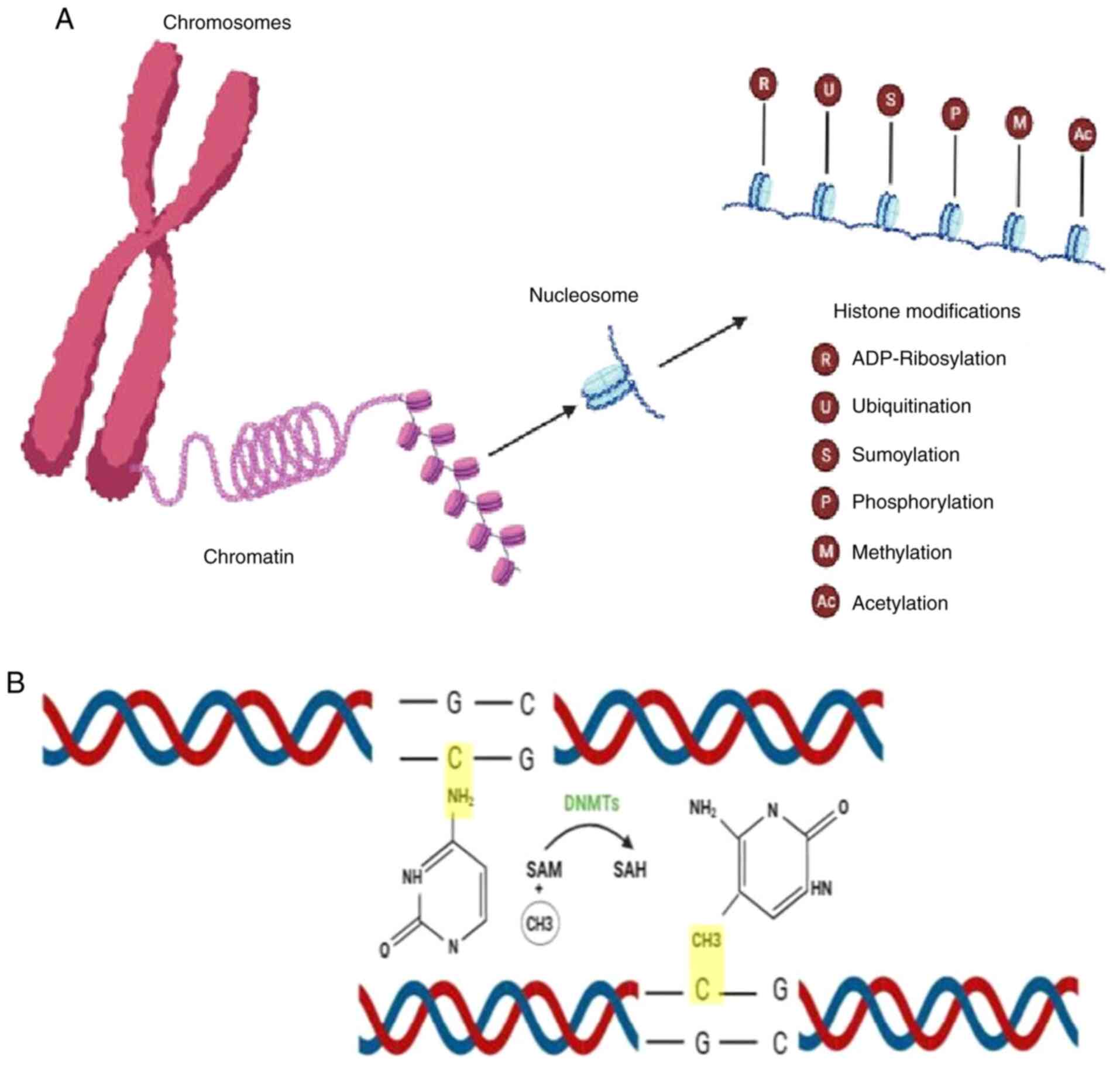
Histone modifications. An essential element
of the epigenetic control of gene expression is histone
modification. Histones are considered to be proteins that
contribute to nucleosomes, which are structural units of DNA. The
abnormal modifications of histone, for instance, the acetylation
and the methylation which affect the chromatin's structure and the
transcription of genes, may be associated with HT. The epigenetic
mechanisms of histone modifications may exert effects on the
expression of thyroid genes associated with auto-immunity and
inflammatory responses (14,15). A
schematic illustration of the modification of histones is presented
in Fig. 5.
MicroRNAs (miRNAs/miRs). Various genes
accelerate the development of HT. For example, altered levels of
miRNAs can modulate the immune responses, as well as the
proliferation and apoptosis of thyroid cells in HT. To identify
miRNA expression levels in the thyroid gland in HT, the technique
used is known as miRNA microarray analysis using RNA obtained from
primary HT cases, three cases of HT and papillary thyroid cancer,
and three normal thyroid cases, as previously described (16). A representative image of the role of
miRNAs in thyroid regulation is presented in Fig. 6.
4. Significance and relevance of Hashimoto's
thyroiditis in the context of autoimmune diseases
HT is one of the most common autoimmune diseases
that affects thousands of individuals worldwide. Women are the most
vulnerable to this disease. As it is indicated as a common
autoimmune disease, this reduces the importance of convincing the
public to improve awareness and proper diagnosis. Hashimoto's
disease affects the normal function of the thyroid gland, which is
manifested as an inflammation caused by an attack on the thyroid
tissue by the immune system which leads to its destruction. In this
condition, the body tends to produce autoantibodies that react to
its own tissues. This is the main reason affected individuals are
tested for anti-thyroid peroxidase antibodies and
anti-thyroglobulin antibodies (17,18).
Association with other autoimmune
diseases
There is frequently a situation in HT when the
disease occurs simultaneously with other autoimmune disease, such
as Graves' disease, rheumatoid arthritis, type 1 diabetes and
celiac disease. This association thus uncovers common genetic
predispositions and immunological components, which are disordered
among the autoimmune diseases (19).
Clinical manifestations and impact on
health
HT can eventually develop into hypothyroidism; the
most common symptoms in adults are fatigue, lethargy, cold
intolerance, weight gain, constipation, a change in voice and dry
skin; however, the clinical presentation can differ with age and
sex, among other factors, as well as cognitive impairments. HT can
not only cause not only thyroid-related symptoms, but also some
autoimmune-related complications, including the enlargement or
presence of nodules in the thyroid gland, as well as a very low
percentage of thyroid hormones. Furthermore, persistent or
inappropriately managed hypothyroidism can have severe detrimental
effects on human health and on the wellbeing of the affected
individual (20).
Diagnostic and therapeutic
implications
The diagnosis of HT is mostly based on an
ultrasonography, which is a useful and essential tool for diagnosis
based on the characteristics of the disease. In the differential
diagnosis of thyroid nodules, ultrasound-guided fine-needle biopsy
is an effective method used to distinguish HT from other thyroid
disorders by the histological features of HT. A notable and recent
advancement is that non-invasive ultrasound-based methods have
supplemented fine-needle aspiration to diagnose HT under more
complex conditions. The development of screening tests for thyroid
function and antithyroid antibodies has enabled the rapid detection
of the disease during the early stages. Primary treatment brings
relief of the symptoms and prevents long-term complications is
thyroid hormone replacement with levothyroxine (21).
5. Pathophysiology of Hashimoto's
thyroiditis
The clinical characteristics of Hashimoto's disease
are a result of the interplay and interaction of the genetic and
environmental components that underlie and provoke the disease
(HT). Moreover, HT is an intricate autoimmune response manifested
by immune-mediated inflammation, thyroid tissue destruction and
ultimately, hypothyroidism (22,23).
Genetic predisposition
Individuals with a family history of autoimmune
diseases, particularly HT are more than likely to suffer from the
same condition. Specific gene variants, particularly in the HLA
region and the genes outside the HLA, involved in immune function,
can be traced back to be the genetic risk for HT (9).
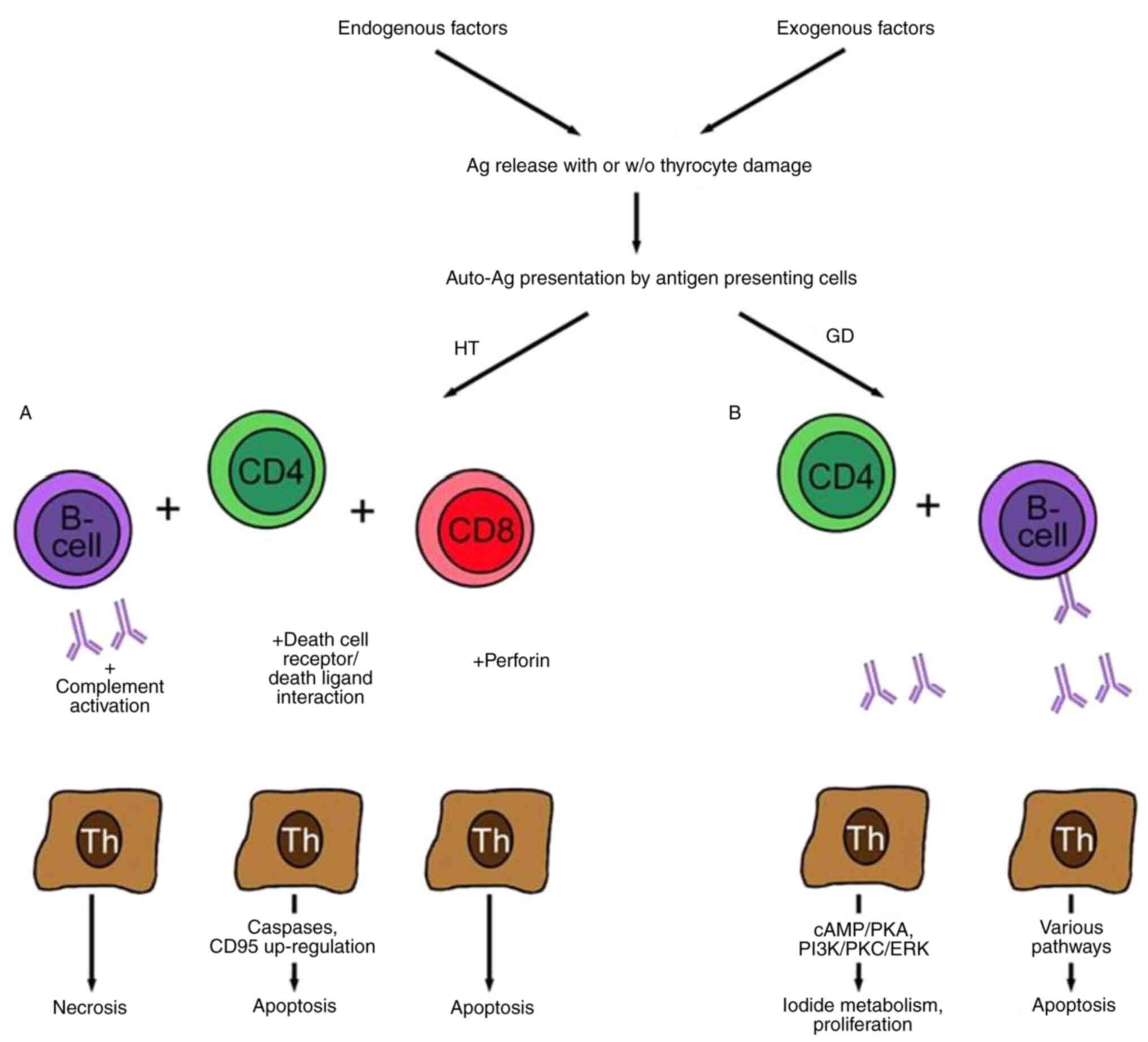
Immune dysregulation
HT is marked by a particular type of immune-mediated
inflammation that targets the thyroid. Predisposed subjects who
encounter environmental triggers, such as viral infections or
stressors have an altered response. The immune system attacks its
own thyroid cells, mistaking them as foreign bodies. As a result,
the process of autoreactive T-cell activation is triggered, and
these cells begin penetrating the thyroid gland where they identify
thyroid-specific antigens known as thyroglobulin and thyroid
peroxidase (24).
Thyroid inflammation
The thyroid gland is one of the organs most affected
by autoimmune processes; numerous patients with HT seek medical
advice on lifestyle changes and dietary modifications in order to
improve and maintain their thyroid function. In HT, T-cells
stimulate B-cells to produce antinuclear antibodies, such as
anti-thyroid peroxidase and anti-thyroglobulin antibodies. The
autoantibodies, and the pro-inflammatory cytokines released by the
activated immune cells induce secondary inflammation within the
gland. Due to the infiltration of lymphocytes in the thyroid
tissue, the formation of lymphoid follicles is generated, which in
turn leads to the enhancement of the inflammatory response
(25).
Thyroid damage
Disruptive inflammation and self-immune reactions
against thyroid connective tissues lead to the continuous
destruction of thyroid follicles, resulting in their inefficiency
to perform their function of thyroid hormone synthesis. With
thyrocyte cells being eliminated, thyroglobulin and thyroid
peroxidase are released into the bloodstream, contributing to
higher levels of the two thyroid autoantibodies in serum (26).
Hypothyroidism
Hypothyroidism is a common condition of thyroid
hormone deficiency, which is readily diagnosed and managed;
however, if left untreated, it can be potentially fatal in severe
cases. The definition of hypothyroidism is based on statistical
reference ranges of the relevant biochemical parameters and is
increasingly a matter of debate. The clinical manifestations of
hypothyroidism range from life threatening to no signs or symptoms.
The most common symptoms in adults are fatigue, lethargy, cold
intolerance, weight gain, constipation, a change in voice and dry
skin, although the clinical presentation can differ with age and
sex, among other factors, such as genetic factors, environmental
factors, hormonal changes and nutritional status. The standard
treatment is thyroid hormone replacement therapy with levothyroxine
(23). HT is the most common cause
of hypothyroidism in iodine-sufficient areas worldwide. An
excessive iodine intake is associated with a higher prevalence of
autoimmune thyroiditis; however, a lower prevalence of the
condition is observed in iodine-deficient areas. For example, in
China, autoimmune thyroiditis is observed in 0.3% of individuals in
mildly iodine-deficient areas, while it is observed in 1.3% of
individuals with excessive iodine intake (27).
Hashimoto's encephalopathy
Hashimoto's encephalopathy or encephalitis is a very
rare complication of HT. Neurological complications are sometimes
associated with thyroid dysfunction, although patients with this
type of encephalopathy are usually euthyroid. It is treatable,
steroid-responsive, progressive or relapsing encephalopathy
associated with an elevation in the levels of of thyroid-specific
autoantibodies (28).
Hashimoto's ophthalmopathy
Thyroid-associated orbitopathy usually occurs in
Graves's disease with hyperthyroidism, and sometimes, in euthyroid
and hypothyroid patients. Since the majority of euthyroid and
hypothyroid patients with orbitopathy are thyrotropin receptor
antibody (TRAb)-positive, they are diagnosed as having euthyroid
Graves' disease or hypothyroid Graves' disease. When euthyroid and
hypothyroid patients with orbitopathy are TRAb-negative, but have
HT, Hashimoto's ophthalmopathy may be considered. As patients with
HT test negative for TRAb, other autoantibodies against an eye
muscle antigen, such as calsequestrin, flavoprotein, or G2s are
considered to be involved (29).
6. Diagnosis of Hashimoto's thyroiditis
The diagnosis of HT often results from a synthesis
of a clinical examination, the examination of TSH levels and the
assay of anti-thyroid auto-antibodies (8). A description of the diagnostic
measures used for HT is presented below:
Clinical evaluation
Although the diagnosis of HT usually begins with a
comprehensive medical history and physical examination by a health
care provider, sometimes, other imaging and laboratory tests are
performed to help confirm diagnosis. The appearance of certain
symptoms of hypothyroidism, such as exhaustion, weight gain, cold
intolerance, constipation, dry skin and irregular menstruation in
women, may trigger more attacks, which will increase the likelihood
of further investigations (8).
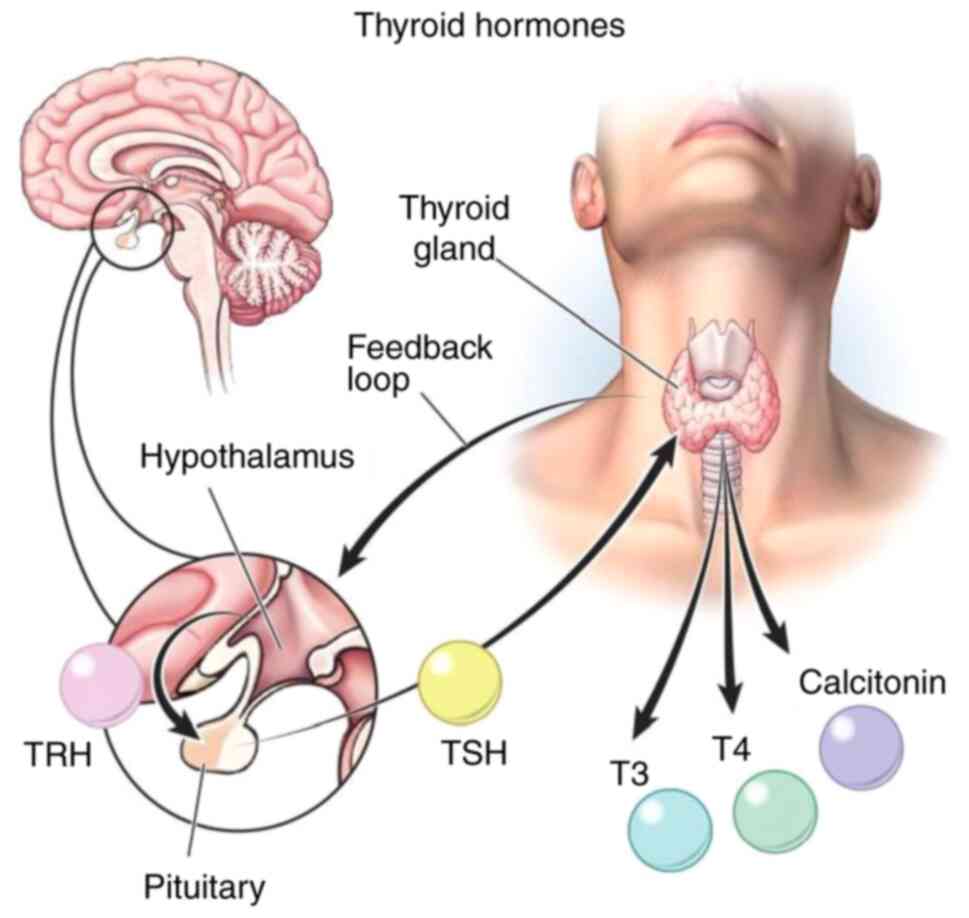
Thyroid function tests
The most fundamental investigation is thyroid
function tests used to assess the levels of hormones (Fig. 7) produced by the thyroid and are
used in the discovery of the thyroid disorder (27). The most commonly performed tests are
the following:
TSH. TSH is considered to be the most
sensitive and specific indicator of thyroid function as compared to
other available thyroid tests. High TSH levels will most likely
occur due to HT, the hereditary form of thyroid disease (30).
Free thyroxine (FT4). T4 is referred to as
FT4 and represents the amounts of thyroxine, the primary hormone
that the thyroid gland secretes. In the case of HT, the FT4 level
tends to be abnormal or low, depending on the stage of the disease
(30).
Triiodothyronine (T3). The T3 levels may be
screened as well; however, as it is frequently found that the T3
levels are usually within the normal range in patients with
hyperthyroidism (30).
Autoimmune thyroid antibodies
The evaluation of autoimmune thyroid antibodies
(Fig. 8) is a strategy used to
identify the factors that have triggered HT attacks and rule out
other causes of hypothyroidism. The following antibodies are
usually assessed (31).
Anti-thyroid peroxidase antibodies. Thyroid
peroxidase bound antibodies (TPO Ab) can be found in >90% of
individuals with HT, and it has now been proven that their
existence defines the disease (32).
Anti-thyroglobulin antibodies. HT may, to a
certain extent, also be related to the presence of a thyroglobulin
antibody, although these are generally less specific than TPO
antibodies (32).
Thyroid-stimulating immunoglobulins (TSI).
The ability to differentiate HT from Graves' disease, another
autoimmune thyroid condition, is aided by the presence of TSI
antibodies. Similar to patients with HT, individuals with Graves'
disease also experience hypothyroidism (33).
Imaging studies
Two-dimensional (2D) imaging may be done with the
aid of a thyroid ultrasound to analyze the size and shape of the
thyroid gland. In HT, the ultrasound may demonstrate either diffuse
or heterogeneous echogenicity of the thyroid gland, bilateral
thyroid enlarge (goiter) or presence of thyroid nodules (2).
Fine-needle aspiration (FNA) biopsy
(if indicated)
During an ultrasound examination of thyroid nodules,
a biopsy procedure is often administered to diagnose thyroid
abnormality if deemed necessary (Fig.
9) (2).
Clinical criteria
Clinical factors, such as goiter (Fig. 10) or the family history of a
patient are also crucial, as they may be useful to assist to
diagnose HT as well, although they are not very specific to this
disease (28).
7. Treatment of Hashimoto's thyroiditis
The management of HT involves medication for thyroid
hormone replacement to control hypothyroidism, lifestyle changes,
keen regular monitoring and appropriate management for symptom
relief and improvement in the life quality. With appropriate
treatment, related complications and risk factors can be reduced.
Collaborative treatment requires various healthcare professionals,
and patients and their care team have to work together to
successfully manage HT (27,34).
Thyroid hormone replacement
therapy
The treatment of HT-induced hypothyroidism requires
three steps: First, the establishment of a correct diagnosis by
measuring thyroid hormone and thyrotropin levels should be carried
out. Second, the replacement of insufficient thyroid hormones is
required. The patients are treated with synthetic T4 medications,
such as levothyroxine (35).
In the majority of cases, levothyroxine is received
by mouth once per day, the majority of which have been prescribed
to be taken in the morning on an empty stomach to produce optimum
absorption levels (35). It is
necessary to adjust the levothyroxine dose based on personal
factors, including age, weight, severity and other health disorders
(35). Periodic blood examinations
that include TSH stability are necessary to control levothyroxine
dosing, and to ensure that thyroid hormone levels are within the
target range (35).
Lifestyle modifications
Patients with HT can benefit by adopting a healthy
lifestyle, which should include a balanced diet, regular exercise,
stress management and getting a sufficient amount of sleep.
Diet-related factors can encompass sufficient iodine supply (if
deficient), avoiding excess supplementation, and consuming minimal
amounts of goitrogenic foods which can aggravate the condition
(e.g., cruciferous vegetables). Smoking cessation is necessary due
to the fact that it may aggravate autoimmune thyroid diseases, as
well as the passage of thyroid hormones through the metabolism
process.
Monitoring and follow-up
The dose of the medication will be adjusted as per
the TSH levels, and patients should be monitored regularly for
their TSH levels. Depending on the result, the dose of
levothyroxine is adjusted accordingly (36). A follow-up appointment with an
endocrinologist at 8-12 weeks following the start of treatment
should be scheduled, and patients can monitor their symptoms and
TSH levels by frequently visiting their physician. Patients and
physicians should work together to ensure the successful management
of the disease and to maintain the patient's health (36).
Management of symptoms
In addition to thyroid hormone replacement therapy,
symptomatic management may be required to reduce other diseased
aspects (fatigue, weight gain, over-dried and cold-intolerant skin,
and constipation) (36). When
patients also have symptoms of depression and mood disturbances,
mental health services are recommended (36).
Complications
In patients with HT, tests for complications and
comorbidities that are associated with hypothyroidism may be
considered, such as hyperlipidemia, cardiovascular diseases and
osteoporosis. The therapy of these diseases may require other
tactics, such as consuming fewer fat foods or tailoring
cardiovascular risk components, as well as taking calcium/vitamin D
supplements (37).
Patient education and support
Making patients aware of the nature of HT, the
importance of adhering to medication, and the need for a
considerable amount of follow-up is critical. Patient advocacy
groups and online help sources can share knowledge, inspiration and
help patients with HT bear these challenges (38).
8. Conclusion and future perspectives
In conclusion, the study of the genetic and
epigenetic markers of HT helps to understand the disease mechanisms
and enhances the diversity of diagnostic and treatment options.
Through gene investigations, some exclusive variants in genes such
as HLA and non-HLA gene variants have been identified, thus
highlighting how genetics is a precursor to the development of the
disease and its interactive role with immunity, thyroid functions
and cytokine signaling. Of note, epigenetic mechanisms, such as DNA
methylation, histone modifications and miRNAs play a critical role
in gene expression and the regulation of the immune system. The
dysregulation of epigenetic processes, and their role in the
development of HT is becoming clearer, which paves the way for
treatment by way of intervention. The combination of genetic and
epigenetic data could provide a novel strategy for the health
management of patients, including diagnostic, prognostic and
treatment approaches that are tailored to individual patients.
Furthermore, by tracing how genes, the environment and epigenetics
interact, doctors are better able to account for the challenges
associated with HT and can thus develop more specific and effective
strategies for controlling HT in individuals. Nevertheless, further
studies are required to understand, confirm and enhance the
conciseness of the previously identified genetic and epigenetic
markers, explore their functional significance and search for more
possible treatments. Strategic alliance between basic scientists,
clinicians and bioinformaticians is mandatory in order to translate
these outcomes to clinical practice and develop the necessary tools
that can be used improve the quality of lives of patients with HT.
In brief, researching genetic and epigenetic markers of HT is an
encouraging direction which can be used to advance both the
knowledge of a complex autoimmune diseases and improve the quality
of care for patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding received.
Availability of data and materials
Not applicable.
Authors' contributions
All authors (SSA, HOS and AFS) conceptualized the
study. SSA wrote the original draft of the manuscript. HOS and AFS
provided critical revisions. All authors contributed to manuscript
revision and have read and approved the final version of
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Weetman AP: An update on the pathogenesis
of Hashimoto's thyroiditis. J Endocrinol Invest. 44:883–890.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ralli M, Angeletti D, Fiore M, D'Aguanno
V, Lambiase A, Artico M, de Vincentiis M and Greco A: Hashimoto's
thyroiditis: An update on pathogenic mechanisms, diagnostic
protocols, therapeutic strategies, and potential malignant
transformation. Autoimmun Rev. 19(102649)2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mincer DL and Jialal I: Hashimoto
Thyroiditis. In: StatPearls. StatPearls Publishing, Treasure
Island, FL, 2024.
|
|
4
|
de Oliveira Andrade LJ, de Oliveira LM, de
Oliveira LCM and de Oliveira GCM: Bioinformatics unravels the
epigenetic mechanisms of hashimoto's thyroiditis: Deciphering
molecular complexity. medrxiv: doi: https://doi.org/10.1101/2023.07.25.23293163.
|
|
5
|
Pyzik A, Grywalska E, Matyjaszek-Matuszek
B and Roliński J: Immune disorders in Hashimoto's thyroiditis: What
do we know so far? J Immunol Res. 2015(979167)2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Danailova Y, Velikova T, Nikolaev G,
Mitova Z, Shinkov A, Gagov H and Konakchieva R: Nutritional
management of thyroiditis of hashimoto. Int J Mol Sci.
23(5144)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mikulska AA, Karaźniewicz-Łada M,
Filipowicz D, Ruchała M and Główka FK: Metabolic characteristics of
hashimoto's thyroiditis patients and the role of microelements and
diet in the disease management-an overview. Int J Mol Sci.
23(6580)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Caturegli P, De Remigis A and Rose NR:
Hashimoto thyroiditis: Clinical and diagnostic criteria. Autoimmun
Rev. 13:391–397. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ihnatowicz P, Drywień M, Wątor P and
Wojsiat J: The importance of nutritional factors and dietary
management of Hashimoto's thyroiditis. Ann Agric Environ Med.
27:184–193. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Casto C, Pepe G, Li Pomi A, Corica D,
Aversa T and Wasniewska M: Hashimoto's thyroiditis and graves'
disease in genetic syndromes in pediatric age. Genes (Basel).
12(222)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Aversa T, Corica D, Zirilli G, Pajno GB,
Salzano G, De Luca F and Wasniewska M: Phenotypic expression of
autoimmunity in children with autoimmune thyroid disorders. Front
Endocrinol (Lausanne). 10(476)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bender J: DNA methylation and epigenetics.
Annu Rev Plant Biol. 55:41–68. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Jones PA and Takai D: The role of DNA
methylation in mammalian epigenetics. Science. 293:1068–1070.
2001.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lennartsson A and Ekwall K: Histone
modification patterns and epigenetic codes. Biochim Biophys Acta.
1790:863–868. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhang Y, Sun Z, Jia J, Du T, Zhang N, Tang
Y, Fang Y and Fang D: Overview of histone modification. Adv Exp Med
Biol. 1283:1–6. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zadeh-Vakili A, Faam B, Afgar A, Razmpoosh
E, Zarkesh M and Amouzegar A: A systematic review of dysregulated
microRNAs in Hashimoto's thyroiditis. Endocrine. 84:800–811.
2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Brom VC, Burger C, Wirtz DC and Schildberg
FA: The role of immune checkpoint molecules on macrophages in
cancer, infection, and autoimmune pathologies. Front Immunol.
13(837645)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
van Zuuren EJ, Albusta AY, Fedorowicz Z,
Carter B and Pijl H: Selenium supplementation for Hashimoto's
thyroiditis. Cochrane Database Syst Rev.
2013(CD010223)2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Boelaert K, Newby PR, Simmonds MJ, Holder
RL, Carr-Smith JD, Heward JM, Manji N, Allahabadia A, Armitage M,
Chatterjee KV, et al: Prevalence and relative risk of other
autoimmune diseases in subjects with autoimmune thyroid disease. Am
J Med. 123:183.e1–e9. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Özen S, Berk Ö, Şimşek DG and Darcan S:
Clinical course of Hashimoto's thyroiditis and effects of
levothyroxine therapy on the clinical course of the disease in
children and adolescents. J Clin Res Pediatr Endocrinol. 3:192–197.
2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Berghi NO: Immunological mechanisms
implicated in the pathogenesis of chronic urticaria and Hashimoto
thyroiditis. Iran J Allergy Asthma Immunol. 16:358–366.
2017.PubMed/NCBI
|
|
22
|
Chaker L, Razvi S, Bensenor IM, Azizi F,
Pearce EN and Peeters RP: Hypothyroidism. Nat Rev Dis Primers.
8(30)2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Taheri M, Eghtedarian R, Dinger ME and
Ghafouri-Fard S: Dysregulation of non-coding RNAs in autoimmune
thyroid disease. Exp Mol Pathol. 117(104527)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Fariduddin MM and Singh G: Thyroiditis.
In: StatPearls. StatPearls Publishing, Treasure Island, FL,
2024.
|
|
25
|
Bogusławska J, Godlewska M, Gajda E and
Piekiełko-Witkowska A: Cellular and molecular basis of thyroid
autoimmunity. Eur Thyroid J. 11(e210024)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ragusa F, Fallahi P, Elia G, Gonnella D,
Paparo SR, Giusti C, Churilov LP, Ferrari SM and Antonelli A:
Hashimotos' thyroiditis: Epidemiology, pathogenesis, clinic and
therapy. Best Pract Res Clin Endocrinol Metab.
33(101367)2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Biondi B, Cappola AR and Cooper DS:
Subclinical hypothyroidism: A review. JAMA. 322:153–160.
2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Akamizu T and Amino N: Hashimoto's
Thyroiditis. MDText.com, Inc., South Dartmouth, MA, 2000.
|
|
29
|
Radetti G: Clinical aspects of Hashimoto's
thyroiditis. Endocr Dev. 26:158–170. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Malandrini S, Trimboli P, Guzzaloni G,
Virili C and Lucchini B: What about TSH and anti-thyroid antibodies
in patients with autoimmune thyroiditis and celiac disease using a
gluten-free diet? A systematic review. Nutrients.
14(1681)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rayman MP: Multiple nutritional factors
and thyroid disease, with particular reference to autoimmune
thyroid disease. Proc Nutr Soc. 78:34–44. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Dong YH and Fu DG: Autoimmune thyroid
disease: Mechanism, genetics and current knowledge. Eur Rev Med
Pharmacol Sci. 18:3611–3618. 2014.PubMed/NCBI
|
|
33
|
Osowiecka K and Myszkowska-Ryciak J: The
influence of nutritional intervention in the treatment of
Hashimoto's thyroiditis-a systematic review. Nutrients.
15(1041)2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Allelein S, Feldkamp J and Schott M:
Autoimmune diseases of the thyroid gland. Internist (Berl).
58:47–58. 2017.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
35
|
Jiang H, Tian Y, Yan W, Kong Y, Wang H,
Wang A, Dou J, Liang P and Mu Y: The prevalence of thyroid nodules
and an analysis of related lifestyle factors in Beijing
communities. Int J Environ Res Public Health.
13(442)2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Guldvog I, Reitsma LC, Johnsen L, Lauzike
A, Gibbs C, Carlsen E, Lende TH, Narvestad JK, Omdal R, Kvaløy JT,
et al: Thyroidectomy versus medical management for euthyroid
patients with Hashimoto disease and persisting symptoms: A
randomized trial. Ann Intern Med. 170:453–464. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pradeep PV, Ragavan M, Ramakrishna BA,
Jayasree B and Skandha SH: Surgery in Hashimoto's thyroiditis:
Indications, complications, and associated cancers. J Postgrad Med.
57:120–122. 2011.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Abbott RD, Sadowski A and Alt AG: Efficacy
of the autoimmune protocol diet as part of a multi-disciplinary,
supported lifestyle intervention for Hashimoto's thyroiditis.
Cureus. 11(e4556)2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Cavalli G and Heard E: Advances in
epigenetics link genetics to the environment and disease. Nature.
571:489–499. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Kimura H: Histone modifications for human
epigenome analysis. J Hum Genet. 58:439–445. 2013.PubMed/NCBI View Article : Google Scholar
|