|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
Statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Girard L, Rodriguez-Canales J, Behrens C,
Thompson DM, Botros IW, Tang H, Xie Y, Rekhtman N, Travis WD,
Wistuba II, et al: An expression signature as an aid to the
histologic classification of non-small cell lung cancer. Clin
Cancer Res. 22:4880–4889. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nizzoli R, Tiseo M, Gelsomino F,
Bartolotti M, Majori M, Ferrari L, De Filippo M, Rindi G, Silini
EM, Guazzi A and Ardizzoni A: Accuracy of fine needle aspiration
cytology in the pathological typing of non-small cell lung cancer.
J Thorac Oncol. 6:489–493. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Osmani L, Askin F, Gabrielson E and Li QK:
Current WHO guidelines and the critical role of immunohistochemical
markers in the subclassification of non-small cell lung carcinoma
(NSCLC): Moving from targeted therapy to immunotherapy. Semin
Cancer Biol. 52:103–109. 2018. View Article : Google Scholar
|
|
5
|
Watanabe SI, Nakagawa K, Suzuki K,
Takamochi K, Ito H, Okami J, Aokage K, Saji H, Yoshioka H, Zenke Y,
et al: Neoadjuvant and adjuvant therapy for Stage III non-small
cell lung cancer. Jpn J Clin Oncol. 47:1112–1118. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pöttgen C, Eberhardt W, Stamatis G and
Stuschke M: Definitive radiochemotherapy versus surgery within
multimodality treatment in stage III non-small cell lung cancer
(NSCLC)-a cumulative meta-analysis of the randomized evidence.
Oncotarget. 8:41670–41678. 2017. View Article : Google Scholar
|
|
7
|
Masters GA, Temin S, Azzoli CG, Giaccone
G, Baker S Jr, Brahmer JR, Ellis PM, Gajra A, Rackear N, Schiller
JH, et al: Systemic therapy for stage IV non-small-cell lung
cancer: American society of clinical oncology clinical practice
guideline update. J Clin Oncol. 33:3488–3515. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rancoule C, Guy JB, Vallard A, Ben Mrad M,
Rehailia A and Magné N: 50th anniversary of cisplatin. Bull Cancer.
104:167–176. 2017.In French. View Article : Google Scholar
|
|
9
|
Dasari S and Tchounwou PB: Cisplatin in
cancer therapy: Molecular mechanisms of action. Eur J Pharmacol.
740:364–378. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang K, Wang X and Wang H: Effect and
mechanism of Src tyrosine kinase inhibitor sunitinib on the
drug-resistance reversal of human A549/DDP cisplatin-resistant lung
cancer cell line. Mol Med Rep. 10:2065–2072. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yao C, Jiang J, Tu Y, Ye S, Du H and Zhang
Y: β-elemene reverses the drug resistance of A549/DDP lung cancer
cells by activating intracellular redox system, decreasing
mitochondrial membrane potential and P-glycoprotein expression, and
inducing apoptosis. Thorac Cancer. 5:304–312. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lv J and Tian Y: Effect of Src tyrosine
kinase inhibition on the drug-resistance as well as MDR1 and LRP
expression of the human cis-platinum-resistant lung cancer cell
line A549/DDP. Zhongguo Fei Ai Za Zhi. 15:501–506. 2012.In Chinese.
PubMed/NCBI
|
|
13
|
Zhong Y, Lee K, Deng Y, Ma Y, Chen Y, Li
X, Wei C, Yang S, Wang T, Wong NJ, et al: Arctigenin attenuates
diabetic kidney disease through the activation of PP2A in
podocytes. Nat Commun. 10:45232019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wagner L, Cramer H, Klose P, Lauche R,
Gass F, Dobos G and Langhorst J: Herbal medicine for cough: A
systematic review and meta-analysis. Forsch Komplementmed.
22:359–368. 2015.
|
|
15
|
Wong YK, Xu C, Kalesh KA, He Y, Lin Q,
Wong WSF, Shen HM and Wang J: Artemisinin as an anticancer drug:
Recent advances in target profiling and mechanisms of action. Med
Res Rev. 37:1492–1517. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Safarzadeh E, Sandoghchian Shotorbani S
and Baradaran B: Herbal medicine as inducers of apoptosis in cancer
treatment. Adv Pharm Bull. 4(Suppl 1): 421–427. 2014.PubMed/NCBI
|
|
17
|
Roohbakhsh A, Parhiz H, Soltani F, Rezaee
R and Iranshahi M: Molecular mechanisms behind the biological
effects of hesperidin and hesperetin for the prevention of cancer
and cardiovascular diseases. Life Sci. 124:64–74. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
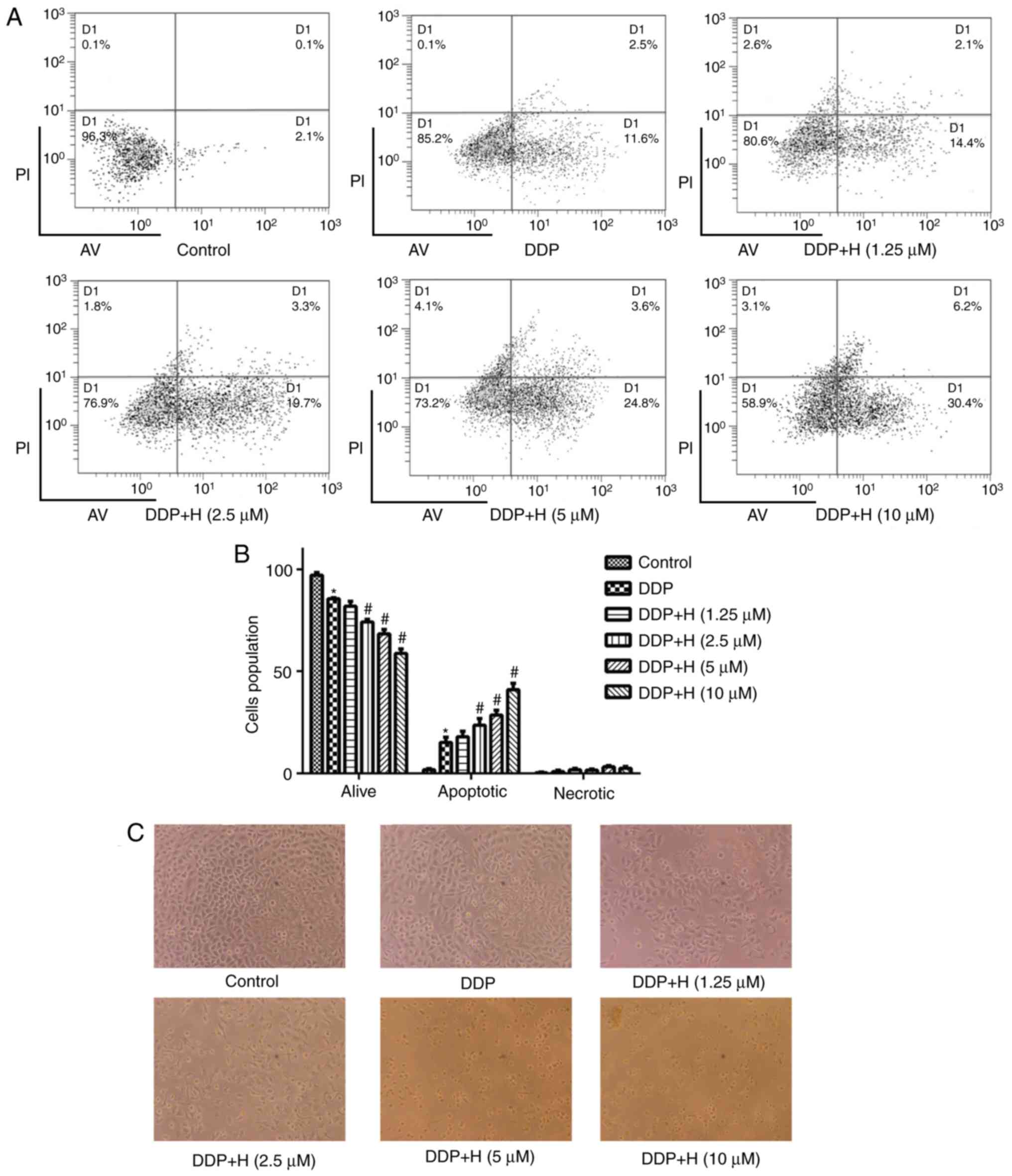
Xia R, Sheng X, Xu X, Yu C and Lu H:
Hesperidin induces apoptosis and G0/G1 arrest in human non-small
cell lung cancer A549 cells. Int J Mol Med. 41:464–472. 2018.
|
|
19
|
Xia R, Xu G, Huang Y, Sheng X, Xu X and Lu
H: Hesperidin suppresses the migration and invasion of non-small
cell lung cancer cells by inhibiting the SDF-1/CXCR-4 pathway. Life
Sci. 201:111–120. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bodduluru LN, Kasala ER, Barua CC, Karnam
KC, Dahiya V and Ellutla M: Antiproliferative and antioxidant
potential of hesperetin against benzo(a)pyrene-induced lung
carcinogenesis in Swiss albino mice. Chem Biol Interact.
242:345–352. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kamaraj S, Anandakumar P, Jagan S,
Ramakrishnan G and Devaki T: Modulatory effect of hesperidin on
benzo(a)pyrene induced experimental lung carcinogenesis with
reference to COX-2, MMP-2 and MMP-9. Eur J Pharmacol. 649:320–327.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kamaraj S, Anandakumar P, Jagan S,
Ramakrishnan G and Devaki T: Hesperidin attenuates mitochondrial
dysfunction during benzo(a)pyrene-induced lung carcinogenesis in
mice. Fundam Clin Pharmacol. 25:91–98. 2011. View Article : Google Scholar
|
|
23
|
Kamaraj S, Ramakrishnan G, Anandakumar P,
Jagan S and Devaki T: Antioxidant and anticancer efficacy of
hesperidin in benzo(a)pyrene induced lung carcinogenesis in mice.
Invest New Drugs. 27:214–222. 2009. View Article : Google Scholar
|
|
24
|
Wolfram J, Scott B, Boom K, Shen J, Borsoi
C, Suri K, Grande R, Fresta M, Celia C, Zhao Y, et al: Hesperetin
liposomes for cancer therapy. Curr Drug Deliv. 13:711–719. 2016.
View Article : Google Scholar
|
|
25
|
El Daibani AA, Xi Y, Luo L, Mei X, Zhou C,
Yasuda S and Liu MC: Sulfation of hesperetin, naringenin and
apigenin by the human cytosolic sulfotransferases: A comprehensive
analysis. Nat Prod Res. 6:1–7. 2018. View Article : Google Scholar
|
|
26
|
Aranganathan S and Nalini N: Efficacy of
the potential chemopreventive agent, hesperetin (citrus flavanone),
on 1,2-dimethylhydrazine induced colon carcinogenesis. Food Chem
Toxicol. 47:2594–2600. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sivagami G, Vinothkumar R, Bernini R,
Preethy CP, Riyasdeen A, Akbarsha MA, Menon VP and Nalini N: Role
of hesperetin (a natural flavonoid) and its analogue on apoptosis
in HT-29 human colon adenocarcinoma cell line-a comparative study.
Food Chem Toxicol. 50:660–671. 2012. View Article : Google Scholar
|
|
28
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
29
|
Heist RS: First-line systemic therapy for
non-small cell lung cancer. Hematol Oncol Clin North Am. 31:59–70.
2017. View Article : Google Scholar
|
|
30
|
Zhang XW, Liu W, Jiang HL and Mao B:
Chinese herbal medicine for advanced non-small-cell lung cancer: A
systematic review and meta-analysis. Am J Chin Med. 46:923–952.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li TM, Yu YH, Tsai FJ, Cheng CF, Wu YC, Ho
TJ, Liu X, Tsang H, Lin TH, Liao CC, et al: Characteristics of
Chinese herbal medicine usage and its effect on survival of lung
cancer patients in Taiwan. J Ethnopharmacol. 213:92–100. 2018.
View Article : Google Scholar
|
|
32
|
Byun EB, Kim HM, Song HY and Kim WS:
Hesperidin structurally modified by gamma irradiation induces
apoptosis in murine melanoma B16BL6 cells and inhibits both
subcutaneous tumor growth and metastasis in C57BL/6 mice. Food Chem
Toxicol. 127:19–30. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Elango R, Athinarayanan J, Subbarayan VP,
Lei DKY and Alshatwi AA: Hesperetin induces an apoptosis-triggered
extrinsic pathway and a p53- independent pathway in human lung
cancer H522 cells. J Asian Nat Prod Res. 20:559–569. 2018.
View Article : Google Scholar
|
|
34
|
Chen X, Wei W, Li Y, Huang J and Ci X:
Hesperetin relieves cisplatin-induced acute kidney injury by
mitigating oxidative stress, inflammation and apoptosis. Chem Biol
Interact. 308:269–278. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Li Q, Miao Z, Wang R, Yang J and Zhang D:
Hesperetin induces apoptosis in human glioblastoma cells via p38
MAPK activation. Nutr Cancer. Jul 11–2019.Epub ahead of print.
|
|
36
|
Shokri Afra H, Zangooei M, Meshkani R,
Ghahremani MH, Ilbeigi D, Khedri A, Shahmohamadnejad S, Khaghani S
and Nourbakhsh M: Hesperetin is a potent bioactivator that
activates SIRT1-AMPK signaling pathway in HepG2 cells. J Physiol
Biochem. 75:125–133. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Mary Lazer L, Sadhasivam B, Palaniyandi K,
Muthuswamy T, Ramachandran I, Balakrishnan A, Pathak S, Narayan S
and Ramalingam S: Chitosan-based nano-formulation enhances the
anticancer efficacy of hesperetin. Int J Biol Macromol.
107:1988–1998. 2018. View Article : Google Scholar
|
|
38
|
Li WX, Chen X, Yang Y, Huang HM, Li HD,
Huang C, Meng XM and Li J: Hesperitin derivative-11 suppress
hepatic stellate cell activation and proliferation by targeting
PTEN/AKT pathway. Toxicology. 381:75–86. 2017. View Article : Google Scholar
|
|
39
|
Zheng HC: The molecular mechanisms of
chemoresistance in cancers. Oncotarget. 8:59950–59964.
2017.PubMed/NCBI
|
|
40
|
Senthebane DA, Rowe A, Thomford NE,
Shipanga H, Munro D, Mazeedi MAMA, Almazyadi HAM, Kallmeyer K,
Dandara C, Pepper MS, et al: The role of tumor microenvironment in
chemo-resistance: To survive, keep your enemies closer. Int J Mol
Sci. 18:E15862017. View Article : Google Scholar
|
|
41
|
Cavaco MC, Pereira C, Kreutzer B, Gouveia
LF, Silva-Lima B, Brito AM and Videira M: Evading P-glycoprotein
mediated-efflux chemoresistance using solid lipid nanoparticles.
Eur J Pharm Biopharm. 110:76–84. 2017. View Article : Google Scholar
|
|
42
|
Hermawan A, Wagner E and Roidl A:
Consecutive salinomycin treatment reduces doxorubicin resistance of
breast tumor cells by diminishing drug efflux pump expression and
activity. Oncol Rep. 35:1732–1740. 2016. View Article : Google Scholar
|
|
43
|
Feng Q, Yang W, Gao Z, Ruan X and Zhang Y:
Up-regulation of P-gp via NF-kB activation confers protection
against oxidative damage in the retinal pigment epithelium cells.
Exp Eye Res. 181:367–373. 2019. View Article : Google Scholar
|
|
44
|
Shi Y, Wang SY, Yao M, Sai WL, Wu W, Yang
JL, Cai Y, Zheng WJ and Yao DF: Chemosensitization of HepG2 cells
by suppression of NF-kappaB/p65 gene transcription with
specific-siRNA. World J Gastroenterol. 21:12814–12821. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
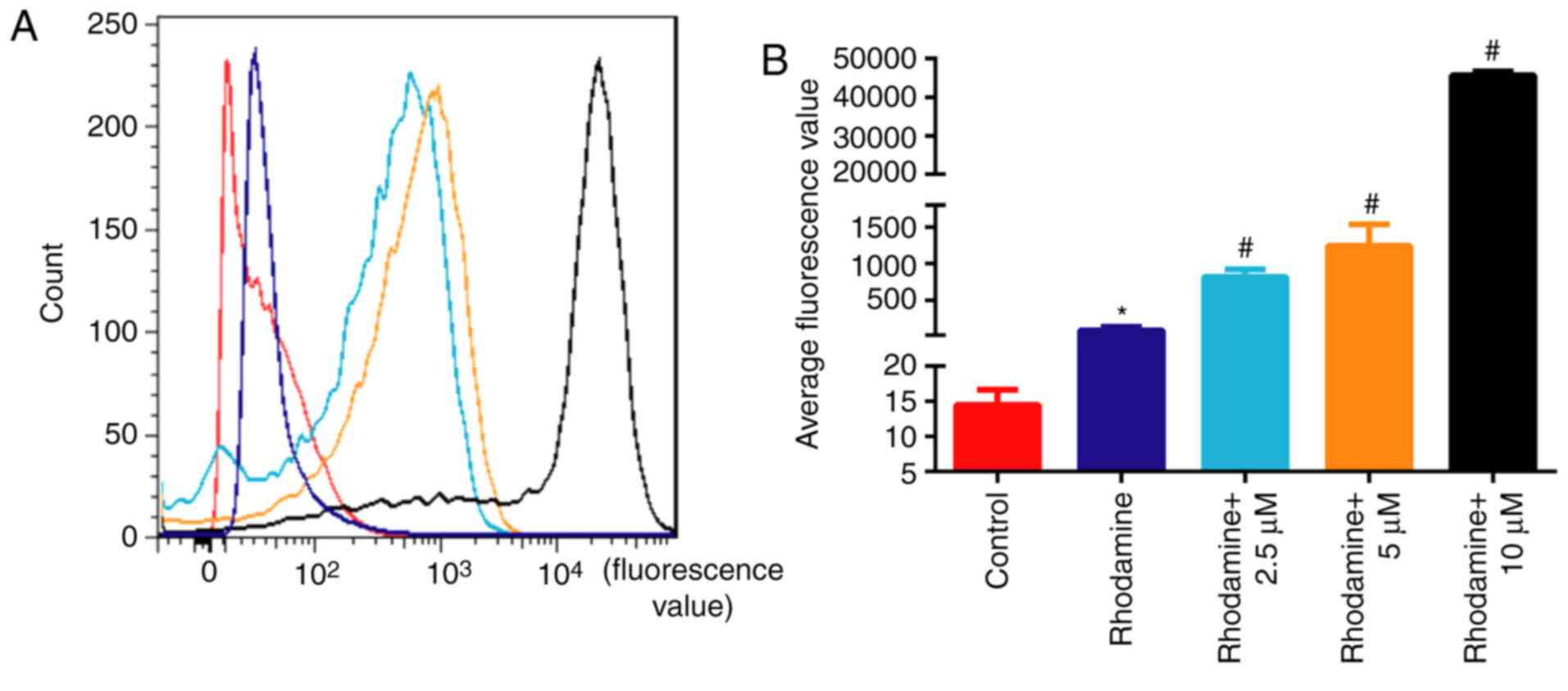
Kim M, Cooper DD, Hayes SF and Spangrude
GJ: Rhodamine-123 staining in hematopoietic stem cells of young
mice indicates mitochondrial activation rather than dye efflux.
Blood. 91:4106–4117. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Jancis EM, Chen HX, Carbone R, Hochberg RB
and Dannies PS: Rapid stimulation of rhodamine 123 efflux from
multidrug-resistant KB cells by progesterone. Biochem Pharmacol.
46:1613–1619. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang Q, Dong X, Li N, Wang Y, Guan X, Lin
Y, Kang J, Zhang X, Zhang Y, Li X and Xu T: JSH-23 prevents
depressive-like behaviors in mice subjected to chronic mild stress:
Effects on inflammation and antioxidant defense in the hippocampus.
Pharmacol Biochem Behav. 169:59–66. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kumar A, Negi G and Sharma SS: JSH-23
targets nuclear factor-kappa B and reverses various deficits in
experimental diabetic neuropathy: Effect on neuroinflammation and
antioxidant defence. Diabetes Obes Metab. 13:750–758. 2011.
View Article : Google Scholar : PubMed/NCBI
|