|
1
|
Simonneau G, Montani D, Celermajer DS,
Denton CP, Gatzoulis MA, Krowka M, Williams PG and Souza R:
Haemodynamic definitions and updated clinical classification of
pulmonary hypertension. Eur Respir J. 53:18019132019. View Article : Google Scholar :
|
|
2
|
Sahay S: Evaluation and classification of
pulmonary arterial hypertension. J Thorac Dis. 11(Suppl 14):
S1789–S1799. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Archer SL, Weir EK and Wilkins MR: Basic
science of pulmonary arterial hypertension for clinicians: New
concepts and experimental therapies. Circulation. 121:2045–2066.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Guignabert C and Dorfmuller P: Pathology
and pathobiology of pulmonary hypertension. Semin Respir Crit Care
Med. 34:551–559. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pullamsetti SS, Schermuly R, Ghofrani A,
Weissmann N, Grimminger F and Seeger W: Novel and emerging
therapies for pulmonary hypertension. Am J Respir Crit Care Med.
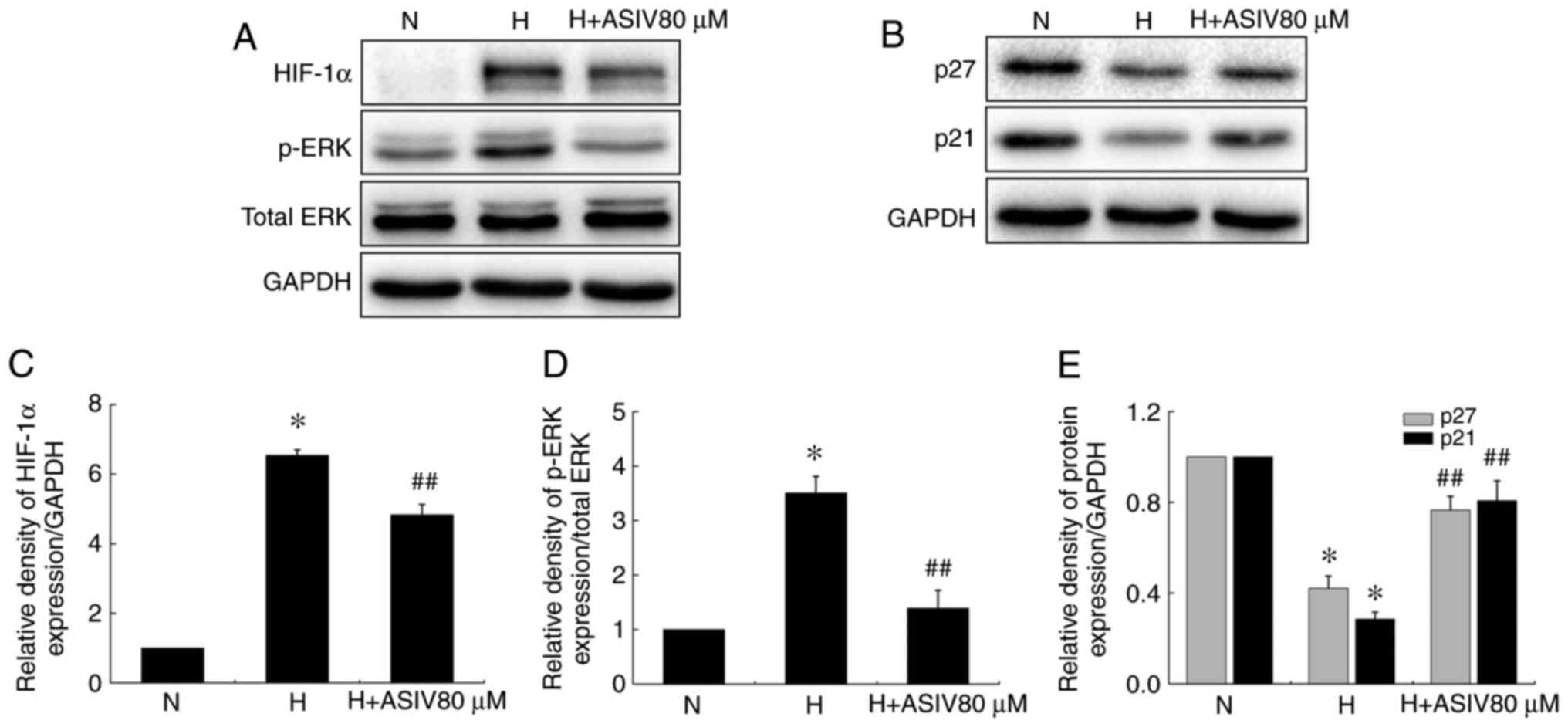
189:394–400. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pugliese SC, Poth JM, Fini MA, Olschewski
A, El Kasmi KC and Stenmark KR: The role of inflammation in hypoxic
pulmonary hypertension: From cellular mechanisms to clinical
phenotypes. Am J Physiol Lung Cell Mol Physiol. 308:L229–L252.
2015. View Article : Google Scholar :
|
|
7
|
Rabinovitch M, Guignabert C, Humbert M and
Nicolls MR: Inflammation and immunity in the pathogenesis of
pulmonary arterial hypertension. Circ Res. 115:165–175. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mushaben EM, Hershey GK, Pauciulo MW,
Nichols WC and Le Cras TD: Chronic allergic inflammation causes
vascular remodeling and pulmonary hypertension in BMPR2 hypomorph
and wild-type mice. PLoS One. 7:e324682012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vaillancourt M, Ruffenach G, Meloche J and
Bonnet S: Adaptation and remodelling of the pulmonary circulation
in pulmonary hypertension. Can J Cardiol. 31:407–415. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Freund-Michel V, Cardoso Dos Santos M,
Guignabert C, Montani D, Phan C, Coste F, Tu L, Dubois M, Girerd B,
Courtois A, et al: Role of nerve growth factor in development and
persistence of experimental pulmonary hypertension. Am J Respir
Crit Care Med. 192:342–355. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jin H, Liu M, Zhang X, Pan J, Han J, Wang
Y, Lei H, Ding Y and Yuan Y: Grape seed procyanidin extract
attenuates hypoxic pulmonary hypertension by inhibiting oxidative
stress and pulmonary arterial smooth muscle cells proliferation. J
Nutr Biochem. 36:81–88. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thenappan T, Ormiston ML, Ryan JJ and
Archer SL: Pulmonary arterial hypertension: Pathogenesis and
clinical management. BMJ. 360:j54922018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li MX, Jiang DQ and Wang Y, Chen QZ, Ma
YJ, Yu SS and Wang Y: Signal mechanisms of vascular remodeling in
the development of pulmonary arterial hypertension. J Cardiovasc
Pharmacol. 67:182–190. 2016. View Article : Google Scholar
|
|
14
|
Nogueira-Ferreira R, Vitorino R, Ferreira
R and Henriques-Coelho T: Exploring the monocrotaline animal model
for the study of pulmonary arterial hypertension: A network
approach. Pulm Pharmacol Ther. 35:8–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xiong PY, Potus F, Chan W and Archer SL:
Models and molecular mechanisms of world health organization group
2 to 4 pulmonary hypertension. Hypertension. 71:34–55. 2018.
View Article : Google Scholar
|
|
16
|
Fu J, Wang Z, Huang L, Zheng S, Wang D,
Chen S, Zhang H and Yang S: Review of the botanical
characteristics, phytochemistry, and pharmacology of Astragalus
membranaceus (Huangqi). Phytother Res. 28:1275–1283. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li X, Qu L, Dong Y, Han L, Liu E, Fang S,
Zhang Y and Wang T: A review of recent research progress on the
astragalus genus. Molecules. 19:18850–18880. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li L, Hou X, Xu R, Liu C and Tu M:
Research review on the pharmacological effects of astragaloside IV.
Fundam Clin Pharmacol. 31:17–36. 2017. View Article : Google Scholar
|
|
19
|
Qiu L, Yin G, Cheng L, Fan Y, Xiao W, Yu
G, Xing M, Jia R, Sun R, Ma X, et al: Astragaloside IV ameliorates
acute pancreatitis in rats by inhibiting the activation of nuclear
factor-κB. Int J Mol Med. 35:625–636. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu X, Zhang J, Wang S, Qiu J and Yu C:
Astragaloside IV attenuates the H2O2-induced apoptosis of neuronal
cells by inhibiting α-synuclein expression via the p38 MAPK
pathway. Int J Mol Med. 40:1772–1780. 2017.PubMed/NCBI
|
|
21
|
Wang J, Zhou Y, Wu S, Huang K, Thapa S,
Tao L, Wang J, Shen Y, Wang J, Xue Y and Ji K: Astragaloside IV
attenuated 3,4-benzopyrene-induced abdominal aortic aneurysm by
ameliorating macrophage-mediated inflammation. Front Pharmacol.
9:4962018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lu Y, Li S, Wu H, Bian Z, Xu J, Gu C, Chen
X and Yang D: Beneficial effects of astragaloside IV against
angio-tensin II-induced mitochondrial dysfunction in rat vascular
smooth muscle cells. Int J Mol Med. 36:1223–1232. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Qian W, Cai X, Qian Q, Zhang W and Wang D:
Astragaloside IV modulates TGF-β1-dependent epithelial-mesenchymal
transition in bleomycin-induced pulmonary fibrosis. J Cell Mol Med.
22:4354–4365. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
West J and Hemnes A: Experimental and
transgenic models of pulmonary hypertension. Compr Physiol.
1:769–782. 2011.PubMed/NCBI
|
|
25
|
Jin H, Wang Y, Zhou L, Liu L, Zhang P,
Deng W and Yuan Y: Melatonin attenuates hypoxic pulmonary
hypertension by inhibiting the inflammation and the proliferation
of pulmonary arterial smooth muscle cells. J Pineal Res.
57:442–450. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
27
|
Matura LA, Ventetuolo CE, Palevsky HI,
Lederer DJ, Horn EM, Mathai SC, Pinder D, Archer-Chicko C, Bagiella
E, Roberts KE, et al: Interleukin-6 and tumor necrosis factor-α are
associated with quality of life-related symptoms in pulmonary
arterial hypertension. Ann Am Thorac Soc. 12:370–375. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Itoh A, Nishihira J, Makita H, Miyamoto K,
Yamaguchi E and Nishimura M: Effects of IL-1beta, TNF-alpha, and
macrophage migration inhibitory factor on prostacyclin synthesis in
rat pulmonary artery smooth muscle cells. Respirology. 8:467–472.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fujita M, Shannon JM, Irvin CG, Fagan KA,
Cool C, Augustin A and Mason RJ: Overexpression of tumor necrosis
factor-alpha produces an increase in lung volumes and pulmonary
hypertension. Am J Physiol Lung Cell Mol Physiol. 280:L39–L49.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Groth A, Vrugt B, Brock M, Speich R,
Ulrich S and Huber LC: Inflammatory cytokines in pulmonary
hypertension. Respir Res. 15:472014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang Q, Zuo XR, Wang YY, Xie WP, Wang H
and Zhang M: Monocrotaline-induced pulmonary arterial hypertension
is attenuated by TNF-α antagonists via the suppression of TNF-α
expression and NF-κB pathway in rats. Vascul Pharmacol. 58:71–77.
2013. View Article : Google Scholar
|
|
32
|
Campos M and Schiopu E: Pulmonary arterial
hypertension in adult-onset still's disease: Rapid response to
anakinra. Case Rep Rheumatol. 2012:5376132012.PubMed/NCBI
|
|
33
|
Jiang P, Ma D, Wang X, Wang Y, Bi Y, Yang
J, Wang X and Li X: Astragaloside IV prevents obesity-associated
hypertension by improving pro-inflammatory reaction and leptin
resistance. Mol Cells. 41:244–255. 2018.PubMed/NCBI
|
|
34
|
Meiqian Z, Leying Z and Chang C:
Astragaloside IV inhibits cigarette smoke-induced pulmonary
inflammation in mice. Inflammation. 41:1671–1680. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Paulin R and Michelakis ED: The metabolic
theory of pulmonary arterial hypertension. Circ Res. 115:148–164.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ball MK, Waypa GB, Mungai PT, Nielsen JM,
Czech L, Dudley VJ, Beussink L, Dettman RW, Berkelhamer SK,
Steinhorn RH, et al: Regulation of hypoxia-induced pulmonary
hypertension by vascular smooth muscle hypoxia-inducible factor-1α.
Am J Respir Crit Care Med. 189:314–324. 2014. View Article : Google Scholar :
|
|
37
|
Wang G, Wang JJ, Fu XL, Guang R and To ST:
Advances in the targeting of HIF-1α and future therapeutic
strategies for glioblastoma multiforme (Review). Oncol Rep.
37:657–670. 2017. View Article : Google Scholar
|
|
38
|
Fouty BW, Grimison B, Fagan KA, Le Cras
TD, Harral JW, Hoedt-Miller M, Sclafani RA and Rodman DM: p27(Kip1)
is important in modulating pulmonary artery smooth muscle cell
proliferation. Am J Respir Cell Mol Biol. 25:652–658. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mizuno S, Kadowaki M, Demura Y, Ameshima
S, Miyamori I and Ishizaki T: p42/44 mitogen-activated protein
kinase regulated by p53 and nitric oxide in human pulmonary
arterial smooth muscle cells. Am J Respir Cell Mol Biol.
31:184–192. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ashok C, Owais S, Srijyothi L, Selvam M,
Ponne S and Baluchamy S: A feedback regulation of CREB activation
through the CUL4A and ERK signaling. Med Oncol. 36:202019.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Humbert M, Guignabert C, Bonnet S,
Dorfmüller P, Klinger JR, Nicolls MR, Olschewski AJ, Pullamsetti
SS, Schermuly RT, Stenmark KR and Rabinovitch M: Pathology and
pathobiology of pulmonary hypertension: State of the art and
research perspectives. Eur Respir J. 53:18018872019. View Article : Google Scholar :
|
|
42
|
Budhiraja R, Tuder RM and Hassoun PM:
Endothelial dysfunction in pulmonary hypertension. Circulation.
109:159–165. 2004. View Article : Google Scholar : PubMed/NCBI
|