|
1
|
Kumar KG, Trevaskis JL, Lam DD, Sutton GM,
Koza RA, Chouljenko VN, Kousoulas KG, Rogers PM, Kesterson RA,
Thearle M, et al: Identification of adropin as a secreted factor
linking dietary macronutrient intake with energy homeostasis and
lipid metabolism. Cell Metab. 8:468–481. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marczuk N, Cecerska-Heryć E, Jesionowska A
and Dołęgowska B: Adropin-physiological and pathophysiological
role. Postepy Hig Med Dosw (Online). 70:981–988. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aydin S, Kuloglu T, Aydin S, Eren MN,
Yilmaz M, Kalayci M, Sahin I, Kocaman N, Citil C and Kendir Y:
Expression of adropin in rat brain, cerebellum, kidneys, heart,
liver, and pancreas in streptozotocin-induced diabetes. Mol Cell
Biochem. 380:73–81. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen X, Chen S, Shen T, Yang W, Chen Q,
Zhang P, You Y, Sun X, Xu H, Tang Y, et al: Adropin regulates
hepatic glucose production via PP2A/AMPK pathway in
insulin-resistant hepatocytes. FASEB J. 34:10056–10072. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Erman H, Ozdemir A, Sitar ME, Cetin SI and
Boyuk B: Role of serum adropin measurement in the assessment of
insulin resistance in obesity. J Investig Med. 69:1318–1323. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Akcılar R, Emel Koçak F, Şimşek H, Akcılar
A, Bayat Z, Ece E and Kökdaşgil H: The effect of adropin on lipid
and glucose metabolism in rats with hyperlipidemia. Iran J Basic
Med Sci. 19:245–251. 2016.
|
|
7
|
Gao S, McMillan RP, Zhu Q, Lopaschuk GD,
Hulver MW and Butler AA: Therapeutic effects of adropin on glucose
tolerance and substrate utilization in diet-induced obese mice with
insulin resistance. Mol Metab. 4:310–324. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yu M, Wang D, Zhong D, Xie W and Luo J:
adropin carried by reactive oxygen species-responsive nanocapsules
ameliorates renal lipid toxicity in diabetic mice. ACS Appl Mater
Interfaces. 14:37330–37344. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lovren F, Pan Y, Quan A, Singh KK, Shukla
PC, Gupta M, Al-Omran M, Teoh H and Verma S: Adropin is a novel
regulator of endothelial function. Circulation. 122(11 Suppl):
S185–S192. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang L, Jin F, Wang P, Hou S, Jin T, Chang
X and Zhao L: Adropin inhibits vascular smooth muscle cell
osteogenic differentiation to alleviate vascular calcification via
the JAK2/STAT3 signaling pathway. Biomed Res Int.
2022:91222642022.PubMed/NCBI
|
|
11
|
Ali II, D'Souza C, Singh J and Adeghate E:
Adropin's role in energy homeostasis and metabolic disorders. Int J
Mol Sci. 23:83182022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jasaszwili M, Billert M, Strowski MZ,
Nowak KW and Skrzypski M: Adropin as A Fat-Burning hormone with
multiple functions-review of a decade of research. Molecules.
25:5492020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li L, Xie W, Zheng XL, Yin WD and Tang CK:
A novel peptide adropin in cardiovascular diseases. Clin Chim Acta.
453:107–113. 2016. View Article : Google Scholar
|
|
14
|
Niepolski L and Grzegorzewska AE: Salusins
and adropin: New peptides potentially involved in lipid metabolism
and atherosclerosis. Adv Med Sci. 61:282–287. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Petersen TN, Brunak S, von Heijne G and
Nielsen H: SignalP 4.0: discriminating signal peptides from
transmembrane regions. Nat Methods. 8:785–786. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wong CM, Wang Y, Lee JT, Huang Z, Wu D, Xu
A and Lam KS: Adropin is a brain membrane-bound protein regulating
physical activity via the NB-3/Notch signaling pathway in mice. J
Biol Chem. 289:25976–25986. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang C, Yan Y, Zhang Q and Jiang Q:
Molecular cloning and characterization of the novel adropin from
tilapia (Oreochromis niloticus): Involvement in the control of food
intake. Neuropeptides. 88:1021652021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ganesh Kumar K, Zhang J, Gao S, Rossi J,
McGuinness OP, Halem HH, Culler MD, Mynatt RL and Butler AA:
Adropin deficiency is associated with increased adiposity and
insulin resistance. Obesity (Silver Spring). 20:1394–1402. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
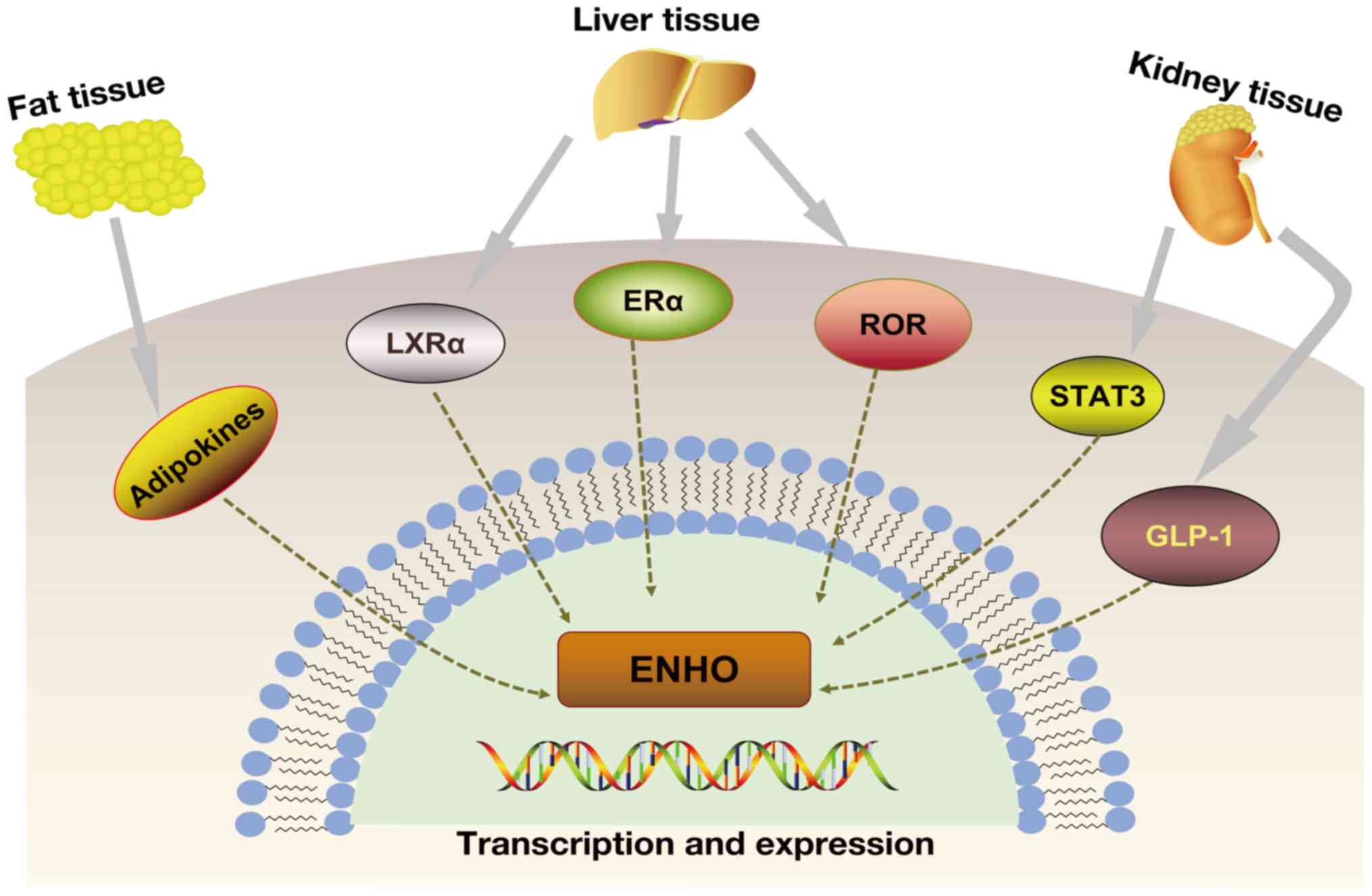
Bindesbøll C, Fan Q, Nørgaard RC,
MacPherson L, Ruan HB, Wu J, Pedersen TA, Steffensen KR, Yang X,
Matthews J, et al: Liver X receptor regulates hepatic nuclear
O-GlcNAc signaling and carbohydrate responsive element-binding
protein activity. J Lipid Res. 56:771–785. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stayrook KR, Rogers PM, Savkur RS, Wang Y,
Su C, Varga G, Bu X, Wei T, Nagpal S, Liu XS and Burris TP:
Regulation of human 3 alpha-hydroxysteroid dehydrogenase (AKR1C4)
expression by the liver X receptor alpha. Mol Pharmacol.
73:607–612. 2008. View Article : Google Scholar
|
|
21
|
Ghoshal S, Stevens JR, Billon C, Girardet
C, Sitaula S, Leon AS, Rao DC, Skinner JS, Rankinen T, Bouchard C,
et al: Adropin: An endocrine link between the biological clock and
cholesterol homeostasis. Mol Metab. 8:51–64. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Meda C, Dolce A, Vegeto E, Maggi A and
Della Torre S: ERα-Dependent regulation of adropin predicts sex
differences in liver homeostasis during high-fat diet. Nutrients.
14:32622022. View Article : Google Scholar
|
|
23
|
Stokar J, Gurt I, Cohen-Kfir E, Yakubovsky
O, Hallak N, Benyamini H, Lishinsky N, Offir N, Tam J and
Dresner-Pollak R: Hepatic adropin is regulated by estrogen and
contributes to adverse metabolic phenotypes in ovariectomized mice.
Mol Metab. 60:1014822022. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kuo FY, Cheng KC, Li Y, Cheng JT and Tsai
CC: Promotion of adropin expression by hyperglycemia is associated
with STAT3 activation in diabetic rats. Diabetes Metab Syndr Obes.
13:2269–2277. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li YX, Cheng KC, Liu IM and Niu HS:
Myricetin Increases circulating adropin level after activation of
glucagon-like peptide 1 (GLP-1) receptor in type-1 diabetic rats.
Pharmaceuticals (Basel). 15:1732022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Thapa D, Xie B, Manning JR, Zhang M,
Stoner MW, Huckestein BR, Edmunds LR, Zhang X, Dedousis NL,
O'Doherty RM, et al: Adropin reduces blood glucose levels in mice
by limiting hepatic glucose production. Physiol Rep. 7:e140432019.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jasaszwili M, Pruszyńska-Oszmałek E,
Wojciechowicz T, Strowski MZ, Nowak KW and Skrzypski M: Adropin
slightly modulates lipolysis, lipogenesis and expression of
adipokines but not glucose uptake in rodent adipocytes. Genes
(Basel). 12:9142021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yu HY, Zhao P, Wu MC, Liu J and Yin W:
Serum adropin levels are decreased in patients with acute
myocardial infarction. Regul Pept. 190-191:46–49. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ding F, Liu G, Gao F, Zheng Z, Hong Y,
Chen Y and Weng S: Adropin attenuates pancreatitis-associated lung
injury through PPARγ phosphorylation-related macrophage
polarization. Int J Mol Med. 52:952023. View Article : Google Scholar
|
|
30
|
Kutlu O, Altun Ö, Dikker O, Aktaş Ş, Özsoy
N, Arman Y, Özgün Çil E, Özcan M, Aydın Yoldemir Ş, Akarsu M, et
al: Serum adropin levels are reduced in adult patients with
nonalcoholic fatty liver disease. Med Princ Pract. 28:463–469.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Berezina TA, Obradovic Z, Boxhammer E,
Berezin AA, Lichtenauer M and Berezin AE: Adropin predicts chronic
kidney disease in type 2 diabetes mellitus patients with chronic
heart failure. J Clin Med. 12:22312023. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kuliczkowska-Płaksej J, Mierzwicka A,
Jończyk M, Stachowska B, Urbanovych A and Bolanowski M: Adropin in
women with polycystic ovary syndrome. Endokrynol Pol. 70:151–156.
2019. View Article : Google Scholar
|
|
33
|
Herrero L, de Dios O, Gavela-Pérez T,
Riestra P, Jois A, Soriano-Guillén L and Garcés C: Opposite
association of adropin concentrations with obesity in prepubertal
children compared with adolescents. Obesity (Silver Spring).
28:1736–1741. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wei W, Liu H, Qiu X, Zhang J, Huang J,
Chen H, Qiu S, Lin R, Li S and Tu M: The association between serum
adropin and carotid atherosclerosis in patients with type 2
diabetes mellitus: A cross-sectional study. Diabetol Metab Syndr.
14:272022. View Article : Google Scholar
|
|
35
|
Zhao LP, You T, Chan SP, Chen JC and Xu
WT: Adropin is associated with hyperhomocysteine and coronary
atherosclerosis. Exp Ther Med. 11:1065–1070. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liang M, Dickel N, Györfi AH,
SafakTümerdem B, Li YN, Rigau AR, Liang C, Hong X, Shen L, Matei
AE, et al: Attenuation of fibroblast activation and fibrosis by
adropin in systemic sclerosis. Sci Transl Med. 16:eadd65702024.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tuna BG, Atalay PB, Altunbek M, Kalkan BM
and Dogan S: Effects of chronic and intermittent calorie
restriction on adropin levels in breast cancer. Nutr Cancer.
69:1003–1010. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Nergiz S, Altinkaya SO, Kurt Ömürlü İ,
Yuksel H, Küçük M and Demircan Sezer S: Circulating adropin levels
in patients with endometrium cancer. Gynecol Endocrinol.
31:730–735. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Reed GW, Rossi JE and Cannon CP: Acute
myocardial infarction. Lancet. 389:197–210. 2017. View Article : Google Scholar
|
|
40
|
Altamimi TR, Gao S, Karwi QG, Fukushima A,
Rawat S, Wagg CS, Zhang L and Lopaschuk GD: Adropin regulates
cardiac energy metabolism and improves cardiac function and
efficiency. Metabolism. 98:37–48. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Aydin S, Kuloglu T, Aydin S, Kalayci M,
Yilmaz M, Çakmak T and Eren MN: Elevated adropin: A candidate
diagnostic marker for myocardial infarction in conjunction with
troponin-I. Peptides. 58:91–97. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li B, Wang Z, He Y, Chen T, Zhang Y, Yuan
X and Li P: Adropin improves radiation-induced myocardial injury
via VEGFR2/PI3K/Akt pathway. Oxid Med Cell Longev.
2022:82302142022.PubMed/NCBI
|
|
43
|
Adıyaman M, Canpolat Erkan RE, Kaya İ and
Aba Adıyaman Ö: Serum adropin level in the early period of
ST-Elevation myocardial infarction and its relationship with
cobalamin and folic acid. Cureus. 14:e327482022.
|
|
44
|
Chang X, Jin F, Wang L, Jiang Y, Wang P,
Liu J and Zhao L: Adropin-A new player in energy regulation
predicts long-term prognosis of patients with acute myocardial
infarction. Heliyon. 9:e178032023. View Article : Google Scholar
|
|
45
|
Foucher P, Heeringa P, Petersen AH,
Huitema MG, Brouwer E, Tervaert JW, Prop J, Camus P, Weening JJ and
Kallenberg CG: Antimyeloperoxidase-associated lung disease. An
experimental model. Am J Respir Crit Care Med. 160:987–994. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Saeki T, Fujita N, Kourakata H, Yamazaki H
and Miyamura S: Two cases of hypertrophic pachymeningitis
associated with myeloperoxidase antineutrophil cytoplasmic
autoantibody (MPO-ANCA)-positive pulmonary silicosis in tunnel
workers. Clin Rheumatol. 23:76–80. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Gao F, Fang J, Chen F, Wang C, Chen S,
Zhang S, Lv X, Zhang J, He Q, Weng S, et al: Enho mutations causing
low adropin: A possible pathomechanism of MPO-ANCA Associated lung
injury. EBioMedicine. 9:324–335. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Rizk FH, El-Saka MH, Ibrahim RR, El-Deeb
OS, Ibrahim HA, El Saadany AA, Mashal SS, Ammar L, Abdelsattar AM
and Barhoma RA: Possible mitigating effect of adropin on lung
injury in diabetic rats: Targeting the role of Rho A/Rho-associated
kinase pathway. Biofactors. 49:928–939. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Orun S, Celikkol A, Basol BI and Yeniay E:
Diagnostic accuracy of adropin as a preliminary test to exclude
acute pulmonary embolism: a prospective study. BMC Pulm Med.
22:3512022. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Byrne CD and Targher G: NAFLD: A
multisystem disease. J Hepatol. 62(1 Suppl): S47–S64. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Younossi Z, Tacke F, Arrese M, Chander
Sharma B, Mostafa I, Bugianesi E, Wai-Sun Wong V, Yilmaz Y, George
J, Fan J and Vos MB: Global perspectives on nonalcoholic fatty
liver disease and nonalcoholic steatohepatitis. Hepatology.
69:2672–2682. 2019. View Article : Google Scholar
|
|
52
|
Zhang C, Zhang Q, Huang Z and Jiang Q:
Adropin inhibited tilapia hepatic glucose output and triglyceride
accumulation via AMPK activation. J Endocrinol. 246:109–122. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Chen X, Sun X, Shen T, Chen Q, Chen S,
Pang J, Mi J, Tang Y, You Y, Xu H and Ling W: Lower adropin
expression is associated with oxidative stress and severity of
nonalcoholic fatty liver disease. Free Radic Biol Med. 160:191–198.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Yang W, Liu L, Wei Y, Fang C, Liu S, Zhou
F, Li Y, Zhao G, Guo Z, Luo Y and Li L: Exercise suppresses NLRP3
inflammasome activation in mice with diet-induced NASH: A plausible
role of adropin. Lab Invest. 101:369–380. 2021. View Article : Google Scholar
|
|
55
|
Li N, Xie G, Zhou B, Qu A, Meng H, Liu J
and Wang G: Serum adropin as a potential biomarker for predicting
the development of type 2 diabetes mellitus in individuals with
metabolic dysfunction-associated fatty liver disease. Front
Physiol. 12:6961632021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang L, Wu X, Li X, Chang X, Ding X, Wang
Q, Jiang T, Wang G and Liu J: Longitudinal changes in serum adropin
levels and liver fat content during liraglutide treatment in newly
diagnosed patients with type 2 diabetes mellitus and metabolic
dysfunction-associated fatty liver disease. Acta Diabetol.
60:971–979. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zhu T, Du Y, Xuan M, Guo C and Rao X:
Clinical characteristics and Chinese Medicine therapy of chronic
kidney disease combined with cardiovascular disease. Integr Med
Nephrol Androl. 10:e000232023. View Article : Google Scholar
|
|
58
|
Song Z and Gong X: research progress on
the potential mechanisms of acute kidney injury and chronic kidney
disease induced by proton pump inhibitors. Integr Med Nephrol
Androl. 10:e000272023. View Article : Google Scholar
|
|
59
|
Tao P, Huo J and Chen L: Bibliometric
analysis of the relationship between gut microbiota and chronic
kidney disease from 2001-2022. Integr Med Nephrol Androl.
11:e000172024. View Article : Google Scholar
|
|
60
|
Zhang HQ, Wu S, Chen X, Fang YX, Lan QM,
Zhou ZJ, Qiao YH, Li J, Zhao YR, Pei M and Yang B: Potential
efficacy and mechanism of medicinal plants on chronic kidney
disease-associated vascular calcification: A review. Tradit Med
Res. 9:512024. View Article : Google Scholar
|
|
61
|
Memi G and Yazgan B: Adropin and spexin
hormones regulate the systemic inflammation in adenine-induced
chronic kidney failure in rat. Chin J Physiol. 64:194–201. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Grzegorzewska AE, Niepolski L, Mostowska
A, Warchoł W and Jagodziński PP: Involvement of adropin and
adropin-associated genes in metabolic abnormalities of hemodialysis
patients. Life Sci. 160:41–46. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kałużna M, Hoppe K, Schwermer K, Ibrahim
AY, Pawlaczyk K and Ziemnicka K: Adropin and irisin levels in
relation to nutrition, body composition, and insulin resistance in
patients with end-stage renal disease on chronic hemodialysis and
peritoneal dialysis. Pol Arch Med Wewn. 126:474–482. 2016.
|
|
64
|
Kałużna M, Pawlaczyk K, Schwermer K, Hoppe
K, Człapka-Matyasik M, Ibrahim AY, Sawicka-Gutaj N, Minczykowski A,
Ziemnicka K, Oko A and Ruchała M: Adropin and irisin: New
biomarkers of cardiac status in patients with end-stage renal
disease? A preliminary study. Adv Clin Exp Med. 28:347–353. 2019.
View Article : Google Scholar
|
|
65
|
Cecerska-Heryć E, Adamiak D, Serwin N,
Grygorcewicz B and Dołęgowska B: Comparative analysis of adropin
concentration changes in response to kidney transplantation. Eur J
Intern Med. 84:112–114. 2021. View Article : Google Scholar
|
|
66
|
Maciorkowska M, Musiałowska D and Małyszko
J: Adropin and irisin in arterial hypertension, diabetes mellitus
and chronic kidney disease. Adv Clin Exp Med. 28:1571–1575. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Kaur R, Krishan P, Kumari P, Singh T,
Singh V, Singh R and Ahmad SF: Clinical significance of adropin and
afamin in evaluating renal function and cardiovascular health in
the presence of CKD-MBD biomarkers in chronic kidney disease.
Diagnostics (Basel). 13:31582023. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Liu F, Cui B, Zhao X, Wu Y, Qin H, Guo Y,
Wang H, Lu M, Zhang S, Shen J, et al: Correlation of serum adropin
levels with risk factors of cardiovascular disease in hemodialysis
patients. Metab Syndr Relat Disord. 19:401–408. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Boric-Skaro D, Mizdrak M, Luketin M,
Martinovic D, Tokic D, Vilovic M, Supe-Domic D, Kurir TT and Bozic
J: Serum adropin levels in patients on hemodialysis. Life (Basel).
11:3372021.PubMed/NCBI
|
|
70
|
Kume T, Calan M, Yilmaz O, Kocabas GU,
Yesil P, Temur M, Bicer M and Calan OG: A possible connection
between tumor necrosis factor alpha and adropin levels in
polycystic ovary syndrome. J Endocrinol Invest. 39:747–754. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Bousmpoula A, Kouskouni E, Benidis E,
Demeridou S, Kapeta-Kourkouli R, Chasiakou A and Baka S: Adropin
levels in women with polycystic ovaries undergoing ovarian
stimulation: Correlation with lipoprotein lipid profiles. Gynecol
Endocrinol. 34:153–156. 2018. View Article : Google Scholar
|
|
72
|
Inal ZO, Erdem S, Gederet Y, Duran C,
Kucukaydin Z, Kurku H and Sakarya DK: The impact of serum adropin
and ischemia modified albumin levels based on BMI in PCOS.
Endokrynol Pol. 69:135–141. 2018.PubMed/NCBI
|
|
73
|
Ye Z, Zhang C and Zhao Y: Potential
effects of adropin on systemic metabolic and hormonal abnormalities
in polycystic ovary syndrome. Reprod Biomed Online. 42:1007–1014.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Varikasuvu SR, Reddy EP, Thangappazham B,
Varshney S, Das VL and Munikumar M: Adropin levels and its
associations as a fat-burning hormone in patients with polycystic
ovary syndrome: A correlational meta-analysis. Gynecol Endocrinol.
37:879–884. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ke Y, Hu J, Zhu Y, Wang Y, Chen S and Liu
S: Correlation between circulating adropin levels and patients with
PCOS: An updated systematic review and meta-analysis. Reprod Sci.
29:3295–3310. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Engin A: The definition and prevalence of
obesity and metabolic syndrome. Adv Exp Med Biol. 960:1–17. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Gao S, Ghoshal S, Zhang L, Stevens JR,
McCommis KS, Finck BN, Lopaschuk GD and Butler AA: The peptide
hormone adropin regulates signal transduction pathways controlling
hepatic glucose metabolism in a mouse model of diet-induced
obesity. J Biol Chem. 294:13366–13377. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Dye L, Boyle NB, Champ C and Lawton C: The
relationship between obesity and cognitive health and decline. Proc
Nutr Soc. 76:443–454. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Miller AA and Spencer SJ: Obesity and
neuroinflammation: A pathway to cognitive impairment. Brain Behav
Immun. 42:10–21. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ghoshal S, Banerjee S, Zhang J, Niehoff
ML, Farr SA and Butler AA: Adropin transgenesis improves
recognition memory in diet-induced obese LDLR-deficient C57BL/6J
mice. Peptides. 146:1706782021. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Altincik A and Sayin O: Evaluation of the
relationship between serum adropin levels and blood pressure in
obese children. J Pediatr Endocrinol Metab. 28:1095–1100. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chen RM, Yuan X, Ouyang Q, Lin XQ, Ai ZZ,
Zhang Y and Yang XH: Adropin and glucagon-like peptide-2 are
associated with glucose metabolism in obese children. World J
Pediatr. 15:565–571. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Yuan X, Chen R, Ouyang Q, Lin X, Ai Z,
Zhang Y and Yang X: Novel associations of serum adropin and
lipopolysaccharide-binding protein versus lipid profiles in
childhood obesity. J Pediatr Endocrinol Metab. 33:265–270. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Yin C, Zhang H, Zhang M and Xiao Y:
Adropin and apelin-12 efficiently predict metabolic syndrome in
obese children. Pediatr Diabetes. 21:1132–1139. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Soltani S, Kolahdouz-Mohammadi R, Aydin S,
Yosaee S, Clark CCT and Abdollahi S: Circulating levels of adropin
and overweight/obesity: A systematic review and meta-analysis of
observational studies. Hormones (Athens). 21:15–22. 2022.
View Article : Google Scholar
|
|
86
|
He L, Zhang FJ, Li HY, Li L, Song LG, Mao
Y, Li J, Liu HM, Li FL, Xu LY, et al: Anti-diabetic role of adropin
in streptozotocin induced diabetic rats via alteration of PI3K/Akt
and insulin signaling pathway. J Oleo Sci. 70:657–664. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Hu W and Chen L: Association of serum
adropin concentrations with diabetic nephropathy. Mediators
Inflamm. 2016:60382612016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Li B, Li N, Guo S, Zhang M, Li J, Zhai N,
Wang H and Zhang Y: The changing features of serum adropin,
copeptin, neprilysin and chitotriosidase which are associated with
vascular endothelial function in type 2 diabetic retinopathy
patients. J Diabetes Complications. 34:1076862020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Jiang S, Young JL, Wang K, Qian Y and Cai
L: Diabetic-induced alterations in hepatic glucose and lipid
metabolism: The role of type 1 and type 2 diabetes mellitus
(Review). Mol Med Rep. 22:603–611. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Jones JG: Hepatic glucose and lipid
metabolism. Diabetologia. 59:1098–1103. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Thapa D, Xie B, Zhang M, Stoner MW,
Manning JR, Huckestein BR, Edmunds LR, Mullett SJ, McTiernan CF,
Wendell SG, et al: Adropin treatment restores cardiac glucose
oxidation in pre-diabetic obese mice. J Mol Cell Cardiol.
129:174–178. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Skrzypski M, Kołodziejski PA,
Pruszyńska-Oszmałek E, Wojciechowicz T, Janicka P, Krążek M, Małek
E, Strowski MZ and Nowak KW: Daily treatment of mice with type 2
diabetes with adropin for four weeks improves glucolipid profile,
reduces hepatic lipid content and restores elevated hepatic enzymes
in serum. Int J Mol Sci. 23:98072022. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Zang H, Jiang F, Cheng X, Xu H and Hu X:
Serum adropin levels are decreased in Chinese type 2 diabetic
patients and negatively correlated with body mass index. Endocr J.
65:685–691. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Choi HN and Yim JE: Plasma adropin as a
potential marker predicting obesity and obesity-associated cancer
in korean patients with type 2 diabetes mellitus. J Cancer Prev.
23:191–196. 2018. View Article : Google Scholar
|
|
95
|
Soltani S, Beigrezaei S, Malekahmadi M,
Clark CCT and Abdollahi S: Circulating levels of adropin and
diabetes: A systematic review and meta-analysis of observational
studies. BMC Endocr Disord. 23:732023. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Palizban AA, Yazdani AH and
Jahanbani-Ardakani H: Role of rs7903146 polymorphism and adropin
serum level in patients with diabetes mellitus; a case-control
study from Isfahan, Iran. Arch Physiol Biochem. 128:378–381. 2022.
View Article : Google Scholar
|
|
97
|
Davoodi M, Hesamabadi BK, Ariabood E,
Izadi MR, Ghardashi-Afousi A, Bigi MAB, Asvadi-Fard M and Gaeini
AA: Improved blood pressure and flow-mediated dilatation via
increased plasma adropin and nitrate/nitrite induced by
high-intensity interval training in patients with type 2 diabetes.
Exp Physiol. 107:813–824. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Tičinović Kurir T, Miličević T, Novak A,
Vilović M and Božić J: Adropin-potential link in cardiovascular
protection for obese male type 2 diabetes mellitus patients treated
with liraglutide. Acta Clin Croat. 59:344–350. 2020.
|
|
99
|
Wang Q, An Y, Zhang L, Zhang Y, Wang G and
Liu J: Regulation of Adropin by Sitagliptin monotherapy in
participants with newly diagnosed type 2 diabetes. BMC Endocr
Disord. 22:3062022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Wang X, Liu C, Jiang H, Chen BC, Yang X,
Xiao M, Xie YQ and Li K: Network pharmacology and verification
experiment-based prediction of active components and potential
targets of Alpiniae Oxyphyllae Fructus-Saposhnikoviae Radix
(Yizhiren-Fangfeng) for treatment of diabetic kidney disease.
Tradit Med Res. 8:262023. View Article : Google Scholar
|
|
101
|
Liu SM, Yan ZJ, Xiao M and Xie YQ:
Mechanistic study of lipid metabolism disorders in diabetic kidney
disease treated with GLQMP based on network pharmacology, molecular
docking and in vitro experiments. Tradit Med Res. 9:112024.
View Article : Google Scholar
|
|
102
|
Es-Haghi A, Al-Abyadh T and Mehrad-Majd H:
The clinical value of serum adropin level in early detection of
diabetic nephropathy. kidney Blood Press Res. 46:734–740. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Liu M, Ai J, Shuai Z, Tang K, Li Z and
Huang Y: Adropin alleviates myocardial fibrosis in diabetic
cardiomyopathy rats: A preliminary study. Front Cardiovasc Med.
8:6885862021. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Li S, Sun J, Hu W, Liu Y, Lin D, Duan H
and Liu F: The association of serum and vitreous adropin
concentrations with diabetic retinopathy. Ann Clin Biochem.
56:253–258. 2019. View Article : Google Scholar
|
|
105
|
Yang C, DeMars KM and Candelario-Jalil E:
Age-Dependent decrease in adropin is associated with reduced levels
of endothelial nitric oxide synthase and increased oxidative stress
in the rat brain. Aging Dis. 9:322–330. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Shahdadian F, Saneei P, Lotfi K, Feizi A,
Askari G and Safavi SM: Association of plant-based diets with
adropin, atherogenic index of plasma, and metabolic syndrome and
its components: A cross-sectional study on adults. Front Nutr.
10:10777092023. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Yang C, DeMars KM, Hawkins KE and
Candelario-Jalil E: Adropin reduces paracellular permeability of
rat brain endothelial cells exposed to ischemia-like conditions.
Peptides. 81:29–37. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Jurrissen TJ, Ramirez-Perez FI,
Cabral-Amador FJ, Soares RN, Pettit-Mee RJ, Betancourt-Cortes EE,
McMillan NJ, Sharma N, Rocha HNM, Fujie S, et al: Role of adropin
in arterial stiffening associated with obesity and type 2 diabetes.
Am J Physiol Heart Circ Physiol. 323:H879–H891. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Sato K, Yamashita T, Shirai R, Shibata K,
Okano T, Yamaguchi M, Mori Y, Hirano T and Watanabe T: Adropin
contributes to anti-atherosclerosis by suppressing
monocyte-endothelial cell adhesion and smooth muscle cell
proliferation. Int J Mol Sci. 19:12932018. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Li L and Xie W: LncRNA HDAC11-AS1
suppresses atherosclerosis by inhibiting HDAC11-Mediated adropin
histone deacetylation. J Cardiovasc Transl Res. 15:1256–1269. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Ying T, Wu L, Lan T, Wei Z, Hu D, Ke Y,
Jiang Q and Fang J: Adropin inhibits the progression of
atherosclerosis in ApoE(−/−)/Enho(−/−) mice by regulating
endothelial-to-mesenchymal transition. Cell Death Discov.
9:4022023. View Article : Google Scholar
|
|
112
|
Abbasian S, Ravasi AA, Soori R and Aydin
S, Choobineh S and Aydin S: High-intensity interval training
ameliorates endothelial dysfunction through adropin, nitric oxide,
MR-proADM, and copeptin changes in overweight subjects. Hormones
(Athens). 21:707–717. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Kamma E, Lasisi W, Libner C, Ng HS and
Plemel JR: Central nervous system macrophages in progressive
multiple sclerosis: Relationship to neurodegeneration and
therapeutics. J Neuroinflammation. 19:452022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
McGinley MP, Goldschmidt CH and Rae-Grant
AD: Diagnosis and treatment of multiple sclerosis: A review. JAMA.
325:765–779. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Cinkir U, Bir LS, Topsakal S, Avci Cicek E
and Tekin S: Investigation of blood leptin and adropin levels in
patients with multiple sclerosis: A CONSORT-clinical study.
Medicine (Baltimore). 100:e272472021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Algul S and Ozcelik O: Evaluating the
energy regulatory hormones of nesfatin-1, irisin, adropin and
preptin in multiple sclerosis. Mult Scler Relat Disord.
68:1042212022. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Demirdöğen F, Akdağ T, Gündüz ZB and
Odabaş FO: Investigation of serum adropin levels and its
relationship with hypothalamic atrophy in patients with multiple
sclerosis. Mult Scler Relat Disord. 67:1039992022. View Article : Google Scholar
|
|
118
|
Rao A and Herr DR: G protein-coupled
receptor GPR19 regulates E-cadherin expression and invasion of
breast cancer cells. Biochim Biophys Acta Mol Cell Res.
1864:1318–1327. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Stelcer E, Milecka P, Komarowska H, Jopek
K, Tyczewska M, Szyszka M, Lesniczak M, Suchorska W, Bekova K,
Szczepaniak B, et al: Adropin stimulates proliferation and inhibits
adrenocortical steroidogenesis in the human adrenal carcinoma
(HAC15) cell line. Front Endocrinol (Lausanne). 11:5613702020.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Jia L, Liao L, Jiang Y, Hu X, Lu G, Xiao
W, Gong W and Jia X: Low-dose adropin stimulates inflammasome
activation of macrophage via mitochondrial ROS involved in
colorectal cancer progression. BMC Cancer. 23:10422023. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Hu J, Wu Q, Ding Q, Wu W, Li Q and Zheng
Z: High level of adropin promotes the progression of pancreatic
ductal adenocarcinoma. Curr Cancer Drug Targets. 24:629–641. 2024.
View Article : Google Scholar
|
|
122
|
Butler AA and Havel PJ: Adropin and
insulin resistance: Integration of endocrine, circadian, and stress
signals regulating glucose metabolism. Obesity (Silver Spring).
29:1799–1801. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Smati S, Régnier M, Fougeray T, Polizzi A,
Fougerat A, Lasserre F, Lukowicz C, Tramunt B, Guillaume M, Burnol
AF, et al: Regulation of hepatokine gene expression in response to
fasting and feeding: Influence of PPAR-α and insulin-dependent
signalling in hepatocytes. Diabetes Metab. 46:129–136. 2020.
View Article : Google Scholar
|
|
124
|
Ozkan A, Aslan MA, Sinen O, Munzuroglu M,
Derin N, Parlak H, Bulbul M and Agar A: Effects of adropin on
learning and memory in rats tested in the Morris water maze.
Hippocampus. 32:253–263. 2022. View Article : Google Scholar : PubMed/NCBI
|