Introduction
Clinical management of metastatic colorectal cancer
(MCRC) faces with different options and lines of treatment
according to patients’ fitness [age, performance status (PS),
comorbidities], extension of metastatic disease [liver-limited
(L-L) or other/multiple metastatic (O/MM)], KRAS genotype
(1–4). First line triplet chemotherapy, or
doublets plus bevacizumab (BEV) or cetuximab, reported overlapping
activity and efficacy in phase III trials, ranging between ORR
39–68%, PFS 7.2–10.6 months and OS 19.9–26.1 months (2,5,6).
More intensive regimens, consisting of triplet chemotherapy plus
targeted agents, can further increase activity, efficacy and
effectiveness of liver metastasectomies (7–9).
In clinical practice, a decision-making process
including functional, nutritional, and co-morbidity status is
required to tailor first line medical treatment (10). Elderly status (age >65 years),
PS >2, and/or comorbidities represent major features, to limit
toxicities and maintain quality of life (QoL). Elderly MCRC
patients are prevalent, and a clinical challenge is to select
between intensive or tailored medical treatments, by properly
weighing expected safety and efficacy, and according to prognostic
factors. Retrospective studies showed that elderly patients benefit
from 5-fluorouracil (5-FU) (11–13),
irinotecan (CPT-11)-containing therapy (14,15),
FOLFOX (16) to the same extent as
younger (17–19). In the OPTIMOX1 trial, ORR 59%, PFS
9.0 months and OS 20.7 months were comparable between old-elderly
and younger patients treated with FOLFOX (20). Treatment efficacy was also
comparable with BEV associated to 5-FU/CPT-11 (21). In elderly patients, addition of BEV
to 5-FU based chemotherapy significantly prolonged PFS (9.2-9.3
months) and OS (17.4–19.3 months) (22,23).
In BRiTE and BEAT studies, no different PFS was observed in elderly
patients; median OS decreased with age (24,25).
In the randomized phase III trial comparing FOLFIRI with FOLFOXIRI,
age was not significantly related to activity and efficacy, with OS
16.9 and 19.9 months, respectively (26,27).
ORR was significantly lower in older patients treated with
FOLFOXIRI (27). Patients
underwent metastasectomies without increased morbidity or
mortality, irrespective of age. Patients with PS 2 presented a
significantly lower OS and PFS, irrespectively of FOLFIRI or
FOLFOXIRI chemotherapy regimen (27). Age and/or comorbidities did not
affect efficacy in patients treated with cetuximab added to FOLFOX
or FOLFIRI (28). In elderly and
PS 2 patients, PFS was not increased by addition of panitumumab to
FOLFOX (29). A meta-analysis
showed that PS 1 compared to PS 2 significantly affect prognosis,
regardless of treatment, with ORR 43.8 vs 32%, PFS 7.6 vs 4.9
months, OS 17.3 and 8.5 months, respectively (30). The FOCUS2 randomized trial
prospectively evaluated first line chemotherapy options consisting
of 80% dose 5-FU or capecitabine, with or without oxaliplatin
(OXP), in old-elderly and/or frail patients, and showed that
addition of OXP significantly improved ORR (35 vs 13%), a trend of
PFS (5.8 vs. 4.5 months, hazard ratio 0.84, p=0.07), but not OS
(31), without significantly
increasing toxicity, with a negative impact on QoL.
KRAS mutations occur in 35–45% of colorectal
cancer (CRC), mostly codon 12 (80%), prevalently c.35 G>A (G12D)
transversion (32.5%) (32,33), impairing the intrinsic GTPase
activity, and leading to constitutive, growth factor
receptor-independent activation of downstream signalling (34). In the in vitro model
proposed by Guerrero et al (35), codon 12 mutations increase
aggressiveness by the differential regulation of KRAS downstream
pathways that lead to inhibition of apoptosis, enhanced loss of
contact inhibition and increased predisposition to
anchorage-independent growth. KRAS genotype, wild-type or
mutant, addresses the addition of targeted agents in MCRC medical
treatment: anti-EGFR or anti-VEGF to doublet chemotherapy in
KRAS wild-type (36–39);
BEV to 5-FU, CPT-11 in KRAS mutant, significantly predicting
prolonged PFS, while not OS and activity (36,37).
Clinical outcome in wild-type and mutant patients
assesses the prognostic relevance of KRAS genotype,
depending on differential tumor biological aggressiveness (4), including the predictive effectiveness
of treatment strategies. Median OS of patients treated with BEV
added to CPT-11/5-FU or triplet chemotherapy was different in
KRAS wild-type and mutant patients, but not significantly
(4,8,36,37);
KRAS wild-type L-L patients may achieve a significantly
greater benefit from integration with liver metastasectomies, with
respect to mutant patients (4). We
recently reported that the prevalent KRAS c.35 G>A (G12D)
mutant genotype may significantly affect worse OS of MCRC patients
treated with FIr-B/FOx, compared to wild-type or different other
mutations (40). Here, we report a
retrospective exploratory analysis evaluating tailored first line
treatments, the prognostic value of KRAS genotype, and of
the c.35 G>A mutation, in consecutive MCRC patients not eligible
for intensive first line FIr-B/FOx expanded clinical program, due
to age and/or comorbidities.
Materials and methods
Patient eligibility
Consecutive MCRC patients not eligible, due to
comorbidities and/or age, for expanded clinical program or ongoing
phase II trial proposing intensive regimens consisting of triplet
chemotherapy plus targeted agent, were treated in clinical practice
with first line medical and/or surgical treatments, chosen among
those in indication for MCRC treatment and approved by Agenzia
Italiana del Farmaco (AIFA) for administration in label in
Italian public hospitals, and published in Gazzetta Ufficiale
Repubblica Italiana (‘Elenco dei Medicinali erogabili a totale
carico del Servizio sanitaria nazionale’, Gazzetta Ufficiale
Repubblica Italiana N.1, 2 Gennaio 2009). Thus, it was not a
clinical trial and approval by ethics committee and institutional
review board was not necessary, because patients were treated with
conventional treatments without any additional medical intervention
out of the best common clinical practice. Patients had histological
confirmed diagnosis of MCRC, age ≥18 years, PS ≤2. Criteria to
define patients unfit, or not eligible for intensive regimens were:
age ≥75 years; uncontrolled severe diseases; cardiovascular disease
(uncontrolled hypertension, uncontrolled arrhythmia, ischemic
cardiac diseases in the last year); thromboembolic disease,
coagulopathy, preexisting bleeding diatheses; proteinuria >1
g/24 h. Patients were classified according to Cumulative Illness
Rating Scale (CIRS) (10).
Treatment options were tailored according to age (< or ≥75
years), patient’s fitness (PS, CIRS), KRAS genotype.
Patients with PS 3 were not treated. All patients provided written,
informed consent to the proposed in label treatment
option.
Methods
Medical treatment regimens
Medical treatments included triplet, doublet, or
mono-chemotherapy. Triplet FIr/FOx schedule consisted of weekly
timed-flat-infusion 5-FU (TFI 5-FU), associated to weekly
alternating CPT-11 or L-OXP (41):
TFI/5-FU (Fluorouracil Teva; Teva Italia, Milan, Italy), 750–900
mg/m2/die, over 12 h (from 10:00 pm to 10:00 am), days
1–2, 8–9, 15–16, 22–23; CPT-11 (Campto; Pfizer, Latina, Italy),
120–160 mg/m2, days 1 and 15; l-OXP (Eloxatin;
Sanofi-Aventis, Milan, Italy), 70–80 mg/m2, days 8 and
22; cycles every 4 weeks. Other triplet, doublet and mono-regimens
were administered according to previously reported schedules
(7,41,42).
Targeted agents were: BEV (Avastin; Roche, Welwyn Garden City, UK),
5 mg/kg, days 1 and 15; cetuximab (Erbitux; Merck, Darmstadt,
Germany), 400 mg/m2 initial dose, then 250
mg/m2/week.
Mutational analysis
Genetic analyses were performed on paraffin-embedded
tissue blocks from primary tumor and/or metastatic sites, as
previously reported (4). Genotype
status was assessed for KRAS codon 12 and 13 mutations by
direct sequencing. KRAS exon 2 sequence was performed from
PCR-amplified tumor DNA using the Big Dye V3.1 Terminator kit,
electrophoresis in ABI PRISM 3130xl Genetic Analyzer, and analysis
using the GeneMapper Analysis software version 4.0 (Applied
Biosystems, Foster City, CA, USA).
Study design
Activity, efficacy, and prognostic relevance of
first line treatments, and KRAS genotype on clinical
outcomes were evaluated. Patients were classified according to:
metastatic extension, L-L and O/MM (3,4);
age, non-elderly (<65 years), young-elderly (≥65 <75 years),
old-elderly (≥75 years); CIRS stage primary, intermediate,
secondary. Clinical evaluation of response was made by CT scan; PET
was added based on investigators’ assessment. Follow-up was
scheduled every two-three months up to disease progression or
death. L-L patients were evaluated at baseline and every two-three
cycles of treatment by a multidisciplinary team, to evaluate
resectability defined according to reported categories (3). Liver metastasectomies were defined as
R0, if radical surgery, R1, if radioablation was added. Surgery was
recommended >4 weeks after BEV discontinuation.
Clinical criteria of activity and efficacy were ORR,
resection rate of metastases, PFS and OS: ORR, evaluated according
to RECIST criteria (43);
pathologic complete response, defined as no residual cancer cells
in surgical specimens; PFS and OS, evaluated using the Kaplan-Meier
method (44). PFS was defined as
the length of time from the beginning of treatment and disease
progression or death (resulting from any cause) or to the last
contact; OS as the length of time between the beginning of
treatment and death or to last contact. Log-rank test was used to
compare PFS and OS according to medical treatment, KRAS
genotype, metastatic extension, age and comorbidity stage (45).
Results
Patient demographics
Forty patients unfit for intensive regimens, among
72 consecutive MCRC (56%), were treated with (Table I): medical treatments, 37 patients
(92.5%); surgery, 3 (7.5%). First line medical treatments: triplet,
18 (45%); doublet, 15 (37.5%); mono-therapy, 4 (10%). Among 39
KRAS evaluated patients (97.5%), 23 (59%) were wild-type and
16 (41%) mutant. Clinical features of the 37 patients who underwent
first line medical treatments were (Table IIA): male/female ratio, 22/15;
median age, 75 years; young- and old-elderly, 28 (76%) and 20
(54%), respectively; PS 0, 15 (41%) and 1–2, 22 (59%); metastatic
disease metachronous 24%, synchronous 76%. Liver metastases, 26
patients (70%); L-L 8 (22%), O/MM 29 79%). Distribution of patients
according to age and comorbidity stage (Table IIB): non-elderly 9 (24%),
young-elderly 8 (22%), old-elderly 20 (54%); CIRS stage primary 4
(11%), intermediate 15 (40%), secondary 18 (42%). KRAS
mutations detected in 15 patients were: codon 12, 13 (36.1%),
specifically c.35 G>A (G12D), 7 (19.4%), c.35 G>T (G12V), 6
(16.6%); codon 13, 2 (5.5%), c.37 G>T (G13V), 1 (2.7%) and c.38
G>A (G13D), 1 (2.7%).
 | Table I.First line clinical management of
unfit MCRC patients. |
Table I.
First line clinical management of
unfit MCRC patients.
| Overall | KRAS
genotype |
|---|
|
|
|---|
| No. of patients
(%) | Wild-type (%) | Mutant (%) |
|---|
| Total no. | 40 | 23 | 16 |
| Medical
treatment | 37 (92.5) | 21 (91) | 15 (94) |
| Triplet
regimen | 18 (45) | 8 (35) | 10 (62.5) |
| Doublet
chemotherapy plus bevacizumab | 3 | 1 | 2 |
| Doublet
chemotherapy plus cetuximab | 5 | 5 | - |
| Triplet
chemotherapy | 10 | 2 | 8 |
| Doublet
regimen | 15 (37.5) | 12 (52) | 3 (19) |
| Mono-chemotherapy
plus bevacizumab | 2 | - | 2 |
| Mono-chemotherapy
plus cetuximab | 8 | 8 | - |
| Doublet
chemotherapy | 5 | 4 | 1 |
| Mono-therapy | 4 (10) | 1 (4) | 2 (12.5) |
|
Mono-chemotherapy | 4 | 1 | 2 |
| Surgery | 3 | 2 | 1 |
 | A, Features of the unfit patients |
A, Features of the unfit patients
| Overall treated
Total no. (%) | KRAS
wild-type Total no. (%) | KRAS mutant
Total no. (%) |
|---|
| No. of
patients | 37 | 21 (58) | 15 (42) |
| Gender | | | |
| Male/female | 22/15 | 12/9 | 10/5 |
| Age, years | | | |
| Median | 75 | 77 | 69 |
| Range | 45–87 | 45–83 | 50–87 |
| Elderly | | | |
| ≥65 years | 28 (76) | 18 (86) | 9 (60) |
| ≥75 years | 20 (54) | 13 (62) | 7 (47) |
| WHO performance
status | | | |
| 0 | 15 (41) | 10 (48) | 5 (33) |
| 1–2 | 22 (59) | 11 (52) | 10 (69) |
| CIRS stage | | | |
| Primary | 4 (11) | 1 (5) | 2 (13) |
| Intermediate | 15 (41) | 7 (33) | 8 (53) |
| Secondary | 18 (48) | 13 (62) | 5 (33) |
| Metastatic
disease | | | |
| Metachronous | 9 (24) | 5 (24) | 3 (20) |
| Synchronous | 28 (76) | 16 (76) | 12 (80) |
| Primary tumor | | | |
| Colon | 25 (68) | 13 (62) | 12 (80) |
| Rectum | 12 (32) | 8 (38) | 3 (20) |
| Sites of
metastases | | | |
| Liver | 26 (70) | 16 (76) | 9 (60) |
| Lung | 14 (38) | 6 (29) | 8 (53) |
| Lymph nodes | 11 (30) | 6 (29) | 4 (27) |
| Local | 7 (19) | 2 (9) | 4 (27) |
| Other | 7 (19) | 4 (19) | 3 (20) |
| No. of involved
sites | | | |
| 1 | 14 (38) | 9 (43) | 5 (33) |
| ≥2 | 23 (62) | 12 (57) | 10 (69) |
| Single metastatic
sites | | | |
|
Liver-limited | 8 (22) | 7 (33) | 1 (7) |
| Other than
liver | 8 (22) | 3 (14) | 5 (33) |
| Lung | 3 (8) | - | 3 (20) |
| Lymph
nodes | 1 (3) | 1 (5) | - |
| Local | 4 (11) | 2 (9) | 2 (13) |
| Multiple metastatic
sites | 21 (57) | 11 (52) | 9 (60) |
| Liver
metastases | | | |
| Single | 3 (8) | 3 (14) | - |
| Multiple | 23 (62) | 13 (62) | 9 (60) |
| Previous adjuvant
chemotherapy: | 7 (19) | 2 (9) | 5 (33) |
| FA/5-FU
bolus | 1 (3) | 1 (5) | - |
| XelOx or
5-FU/OXP | 6 (16) | 1 (5) | 5 (33) |
| Previous
radiotherapy: | 4 (11) | 3 (14) | 1 (7) |
| RT+CT (5-FU
continous infusion) | 3 (8) | 2 (9) | 1 (7) |
| RT+CT
(XELOX) | 1 (3) | 1 (5) | - |
 | B, Age and comorbidity stage in unfit
patients |
B, Age and comorbidity stage in unfit
patients
| Age | Cumulative illness
rating scale (CIRS) | Total no. (%) |
|---|
|
|---|
| Primary | Intermediate | Secondary |
|---|
| Non-elderly | 2 | 5 | 2 | 9 (24) |
| Young-elderly | 1 | 3 | 4 | 8 (22) |
| Old-elderly | 1 | 7 | 12 | 20 (54) |
| Total no. (%) | 4 (11) | 15 (40) | 18 (49) | 37 |
Medical treatments were tailored according to age
and CIRS stage. Triplet regimens were administered in 18 patients
(49%): non-elderly 6, young-elderly 4, old-elderly 8; CIRS primary
2, intermediate 10, secondary 6. Doublet regimens were administered
in 15 patients (40%): non-elderly 3, young-elderly 3, old-elderly
9; CIRS primary 1, intermediate 4, secondary 10. Mono-regimens were
administered in 4 patients (11%): young-elderly 1, old-elderly 3;
CIRS primary 1, intermediate 1, secondary 2.
Overall activity and efficacy
Among the 37 patients who underwent medical
treatments, 10 were not evaluable for activity: 7 (19%) did not
receive at least 2 cycles of treatment; 3 were on-treatment. The
intent-to-treat analysis of 27 patients showed ORR 37% (α 0.05, CI
± 19) (Table IIIA). We observed
10 objective responses: 9 partial (33%) and 1 complete (CR 4%); 9
stable diseases (33%); 8 progressive diseases (30%). Disease
control rate was 67% (α 0.05, CI ± 18). After median follow-up of 8
months, median PFS was 7 months (1-13+): 28 events occurred. Median
OS was 13 months (1+−23+): 22 events occurred (Fig. 1A). R0 liver metastasectomies were
performed in 3 patients (8%): 3 out of 8 L-L (37.5%). No
surgery-related complications were reported. Overall, 1 clinical
plus 1 pathologic CR were reported (7%); 1 patient showed a
progressive disease at 8 months; 1 patient was progression-free at
10 months. Pathologic CR was obtained in 1 KRAS wild-type
patient (33%), with primary rectal tumor and a single L-L
metastasis. Twelve patients (32%) received, at least, a second line
treatment.
 | A, Activity, efficacy and
effectiveness of first line regimens in unfit patients according to
KRAS genotype |
A, Activity, efficacy and
effectiveness of first line regimens in unfit patients according to
KRAS genotype
| All treated
Intent-to-treat Analysis | KRAS
wild-type Intent-to-treat Analysis | KRAS mutant
Intent-to-treat Analysis |
|---|
|
|
|
|---|
| No. | % | No. | % | No. | % |
|---|
| Enrolled
patients | 37 | 100 | 21 | 100 | 15 | 100 |
| Evaluable
patients | 27 | 70 | 14 | 67 | 12 | 80 |
| Objective
response | 10 | 37 (CI ± 19) | 7 | 50 (CI ± 27) | 3 | 25 (CI ± 26) |
| Partial
response | 9 | 33 | 6 | 43 | 3 | 25 |
| Complete
response | 1 | 4 | 1 | 7 | - | - |
| Stable disease | 9 | 33 | 4 | 29 | 5 | 42 |
| Progressive
disease | 8 | 30 | 3 | 21 | 4 | 33 |
| Median PFS,
months | 7 | | 8 | | 6 | |
| Range | 1−13+ | | 1+−13+ | | 1–11 | |
| Progression
events | 28 | 76 | 15 | 71 | 12 | 80 |
| Median OS,
months | 13 | | 13 | | 9 | |
| Range | 1+−23+ | | 1+−23+ | | 3–18 | |
| Deaths | 22 | 59 | 11 | 52 | 10 | 67 |
| Liver
metastasectomies | 3 | | 3 | | - | |
| No/overall
pts | 3/37 | 8 | 3/21 | 14 | - | - |
| No/patients with
liver metastases | 3/26 | 11.5 | 3/16 | 19 | - | - |
| No/patients with
L-L metastases | 3/8 | 37.5 | 3/7 | 43 | - | - |
| Pathologic complete
responses | 1 | 33 | 1 | 33 | - | - |
Among 7 evaluable L-L patients, ORR was 71%; 3
performed liver metastasectomies (43%) and 1 cCR (14%); median PFS
11 months (3–13+ months); median OS 12 months (3–13+ months). Among
20 evaluable O/MM patients, ORR was 25%; median PFS 6 months (1–12
months); median OS 13 months (1+−23+ months). Clinical outcome (PFS
and OS) in L-L compared to O/MM patients was not significantly
different (Fig. 1B).
Activity and efficacy according to
first line treatment, elderly and comorbidity status
Among 16 evaluable patients treated with triplet
regimens (Table IIIB), ORR was
37.5% (α 0.05, CI ± 24). We observed 6 partial responses (37.5%); 5
stable diseases (31%); 5 progressive diseases (31%). Median PFS was
8 months (3–12): 14 events occurred. Median OS was 12
months (3–23+ months): 12 events occurred. Secondary metastasectomy
was performed in 1 patient (6%). Among 15 patients treated with
doublet regimens (Table IIIB),
ORR was 44% (α 0.05, CI ± 34). We observed 3 partial responses
(33%); 1 CR (11%); 3 stable diseases (33%); 2 progressive diseases
(22%). Median PFS was 8 months (1–13+): 9 events occurred. Median
OS was 15 months (1+−23+ months): 7 events occurred. Among 4
patients treated with mono-regimens, median PFS was 5 months (3–6
months), median OS 6 months (3−13+ months). Among 3 patients who
underwent surgery as first line treatment, median PFS was not
reached (3+−19+ months); median OS not reached (3+−19+ months). PFS
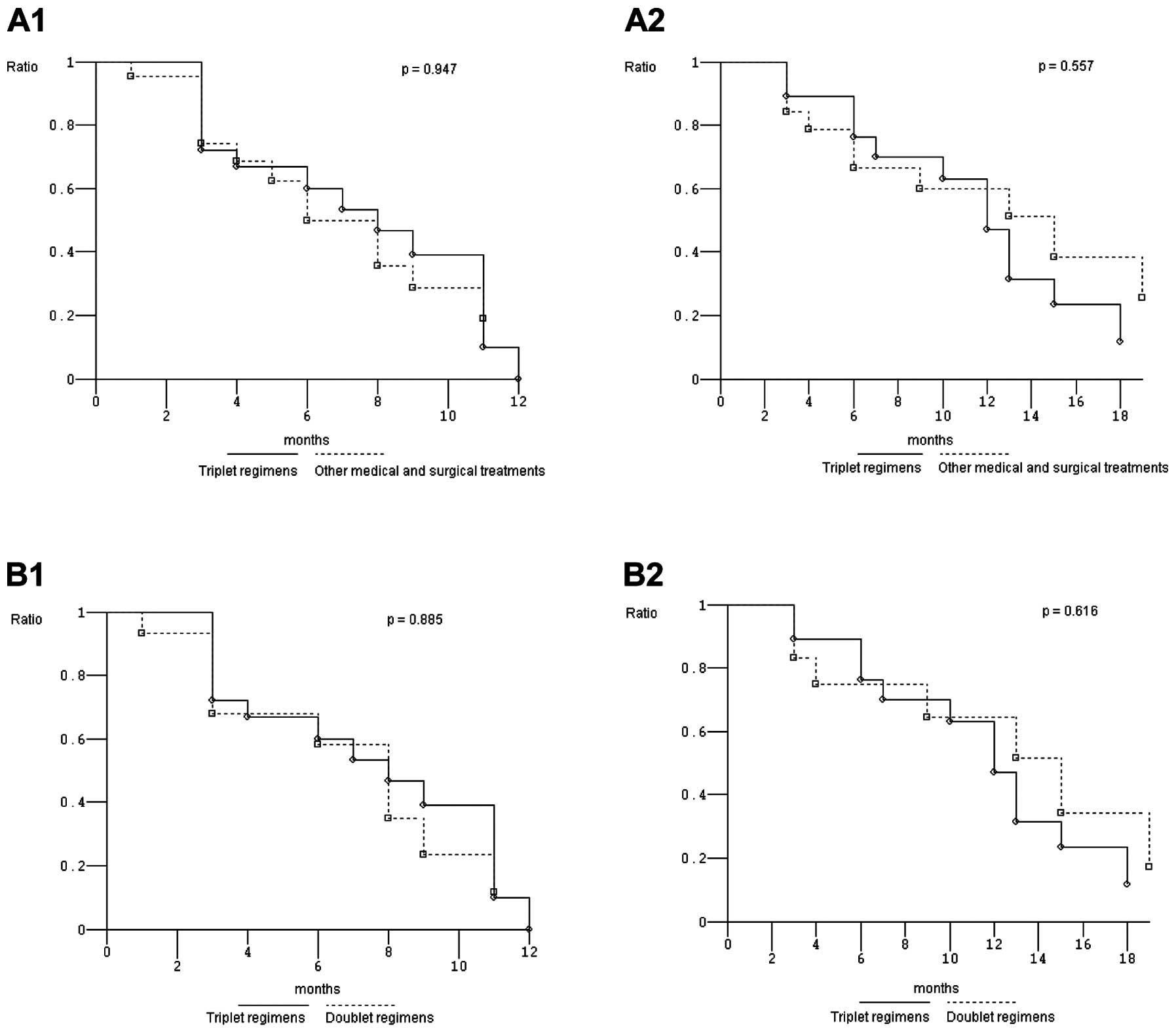
and OS were not significantly different in patients treated with
triplet compared to other first line treatments (p=0.947 and 0.557,
respectively), and to doublet regimens (p= 0.885 and 0.616,
respectively) (Fig. 2).
 | B, Activity, efficacy and
effectiveness according to first line treatments |
B, Activity, efficacy and
effectiveness according to first line treatments
| Intent-to-treat
analysis |
|---|
|
|---|
| Triplet
regimen | Doublet
regimen |
|---|
|
|
|---|
| No. | % | No. | % |
|---|
| Enrolled
patients | 18 | 100 | 15 | 100 |
| Evaluable
patients | 16 | 89 | 9 | 60 |
| Objective
response | 6 | 37.5 (CI ± 24) | 4 | 44 (CI ± 34) |
| Partial
response | 6 | 37.5 | 3 | 33 |
| Complete
response | - | - | 1 | 11 |
| Stable disease | 5 | 31 | 3 | 33 |
| Progressive
disease | 5 | 31 | 2 | 22 |
| Median PFS,
months | 8 | | 8 | |
| Range | 3–12 | | 1−13+ | |
| Progression
events | 14 | 78 | 9 | 60 |
| Median OS,
months | 12 | | 15 | |
| Range | 3−23+ | | 1+−23+ | |
| Deaths | 12 | 67 | 7 | 47 |
| Liver
metastasectomies | 1 | 6 | 1 | 11 |
| Pathologic complete
responses | 1 | 100 | - | - |
Moreover, PFS and OS were not significantly
different in non-elderly and young-elderly compared to old-elderly
patients (p=0.240 and 0.750, respectively), and in primary and
intermediate CIRS stage compared to secondary stage patients
(p=0.494 and 0.364, respectively).
Prognostic relevance of KRAS genotype
and c.35 G>A KRAS mutation
Among 14 KRAS wild-type patients evaluable
for activity, ORR was 50% (α 0.05, CI ± 27) (Table IIIA). We observed 7 objective
responses: 6 partial (43%) and 1 CR (7%); 4 stable diseases (29%);
3 progressive diseases (21%). Disease control rate was 79% (α 0.05,
CI ± 22). Liver metastasectomies were performed in 3 patients
(14%), 3 out of 7 L-L (43%). Median PFS was 8 months (1+−13+
months), 15 events occurred (71%). Median OS was 13 months (1+−23+
months), 11 events occurred. Among 12 KRAS mutant patients
evaluable for activity, ORR was 25% (α 0.05, CI ± 26). We observed
3 partial responses (25%); 5 stable diseases (42%); 4 progressive
diseases (33%). Disease control rate was 67% (α 0.05, CI ± 28). No
liver metastasectomies were performed. Median PFS was 6 months
(1–11 months), 12 events occurred (80%). Median OS was 8 months
(3–18 months), 10 events occurred. KRAS wild-type compared
with mutant patients showed significantly different PFS (p=0.043),
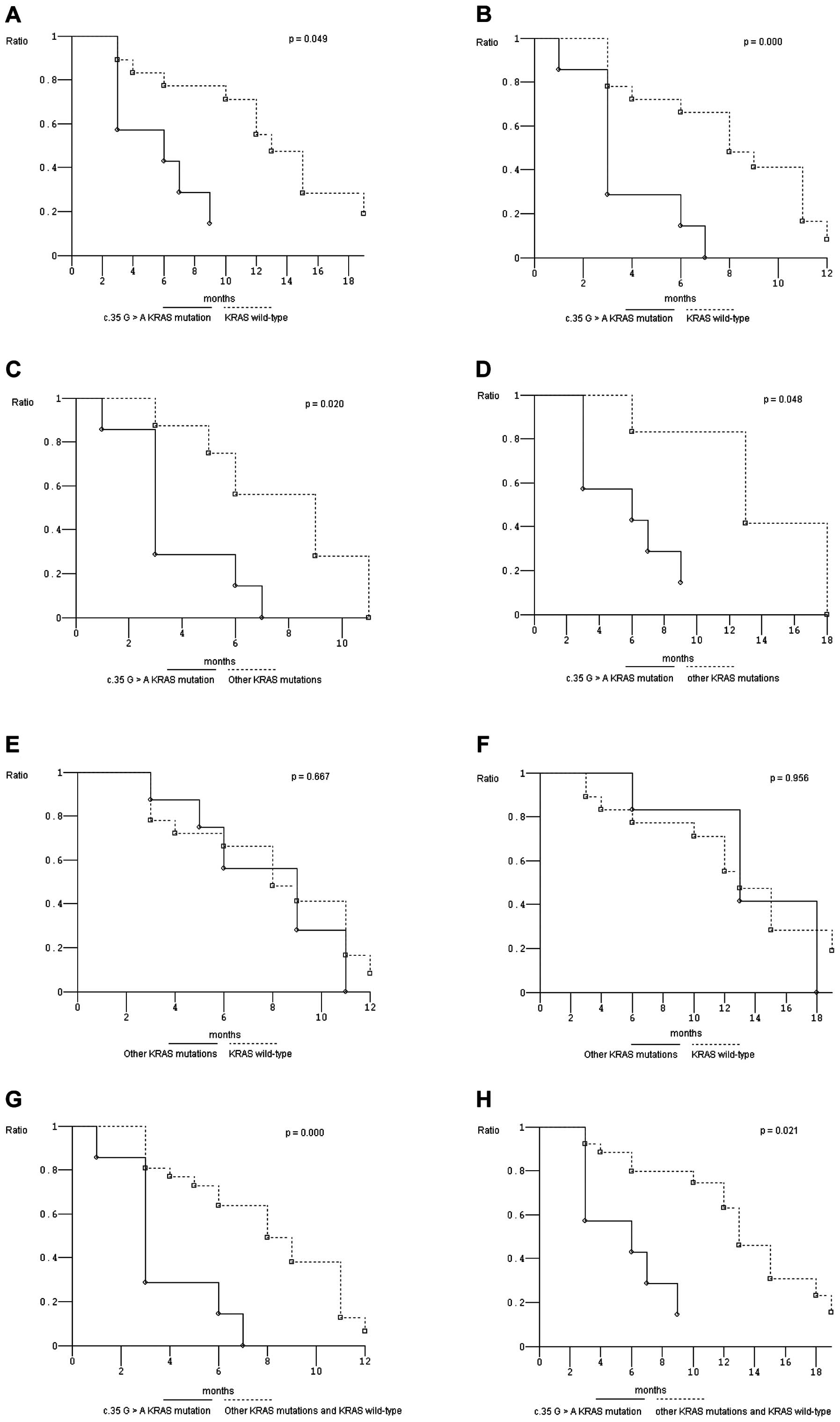
but not OS (Fig. 1C). KRAS
c.35 G>A mutant patients showed significantly worse PFS and OS
compared to wild-type (p=0.000, and 0.049, respectively) (Fig. 3A and B), and to other mutant
patients (p=0.020 and 0.048, respectively) (Fig. 3C and D). No different clinical
outcomes were reported in other than c.35 G>A KRAS mutant
compared to wild-type patients (Fig.
3E and F). PFS and OS were also significantly worse in c.35
G>A KRAS mutant patients compared to other mutant plus
wild-type patients (p=0.000, and 0.021, respectively) (Fig. 3G and H).
Discussion
Patients unfit for first line FIr-B/FOx intensive
regimen, due to age (≥75 years) and/or comorbidities, were
prevalent (56%), mostly elderly (76%), particularly old-elderly
patients (54%), prevalently PS 1–2 (59%), CIRS stage
intermediate/secondary (89%), O/MM disease (79%). Most unfit MCRC
patients were treated with triplet or doublet regimens (49 and 40%,
respectively), and some (19%) did not reach the first evaluation of
activity at 2–3 months.
Retrospective evaluations of doublets consisting of
CPT-11 or OXP, associated to 5-FU or capecitabine in elderly
patients eligible for clinical trials gained ORR 18–59.4%, PFS
4.9–10.0 months and OS 8.5–20.7 months (11–16,20,30,31,46).
BEV addition to 5-FU-based chemotherapy in elderly patients
significantly increased PFS up to 9.2–9.3 months and OS up to
17.4–19.3 months (22,23). Triplet chemotherapy or doublets
plus BEV obtained ORR 34.9–45.9%, PFS 7.9–9.3 months and OS
17.4–20.5 months (23–25). The present tailored approach, based
on evaluation of elderly status and/or CIRS, prevalently addressing
doublet and triplet regimens, reported ORR 37%, PFS 7 months and OS
13 months. Selected medical treatment, triplet compared to doublet,
did not significantly affected PFS and OS, nor advanced age, or
CIRS stage. The FOCUS2 randomized trial evaluating first line
reduced dose 5-FU or capecitabine and OXP in old-elderly and/or
frail patients showed significantly improved ORR 35%, with PFS 5.8
months (31). The meta-analysis
evaluating the effect of PS on clinical outcome showed that PS 1
compared to PS 2 significantly affected prognosis, regardless of
treatment, with ORR 43.8 vs 32%, PFS 7.6 vs 4.9 months, OS 17.3 and
8.5 months, respectively (30). In
the HORG-FOLFOXIRI trial, elderly compared to non-elderly patients
treated with FOLFIRI or FOLFOXIRI showed no different clinical
outcome; significantly lower PFS and OS were reported in patients
with PS 2 (26,27).
Young-elderly patients eligible for FIr-B/FOx
intensive regimen, prevalently characterised by PS 0 (89%) and
intermediate CIRS stage (93%), reported ORR 79%, PFS 11 months, OS
21 months, equivalent to overall patients (7,47). A
complex decision-making process discriminating patients’ fitness,
and tailoring a personalized medical treatment, is challenging:
patients unfit for FIr-B/FOx can be treated with a two-drug first
line combination regimen (31),
but showed worse clinical outcome. No increased morbidity, nor
mortality was reported in unfit patients who underwent secondary
liver metastasectomies, reported as significantly higher in elderly
patients (8%) (48).
Overall in MCRC patients treated with BEV added to
CPT-11/5-FU, or with more intensive regimens (FIr-B/FOx,
FOLFOXIRI/BEV), PFS and OS were not significantly different in
KRAS wild-type and mutant (4,6,8,37) as
well as in young-elderly patients (47). Recently, KRAS geno-type was
reported as significantly affecting PFS and OS in patients treated
with XelOx/BEV (49). We recently
reported in MCRC patients treated with FIr-B/FOx, that the
prevalent KRAS c.35 G>A (G12D) mutant genotype may
significantly affect worse OS, compared to wild-type or other
mutations (40). Present data
reported for the first time that in patients unfit for FIr-B/FOx,
KRAS wild-type compared to mutant patients showed a
significantly different PFS, and not OS. Furthermore, KRAS
c.35 G>A mutant genotype may affect significantly worse PFS and
OS, compared to wild-type and/or other mutant, confirming that
KRAS genotype, particularly c.35 G>A mutant, confers
different biological aggressiveness (35), less effectively overcome by
conventional triplet and doublet regimens. The prognostic relevance
of KRAS genotype, particularly c.35 G>A mutant (4,40),
and the predictive relevance of different medical treatments
according to patients’ fitness for intensive regimens, should be
prospectively evaluated.
In conclusion, in MCRC patients unfit for first line
intensive FIr-B/FOx regimen, tailored doublet and triplet medical
treatments showed similar activity and efficacy, also according to
age and comorbidities. KRAS genotype may indicate different
PFS, and c.35 G>A KRAS mutant a significantly worse PFS
and OS, compared to wild-type and other mutations. Present findings
warrant prospective trials comparing clinical outcome in unfit
patients, according to KRAS genotype.
Acknowledgements
G.B. is a PhD student in
Biotechnology, Department of Biotechnological and Applied Clinical
Sciences, University of L’Aquila, funded by the University of
L’Aquila, Italy.
References
|
1.
|
Schmoll HJ, Van Cutsem E, Stein A,
Valentini V, Glimelius B, Haustermans K, Nordlinger B, van de Velde
CJ, Balmana J, Regula J, Nagtegaal ID, Beets-Tan RG, Arnold D,
Ciardiello F, Hoff P, Kerr D, Köhne CH, Labianca R, Price T,
Scheithauer W, Sobrero A, Tabernero J, Aderka D, Barroso S, Bodoky
G, Douillard JY, El Ghazaly H, Gallardo J, Garin A, Glynne-Jones R,
Jordan K, Meshcheryakov A, Papamichail D, Pfeiffer P, Souglakos I,
Turhal S and Cervantes A: ESMO Consensus Guidelines for management
of patients with colon and rectal cancer. A personalized approach
to clinical decision making. Ann Oncol. 23:2479–2516. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Ficorella C, Bruera G, Cannita K, Porzio
G, Lanfiuti Baldi P, Tinari N, Natoli C and Ricevuto E: Triplet
chemotherapy in patients with metastatic colorectal cancer: toward
the best way to safely administer a highly active regimen in
clinical practice. Clin Colorectal Cancer. 11:229–237. 2012.
View Article : Google Scholar
|
|
3.
|
Bruera G, Cannita K, Giuliante F, Lanfiuti
Baldi P, Vicentini R, Marchetti P, Nuzzo G, Antonucci A, Ficorella
C and Ricevuto E: Effectiveness of liver metastasectomies in
patients with metastatic colorectal cancer treated with FIr-B/FOx
triplet chemotherapy plus bevacizumab. Clin Colorectal Cancer.
11:119–126. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Bruera G, Cannita K, Di Giacomo D, Lamy A,
Troncone G, Dal Mas A, Coletti G, Frébourg T, Sabourin JC, Tosi M,
Ficorella C and Ricevuto E: Prognostic value of KRAS genotype in
metastatic colorectal cancer (MCRC) patients treated with intensive
triplet chemotherapy plus bevacizumab (FIr-B/FOx) according to
extension of metastatic disease. BMC Med. 10:1352012. View Article : Google Scholar
|
|
5.
|
Bruera G and Ricevuto E: Intensive
chemotherapy of meta-static colorectal cancer: weighing between
safety and clinical efficacy. Evaluation of Masi G, Loupakis F,
Salvatore L, et al: Bevacizumab with FOLFOXIRI (irinotecan,
oxaliplatin, fluorouracil, and folinate) as first-line treatment
for metastatic colorectal cancer: a phase 2 trial. Expert Opin Biol
Ther. 11:21–824. 2011.PubMed/NCBI
|
|
6.
|
Masi G, Vasile E, Loupakis F, Cupini S,
Fornaro L, Baldi G, Salvatore L, Cremolini C, Stasi I, Brunetti I,
Fabbri MA, Pugliesi M, Trenta P, Granetto C, Chiara S, Fioretto L,
Allegrini G, Crinò L, Andreuccetti M and Falcone A: Randomized
trial of two induction chemotherapy regimens in metastatic
colorectal cancer: an updated analysis. J Natl Cancer Inst.
103:21–30. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Bruera G, Santomaggio A, Cannita K,
Lanfiuti Baldi P, Tudini M, De Galitiis F, Mancini M, Marchetti P,
Antonucci A, Ficorella C and Ricevuto E: ‘Poker’ association of
weekly alternating 5-fluorouracil, irinotecan, bevacizumab and
oxaliplatin (FIr-B/FOx) in first line treatment of metastatic
colorectal cancer: a phase II study. BMC Cancer. 10:5672010.
|
|
8.
|
Masi G, Loupakis F, Salvatore L, Fornaro
L, Cremolini C, Cupini S, Ciarlo A, Del Monte F, Cortesi E, Amoroso
D, Granetto C, Fontanini G, Sensi E, Lupi C, Andreuccetti M and
Falcone A: Bevacizumab with FOLFOXIRI (irinotecan, oxaliplatin,
fluorouracil, and folinate) as first-line treatment for metastatic
colorectal cancer: a phase 2 trial. Lancet Oncol. 11:845–852. 2010.
View Article : Google Scholar
|
|
9.
|
Garufi C, Torsello A, Tumolo S, Ettorre
GM, Zeuli M, Campanella C, Vennarecci G, Mottolese M, Sperduti I
and Cognetti F: Cetuximab plus chronomodulated irinotecan,
5-fluorouracil, leucovorin and oxaliplatin as neoadiuvant
chemotherapy in colorectal liver metastases: POCHER trial. Br J
Cancer. 103:1542–1547. 2010. View Article : Google Scholar
|
|
10.
|
Extermann M, Overcash J, Lyman GH, Parr J
and Balducci L: Comorbidity and functional status are independent
in older cancer patients. J Clin Oncol. 16:1582–1587.
1998.PubMed/NCBI
|
|
11.
|
Folprecht G, Cunningham D, Ross P,
Glimelius B, Di Costanzo F, Wils J, Scheithauer W, Rougier P,
Aranda E, Hecker H and Kohne CH: Efficacy of 5-fluorouracil-based
chemotherapy in elderly patients with metastatic colorectal cancer:
a pooled analysis of clinical trials. Ann Oncol. 15:1330–1338.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Popescu RA, Norman A, Ross PJ, Parikh B
and Cunningham D: Adjuvant or palliative chemotherapy for
colorectal cancer in patients 70 years or older. J Clin Oncol.
17:2412–2418. 1999.PubMed/NCBI
|
|
13.
|
Chiara S, Nobile MT, Vincenti M, Lionetto
R, Gozza A, Barzacchi MC, Sanguineti O, Repetto L and Rosso R:
Advanced colorectal cancer in the elderly: results of consecutive
trials with 5-fluorouracil-based chemotherapy. Cancer Chemother
Pharmacol. 42:336–340. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Folprecht G, Seymour MT, Saltz L,
Douillard JY, Hecker H, Stephens RJ, Maughan TS, Van Cutsem E,
Rougier P, Mitry E, Schubert U and Kohne CH:
Irinotecan/fluorouracil combination in first-line therapy of older
and younger patients with meta-static colorectal cancer: combined
analysis of 2,691 patients in randomized controlled trials. J Clin
Oncol. 26:1443–1451. 2008. View Article : Google Scholar
|
|
15.
|
Mitry E, Douillard JY, Van Cutsem E,
Cunningham D, Magherini E, Mery-Mignard D, Awad L and Rouigier P:
Predictive factors of survival in patients with advanced colorectal
cancer: an individual data analysis of 602 patients included in
irinotecan phase III trials. Ann Oncol. 15:1013–1017. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Goldberg RM, Tabah-Fisch I, Bleiberg H, de
Gramont A, Tournigand C, Andre T, Rothenberg ML, Green E and
Sargent DJ: Pooled analysis of safety and efficacy of oxaliplatin
plus fluorouracil/leucovorin administered bimonthly in elderly
patients with colorectal cancer. J Clin Oncol. 24:4085–4091. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Pallis AG, Papamichael D, Audisio R,
Peeters M, Folprecht G, Lacombe D and Van Cutsem E: EORTC Elderly
Task Force experts’ opinion for the treatment of colon cancer in
older patients. Cancer Treat Rev. 36:83–90. 2010.
|
|
18.
|
Papamichael D, Audisio R, Horiot JC,
Glimelius B, Sastre J, Mitry E, Van Cutsem E, Gosney M, Kohne CH
and Aapro M: Treatment of the elderly colorectal cancer patient:
SIOG expert recommendations. Ann Oncol. 20:5–16. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Audisio RA and Papamichael D: Treatment of
colorectal cancer in older patients. Nat Rev Gastroenterol Hepatol.
9:716–725. 2012. View Article : Google Scholar
|
|
20.
|
Figer A, Perez-Staub N, Carola E,
Tournigand C, Lledo G, Flesch M, Barcelo R, Cervantes A, André T,
Colin P, Louvet C and de Gramont A: FOLFOX in patients aged between
76 and 80 years with metastatic colorectal cancer an exploratory
cohort of the OPTIMOX1 study. Cancer. 110:2666–2671.
2007.PubMed/NCBI
|
|
21.
|
Hurwitz HI, Fehrenbacher L, Novotny WF,
Cartwright T, Hainsworth J, Meropol NJ, Heim W, Berlin J, Baron A,
Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross M and
Kabbinavar FF: Bevacizumab plus irinotecan, fluorouracil, and
leucovorin for metastatic colorectal cancer. N Engl J Med.
350:2335–2342. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Kabbinavar FF, Hurwitz HI, Yi J, Sarkar S
and Rosen O: Addition of bevacizumab to fluorouracil-based
first-line treatment of metastatic colorectal cancer: pooled
analysis of cohorts of older patients from two randomized clinical
trials. J Clin Oncol. 27:199–205. 2008. View Article : Google Scholar
|
|
23.
|
Cassidy J, Saltz LB, Giantonio BJ,
Kabbinavar FF, Hurwitz HI and Rohr UP: Effect of bevacizumab in
older patients with metastatic colorectal cancer: pooled analysis
of four randomized studies. J Cancer Res Clin Oncol. 136:737–743.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Kozloff MF, Berlin J, Flynn PJ, Kabbinavar
F, Ashby M, Dong W, Sing AP and Grothey A; for the BRiTE
Investigators: Clinical outcomes in elderly patients with
metastatic colorectal cancer receiving bevacizumab and
chemotherapy: results from the BRiTE observational cohort study.
Oncology. 78:329–339. 2010. View Article : Google Scholar
|
|
25.
|
Van Cutsem E, Rivera F, Berry S,
Kretzschmar A, Michael M, Di Bartolomeo M, Mazier MA, Canon JL,
Georgoulias V, Peeters M, Bridgewater J and Cunningham D; on behalf
of the First BEAT investigators: Safety and efficacy of first-line
bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in
metastatic colorectal cancer: the BEAT study. Ann Oncol.
20:1842–1847. 2009.PubMed/NCBI
|
|
26.
|
Souglakos J, Andrulakis N, Syrigos K,
Polyzos A, Ziras N, Athanasiadis A, Kalolyris S, Tsousis S,
Kouroussis CH, Vamvakas L, Kalykaki A, Samonis G, Mavroudis D and
Georgoulias V: FOLFOXIRI (folin acid, 5-fluorouracil, oxaliplatin
and irinotecan) vs FOLFIRI (folin acid, 5-fluorouracil and
irinotecan) as first-line treatment in metestatic colorectal cancer
(MCC): a multicentre randomised phase III trial from the Hellenic
Oncology Research Group (HORG). Br J Cancer. 94:798–805. 2006.
|
|
27.
|
Vamvakas L, Athanasiadis A, Karampeazis A,
Kakolyris S, Polyzos A, Kouroussis C, Ziras N, Kalbakis K,
Georgoulias V and Souglakos J: Clinical outcome of elderly patients
with metastatic colorectal cancer treated with FOLFOXIRI versus
FOLFIRI: Subgroup analysis of a randomized phase III trial from the
Hellenic Oncology Research Group (HORG). Crit Rev Oncol Hematol.
76:61–70. 2010. View Article : Google Scholar
|
|
28.
|
Meyerhardt JA, Jackson McCleary N,
Niedzwiecki D, Hollis D, Venook A, Mayer R and Goldberg R: Impact
of age and comorbidities on treatment effect, tolerance, and
toxicity in metastatic colorectal cancer (mCRC) patients treated on
CALGB 80203. J Clin Oncol. 27(Suppl 15)4038:2009
|
|
29.
|
Douillard J, Siena S, Cassidy J, Tabernero
J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem
J, Rivera F, Kocàkova I, Ruff P, Blasinska-Morawiec M, Smakal M,
Canon JL, Rother M, Oliner KS, Wolf M and Gansert J: Randomized,
phase III trial of Panitumumab with infusional fluorouracil,
leicovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as
first-line treatment in patients with previously untreated
metastatic colorectal cancer: the PRIME trial. J Clin Oncol.
28:4697–4705. 2010. View Article : Google Scholar
|
|
30.
|
Sargent DJ, Kohne CH, Kelly Sanoff H, Bot
BM, Seymour MT, de Gramont A, Porschen R, Saltz LB, Rougier P,
Tournigand C, Douillard JY, Stephens RJ, Grothey A and Goldberg RM:
Pooled safety and efficacy analysis examining the effect of
performance status on outcomes in nine first-line treatment trials
using individual data from patients with metastatic colorectal
cancer. J Clin Oncol. 27:1948–1955. 2009. View Article : Google Scholar
|
|
31.
|
Seymour MT, Thompson LC, Wasan HS,
Middleton G, Brewster AE, Shepherd SF, O’Mahony MS, Maughan TS,
Parmar M and Langley RE; on behalf of the FOCUS2 Investigators, and
the National Cancer Research Institute Colorectal Cancer Clinical
Studies Group: Chemotherapy options in elderly and frail patients
with metastatic colorectal cancer (MRC FOCUS2): an open-label,
randomised factorial trial. Lancet. 377:1749–1759. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Andreyev HJ, Norman AR, Cunningham D,
Oates J, Dix BR, Iacopetta BJ, Young Y, Walsh T, Ward R, Hawkins N,
Beranek M, Jandik P, Benamouzig R, Jullian E, Laurent-Puig P,
Olschwang S, Muller O, Hoffmann I, Rabes HM, Zietz C, Troungos C,
Valavanis C, Yuen ST, Ho JWC, Croke CT, O’Donoghue DP, Giaretti W,
Rapallo A, Russo A, Bazan V, et al: Kirsten ras mutations in
patients with colorectal cancer: the ‘RASCAL II’ study. Br J
Cancer. 85:692–696. 2001.
|
|
33.
|
Normanno N, Tejpar S, Morbillo F, De Luca
A, Van Cutsem E and Ciardiello F: Implication of KRAS status and
EGFR-targeted therapies in metastatic CRC. Nat Rev Clin Oncol.
6:519–527. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
De Roock W, Claes B, Bernasconi D, De
Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V,
Papamichael D, Laurent-Puig P, Penault-Llorca F, Rougier P,
Vincenzi B, Santini D, Tonini G, Cappuzzo F, Frattini M, Molinari
F, Saletti P, De Dosso S, Martini M, Bardelli A, Siena S,
Sartore-Bianchi A, Tabernero J, Macarulla T, Di Fiore F, Gangloff
AO, Ciardiello F, Pfeiffer P, et al: Effects of KRAS, BRAF, NRAS,
and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy
in chemotherapy-refractory metastatic colorectal cancer: a
retrospective consortium analysis. Lancet Oncol. 11:753–762.
2010.PubMed/NCBI
|
|
35.
|
Guerrero S, Casanova I, Farrè L, Mazo A,
Capellà G and Mangues R: K-ras codon 12 mutation induces higher
level of resistance to apoptosis and predisposition to
anchorage-independent growth than codon 13 mutation or
proto-oncogene overexpression. Cancer Res. 60:6750–6756. 2000.
|
|
36.
|
Ince WL, Jubb AM, Holden SN, Holmgren EB,
Tobin P, Sridhar M, Hurwitz HI, Kabbinavar F, Novotny WF, Hillan KJ
and Koeppen H: Association of K-ras, B-raf, and p53 status with the
treatment effect of bevacizumab. J Natl Cancer Inst. 97:981–989.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Hurwitz HI, Yi J, Ince W, Novotny WF and
Rosen O: The clinical benefit of bevacizumab in metastatic
colorectal cancer is independent of K-ras mutation status: analysis
of a phase III study of bevacizumab with chemotherapy in previously
untreated metastatic colorectal cancer. Oncologist. 14:22–28. 2009.
View Article : Google Scholar
|
|
38.
|
Van Cutsem E, Köhne CH, Làng I, Folprecht
G, Nowacki MP, Cascinu S, Shchepotin I, Maurel J, Cunningham D,
Tejpar S, Schlichting M, Zubel A, Celik I, Rougier P and Ciardiello
F: Cetuximab plus irinotecan, fluorouracil, and leucovorin as
first-line treatment for metastatic colorectal cancer: updated
analysis of overall survival according to tumor KRAS and BRAF
mutation status. J Clin Oncol. 29:2011–2019. 2011.
|
|
39.
|
Bokemeyer C, Bondarenko I, Hartmann JT, de
Braud F, Schuch G, Zubel A, Celik I, Schlichting M and Koralewski
P: Efficacy according to biomarker status of cetuximab plus
FOLFOX-4 as first-line treatment for metastatic colorectal cancer:
the OPUS study. Ann Oncol. 22:1535–1546. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Bruera G, Cannita K, Di Giacomo D, Lamy A,
Frébourg T, Sabourin JC, Tosi M, Alesse E, Ficorella C and Ricevuto
E: Worse prognosis of KRAS c.35 G>A mutant metastatic colorectal
cancer (MCRC) patients treated with intensive triplet chemotherapy
plus bevacizumab (FIr-B/FOx). BMC Med. 11:592013.
|
|
41.
|
Morelli MF, Santomaggio A, Ricevuto E,
Cannita K, De Galitiis F, Tudini M, Bruera G, Mancini M,
Pelliccione M, Calista F, Guglielmi F, Martella F, Lanfiuti Baldi
P, Porzio G, Russo A, Gebbia N, Iacobelli S, Marchetti P and
Ficorella C; on behalf of CINBO (Consorzio Interuniversitario
Nazionale per la Bio-Oncologia): Triplet schedule of weekly
5-fluorouracil and alternating irinotecan or oxaliplatin in
advanced colorectal cancer: a dose-finding and phase II study.
Oncol Rep. 23:1635–1640. 2010.PubMed/NCBI
|
|
42.
|
Ficorella C, Ricevuto E, Morelli MF,
Morese R, Cannita K, Cianci G, Di Rocco ZC, De Galitiis F, De Tursi
M, Tinari N, Iacobelli S and Marchetti P: Increased tolerability of
bimonthly 12-hour timed flat infusion 5-fluorouracil/irinotecan
regimen in advanced colorectal cancer: a dose-finding study. Oncol
Rep. 15:1345–1350. 2006.
|
|
43.
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, Verweij J, Glabbeke MV, van
Oosterom AT, Christian MC and Gwyther SG: New guidelines to
evaluate the response to treatment in solid tumors: European
Organization for Research and Treatment of Cancer, National Cancer
Institute of the United States, National Cancer Institute of
Canada. J Natl Cancer Inst. 92:205–216. 2000. View Article : Google Scholar
|
|
44.
|
Kaplan EL and Meier P: Nonparametric
estimation of incomplete observations. J Am Statist Assoc.
53:457–481. 1958. View Article : Google Scholar
|
|
45.
|
Peto R and Peto J: Asymptomatically
efficient rank invariant test procedures. J R Stat Soc A.
135:185–207. 1972. View Article : Google Scholar
|
|
46.
|
Tebbutt NC, Wilson K, Gebski VJ, Cummins
MM, Zannino D, van Hazel GA, Robinson B, Broad A, Ganju V, Ackland
SP, Forgeson G, Cunningham D, Saunders MP, Stockler MR, Chua Y,
Zalcberg JR, Simes RJ and Price TJ: Capecitabine, bevacizumab, and
mitomycin in first-line treatment of metastatic colorectal cancer:
results of the Australasian Gastrointestinal Trials Group
randomized phase III MAX study. J Clin Oncol. 28:3191–3198. 2010.
View Article : Google Scholar
|
|
47.
|
Bruera G, Cannita K, Giordano AV,
Vicentini R, Ficorella C and Ricevuto E: Effectiveness and safety
of intensive triplet chemotherapy plus bevacizumab, FIr-B/FOx, in
young-elderly Metastatic Colorectal Cancer (MCRC) patients. BioMed
Res Int. 2013:1432732013. View Article : Google Scholar
|
|
48.
|
Figueras J, Ramos E, López-Ben S, Torras
J, Albiol M, Llado L, González HD and Rafecas A: Surgical treatment
of liver metastases from colorectal carcinoma in elderly patients.
When is it worthwhile? Clin Transl Oncol. 9:392–400. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
49.
|
Diaz-Rubio E, Gomez-Espana A, Massuti B,
Sastre J, Reboredo M, Manzano JL, Rivera F, Safont Mj, Montagut C,
lez EG, Benavides M, Marcuello E, Cervantes A, de Prado PM,
Fernandez-Martos C, Arrivi A, Bando I and Aranda E; on behalf of
the Spanish Cooperative Group for the Treatment of Digestive Tumors
(TTD): Role of Kras status in patients with metastatic colorectal
cancer receiving first-line chemotherapy plus bevacizumab: a TTD
group cooperative study. PLoS One. 7:e473452012. View Article : Google Scholar : PubMed/NCBI
|