|
1
|
Clézardin P, Coleman R, Puppo M, Ottewell
P, Bonnelye E, Paycha F, Confavreux CB and Holen I: Bone
metastasis: Mechanisms, therapies, and biomarkers. Physiol Rev.
101:797–855. 2021. View Article : Google Scholar
|
|
2
|
Falk S and Dickenson AH: Pain and
nociception: Mechanisms of cancer-induced bone pain. J Clin Oncol.
32:1647–1654. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Qiao RQ, Zhang HR, Ma RX, Li RF and Hu YC:
Prognostic factors for bone survival and functional outcomes in
patients with breast cancer spine metastases. Technol Cancer Res
Treat. 21:153303382211226422022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hu W, Zhang L, Dong Y, Tian Z, Chen Y and
Dong S: Tumour dormancy in inflammatory microenvironment: A
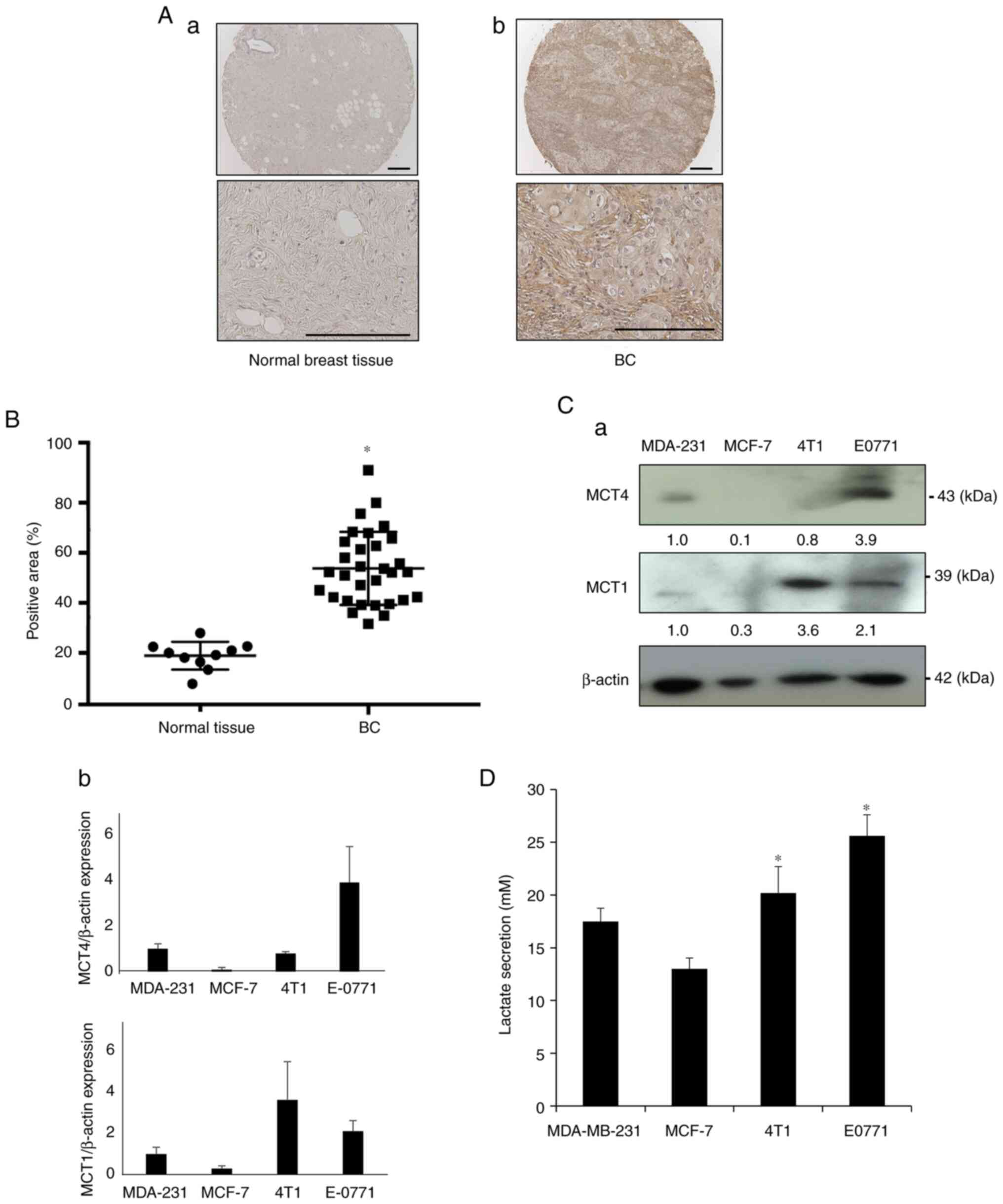
promising therapeutic strategy for cancer-related bone metastasis.
Cell Mol Life Sci. 77:5149–5169. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Infante M, Fabi A, Cognetti F, Gorini S,
Caprio M and Fabbri A: RANKL/RANK/OPG system beyond bone
remodeling: Involvement in breast cancer and clinical perspectives.
J Exp Clin Cancer Res. 38:122019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ngo DC, Ververis K, Tortorella SM and
Karagiannis TC: Introduction to the molecular basis of cancer
metabolism and the Warburg effect. Mol Biol Rep. 42:819–823. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tiedemann K, Hussein O and Komarova SV:
Role of altered metabolic microenvironment in osteolytic
metastasis. Front Cell Dev Biol. 8:4352020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Avnet S, Di Pompo G, Lemma S and Baldini
N: Cause and effect of microenvironmental acidosis on bone
metastases. Cancer Metastasis Rev. 38:133–147. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hiasa M, Okui T, Allette YM, Ripsch MS,
Sun-Wada GH, Wakabayashi H, Roodman GD, White FA and Yoneda T: Bone
pain induced by multiple myeloma is reduced by targeting V-ATPase
and ASIC3. Cancer Res. 77:1283–1295. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yoneda T, Hiasa M, Nagata Y, Okui T and
White FA: Acidic microenvironment and bone pain in cancer-colonized
bone. Bonekey Rep. 4:6902015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brooks GA: The science and translation of
lactate shuttle theory. Cell Metab. 27:757–785. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Magistretti PJ and Allaman I: Lactate in
the brain: From metabolic end-product to signalling molecule. Nat
Rev Neurosci. 19:235–249. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Payen VL, Mina E, Van Hée VF, Porporato PE
and Sonveaux P: Monocarboxylate transporters in cancer. Mol Metab.
33:48–66. 2020. View Article : Google Scholar :
|
|
14
|
Cai TQ, Ren N, Jin L, Cheng K, Kash S,
Chen R, Wright SD, Taggart AK and Waters MG: Role of GPR81 in
lactate-mediated reduction of adipose lipolysis. Biochem Biophys
Res Commun. 377:987–991. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
de Castro Abrantes H, Briquet M,
Schmuziger C, Restivo L, Puyal J, Rosenberg N, Rocher AB,
Offermanns S and Chatton JY: The Lactate Receptor HCAR1 Modulates
neuronal network activity through the activation of Gα
and Gβγ Subunits. J Neurosci. 39:4422–4433. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Francel PC, Harris K, Smith M, Fishman MC,
Dawson G and Miller RJ: Neurochemical characteristics of a novel
dorsal root ganglion X neuroblastoma hybrid cell line, F-11. J
Neurochem. 48:1624–1631. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakanishi M, Hata K, Nagayama T, Sakurai
T, Nishisho T, Wakabayashi H, Hiraga T, Ebisu S and Yoneda T: Acid
activation of Trpv1 leads to an up-regulation of calcitonin
gene-related peptide expression in dorsal root ganglion neurons via
the CaMK-CREB cascade: A potential mechanism of inflammatory pain.
Mol Biol Cell. 21:2568–2577. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Okui T, Shimo T, Fukazawa T, Kurio N,
Hassan NM, Honami T, Takaoka M, Naomoto Y and Sasaki A: Antitumor
effect of temsirolimus against oral squamous cell carcinoma
associated with bone destruction. Mol Cancer Ther. 9:2960–2969.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Okui T, Hiasa M, Ryumon S, Ono K, Kunisada
Y, Ibaragi S, Sasaki A, Roodman GD, White FA and Yoneda T: The
HMGB1/RAGE axis induces bone pain associated with colonization of
4T1 mouse breast cancer in bone. J Bone Oncol. 26:1003302021.
View Article : Google Scholar
|
|
20
|
Russell FA, King R, Smillie SJ, Kodji X
and Brain SD: Calcitonin gene-related peptide: Physiology and
pathophysiology. Physiol Rev. 94:1099–1142. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hiraga T, Myoui A, Hashimoto N, Sasaki A,
Hata K, Morita Y, Yoshikawa H, Rosen CJ, Mundy GR and Yoneda T:
Bone-derived IGF mediates crosstalk between bone and breast cancer
cells in bony metastases. Cancer Res. 72:4238–4249. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kawasaki Y, Kohno T, Zhuang ZY, Brenner
GJ, Wang H, Van Der Meer C, Befort K, Woolf CJ and Ji RR:
Ionotropic and metabotropic receptors, protein kinase A, protein
kinase C, and Src contribute to C-fiber-induced ERK activation and
cAMP response element-binding protein phosphorylation in dorsal
horn neurons, leading to central sensitization. J Neurosci.
24:8310–8321. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Leffler A, Mönter B and Koltzenburg M: The
role of the capsaicin receptor TRPV1 and acid-sensing ion channels
(ASICS) in proton sensitivity of subpopulations of primary
nociceptive neurons in rats and mice. Neuroscience. 139:699–709.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ouyang K, Zheng H, Qin X, Zhang C, Yang D,
Wang X, Wu C, Zhou Z and Cheng H: Ca2+ sparks and secretion in
dorsal root ganglion neurons. Proc Natl Acad Sci USA.
102:12259–12264. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pastori V, D'Aloia A, Blasa S and Lecchi
M: Serum-deprived differentiated neuroblastoma F-11 cells express
functional dorsal root ganglion neuron properties. PeerJ.
7:e79512019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lauritzen KH, Morland C, Puchades M,
Holm-Hansen S, Hagelin EM, Lauritzen F, Attramadal H,
Storm-Mathisen J, Gjedde A and Bergersen LH: Lactate receptor sites
link neurotransmission, neurovascular coupling, and brain energy
metabolism. Cereb Cortex. 24:2784–2795. 2014. View Article : Google Scholar
|
|
27
|
Liu C, Kuei C, Zhu J, Yu J, Zhang L, Shih
A, Mirzadegan T, Shelton J, Sutton S, Connelly MA, et al:
3,5-Dihydroxybenzoic acid, a specific agonist for hydroxycarboxylic
acid 1, inhibits lipolysis in adipocytes. J Pharmacol Exp Ther.
341:794–801. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hasegawa K, Okui T, Shimo T, Ibaragi S,
Kawai H, Ryumon S, Kishimoto K, Okusha Y, Monsur Hassan NM and
Sasaki A: Lactate transporter monocarboxylate transporter 4 induces
bone pain in head and neck squamous cell carcinoma. Int J Mol Sci.
19:33172018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Doherty JR and Cleveland JL: Targeting
lactate metabolism for cancer therapeutics. J Clin Invest.
123:3685–3692. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Liang L, Li W, Li X, Jin X, Liao Q, Li Y
and Zhou Y: 'Reverse Warburg effect' of cancer-associated
fibroblasts (Review). Int J Oncol. 60:672022. View Article : Google Scholar
|
|
31
|
Corbet C and Feron O: Tumour acidosis:
From the passenger to the driver's seat. Nat Rev Cancer.
17:577–593. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Doyen J, Trastour C, Ettore F, Peyrottes
I, Toussant N, Gal J, Ilc K, Roux D, Parks SK, Ferrero JM and
Pouysségur J: Expression of the hypoxia-inducible monocarboxylate
transporter MCT4 is increased in triple negative breast cancer and
correlates independently with clinical outcome. Biochem Biophys Res
Commun. 451:54–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hong CS, Graham NA, Gu W, Espindola
Camacho C, Mah V, Maresh EL, Alavi M, Bagryanova L, Krotee PAL,
Gardner BK, et al: MCT1 modulates cancer cell pyruvate export and
growth of tumors that Co-express MCT1 and MCT4. Cell Rep.
14:1590–1601. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Órdenes P, Villar PS, Tarifeño-Saldivia E,
Salgado M, Elizondo-Vega R, Araneda RC and García-Robles MA:
Lactate activates hypothalamic POMC neurons by intercellular
signaling. Sci Rep. 11:216442021. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Roland CL, Arumugam T, Deng D, Liu SH,
Philip B, Gomez S, Burns WR, Ramachandran V, Wang H,
Cruz-Monserrate Z and Logsdon CD: Cell surface lactate receptor
GPR81 is crucial for cancer cell survival. Cancer Res.
74:5301–5310. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ishihara S, Hata K, Hirose K, Okui T,
Toyosawa S, Uzawa N, Nishimura R and Yoneda T: The lactate sensor
GPR81 regulates glycolysis and tumor growth of breast cancer. Sci
Rep. 12:62612022. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Venkatesh HS: The neural regulation of
cancer. Science. 366:9652019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zahalka AH and Frenette PS: Nerves in
cancer. Nat Rev Cancer. 20:143–157. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Silverman DA, Martinez VK, Dougherty PM,
Myers JN, Calin GA and Amit M: Cancer-associated neurogenesis and
nerve-cancer cross-talk. Cancer Res. 81:1431–1440. 2021. View Article : Google Scholar
|
|
40
|
Brown TP, Bhattacharjee P, Ramachandran S,
Sivaprakasam S, Ristic B, Sikder MOF and Ganapathy V: The lactate
receptor GPR81 promotes breast cancer growth via a paracrine
mechanism involving antigen-presenting cells in the tumor
microenvironment. Oncogene. 39:3292–3304. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|