Nasopharyngeal carcinoma (NPC) is an epithelial
tumor of the head and neck with a well-defined geographical
distribution (1). According to
global cancer statistics from 2020, >75% of NPC cases are
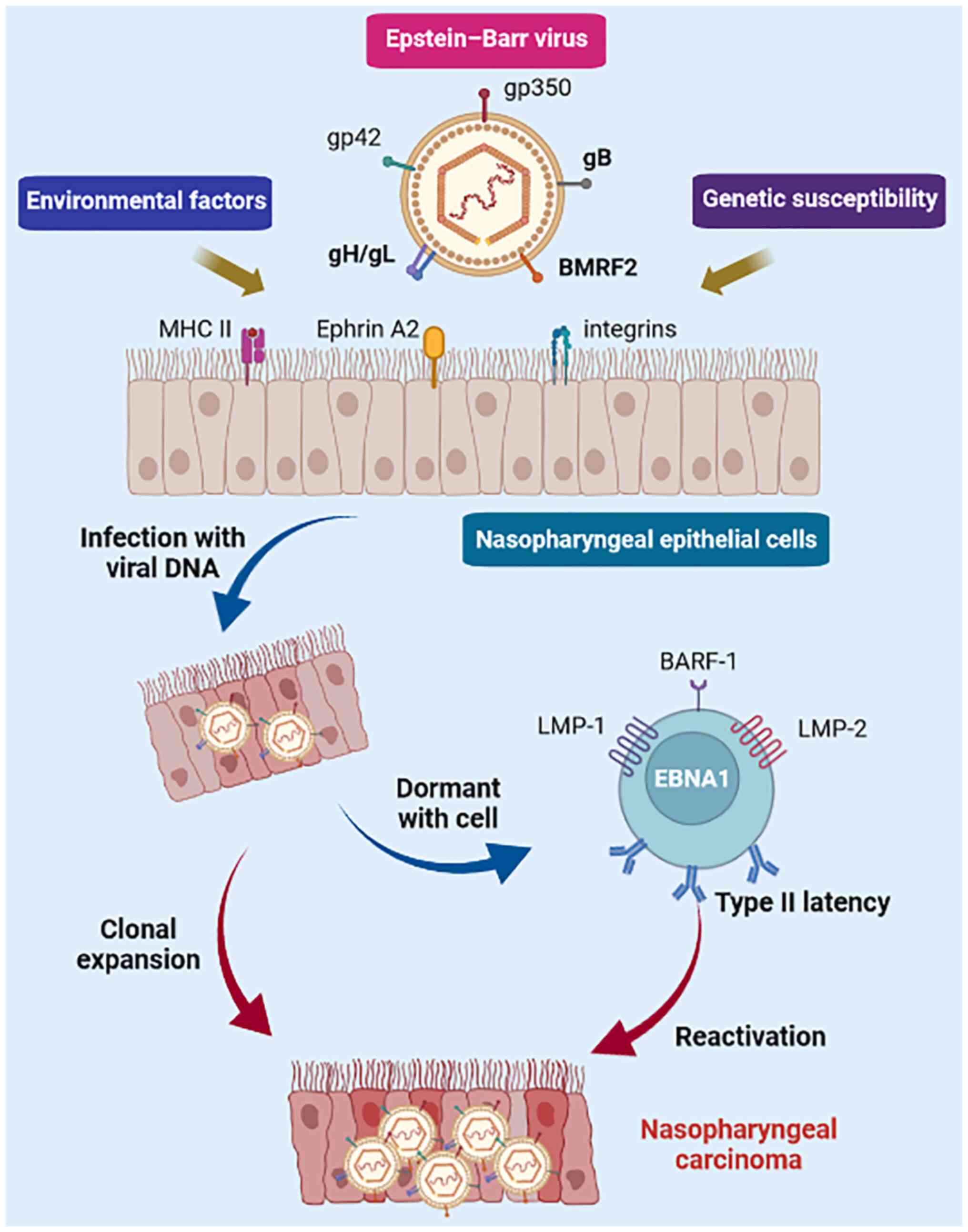
diagnosed in Southeast Asia and Southern China (2). NPC is thought to be mediated by the
interaction of Epstein-Barr virus (EBV) infection, environmental
factors (diet and smoking) and genetic susceptibility [high-risk
human leukocyte antigen (HLA) allotypes] (Fig. 1) (3). The non-keratinizing subtype accounts
for >95% of NPCs in endemic areas, while it accounts for 75% in
the United States (4). This unique
geographic distribution is etiologically attributable to genetic
and environmental factors (5-8). In
addition, EBV infection is ubiquitous in non-keratinizing NPC and
has an important pathogenic role (9). Furthermore, the interaction of unique
genetic factors and EBV variants may lead to an increased risk of
persistent infection and clonal expansion of EBV-infected
epithelial cells, ultimately culminating in an invasive phenotype
promoting NPC progression (10,11).
Of note, improvements in diagnostic imaging technology, the
widespread use of intensity-modulated radiotherapy (IMRT) and the
optimization of chemotherapy regimens have significantly improved
the survival of patients with NPC (12-14).
Approximately 90% of patients with early-stage disease can be cured
by IMRT alone (15). However, due
to the hidden anatomical location of the nasopharynx and atypical
early symptoms, >70% of patients with NPC are at stage III or IV
at the time of initial diagnosis (16). Approximately 20-30% of patients
with advanced NPC still fail treatment, mainly because of
recurrence and/or metastasis (R/M) (17).
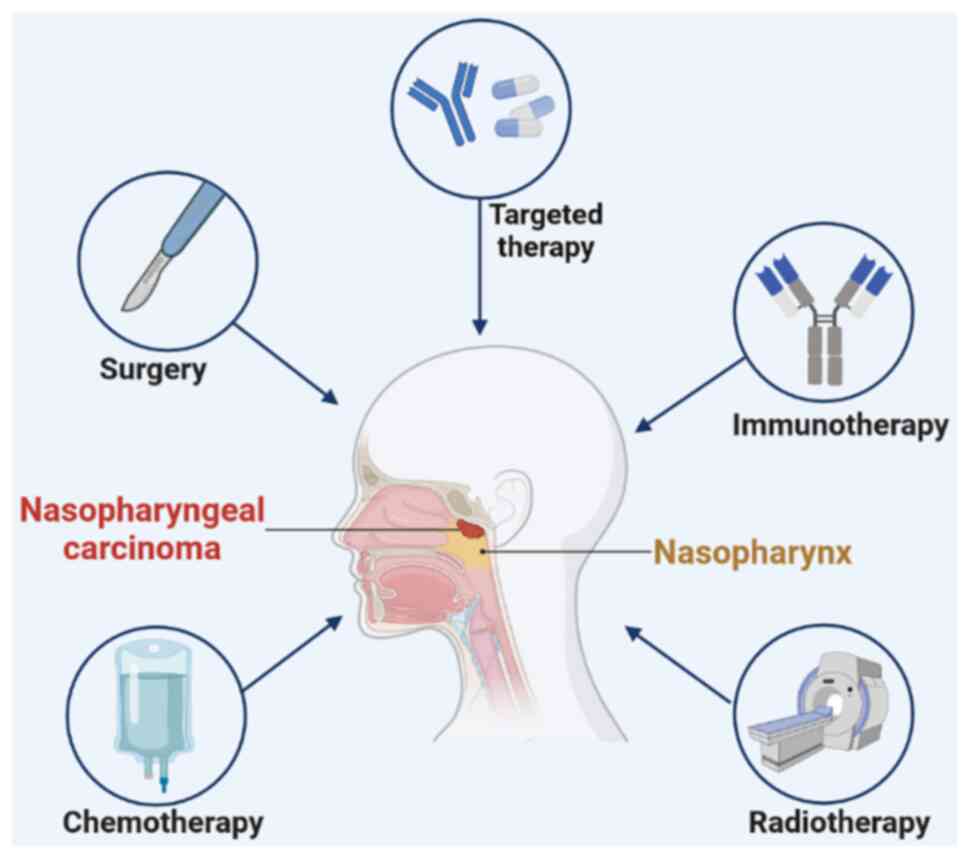
Conventional salvage treatments for R/M NPC include
radiotherapy, chemotherapy and surgery (Fig. 2), but none are satisfactory.
Current NCCN Head and Neck Cancer Clinical Practice
Guidelines® (https://www.nccn.org/) recommend gemcitabine plus
cisplatin (GP) (Category 1 recommendation) as the preferred
first-line systemic treatment for R/M NPC. However, the prognosis
of these patients remains suboptimal, with a median overall
survival (OS) of ~20-30 months (18,19).
Furthermore, the outcome of patients with advanced recurrent
disease who undergo salvage IMRT is poor, with a 5-year survival
rate of ~30%, and radiation-induced injuries are also serious, with
46-70% of all deaths being due to severe radiotherapy sequelae
(20,21). Therefore, R/M has become a
challenge and research priority in the clinical management of NPC.
Novel treatment strategies are desperately needed to improve the
prognosis of patients with advanced NPC.
In recent years, immunotherapy has sparked a
revolution in the clinical management of cancer. Immunotherapy
activates the immune response in the tumor microenvironment by
altering the biological properties of immune effector cells,
thereby inhibiting or killing cancer cells (22). At present, immunotherapy has
emerged as a promising treatment modality for R/M NPC. An
increasing number of clinical studies have investigated the safety
and efficacy of immunotherapy for advanced NPC and have shown
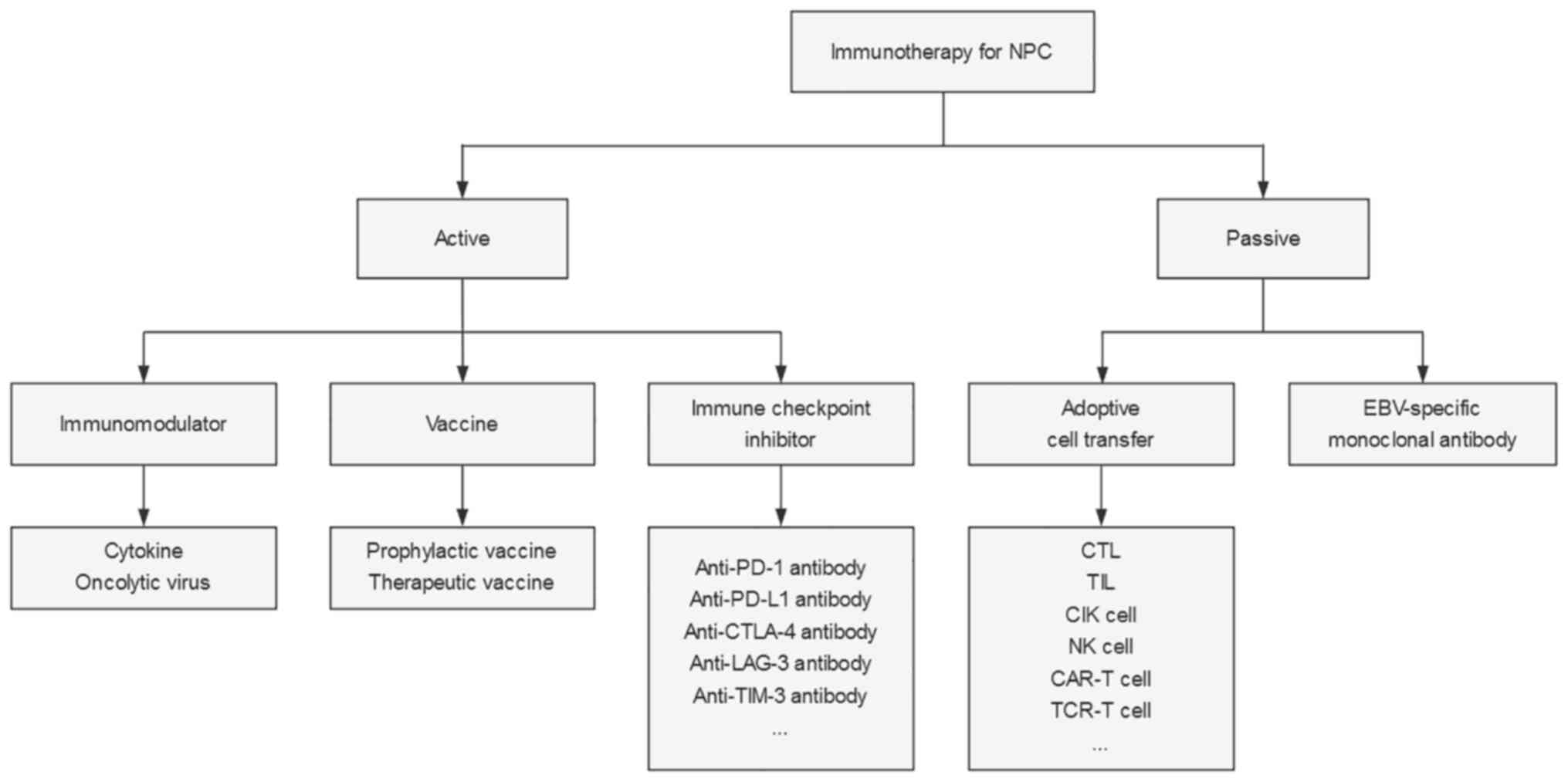
considerable progress. In general, immunotherapy for NPC may be
divided into two major approaches: i) Active immunotherapy, which
relies on the ability of the patient's immune system to mount a
specific immune response to tumor-associated antigens and includes
immune checkpoint inhibitors (ICIs), vaccines and immunomodulators;
and ii) passive immunotherapy, which uses exogenous lymphocytes or
antibodies to mediate immune responses and immune stimulation, such
as adoptive cell transfer (ACT) and EBV-specific monoclonal
antibodies (Fig. 3). In the
present article, the available clinical evidence on different
immunotherapeutic approaches for NPC was reviewed and summarized to
provide insight for future investigation.
Studies have indicated that NPC is primarily
suitable for immunotherapy due to the following reasons: The
expression of EBV antigens and CD4+/CD8+
T-cell target proteins (23,24),
massive lymphocytic infiltration (25), programmed death ligand-1 (PD-L1)
expression of up to 89-95% (26)
and the presence of several key immune molecules (CD40, CD70, CD80
and CD86) that regulate T-cell activation (27). In China, >95% of NPCs are
undifferentiated nonkeratinizing carcinomas and are widely
considered to be associated with EBV infection (12). EBV exists in a type II latency
state and has an important role in inducing NPC development
(Fig. 1) (1). EBV-infected nasopharyngeal epithelial
cells usually express EBV antigens, including Epstein-Barr nuclear
antigen 1 (EBNA1), latent membrane protein 1/2 (LMP1/2) and BamH1-A
right frame 1 (BARF1) (28). EBNA1
induces the transformation of nasopharyngeal epithelial cells into
NPC cells and is associated with invasion and metastasis of NPC
(29). EBNA1 is a major target of
CD4+ T cells (30).
LMP1 promotes cancer cell growth during NPC development and
promotes NPC cells to interact with surrounding stromal cells and
induce invasion, angiogenesis and immune regulation (31). LMP1 is detected in 100% of
preinvasive NPC and ~50% of advanced diseases (32). LMP2 contains substantial
CD8+ T-cell epitopes and is therefore considered to be a
major target for CD8+ T cells (33).
NPC is characterized by numerous immune infiltrates
in the primary tumor, including T cells, B cells, dendritic cells
(DCs), monocytes and eosinophils (34). However, due to the
immunosuppressive tumor microenvironment, NPC cells can continue to
proliferate (35). Data from
whole-exome sequencing and single-cell sequencing studies have
gradually revealed the immune profile of NPC (36,37).
The immunosuppressive tumor microenvironment in NPC is infiltrated
by dysfunctional and depleted CD8+ T cells and effector
T cells that overexpress suppressive immune checkpoint signaling
molecules, such as programmed cell death protein-1 (PD-1) or its
ligand PD-L1, as well as various chemokines and cytokines. The
depletion and weakness of immune cells allow NPC cells to evade
immune clearance by the host.
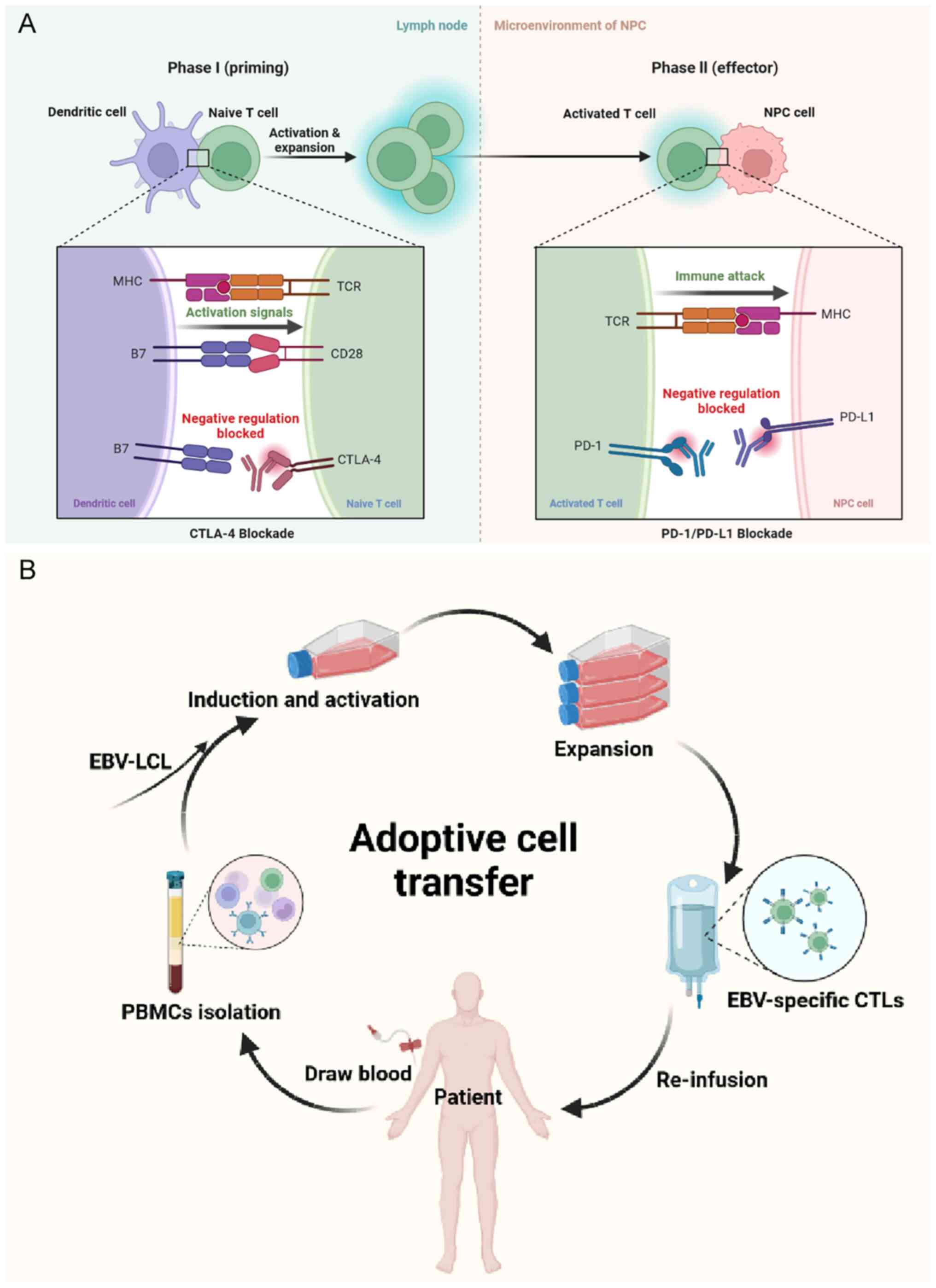
Based on current clinical research evidence, the
most promising approach to activate therapeutic antitumor immunity
in NPC is ICIs. Immune checkpoints refer to a plethora of
inhibitory pathways in the immune system. They are essential for
maintaining self-tolerance and regulating the duration and
magnitude of physiological immune responses in peripheral tissues
(38). However, cancer cells
frequently evade immunity by suppressing immune responses through
immune checkpoints. In NPC, immune checkpoints that have been
extensively studied include PD-1/PD-L1 and cytotoxic T-lymphocyte
(CTL)-associated antigen-4 (CTLA-4). ICIs acting on these targets
can effectively inhibit the binding of immunosuppressive signals to
the corresponding ligands, thereby blocking the transduction of
immunosuppressive signals, weakening the negative immune regulation
in the tumor microenvironment, relieving the suppressive state of T
cells and preventing immune escape (Fig. 4A).
PD-1, a member of the CD28 superfamily, is an
inhibitory receptor expressed on the surface of antigen-activated T
cells. PD-1 has a vital role in limiting normal host adaptive
immunity and preventing autoimmune and autoinflammatory responses
(39,40). PD-L1 is generally expressed on the
surface of antigen-presenting cells and cancer cells (41). The PD-1/PD-L1 interactions have a
leading role in the inhibition of T-cell responses in vivo,
particularly in the tumor microenvironment (38,41-43).
The results of published clinical trials of PD-1/PD-L1 inhibitors
for R/M NPC are summarized in Table
I.
A phase II clinical study (CAPTAIN study) was
conducted to investigate the antitumor activity and predictive
biomarkers of camrelizumab (SHR-1210) in NPC (46). A total of 156 patients with R/M NPC
who had failed at least two lines of chemotherapy were enrolled.
The ORR was 28.2%. The median duration of response (DoR) was not
reached. The median PFS and OS were 3.7 and 17.4 months,
respectively. Grade ≥3 TRAEs were reported in 24 patients (15.4%).
The combination of both major histocompatibility complex
(MHC)-II-positive cell density and PD-L1 expression may allow for
better patient selection.
The above studies suggest that anti-PD-1/PD-L1
antibody monotherapy has clinically meaningful antitumor activity
as a third- or later-line treatment in patients with R/M NPC.
Similar studies are being conducted using bintrafusp alfa [a
bifunctional fusion protein targeting transforming growth factor-β
(TGF-β) and PD-L1] (NCT04396886) and penpulimab (AK105, anti-PD-1
antibody) (NCT03866967).
An open-label, non-comparative, phase I/II study was
designed to examine the safety, tolerability and antitumor activity
of tislelizumab in adult Chinese patients with advanced solid
tumors (49). The ORR of the 21
patients with NPC was 42.9%, with a median DoR of 8.3 months and a
median follow-up of 4.8 months. The median PFS was 10.4 months and
the median OS had not been reached. Response to tislelizumab was
seen in multiple tumor types, including NPC, regardless of PD-L1
expression.
A phase II randomized study was conducted to assess
the PFS of spartalizumab (PDR001, an anti-PD-1 antibody) vs.
chemotherapy in 122 patients with nonkeratinizing R/M NPC who
progressed on/after platinum-based chemotherapy (51). Eligible patients were randomly
allocated to the spartalizumab or chemotherapy arm at a 2:1 ratio.
Fewer grade 3/4 TRAEs occurred in the spartalizumab group than in
the chemotherapy arm (16.8 vs. 41.0%). However, spartalizumab did
not improve PFS or OS compared to chemotherapy (median PFS, 1.9 vs.
6.6 months, P=0.915; median OS, 25.2 vs. 15.5 months, P=0.138). The
ORRs were 17.1 and 35.0% in the spartalizumab and chemotherapy
groups, respectively. The median DoR was longer in the
spartalizumab group than in the chemotherapy group (10.2 vs. 5.
months), suggesting an initial durable antitumor effect of
spartalizumab in NPC. However, these results were not conclusive,
as the study was not sufficiently powered to assess the
significance of these endpoints.
The above-mentioned studies suggest that GP plus
anti-PD-1 antibody may be a promising standard of care for patients
with R/M NPC in the first-line setting. Similar studies are being
conducted using nivolumab (NCT04458909) and tislelizumab (anti-PD-1
antibody) (NCT03924986).
Clinical trials on the addition of anti-PD-1/PD-L1
antibodies to chemoradiotherapy are being conducted in different
settings of LANPC at initial diagnosis. Four phase III trials are
evaluating camrelizumab, sintilimab or toripalimab in combination
with induction chemotherapy, concurrent chemoradiotherapy (CCRT),
or as maintenance after radical treatment (NCT03427827,
NCT04453826, NCT03700476 and NCT04557020, respectively). The
results of these different clinical trials may identify an optimal
multidisciplinary management approach in the era of immunotherapy
for NPC. Breakthroughs in the field of LANPC by ICIs are to be
expected.
CTLA-4 is a secondary receptor of B7 (CD80 and CD86)
and is homologous to the CD28 receptor. However, CTLA-4 transmits
different costimulatory signals from CD28. During T-cell
activation, the most important function of CTLA-4 is to compete
with CD28 for binding to CD80/CD86 molecules on the surface of
antigen-presenting cells, thereby negatively regulating T-cell
activation signals (57,58). Cancer cells can activate CTLA-4 to
inactivate activated T cells, allowing immune escape (59).
To date, two CTLA-4 inhibitors, ipilimumab and
tremelimumab, have been approved by the FDA for the treatment of
advanced melanoma and hepatocellular carcinoma (60-62).
However, reports on the application of anti-CTLA-4 anti-bodies in
NPC are scarce. A case-control study showed that CTLA-4
polymorphism was associated with susceptibility to NPC (63). Ahmed et al (64) found that high CTLA-4 expression was
significantly associated with disease progression and worsening OS.
A phase II trial (NCT03097939) to test the hypothesis that
ipilimumab in combination with nivolumab is effective in advanced
NPC is ongoing. Furthermore, four phase I/II clinical trials are
exploring the safety, tolerability and anti-tumor activity of AK104
(PD-1/CTLA-4 bispecific antibody), cadonilimab (PD-1/CTLA-4
bispecific antibody), IBI310 (CTLA-4 antibody) and XmAb20717
(PD-1/CTLA-4 bispecific antibody) in R/M NPC (NCT04220307,
NCT05587374, NCT04945421 and NCT03517488).
Lymphocyte activation gene-3 (LAG-3) and PD-1 are
distinct suppressive immune checkpoints that are often coexpressed
on TILs, thereby promoting tumor-mediated T-cell exhaustion and
immune escape (65-67). Opdualag is the first FDA-approved
antibody against LAG-3 (68),
making LAG-3 the third clinical immune checkpoint after PD-1 and
CTLA-4. Only one registered clinical trial of anti-LAG-3 antibody
is evaluating the safety and tolerability of XmAb22841
(LAG-3/CTLA-4 bispecific antibody) plus pembrolizumab in patients
with advanced solid tumors, including NPC (NCT03849469).
Another major regulatory checkpoint is T-cell
immunoglobulin- and mucin-domain-containing molecule-3 (TIM-3)
(69,70). Tim-3 is a coinhibitory receptor
whose expression is increased when patients develop adaptive
resistance to anti-PD-1 antibodies (71). Inhibition of its ligand,
galectin-9, selectively rejuvenates TILs by interfering with the
interaction between PD-1 and TIM-3 (72). As galectin-9 is specifically
expressed in NPC cells (73),
TIM-3/galectin-9 interaction is a promising approach to overcome
resistance to PD-1/PD-L1 inhibitors. Currently, only one registered
clinical trial is investigating the role of anti-TIM-3 antibodies
in NPC, a phase II trial evaluating the efficacy and safety of
TQB2618 (anti-TIM-3 antibody) in combination with penpulimab in
patients with R/M NPC (NCT05563480).
In general, the ongoing exploration of ICIs has
focused on investigating the long-term effects of these agents on
the toxicity of chemotherapy and/or radiotherapy, the optimal
sequence of chemotherapy and/or radiotherapy, the optimal duration
of treatment, the role of predictive biomarkers in selecting
subgroups of patients more likely to benefit from treatment, and
the cost-effectiveness of these ICIs in routine practice (1). It is reasonable to assume that
combining different ICIs may be a more effective treatment option
for patients with R/M NPC (74).
Cancer vaccines are active immunotherapies that use
cancer cells or tumor antigenic substances to activate the immune
system and induce a specific immune response. Currently, NPC
vaccines are mainly divided into prophylactic vaccines and
therapeutic vaccines.
Five membrane proteins (gp350, gH, gL, gB and gp42)
are needed to infect B cells with EBV, whereas four membrane
proteins (BMFR2, gH, gL and gB) are needed to infect epithelial
cells with EBV (Fig. 1). These
proteins are expressed in EBV and may be good targets for
EBV-preventive vaccines (75-77).
Cui et al (78-80) indicated that serum EBV-neutralizing
titers were higher in rabbits inoculated with trimeric and
monomeric EBV gH/gL, trimeric gB and tetrameric gp350(1-470) than
in those inoculated with monomeric gp350 (1-470). EBV gH/gL and gB
may be better targets for EBV-preventive vaccines than gp350 alone
and the combination of gp350 with gH/gL and gB may yield a more
potent EBV-preventive vaccine. These data strongly suggest that the
combination of the EBV core fusion mechanism envelope protein gH/gL
and trimeric gB is a promising EBV prophylactic vaccine.
In general, despite the progress with EBV vaccines,
DC-based vaccines have few targets and are costly to prepare, while
recombinant viral vectors, although having a broad range of
epitopes, may yield reduced immune function after repeated
immunization. Of note, different routes of administration should be
systematically examined to facilitate EBV vaccination. Future EBV
vaccines containing gp350, gH/gL, gB EBNA1 and LMP1/2 are expected
to be the direction of EBV vaccine research.
Immunomodulators are nonspecific and include mainly
cytokines and oncolytic viruses. Cytokine therapy may alter the
concentration of cytokines in the immune microenvironment and
enhance the antitumor immune response. A study evaluated the
multifunctional antitumor effects of the cytokine recombinant
interferon-α1b (IFN-α1b) (86).
Results from in vitro and in vivo experiments showed
that IFN-α1b inhibited cell growth, promoted apoptosis and
necrosis, suppressed tumor growth and metastasis, reduced
intratumor microvascular density and prolonged survival. Oncolytic
viruses are a class of viruses that replicate in cancer cells
through different regulatory mechanisms and lyse cancer cells
without affecting normal cell proliferation. T-VEC, the first
oncolytic viral treatment approved by the US FDA, was shown to be
effective in advanced melanoma (87). Liu et al (88) found that an oncolytic adenovirus
enhanced antiangiogenic and antitumor effects by rescuing the
selective replication of replication-deficient adenovirus encoding
endothelial repressor in NPC cells. A third-generation oncolytic
virus, G47Δ (HSV-1), demonstrated a reliable antitumor effect in
NPC in vitro and in vivo (89). With the development of genetic
engineering technology and virology, oncolytic viruses are expected
to become an important tool for comprehensive tumor therapy.
As viral proteins are almost exclusively expressed
in cancer cells, ACT that targets EBV antigens holds therapeutic
promise in the treatment of NPC. ACT is a passive immunotherapy
that mainly adopts CTLs, TILs, cytokine-induced killer (CIK) cells
and natural killer (NK) cells. The corresponding active immune
cells are isolated from patients, screened and expanded in
vitro to induce highly specific antitumor immune cells, which
are then injected back into the patient to kill cancer cells
(Fig. 4B). Genetically modified
cellular immunotherapy is also a form of ACT and includes chimeric
antigen receptor-modified T (CAR-T) cell therapy, T-cell
receptor-engineered T (TCR-T) cell therapy and other cellular
immunotherapies.
One of the most promising approaches in antitumor
therapy is CAR-T-cell therapy, where T cells are redirected against
tumors after the engineered expression of CARs (109). CAR-T cells are not restricted by
MHC and can directly recognize tumor cell surface antigens. To
date, six CAR-T-cell products have been approved by the FDA for use
in patients with relapsed and/or refractory B-cell malignancies
(110-115). However, their effects on solid
tumors have not been satisfactory. The low expression rates of
immunosuppressive factors in the tumor microenvironment and
tumor-associated antigens on the surface of solid tumor cells and
the intracellular nature of most cellular proteins have limited the
clinical application of CAR-T-cell therapy in solid tumors. Studies
have confirmed that the main barriers to CAR-T-cell product
development are related to antigen escape and intrinsic T-cell
dysfunction (116). In NPC, Guo
et al (117) designed a
CAR construct that targets the oncofetal antigen 5T4 (5T4-28Z) and
generated CAR-transduced CIK cells. The results indicated that
5T4-28Z-CIK cells were able to efficiently attack NPC cells in
vitro, suggesting that they may be an attractive tool for
developing an efficient therapy for NPC. Chen et al
(118) successfully produced
LMP2A CAR-T cells that exhibited marked targeted cytotoxicity
against LMP2A-positive NPC cells. Tang et al (119,120) demonstrated that LMP1-specific
CAR-T cells mediated antitumor effects against LMP1-positive NPC
cells in vitro and in vivo. These results are
encouraging. At least four registered clinical studies of CAR-T
cells for the treatment of NPC are currently in progress (Table III).
Unlike CAR T-cell therapy, TCR T-cell therapy has
shown encouraging potential in the treatment of solid tumors
(121,122). TCR T cells have distinct
advantages over CAR T cells in the treatment of solid tumors
(123): i) TCR T cells can
recognize antigens expressed on the cell surface and in
intracellular compartments; ii) TCR T cells are more capable of
invading cancer cells; iii) the intracellular proteins targeted by
TCR T cells are tumor-specific; and iv) the neurotoxicity of TCR
T-cell therapy is less severe than that of CAR T-cell therapy.
Based on excellent efficacy data from a randomized phase III trial
(124), the FDA approved
tebentafusp for patients with HLA-A*02:01-positive
metastatic uveal melanoma. Four ongoing clinical trials are
evaluating TCR T-cell therapy for the treatment of NPC (Table III). An early phase I trial was
designed to investigate the safety and efficacy of EBV CAR T/TCR T
cells in the treatment of recurrent/refractory EBV-positive NPC
(NCT05587543). A phase I/II study (NCT03648697) was conducted to
evaluate the safety and tolerability of EBV-TCR-T (YT-E001) in
patients with EBV-positive R/M NPC. Two phase I/II clinical trials
are investigating the role of LMP2-specific TCR T-cells in
EBV-positive R/M NPC (NCT04509726, NCT03925896).
Other emerging cellular immunotherapy strategies,
such as CAR-NK and CAR-macrophage immunotherapy, should be
evaluated in NPC for their promising clinical efficacy in other
cancers (125,126). Overall, treatment specificity and
targeting are the focus of current ACT studies and the direction of
future research. Although ACT has demonstrated good effcacy with
limited side effects, it is associated with technical and financial
limits.
Tumor therapeutic anti-bodies can target specific
antigens on the surface of cancer cells and kill them through
antibody-dependent cell-mediated cytotoxicity and
complement-dependent cell-mediated cytotoxicity. Turrini et al
(127) identified a BARF1-specific monoclonal antibody as a
novel immunotherapeutic tool for EBV-associated tumors through
preclinical models. Ahmed et al (128) constructed a dimeric
T-cell-engaging bispecific antibody (DiBsAb) targeting LMP2A. Their
results suggested that DiBsAb may be a leading candidate for the
treatment of EBV-associated malignancies.
R/M remains the biggest challenge for NPC.
Fortunately, NPC is an 'immune-hot' tumor and the unique immune
environment of NPC provides rational targets for immunotherapy.
ICIs can non-specifically activate the antitumor immune response by
removing or attenuating the negative regulators of immunoreactive
cells. Thus, ICIs, as pan-cancerous antitumor agents, were found to
have equally promising efficacy in NPC. More research is needed to
find suitable biomarkers for predicting the efficacy of ICIs as
monotherapy or combination therapy to maximize personalized
immunotherapy in NPC. Furthermore, based on current findings, ACT
and therapeutic vaccines have shown early success in treating a
small subset of patients with refractory NPC; immunomodulators and
EBV-specific monoclonal antibodies against NPC remain in the
exploratory phase and their clinical translation still has some way
to go. Of note, EBV-specific vaccines, ACTs and monoclonal
antibodies induce specific antitumor responses by directly or
indirectly targeting tumor antigens. These EBV-specific agents have
few targets and are costly and technically immature to produce. In
addition, factors such as mutations in oncogenes, limited antigen
expression, weak immunogenicity, effector cell self-dysfunction and
immunosuppressive microenvironment in different populations of NPC
and route of drug administration contribute to the efficacy and
safety of EBV-specific immunotherapy. Finally, immunotherapy
undoubtedly offers hope for patients with R/M NPC for whom no
standard treatment is available. In clinical practice, certain
patients with effective immunotherapy resumed immunotherapy after
relapse on discontinuation and still achieved good results. Future
studies may consider combination immunotherapy to enhance the
clinical response, such as ICIs in combination with ACT (129) or CAR T-cell therapy in
combination with an oncolytic virus (130). Therefore, the exploration of the
molecular and cellular drivers of immune escape in NPC may lead to
innovative therapeutic options to improve the outcomes for patients
with NPC.
Not applicable.
HH, YY and XD performed the literature review and
wrote the manuscript. HH and ZH revised the figures and tables.
YCC, ZW and HH revised the manuscript. HH and TL were involved in
the conception of the study. All authors contributed to the article
and have read and approved the submitted version. Data
authentication is not applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
This study was supported by the National Natural Science
Foundation of China-Science and Technology Development Fund, Macau
SAR (grant no. 81661168011) and the Regional Innovation and
Cooperation Project of Sichuan Province (grant no.
2021YFQ0037).
|
1
|
Wong KCW, Hui EP, Lo KW, Lam WKJ, Johnson
D, Li L, Tao Q, Chan KCA, To KF, King AD, et al: Nasopharyngeal
carcinoma: An evolving paradigm. Nat Rev Clin Oncol. 18:679–695.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Renaud S, Lefebvre A, Mordon S, Moralès O
and Delhem N: Novel therapies boosting T cell immunity in epstein
barr virus-associated nasopharyngeal carcinoma. Int J Mol Sci.
21:42922020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Marks JE, Phillips JL and Menck HR: The
National Cancer Data Base report on the relationship of race and
national origin to the histology of nasopharyngeal carcinoma.
Cancer. 83:582–588. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang HY, Chang YL, To KF, Hwang JS, Mai
HQ, Feng YF, Chang ET, Wang CP, Kam MK, Cheah SL, et al: A new
prognostic histopathologic classification of nasopharyngeal
carcinoma. Chin J Cancer. 35:412016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tsao SW, Yip YL, Tsang CM, Pang PS, Lau
VM, Zhang G and Lo KW: Etiological factors of nasopharyngeal
carcinoma. Oral Oncol. 50:330–338. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu Z, Chang ET, Liu Q, Cai Y, Zhang Z,
Chen G, Xie SH, Cao SM, Shao JY, Jia WH, et al: Oral hygiene and
risk of nasopharyngeal carcinoma-A Population-based case-control
study in China. Cancer Epidemiol Biomarkers Prev. 25:1201–1207.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chang ET, Liu Z, Hildesheim A, Liu Q, Cai
Y, Zhang Z, Chen G, Xie SH, Cao SM, Shao JY, et al: Active and
passive smoking and risk of nasopharyngeal carcinoma: A
population-based case-control study in Southern China. Am J
Epidemiol. 185:1272–1280. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xu M, Yao Y, Chen H, Zhang S, Cao SM,
Zhang Z, Luo B, Liu Z, Li Z, Xiang T, et al: Genome sequencing
analysis identifies Epstein-Barr virus subtypes associated with
high risk of nasopharyngeal carcinoma. Nat Genet. 51:1131–1136.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lo KW, Chung GT and To KF: Deciphering the
molecular genetic basis of NPC through molecular, cytogenetic, and
epigenetic approaches. Semin Cancer Biol. 22:79–86. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsang CM, Lui VWY, Bruce JP, Pugh TJ and
Lo KW: Translational genomics of nasopharyngeal cancer. Semin
Cancer Biol. 61:84–100. 2020. View Article : Google Scholar
|
|
12
|
Chen YP, Chan ATC, Le QT, Blanchard P, Sun
Y and Ma J: Nasopharyngeal carcinoma. Lancet. 394:64–80. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang H, Miao J, Xiao X, Hu J, Zhang G,
Peng Y, Lu S, Liang Y, Huang S, Han F, et al: Impact on xerostomia
for nasopharyngeal carcinoma patients treated with superficial
parotid lobe-sparing intensity-modulated radiation therapy
(SPLS-IMRT): A prospective phase II randomized controlled study.
Radiother Oncol. 175:1–9. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huang H, Miao J, Zhao C and Wang L:
Response to Gargi S Sarode, Sachin C Sarode, and Rahul Anand's
Letter to the Editor of Radiotherapy and Oncology regarding the
paper titled 'Impact on xerostomia for nasopharyngeal carcinoma
patients treated with superficial parotid lobe-sparing
intensity-modulated radiation therapy (SPLS-IMRT): A prospective
phase II randomized controlled study' by Huang et al. Radiother
Oncol. 177:2532022. View Article : Google Scholar
|
|
15
|
Wang L, Miao J, Huang H, Chen B, Xiao X,
Zhu M, Liang Y, Xiao W, Huang S, Peng Y, et al: Long-term
survivals, toxicities and the role of chemotherapy in Early-stage
nasopharyngeal carcinoma patients treated with Intensity-modulated
radiation therapy: A retrospective study with 15-year Follow-up.
Cancer Res Treat. 54:118–129. 2022. View Article : Google Scholar :
|
|
16
|
Pan JJ, Ng WT, Zong JF, Chan LL,
O'Sullivan B, Lin SJ, Sze HC, Chen YB, Choi HC, Guo QJ, et al:
Proposal for the 8th edition of the AJCC/UICC staging system for
nasopharyngeal cancer in the era of intensity-modulated
radiotherapy. Cancer. 122:546–558. 2016. View Article : Google Scholar
|
|
17
|
Chen L, Zhang Y, Lai SZ, Li WF, Hu WH, Sun
R, Liu LZ, Zhang F, Peng H, Du XJ, et al: 10-year results of
therapeutic ratio by Intensity-modulated radiotherapy versus
two-dimensional radiotherapy in patients with nasopharyngeal
carcinoma. Oncologist. 24:e38–e45. 2019. View Article : Google Scholar
|
|
18
|
Zhang L, Huang Y, Hong S, Yang Y, Yu G,
Jia J, Peng P, Wu X, Lin Q, Xi X, et al: Gemcitabine plus cisplatin
versus fluorouracil plus cisplatin in recurrent or metastatic
nasopharyngeal carcinoma: A multicentre, randomised, open-label,
phase 3 trial. Lancet. 388:1883–1892. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hong S, Zhang Y, Yu G, Peng P, Peng J, Jia
J, Wu X, Huang Y, Yang Y, Lin Q, et al: Gemcitabine plus cisplatin
versus fluorouracil plus cisplatin as First-line therapy for
recurrent or metastatic nasopharyngeal carcinoma: Final overall
survival analysis of GEM20110714 phase III study. J Clin Oncol.
39:3273–3282. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hua YJ, Han F, Lu LX, Mai HQ, Guo X, Hong
MH, Lu TX and Zhao C: Long-term treatment outcome of recurrent
nasopharyngeal carcinoma treated with salvage intensity modulated
radiotherapy. Eur J Cancer. 48:3422–3428. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xiao W, Liu S, Tian Y, Guan Y, Huang S,
Lin C, Zhao C, Lu T and Han F: Prognostic significance of tumor
volume in locally recurrent nasopharyngeal carcinoma treated with
salvage intensity-modulated radiotherapy. PLoS One.
10:e01253512015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Palucka AK and Coussens LM: The basis of
oncoimmunology. Cell. 164:1233–1247. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Smith C, Wakisaka N, Crough T, Peet J,
Yoshizaki T, Beagley L and Khanna R: Discerning regulation of cis-
and trans-presentation of CD8+ T-cell epitopes by EBV-encoded
oncogene LMP-1 through self-aggregation. Blood. 113:6148–6152.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Münz C, Bickham KL, Subklewe M, Tsang ML,
Chahroudi A, Kurilla MG, Zhang D, O'Donnell M and Steinman RM:
Human CD4(+) T lymphocytes consistently respond to the latent
Epstein-Barr virus nuclear antigen EBNA1. J Exp Med. 191:1649–1660.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee AZE, Tan LSY and Lim CM:
Cellular-based immunotherapy in Epstein-Barr virus induced
nasopharyngeal cancer. Oral Oncol. 84:61–70. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Outh-Gauer S, Alt M, Le Tourneau C,
Augustin J, Broudin C, Gasne C, Denize T, Mirghani H, Fabre E,
Ménard M, et al: Immunotherapy in head and neck cancers: A new
challenge for immunologists, pathologists and clinicians. Cancer
Treat Rev. 65:54–64. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Agathanggelou A, Niedobitek G, Chen R,
Nicholls J, Yin W and Young LS: Expression of immune regulatory
molecules in Epstein-Barr virus-associated nasopharyngeal
carcinomas with prominent lymphoid stroma. Evidence for a
functional interaction between epithelial tumor cells and
infiltrating lymphoid cells. Am J Pathol. 147:1152–1160.
1995.PubMed/NCBI
|
|
28
|
Cui X and Snapper CM: Epstein Barr Virus:
Development of vaccines and immune cell therapy for EBV-associated
diseases. Front Immunol. 12:7344712021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang L, Tian WD, Xu X, Nie B, Lu J, Liu X,
Zhang B, Dong Q, Sunwoo JB, Li G, et al: Epstein-Barr virus nuclear
antigen 1 (EBNA1) protein induction of epithelial-mesenchymal
transition in nasopharyngeal carcinoma cells. Cancer. 120:363–372.
2014. View Article : Google Scholar
|
|
30
|
Fu T, Voo KS and Wang RF: Critical role of
EBNA1-specific CD4+ T cells in the control of mouse
Burkitt lymphoma in vivo. J Clin Invest. 114:542–550. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Young LS, Yap LF and Murray PG:
Epstein-Barr virus: More than 50 years old and still providing
surprises. Nat Rev Cancer. 16:789–802. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yoshizaki T, Kondo S, Endo K, Nakanishi Y,
Aga M, Kobayashi E, Hirai N, Sugimoto H, Hatano M, Ueno T, et al:
Modulation of the tumor microenvironment by Epstein-Barr virus
latent membrane protein 1 in nasopharyngeal carcinoma. Cancer Sci.
109:272–278. 2018. View Article : Google Scholar :
|
|
33
|
Lin CL, Lo WF, Lee TH, Ren Y, Hwang SL,
Cheng YF, Chen CL, Chang YS, Lee SP, Rickinson AB, et al:
Immunization with Epstein-Barr Virus (EBV) peptide-pulsed dendritic
cells induces functional CD8+ T-cell immunity and may lead to tumor
regression in patients with EBV-positive nasopharyngeal carcinoma.
Cancer Res. 62:6952–6958. 2002.PubMed/NCBI
|
|
34
|
Le QT, Colevas AD, O'Sullivan B, Lee AWM,
Lee N, Ma B, Siu LL, Waldron J, Lim CM, Riaz N, et al: Current
treatment landscape of nasopharyngeal carcinoma and potential
trials evaluating the value of immunotherapy. J Natl Cancer Inst.
111:655–663. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Gourzones C, Barjon C and Busson P:
Host-tumor interactions in nasopharyngeal carcinomas. Semin Cancer
Biol. 22:127–136. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li YY, Chung GT, Lui VW, To KF, Ma BB,
Chow C, Woo JK, Yip KY, Seo J, Hui EP, et al: Exome and genome
sequencing of nasopharynx cancer identifies NF-κB pathway
activating mutations. Nat Commun. 8:141212017. View Article : Google Scholar
|
|
37
|
Chen YP, Yin JH, Li WF, Li HJ, Chen DP,
Zhang CJ, Lv JW, Wang YQ, Li XM, Li JY, et al: Single-cell
transcriptomics reveals regulators underlying immune cell diversity
and immune subtypes associated with prognosis in nasopharyngeal
carcinoma. Cell Res. 30:1024–1042. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Pardoll DM: The blockade of immune
checkpoints in cancer immunotherapy. Nat Rev Cancer. 12:252–264.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Francisco LM, Sage PT and Sharpe AH: The
PD-1 pathway in tolerance and autoimmunity. Immunol Rev.
236:219–242. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Okazaki T, Chikuma S, Iwai Y, Fagarasan S
and Honjo T: A rheostat for immune responses: The unique properties
of PD-1 and their advantages for clinical application. Nat Immunol.
14:1212–1218. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Farkona S, Diamandis EP and Blasutig IM:
Cancer immunotherapy: The beginning of the end of cancer? BMC Med.
14:732016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Khalil DN, Smith EL, Brentjens RJ and
Wolchok JD: The future of cancer treatment: Immunomodulation, CARs
and combination immunotherapy. Nat Rev Clin Oncol. 13:273–290.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Chen L and Han X: Anti-PD-1/PD-L1 therapy
of human cancer: Past, present, and future. J Clin Investigation.
125:3384–3391. 2015. View Article : Google Scholar
|
|
44
|
Hsu C, Lee SH, Ejadi S, Even C, Cohen RB,
Le Tourneau C, Mehnert JM, Algazi A, van Brummelen EMJ, Saraf S, et
al: Safety and antitumor activity of pembrolizumab in patients with
programmed death-ligand 1-positive nasopharyngeal carcinoma:
Results of the KEYNOTE-028 Study. J Clin Oncol. 35:4050–4056. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ma BBY, Lim WT, Goh BC, Hui EP, Lo KW,
Pettinger A, Foster NR, Riess JW, Agulnik M, Chang AYC, et al:
Antitumor activity of nivolumab in recurrent and metastatic
nasopharyngeal carcinoma: An international, multicenter study of
the mayo clinic phase 2 consortium (NCI-9742). J Clin Oncol.
36:1412–1418. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yang Y, Zhou T, Chen X, Li J, Pan J, He X,
Lin L, Shi YR, Feng W, Xiong J, et al: Efficacy, safety, and
biomarker analysis of camrelizumab in previously treated recurrent
or metastatic nasopharyngeal carcinoma (CAPTAIN study). J
Immunother Cancer. 9:e0037902021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Fang W, Yang Y, Ma Y, Hong S, Lin L, He X,
Xiong J, Li P, Zhao H, Huang Y, et al: Camrelizumab (SHR-1210)
alone or in combination with gemcitabine plus cisplatin for
nasopharyngeal carcinoma: Results from two single-arm, phase 1
trials. Lancet Oncol. 19:1338–1350. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Ma Y, Fang W, Zhang Y, Yang Y, Hong S,
Zhao Y, Tendolkar A, Chen L, Xu D, Sheng J, et al: A Phase I/II
Open-label study of nivolumab in previously treated advanced or
recurrent nasopharyngeal carcinoma and other solid tumors.
Oncologist. 24:891–e431. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Shen L, Guo J, Zhang Q, Pan H, Yuan Y, Bai
Y, Liu T, Zhou Q, Zhao J, Shu Y, et al: Tislelizumab in Chinese
patients with advanced solid tumors: An open-label,
non-comparative, phase 1/2 study. J Immunother Cancer.
8:e0004372020. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang FH, Wei XL, Feng J, Li Q, Xu N, Hu
XC, Liao W, Jiang Y, Lin XY, Zhang QY, et al: Efficacy, safety, and
correlative biomarkers of toripalimab in previously treated
recurrent or metastatic nasopharyngeal carcinoma: A phase II
clinical trial (POLARIS-02). J Clin Oncol. 39:704–712. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Even C, Wang HM, Li SH, Ngan RK,
Dechaphunkul A, Zhang L, Yen CJ, Chan PC, Chakrabandhu S, Ma BBY,
et al: Phase II, randomized study of spartalizumab (PDR001), an
Anti-PD-1 antibody, versus chemotherapy in patients with
recurrent/metastatic nasopharyngeal cancer. Clin Cancer Res.
27:6413–6423. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ding X, Zhang WJ, You R, Zou X, Wang ZQ,
Ouyang YF, Peng L, Liu YP, Duan CY, Yang Q, et al: Camrelizumab
plus apatinib in patients with recurrent or metastatic
nasopharyngeal carcinoma: An Open-label, Single-arm, phase II
study. J Clin Oncol. 41:2571–2582. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yang Y, Qu S, Li J, Hu C, Xu M, Li W, Zhou
T, Shen L, Wu H, Lang J, et al: Camrelizumab versus placebo in
combination with gemcitabine and cisplatin as first-line treatment
for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st):
A multi-centre, randomised, double-blind, phase 3 trial. Lancet
Oncol. 22:1162–1174. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Mai HQ, Chen QY, Chen D, Hu C, Yang K, Wen
J, Li J, Shi YR, Jin F, Xu R, et al: Toripalimab or placebo plus
chemotherapy as first-line treatment in advanced nasopharyngeal
carcinoma: A multicenter randomized phase 3 trial. Nat Med.
27:1536–1543. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hua Y, You R, Wang Z, Huang P, Lin M,
Ouyang Y, Xie Y, Zou X, Liu Y, Duan C, et al: Toripalimab plus
intensity-modulated radiotherapy for recurrent nasopharyngeal
carcinoma: An open-label single-arm, phase II trial. J Immunother
Cancer. 9:e0032902021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhou X, Niu X, Liu P, Ou D, Zhu Y and Wang
X: Is immune therapy plus chemotherapy more effective than immune
therapy alone for unresectable recurrent nasopharyngeal carcinoma?
Front Immunol. 12:7626632021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Postow MA, Callahan MK and Wolchok JD:
Immune checkpoint blockade in cancer therapy. J Clin Oncol.
33:1974–1982. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Buchbinder E and Hodi FS: Cytotoxic T
lymphocyte antigen-4 and immune checkpoint blockade. J Clin
Investigation. 125:3377–3383. 2015. View Article : Google Scholar
|
|
59
|
Yang Y, Li X, Ma Z, Wang C, Yang Q,
Byrne-Steele M, Hong R, Min Q, Zhou G, Cheng Y, et al: CTLA-4
expression by B-1a B cells is essential for immune tolerance. Nat
Commun. 12:5252021. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Larkin J, Chiarion-Sileni V, Gonzalez R,
Grob JJ, Rutkowski P, Lao CD, Cowey CL, Schadendorf D, Wagstaff J,
Dummer R, et al: Five-year survival with combined nivolumab and
ipilimumab in advanced melanoma. N Engl J Med. 381:1535–1546. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
El-Khoueiry AB, Sangro B, Yau T, Crocenzi
TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling THR, et al:
Nivolumab in patients with advanced hepatocellular carcinoma
(CheckMate 040): An open-label, non-comparative, phase 1/2 dose
escalation and expansion trial. Lancet. 389:2492–2502. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kelley RK, Sangro B, Harris W, Ikeda M,
Okusaka T, Kang YK, Qin S, Tai DW, Lim HY, Yau T, et al: Safety,
Efficacy, and pharmacodynamics of tremelimumab plus durvalumab for
patients with unresectable hepatocellular carcinoma: Randomized
expansion of a phase I/II study. J Clin Oncol. 39:2991–3001. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Xiao M, Qi F, Chen X, Luo Z, Zhang L,
Zheng C, Hu S, Jiang X, Zhou M and Tang J: Functional polymorphism
of cytotoxic T-lymphocyte antigen 4 and nasopharyngeal carcinoma
susceptibility in a Chinese population. Int J Immunogenet.
37:27–32. 2010. View Article : Google Scholar
|
|
64
|
Ahmed MM, Gebriel MG, Morad EA, Saber IM,
Elwan A, Salah M, Fakhr AE, Shalaby AM and Alabiad MA: Expression
of immune checkpoint regulators, cytotoxic T-lymphocyte Antigen-4,
and programmed Death-Ligand 1 in Epstein-Barr Virus-associated
Nasopharyngeal Carcinoma. Appl Immunohistochem Mol Morphol.
29:401–408. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yu X, Huang X, Chen X, Liu J, Wu C, Pu Q,
Wang Y, Kang X and Zhou L: Characterization of a novel anti-human
lymphocyte activation gene 3 (LAG-3) antibody for cancer
immunotherapy. MAbs. 11:1139–1148. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Woo SR, Turnis ME, Goldberg MV, Bankoti J,
Selby M, Nirschl CJ, Bettini ML, Gravano DM, Vogel P, Liu CL, et
al: Immune inhibitory molecules LAG-3 and PD-1 synergistically
regulate T-cell function to promote tumoral immune escape. Cancer
Res. 72:917–927. 2012. View Article : Google Scholar
|
|
67
|
Anderson AC, Joller N and Kuchroo VK:
Lag-3, Tim-3, and TIGIT: Co-inhibitory receptors with specialized
functions in immune regulation. Immunity. 44:989–1004. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Tawbi HA, Schadendorf D, Lipson EJ,
Ascierto PA, Matamala L, Castillo Gutiérrez E, Rutkowski P, Gogas
HJ, Lao CD, De Menezes JJ, et al: Relatlimab and nivolumab versus
nivolumab in untreated advanced melanoma. N Engl J Med. 386:24–34.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Solinas C, De Silva P, Bron D,
Willard-Gallo K and Sangiolo D: Significance of TIM3 expression in
cancer: From biology to the clinic. Semin Oncol. 46:372–379. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Chen TC, Chen CH, Wang CP, Lin PH, Yang
TL, Lou PJ, Ko JY, Wu CT and Chang YL: The immunologic advantage of
recurrent nasopharyngeal carcinoma from the viewpoint of
Galectin-9/Tim-3-related changes in the tumour microenvironment.
Sci Rep. 7:103492017. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Das M, Zhu C and Kuchroo VK: Tim-3 and its
role in regulating anti-tumor immunity. Immunol Rev. 276:97–111.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yang R, Sun L, Li CF, Wang YH, Yao J, Li
H, Yan M, Chang WC, Hsu JM, Cha JH, et al: Galectin-9 interacts
with PD-1 and TIM-3 to regulate T cell death and is a target for
cancer immunotherapy. Nat Commun. 12:8322021. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zhang CX, Huang DJ, Baloche V, Zhang L, Xu
JX, Li BW, Zhao XR, He J, Mai HQ, Chen QY, et al: Galectin-9
promotes a suppressive microenvironment in human cancer by
enhancing STING degradation. Oncogenesis. 9:652020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Rotte A, Jin JY and Lemaire V: Mechanistic
overview of immune checkpoints to support the rational design of
their combinations in cancer immunotherapy. Ann Oncol. 29:71–83.
2018. View Article : Google Scholar
|
|
75
|
Shannon-Lowe C and Rowe M: Epstein Barr
virus entry; kissing and conjugation. Curr Opin Virol. 4:78–84.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Cohen JI: Vaccine development for
epstein-barr virus. Adv Exp Med Biol. 1045:477–493. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Jean-Pierre V, Lupo J, Buisson M, Morand P
and Germi R: Main targets of interest for the development of a
prophylactic or therapeutic epstein-barr virus vaccine. Front
Microbiol. 12:7016112021. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Cui X, Cao Z, Sen G, Chattopadhyay G,
Fuller DH, Fuller JT, Snapper DM, Snow AL, Mond JJ and Snapper CM:
A novel tetrameric gp350 1-470 as a potential Epstein-Barr virus
vaccine. Vaccine. 31:3039–3045. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Cui X, Cao Z, Chen Q, Arjunaraja S, Snow
AL and Snapper CM: Rabbits immunized with Epstein-Barr virus gH/gL
or gB recombinant proteins elicit higher serum virus neutralizing
activity than gp350. Vaccine. 34:4050–4055. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Cui X, Cao Z, Ishikawa Y, Cui S, Imadome
KI and Snapper CM: Immunization with Epstein-barr virus core fusion
machinery envelope proteins elicit high titers of neutralizing
activities and protect humanized mice from lethal dose EBV
challenge. Vaccines (Basel). 9:2852021. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Dasari V, Sinha D, Neller MA, Smith C and
Khanna R: Prophylactic and therapeutic strategies for Epstein-Barr
virus-associated diseases: Emerging strategies for clinical
development. Expert Rev Vaccines. 18:457–474. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Li F, Song D, Lu Y, Zhu H, Chen Z and He
X: Delayed-type hypersensitivity (DTH) immune response related with
EBV-DNA in nasopharyngeal carcinoma treated with autologous
dendritic cell vaccination after radiotherapy. J Immunother.
36:208–214. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Chia WK, Wang WW, Teo M, Tai WM, Lim WT,
Tan EH, Leong SS, Sun L, Chen JJ, Gottschalk S, et al: A phase II
study evaluating the safety and efficacy of an
adenovirus-ΔLMP1-LMP2 transduced dendritic cell vaccine in patients
with advanced metastatic nasopharyngeal carcinoma. Ann Oncol.
23:997–1005. 2012. View Article : Google Scholar
|
|
84
|
Hui EP, Taylor GS, Jia H, Ma BB, Chan SL,
Ho R, Wong WL, Wilson S, Johnson BF, Edwards C, et al: Phase I
trial of recombinant modified vaccinia ankara encoding Epstein-Barr
viral tumor antigens in nasopharyngeal carcinoma patients. Cancer
Res. 73:1676–1688. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Taylor GS, Jia H, Harrington K, Lee LW,
Turner J, Ladell K, Price DA, Tanday M, Matthews J, Roberts C, et
al: A recombinant modified vaccinia ankara vaccine encoding
Epstein-Barr Virus (EBV) target antigens: A phase I trial in UK
patients with EBV-positive cancer. Clin Cancer Res. 20:5009–5022.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Liu X, Lu J, He ML, Li Z, Zhang B, Zhou
LH, Li Q, Li G, Wang L, Tian WD, et al: Antitumor effects of
interferon-alpha on cell growth and metastasis in human
nasopharyngeal carcinoma. Curr Cancer Drug Targets. 12:561–570.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Andtbacka RH, Kaufman HL, Collichio F,
Amatruda T, Senzer N, Chesney J, Delman KA, Spitler LE, Puzanov I,
Agarwala SS, et al: Talimogene laherparepvec improves durable
response rate in patients with advanced melanoma. J Clin Oncol.
33:2780–2788. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Liu RY, Zhou L, Zhang YL, Huang BJ, Ke ML,
Chen JM, Li LX, Fu X, Wu JX and Huang W: An oncolytic adenovirus
enhances antiangiogenic and antitumoral effects of a
replication-deficient adenovirus encoding endostatin by rescuing
its selective replication in nasopharyngeal carcinoma cells.
Biochem Biophys Res Commun. 442:171–176. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Wang JN, Hu P, Zeng MS and Liu RB:
Anti-tumor effect of oncolytic herpes simplex virus G47delta on
human nasopharyngeal carcinoma. Chin J Cancer. 30:831–841. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Chua D, Huang J, Zheng B, Lau SY, Luk W,
Kwong DL, Sham JS, Moss D, Yuen KY, Im SW, et al: Adoptive transfer
of autologous Epstein-Barr virus-specific cytotoxic T cells for
nasopharyngeal carcinoma. Int J Cancer. 94:73–80. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Comoli P, De Palma R, Siena S, Nocera A,
Basso S, Del Galdo F, Schiavo R, Carminati O, Tagliamacco A, Abbate
GF, et al: Adoptive transfer of allogeneic Epstein-Barr virus
(EBV)-specific cytotoxic T cells with in vitro antitumor activity
boosts LMP2-specific immune response in a patient with EBV-related
nasopharyngeal carcinoma. Ann Oncol. 15:113–117. 2004. View Article : Google Scholar
|
|
92
|
Straathof KC, Bollard CM, Popat U, Huls
MH, Lopez T, Morriss MC, Gresik MV, Gee AP, Russell HV, Brenner MK,
et al: Treatment of nasopharyngeal carcinoma with Epstein-Barr
virus-specific T lymphocytes. Blood. 105:1898–1904. 2005.
View Article : Google Scholar
|
|
93
|
Comoli P, Pedrazzoli P, Maccario R, Basso
S, Carminati O, Labirio M, Schiavo R, Secondino S, Frasson C,
Perotti C, et al: Cell therapy of stage IV nasopharyngeal carcinoma
with autologous Epstein-Barr virus-targeted cytotoxic T
lymphocytes. J Clin Oncol. 23:8942–8949. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Louis CU, Straathof K, Bollard CM,
Ennamuri S, Gerken C, Lopez TT, Huls MH, Sheehan A, Wu MF, Liu H,
et al: Adoptive transfer of EBV-specific T cells results in
sustained clinical responses in patients with locoregional
nasopharyngeal carcinoma. J Immunother. 33:983–990. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lutzky VP, Crooks P, Morrison L, Stevens
N, Davis JE, Corban M, Hall D, Panizza B, Coman WB, Coman S, et al:
Cytotoxic T cell adoptive immunotherapy as a treatment for
nasopharyngeal carcinoma. Clin Vaccine Immunol. 21:256–259. 2014.
View Article : Google Scholar :
|
|
96
|
Eom HS, Choi BK, Lee Y, Lee H, Yun T, Kim
YH, Lee JJ and Kwon BS: Phase I clinical trial of 4-1BB-based
adoptive T-cell therapy for epstein-barr virus (EBV)-positive
tumors. J Immunother. 39:140–148. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Louis CU, Straathof K, Bollard CM, Gerken
C, Huls MH, Gresik MV, Wu MF, Weiss HL, Gee AP, Brenner MK, et al:
Enhancing the in vivo expansion of adoptively transferred
EBV-specific CTL with lymphodepleting CD45 monoclonal antibodies in
NPC patients. Blood. 113:2442–2450. 2009. View Article : Google Scholar :
|
|
98
|
Secondino S, Zecca M, Licitra L, Gurrado
A, Schiavetto I, Bossi P, Locati L, Schiavo R, Basso S, Baldanti F,
et al: T-cell therapy for EBV-associated nasopharyngeal carcinoma:
Preparative lymphodepleting chemotherapy does not improve clinical
results. Ann Oncol. 23:435–441. 2012. View Article : Google Scholar
|
|
99
|
Smith C, Tsang J, Beagley L, Chua D, Lee
V, Li V, Moss DJ, Coman W, Chan KH, Nicholls J, et al: Effective
treatment of metastatic forms of Epstein-Barr virus-associated
nasopharyngeal carcinoma with a novel adenovirus-based adoptive
immunotherapy. Cancer Res. 72:1116–1125. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Smith C, Lee V, Schuessler A, Beagley L,
Rehan S, Tsang J, Li V, Tiu R, Smith D, Neller MA, et al:
Pre-emptive and therapeutic adoptive immunotherapy for
nasopharyngeal carcinoma: Phenotype and effector function of T
cells impact on clinical response. Oncoimmunol. 6:e12733112017.
View Article : Google Scholar
|
|
101
|
Huang J, Fogg M, Wirth LJ, Daley H, Ritz
J, Posner MR, Wang FC and Lorch JH: Epstein-Barr virus-specific
adoptive immunotherapy for recurrent, metastatic nasopharyngeal
carcinoma. Cancer. 123:2642–2650. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Chia WK, Teo M, Wang WW, Lee B, Ang SF,
Tai WM, Chee CL, Ng J, Kan R, Lim WT, et al: Adoptive T-cell
transfer and chemotherapy in the first-line treatment of metastatic
and/or locally recurrent nasopharyngeal carcinoma. Mol Ther.
22:132–139. 2014. View Article : Google Scholar :
|
|
103
|
Al-Rajhi N, Soudy H, Ahmed SA, Elhassan T,
Mohammed SF, Khoja HA and Ghebeh H: CD3+T-lymphocyte infiltration
is an independent prognostic factor for advanced nasopharyngeal
carcinoma. BMC Cancer. 20:2402020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Li J, Chen QY, He J, Li ZL, Tang XF, Chen
SP, Xie CM, Li YQ, Huang LX, Ye SB, et al: Phase I trial of
adoptively transferred tumor-infiltrating lymphocyte immunotherapy
following concurrent chemoradiotherapy in patients with
locoregionally advanced nasopharyngeal carcinoma. Oncoimmunology.
4:e9765072015. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Introna M: CIK as therapeutic agents
against tumors. J Autoimmun. 85:32–44. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Li JJ, Gu MF, Pan K, Liu LZ, Zhang H, Shen
WX and Xia JC: Autologous cytokine-induced killer cell transfusion
in combination with gemcitabine plus cisplatin regimen chemotherapy
for metastatic nasopharyngeal carcinoma. J Immunother. 35:189–195.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Li Y, Pan K, Liu LZ, Li YQ, Gu MF, Zhang
H, Shen WX, Xia JC and Li JJ: Sequential Cytokine-induced killer
cell immunotherapy enhances the efficacy of the gemcitabine plus
cisplatin chemotherapy regimen for metastatic nasopharyngeal
carcinoma. PLoS One. 10:e01306202015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Lim CM, Liou A, Poon M, Koh LP, Tan LK,
Loh KS, Petersson BF, Ting E, Campana D, Goh BC, et al: Phase I
study of expanded natural killer cells in combination with
cetuximab for recurrent/metastatic nasopharyngeal carcinoma. Cancer
Immunol Immunother. 71:2277–2286. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Depil S, Duchateau P, Grupp SA, Mufti G
and Poirot L: 'Off-the-shelf' allogeneic CAR T cells: Development
and challenges. Nat Rev Drug Discov. 19:185–199. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Neelapu SS, Locke FL, Bartlett NL, Lekakis
LJ, Miklos DB, Jacobson CA, Braunschweig I, Oluwole OO, Siddiqi T,
Lin Y, et al: Axicabtagene Ciloleucel CAR T-Cell Therapy in
Refractory Large B-Cell Lymphoma. The New England journal of
medicine. 2017.377:2531–44. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Maude SL, Laetsch TW, Buechner J, Rives S,
Boyer M, Bittencourt H, Bader P, Verneris MR, Stefanski HE, Myers
GD, et al: Tisagenlecleucel in Children and Young adults with
B-cell lymphoblastic leukemia. N Engl J Med. 378:439–448. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Wang M, Munoz J, Goy A, Locke FL, Jacobson
CA, Hill BT, Timmerman JM, Holmes H, Jaglowski S, Flinn IW, et al:
KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell
lymphoma. N Engl J Med. 382:1331–1342. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Kamdar M, Solomon SR, Arnason J, Johnston
PB, Glass B, Bachanova V, Ibrahimi S, Mielke S, Mutsaers P, Hernan
dez-Ilizaliturri F, et al: Lisocabtagene maraleucel versus standard
of care with salvage chemotherapy followed by autologous stem cell
transplantation as second-line treatment in patients with relapsed
or refractory large B-cell lymphoma (TRANSFORM): Results from an
interim analysis of an open-label, randomised, phase 3 trial.
Lancet. 399:2294–2308. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Munshi NC, Anderson LD Jr, Shah N, Madduri
D, Berdeja J, Lonial S, Raje N, Lin Y, Siegel D, Oriol A, et al:
Idecabtagene Vicleucel in relapsed and refractory multiple myeloma.
N Engl J Med. 384:705–716. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Berdeja JG, Madduri D, Usmani SZ,
Jakubowiak A, Agha M, Cohen AD, Stewart AK, Hari P, Htut M,
Lesokhin A, et al: Ciltacabtagene autoleucel, a B-cell maturation
antigen-directed chimeric antigen receptor T-cell therapy in
patients with relapsed or refractory multiple myeloma
(CARTITUDE-1): A phase 1b/2 open-label study. Lancet. 398:314–324.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Brown CE and Mackall CL: CAR T cell
therapy: Inroads to response and resistance. Nat Rev Immunol.
19:73–74. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Guo X, Zheng H, Luo W, Zhang Q, Liu J and
Yao K: 5T4-specific chimeric antigen receptor modification promotes
the immune efficacy of cytokine-induced killer cells against
nasopharyngeal carcinoma stem cell-like cells. Sci Rep. 7:48592017.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Chen Y, Chen RJ, Huang XC, Tang GX, Kuai
XW, Zhang MJ, Zhang DW, Tang Q, Zhu J and Feng ZQ: Construction of
latent membrane protein 2A chimeric antigen receptor-T cells and
their lethal effects on nasopharyngeal carcinoma cells. Zhonghua Er
Bi Yan Hou Tou Jing Wai Ke Za Zhi. 53:925–930. 2018.In Chinese.
PubMed/NCBI
|
|
119
|
Tang X, Zhou Y, Li W, Tang Q, Chen R, Zhu
J and Feng Z: T cells expressing a LMP1-specific chimeric antigen
receptor mediate antitumor effects against LMP1-positive
nasopharyngeal carcinoma cells in vitro and in vivo. J Biomed Res.
28:468–475. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Tang X, Tang Q, Mao Y, Huang X, Jia L, Zhu
J and Feng Z: CD137 Co-stimulation improves the antitumor effect of
LMP1-specific chimeric antigen receptor T cells in vitro and in
vivo. Onco Targets Ther. 12:9341–9350. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Liu H, Pan C, Song W, Liu D, Li Z and
Zheng L: Novel strategies for immuno-oncology breakthroughs with
cell therapy. Biomarker Res. 9:622021. View Article : Google Scholar
|
|
122
|
Tsimberidou AM, Van Morris K, Vo HH, Eck
S, Lin YF, Rivas JM and Andersson BS: T-cell receptor-based
therapy: An innovative therapeutic approach for solid tumors. J
Hematol Oncol. 14:1022021. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhang Y, Liu Z, Wei W and Li Y: TCR
engineered T cells for solid tumor immunotherapy. Exp Hematol
Oncol. 11:382022. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Nathan P, Hassel JC, Rutkowski P, Baurain
JF, Butler MO, Schlaak M, Sullivan RJ, Ochsenreither S, Dummer R,
Kirkwood JM, et al: Overall survival benefit with tebentafusp in
metastatic uveal melanoma. N Engl J Med. 385:1196–1206. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Xie G, Dong H, Liang Y, Ham JD, Rizwan R
and Chen J: CAR-NK cells: A promising cellular immunotherapy for
cancer. EBioMedicine. 59:1029752020. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Klichinsky M, Ruella M, Shestova O, Lu XM,
Best A, Zeeman M, Schmierer M, Gabrusiewicz K, Anderson NR, Petty
NE, et al: Human chimeric antigen receptor macrophages for cancer
immunotherapy. Nat Biotechnol. 38:947–953. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Turrini R, Merlo A, Martorelli D, Faè DA,
Sommaggio R, Montagner IM, Barbieri V, Marin O, Zanovello P,
Dolcetti R, et al: A BARF1-specific mAb as a new immunotherapeutic
tool for the management of EBV-related tumors. Oncoimmunology.
6:e13043382017. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Ahmed M, Lopez-Albaitero A, Pankov D,
Santich BH, Liu H, Yan S, Xiang J, Wang P, Hasan AN, Selvakumar A,
et al: TCR-mimic bispecific antibodies targeting LMP2A show potent
activity against EBV malignancies. JCI Insight. 3:e978052018.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Smith C, McGrath M, Neller MA, Matthews
KK, Crooks P, Le Texier L, Panizza B, Porceddu S and Khanna R:
Complete response to PD-1 blockade following EBV-specific T-cell
therapy in metastatic nasopharyngeal carcinoma. NPJ Precision
Oncol. 5:242021. View Article : Google Scholar
|
|
130
|
Rezaei R, Esmaeili Gouvarchin Ghaleh H,
Farzanehpour M, Dorostkar R, Ranjbar R, Bolandian M, Mirzaei
Nodooshan M and Ghorbani Alvanegh A: Combination therapy with CAR T
cells and oncolytic viruses: A new era in cancer immunotherapy.
Cancer Gene Ther. 29:647–660. 2022. View Article : Google Scholar
|