|
1
|
Garcia-Vicién G, Mezheyeuski A, Bañuls M,
Ruiz-Roig N and Molleví DG: The Tumor microenvironment in liver
metastases from colorectal carcinoma in the context of the
histologic growth patterns. Int J Mol Sci. 22:15442021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Luo F, Li J, Wu S, Wu X, Chen M, Zhong X
and Liu K: Comparative profiling between primary colorectal
carcinomas and metastases identifies heterogeneity on drug
resistance. Oncotarget. 7:63937–63949. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
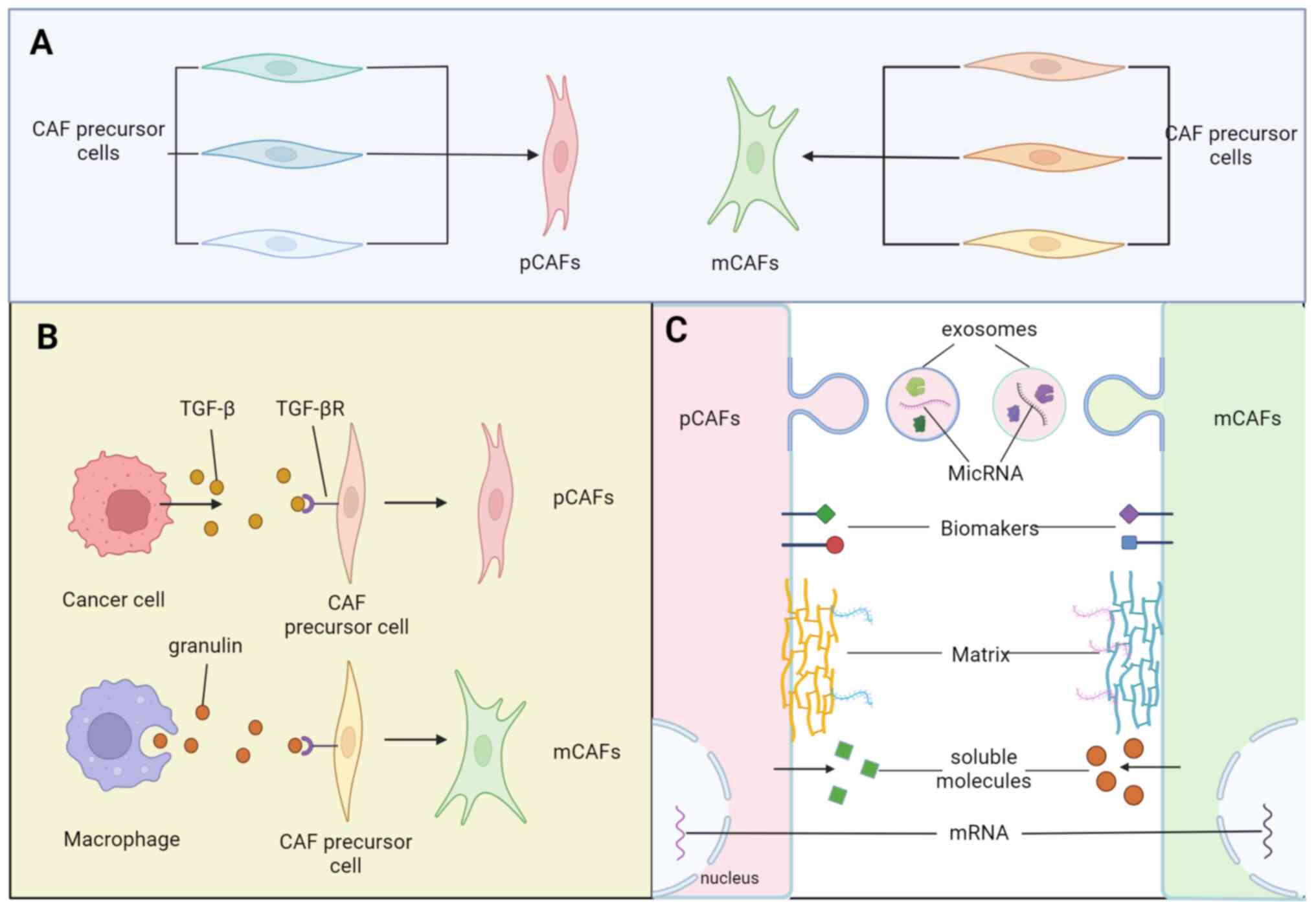
3
|
Hu Z, Li Z, Ma Z and Curtis C:
Multi-cancer analysis of clonality and the timing of systemic
spread in paired primary tumors and metastases. Nat Genet.
52:701–708. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Korentzelos D, Clark AM and Wells A: A
perspective on therapeutic pan-resistance in metastatic cancer. Int
J Mol Sci. 21:73042020. View Article : Google Scholar : PubMed/NCBI
|
|
5
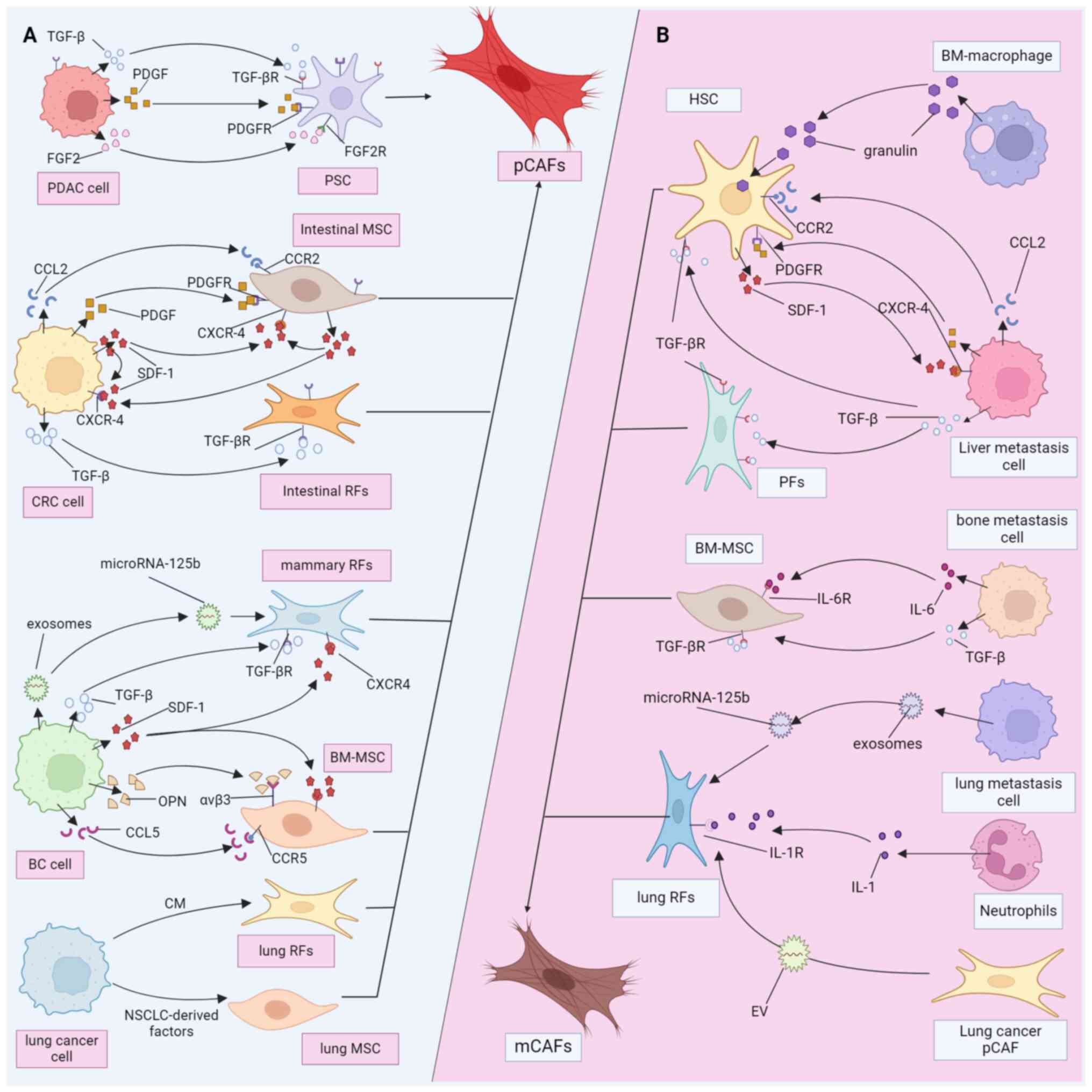
|
Hirata E and Sahai E: Tumor
microenvironment and differential responses to therapy. Cold Spring
Harb Perspect Med. 7:a0267812017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jiménez-Sánchez A, Memon D, Pourpe S,
Veeraraghavan H, Li Y, Vargas HA, Gill MB, Park KJ, Zivanovic O,
Konner J, et al: Heterogeneous tumor-immune microenvironments among
differentially growing metastases in an ovarian cancer patient.
Cell. 170:927–938.e20. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mao X, Xu J, Wang W, Liang C, Hua J, Liu
J, Zhang B, Meng Q, Yu X and Shi S: Crosstalk between
cancer-associated fibroblasts and immune cells in the tumor
microenvironment: New findings and future perspectives. Mol Cancer.
20:1312021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gui Y, Aguilar-Mahecha A, Krzemien U,
Hosein A, Buchanan M, Lafleur J, Pollak M, Ferrario C and Basik M:
Metastatic breast carcinoma-associated fibroblasts have enhanced
protumorigenic properties related to increased IGF2 expression.
Clin Cancer Res. 25:7229–7242. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kalluri R: The biology and function of
fibroblasts in cancer. Nat Rev Cancer. 16:582–598. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen X and Song E: Turning foes to
friends: Targeting cancer-associated fibroblasts. Nat Rev Drug
Discov. 18:99–115. 2019. View Article : Google Scholar
|
|
11
|
Park D, Sahai E and Rullan A: SnapShot:
Cancer-associated fibroblasts. Cell. 181:486–486.e1. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shen Y, Wang X, Lu J, Salfenmoser M,
Wirsik NM, Schleussner N, Imle A, Freire Valls A, Radhakrishnan P,
Liang J, et al: Reduction of liver metastasis stiffness improves
response to bevacizumab in metastatic colorectal cancer. Cancer
Cell. 37:800–817.e7. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ziemys A, Simic V, Milosevic M, Kojic M,
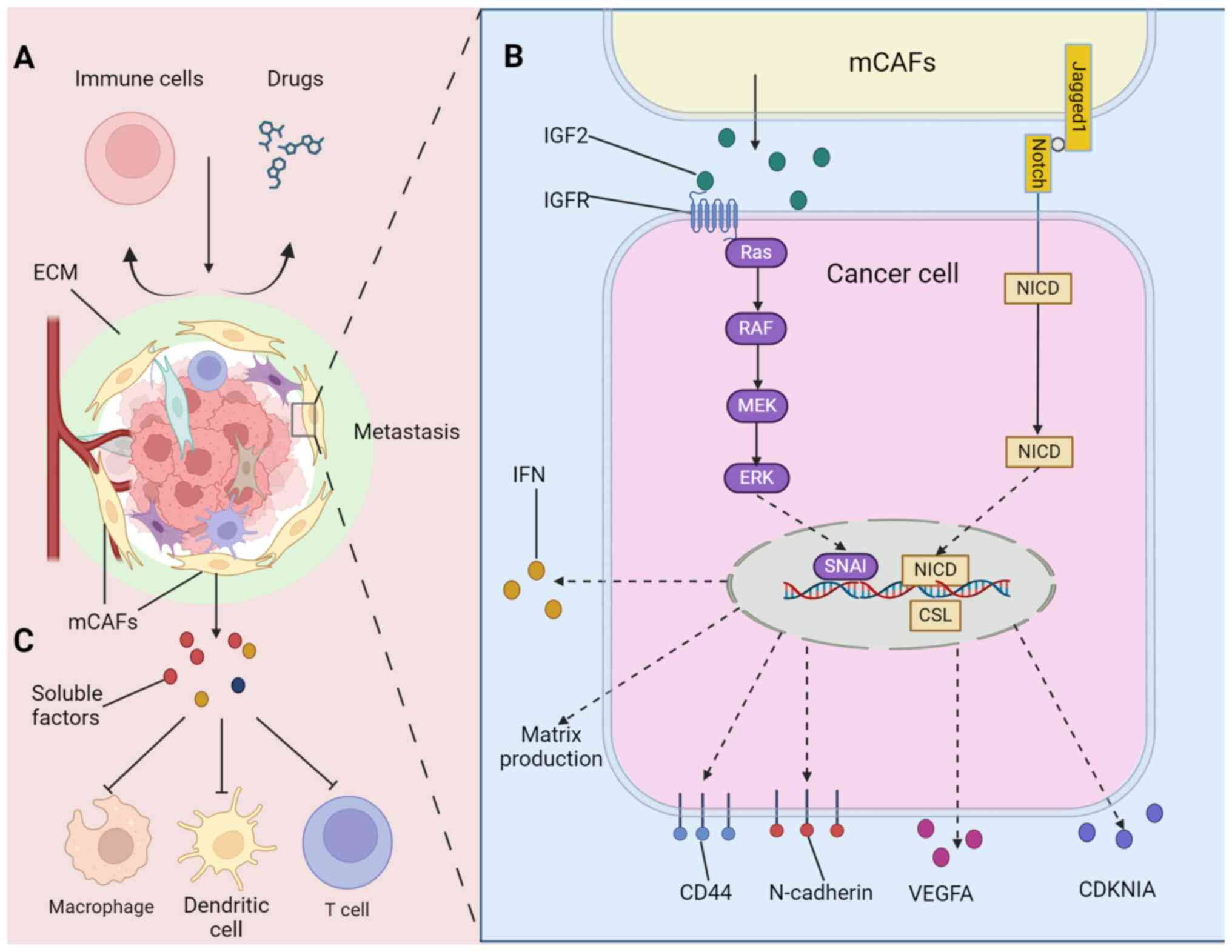
Liu YT and Yokoi K: Attenuated microcirculation in small metastatic
tumors in murine liver. Pharmaceutics. 13:7032021. View Article : Google Scholar : PubMed/NCBI
|
|
14
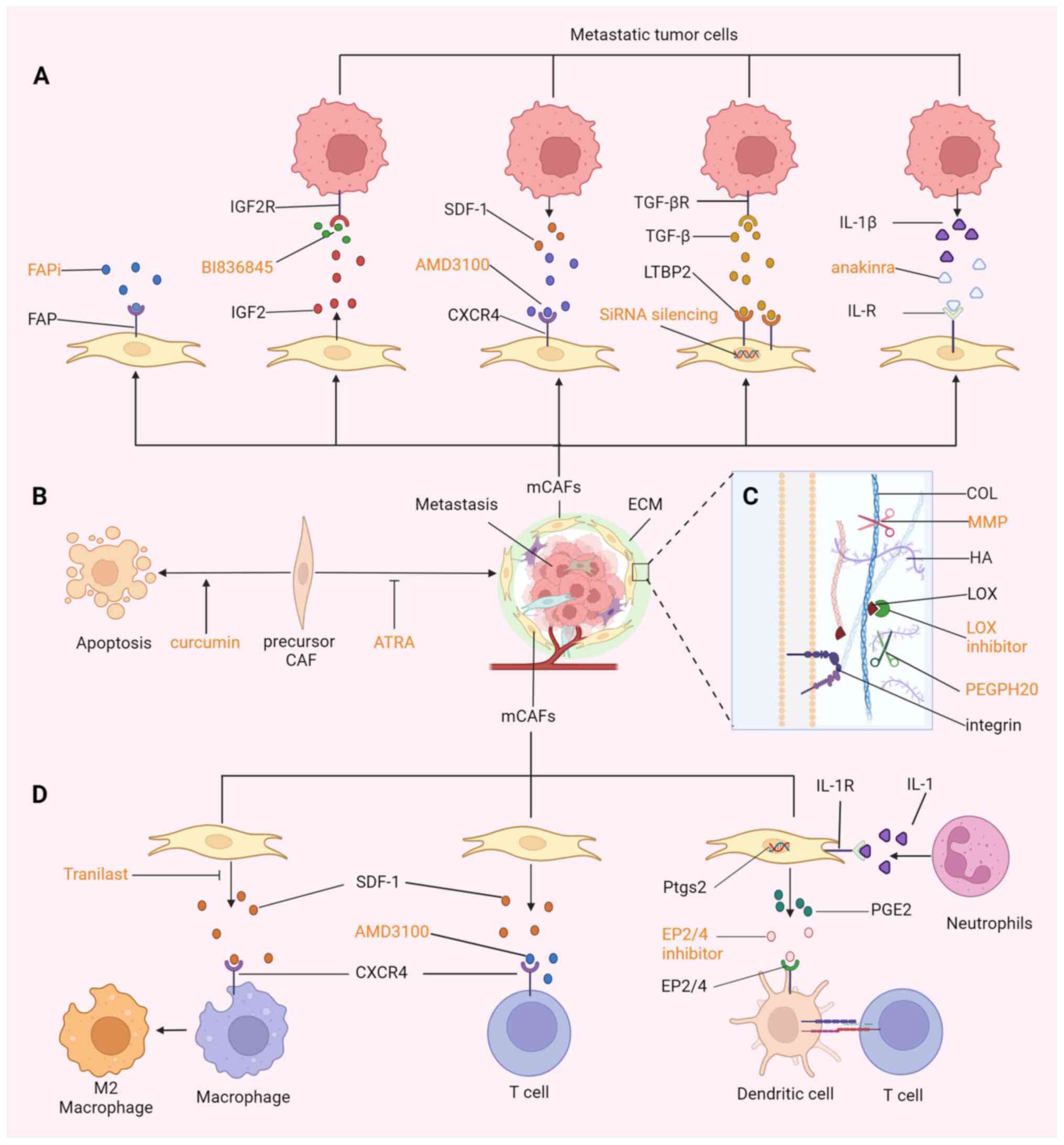
|
Cox TR: The matrix in cancer. Nat Rev
Cancer. 21:217–238. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gertych A, Walts AE, Cheng K, Liu M, John
J, Lester J, Karlan BY and Orsulic S: Dynamic changes in the
extracellular matrix in primary, metastatic, and recurrent ovarian
cancers. Cells. 11:73692022. View Article : Google Scholar
|
|
16
|
Fujimori D, Kinoshita J, Yamaguchi T,
Nakamura Y, Gunjigake K, Ohama T, Sato K, Yamamoto M, Tsukamoto T,
Nomura S, et al: Established fibrous peritoneal metastasis in an
immunocompetent mouse model similar to clinical immune
microenvironment of gastric cancer. BMC Cancer. 20:10142020.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang Z, Liu J, Huang H, Ye M, Li X, Wu R,
Liu H and Song Y: Metastasis-associated fibroblasts: an emerging
target for metastatic cancer. Biomark Res. 9:472021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Biffi G and Tuveson DA: Diversity and
biology of cancer-associated fibroblasts. Physiol Rev. 101:147–176.
2021. View Article : Google Scholar :
|
|
19
|
Miyashita N and Saito A: Organ specificity
and heterogeneity of cancer-associated fibroblasts in colorectal
cancer. Int J Mol Sci. 22:109732021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ganguly D, Chandra R, Karalis J, Teke M,
Aguilera T, Maddipati R, Wachsmann MB, Ghersi D, Siravegna G, Zeh
HJ III, et al: Cancer-associated fibroblasts: versatile players in
the tumor microenvironment. Cancers (Basel). 12:26522020.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bu L, Baba H, Yoshida N, Miyake K, Yasuda
T, Uchihara T, Tan P and Ishimoto T: Biological heterogeneity and
versatility of cancer-associated fibroblasts in the tumor
microenvironment. Oncogene. 38:4887–4901. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bartoschek M, Oskolkov N, Bocci M, Lövrot
J, Larsson C, Sommarin M, Madsen CD, Lindgren D, Pekar G, Karlsson
G, et al: Spatially and functionally distinct subclasses of breast
cancer-associated fibroblasts revealed by single cell RNA
sequencing. Nat Commun. 9:51502018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Potenta S, Zeisberg E and Kalluri R: The
role of endothelial-to-mesenchymal transition in cancer
progression. Br J Cancer. 99:1375–1379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Quante M, Tu SP, Tomita H, Gonda T, Wang
SS, Takashi S, Baik GH, Shibata W, Diprete B, Betz KS, et al: Bone
marrow-derived myofibroblasts contribute to the mesenchymal stem
cell niche and promote tumor growth. Cancer Cell. 19:257–272. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Rhim AD, Mirek ET, Aiello NM, Maitra A,
Bailey JM, McAllister F, Reichert M, Beatty GL, Rustgi AK,
Vonderheide RH, et al: EMT and dissemination precede pancreatic
tumor formation. Cell. 148:349–361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dulauroy S, Di Carlo SE, Langa F, Eberl G
and Peduto L: Lineage tracing and genetic ablation of ADAM12(+)
perivascular cells identify a major source of profibrotic cells
during acute tissue injury. Nat Med. 18:1262–1270. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rinkevich Y, Mori T, Sahoo D, Xu PX,
Bermingham JR Jr and Weissman IL: Identification and prospective
isolation of a mesothelial precursor lineage giving rise to smooth
muscle cells and fibroblasts for mammalian internal organs, and
their vasculature. Nat Cell Biol. 14:1251–1260. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu T, Han C, Wang S, Fang P, Ma Z, Xu L
and Yin R: Cancer-associated fibroblasts: An emerging target of
anti-cancer immunotherapy. J Hematol Oncol. 12:862019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bielczyk-Maczynska E: White adipocyte
plasticity in physiology and disease. Cells. 8:15072019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang X, He C, Hua X, Kan A, Mao Y, Sun S,
Duan F, Wang J, Huang P and Li S: Oxidative stress induces
monocyte-to-myofibroblast transdifferentiation through p38 in
pancreatic ductal adenocarcinoma. Clin Transl Med. 10:e412020.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yamamoto G, Taura K, Iwaisako K, Asagiri
M, Ito S, Koyama Y, Tanabe K, Iguchi K, Satoh M, Nishio T, et al:
Pancreatic stellate cells have distinct characteristics from
hepatic stellate cells and are not the unique origin of
collagen-producing cells in the pancreas. Pancreas. 46:1141–1151.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bachem MG, Schünemann M, Ramadani M, Siech
M, Beger H, Buck A, Zhou S, Schmid-Kotsas A and Adler G: Pancreatic
carcinoma cells induce fibrosis by stimulating proliferation and
matrix synthesis of stellate cells. Gastroenterology. 128:907–921.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Erez N: Fibroblasts form a hospitable
metastatic niche in the liver. Nat Cell Biol. 18:465–466. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bhattacharjee S, Hamberger F, Ravichandra
A, Miller M, Nair A, Affo S, Filliol A, Chin L, Savage TM, Yin D,
et al: Tumor restriction by type I collagen opposes tumor-promoting
effects of cancer-associated fibroblasts. J Clin Invest.
131:e1469872021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Omary MB, Lugea A, Lowe AW and Pandol SJ:
The pancreatic stellate cell: A star on the rise in pancreatic
diseases. J Clin Invest. 117:50–59. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kisseleva T: The origin of fibrogenic
myofibroblasts in fibrotic liver. Hepatology. 65:1039–1043. 2017.
View Article : Google Scholar
|
|
38
|
Klopp AH, Spaeth EL, Dembinski JL,
Woodward WA, Munshi A, Meyn RE, Cox JD, Andreeff M and Marini FC:
Tumor irradiation increases the recruitment of circulating
mesenchymal stem cells into the tumor microenvironment. Cancer Res.
67:11687–11695. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Spaeth EL, Dembinski JL, Sasser AK, Watson
K, Klopp A, Hall B, Andreeff M and Marini F: Mesenchymal stem cell
transition to tumor-associated fibroblasts contributes to
fibrovascular network expansion and tumor progression. PLoS One.
4:e49922009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Mi Z, Bhattacharya SD, Kim VM, Guo H,
Talbot LJ and Kuo PC: Osteopontin promotes CCL5-mesenchymal stromal
cell-mediated breast cancer metastasis. Carcinogenesis. 32:477–487.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Raz Y, Cohen N, Shani O, Bell RE,
Novitskiy SV, Abramovitz L, Levy C, Milyavsky M, Leider-Trejo L,
Moses HL, et al: Bone marrow-derived fibroblasts are a functionally
distinct stromal cell population in breast cancer. J Exp Med.
215:3075–3093. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Liu Z, Wang H, He J, Yuan X and Sun W:
Rictor ablation in BMSCs inhibits bone metastasis of TM40D cells by
attenuating osteolytic destruction and CAF formation. Int J Biol
Sci. 15:2448–2460. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Jiang Z, Zhou J, Li L, Liao S, He J, Zhou
S and Zhou Y: Pericytes in the tumor microenvironment. Cancer Lett.
556:2160742023. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hosaka K, Yang Y, Seki T, Fischer C, Dubey
O, Fredlund E, Hartman J, Religa P, Morikawa H, Ishii Y, et al:
Pericyte-fibroblast transition promotes tumor growth and
metastasis. Proc Natl Acad Sci USA. 113:E5618–E5627. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bakir B, Chiarella AM, Pitarresi JR and
Rustgi AK: EMT, MET, plasticity, and tumor metastasis. Trends Cell
Biol. 30:764–776. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Erez N, Truitt M, Olson P, Arron ST and
Hanahan D: Cancer-associated fibroblasts are activated in incipient
neoplasia to orchestrate tumor-promoting inflammation in an
NF-kappaB-dependent manner. Cancer Cell. 17:135–147. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Sharon Y, Raz Y, Cohen N, Ben-Shmuel A,
Schwartz H, Geiger T and Erez N: Tumor-derived osteopontin
reprograms normal mammary fibroblasts to promote inflammation and
tumor growth in breast cancer. Cancer Res. 75:963–973. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Vu LT, Peng B, Zhang DX, Ma V,
Mathey-Andrews CA, Lam CK, Kiomourtzis T, Jin J, McReynolds L,
Huang L, et al: Tumor-secreted extracellular vesicles promote the
activation of cancer-associated fibroblasts via the transfer of
microRNA-125b. J Extracell Vesicles. 8:15996802019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gong Z, Li Q, Shi J, Wei J, Li P, Chang
CH, Shultz LD and Ren G: Lung fibroblasts facilitate pre-metastatic
niche formation by remodeling the local immune microenvironment.
Immunity. 55:1483–1500.e9. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
D'Arcangelo E, Wu NC, Cadavid JL and
McGuigan AP: The life cycle of cancer-associated fibroblasts within
the tumour stroma and its importance in disease outcome. Br J
Cancer. 122:931–942. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Koliaraki V, Pallangyo CK, Greten FR and
Kollias G: Mesenchymal cells in colon cancer. Gastroenterology.
152:964–979. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Hawinkels LJAC, Paauwe M, Verspaget HW,
Wiercinska E, van der Zon JM, van der Ploeg K, Koelink PJ, Lindeman
JHN, Mesker W, ten Dijke P and Sier CFM: Interaction with colon
cancer cells hyperactivates TGF-β signaling in cancer-associated
fibroblasts. Oncogene. 33:97–107. 2014. View Article : Google Scholar
|
|
53
|
Kobayashi H, Gieniec KA, Lannagan TRM,
Wang T, Asai N, Mizutani Y, Iida T, Ando R, Thomas EM, Sakai A, et
al: The origin and contribution of cancer-associated fibroblasts in
colorectal carcinogenesis. Gastroenterology. 162:890–906. 2022.
View Article : Google Scholar
|
|
54
|
Shinagawa K, Kitadai Y, Tanaka M, Sumida
T, Kodama M, Higashi Y, Tanaka S, Yasui W and Chayama K:
Mesenchymal stem cells enhance growth and metastasis of colon
cancer. Int J Cancer. 127:2323–2333. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Flier SN, Tanjore H, Kokkotou EG, Sugimoto
H, Zeisberg M and Kalluri R: Identification of epithelial to
mesenchymal transition as a novel source of fibroblasts in
intestinal fibrosis. J Biol Chem. 285:20202–20212. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Apte MV, Park S, Phillips PA, Santucci N,
Goldstein D, Kumar RK, Ramm GA, Buchler M, Friess H, McCarroll JA,
et al: Desmoplastic reaction in pancreatic cancer: Role of
pancreatic stellate cells. Pancreas. 29:179–187. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Houg DS and Bijlsma MF: The hepatic
pre-metastatic niche in pancreatic ductal adenocarcinoma. Mol
Cancer. 17:952018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Öhlund D, Handly-Santana A, Biffi G,
Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA,
Lee EJ, et al: Distinct populations of inflammatory fibroblasts and
myofibroblasts in pancreatic cancer. J Exp Med. 214:579–596. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Elyada E, Bolisetty M, Laise P, Flynn WF,
Courtois ET, Burkhart RA, Teinor JA, Belleau P, Biffi G, Lucito MS,
et al: Cross-species single-cell analysis of pancreatic ductal
adenocarcinoma reveals antigen-presenting cancer-associated
fibroblasts. Cancer Discov. 9:1102–1123. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Tsoumakidou M: The advent of immune
stimulating CAFs in cancer. Nat Rev Cancer. 23:258–269. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Dominguez CX, Müller S, Keerthivasan S,
Koeppen H, Hung J, Gierke S, Breart B, Foreman O, Bainbridge TW,
Castiglioni A, et al: Single-cell RNA sequencing reveals stromal
evolution into LRRC15+ myofibroblasts as a determinant
of patient response to cancer immunotherapy. Cancer Discov.
10:232–253. 2020. View Article : Google Scholar
|
|
62
|
Huang H, Wang Z, Zhang Y, Pradhan RN,
Ganguly D, Chandra R, Murimwa G, Wright S, Gu X, Maddipati R, et
al: Mesothelial cell-derived antigen-presenting cancer-associated
fibroblasts induce expansion of regulatory T cells in pancreatic
cancer. Cancer Cell. 40:656–673.e7. 2022. View Article : Google Scholar :
|
|
63
|
Iwaisako K, Jiang C, Zhang M, Cong M,
Moore-Morris TJ, Park TJ, Liu X, Xu J, Wang P, Paik YH, et al:
Origin of myofibroblasts in the fibrotic liver in mice. Proc Natl
Acad Sci USA. 111:E3297–E3305. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Lua I, Li Y, Zagory JA, Wang KS, French
SW, Sévigny J and Asahina K: Characterization of hepatic stellate
cells, portal fibroblasts, and mesothelial cells in normal and
fibrotic livers. J Hepatol. 64:1137–1146. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Tsuchida T and Friedman SL: Mechanisms of
hepatic stellate cell activation. Nat Rev Gastroenterol Hepatol.
14:397–411. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
O'Hara SP and LaRusso NF: Portal
fibroblasts: A renewable source of liver myofibroblasts.
Hepatology. 76:1240–1242. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Xie Z, Gao Y, Ho C, Li L, Jin C, Wang X,
Zou C, Mao Y, Wang X, Li Q, et al: Exosome-delivered CD44v6/C1QBP
complex drives pancreatic cancer liver metastasis by promoting
fibrotic liver microenvironment. Gut. 71:568–579. 2022. View Article : Google Scholar
|
|
68
|
Giguelay A, Turtoi E, Khelaf L, Tosato G,
Dadi I, Chastel T, Poul MA, Pratlong M, Nicolescu S, Severac D, et
al: The landscape of cancer-associated fibroblasts in colorectal
cancer liver metastases. Theranostics. 12:7624–7639. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Tan HX, Gong WZ, Zhou K, Xiao ZG, Hou FT,
Huang T, Zhang L, Dong HY, Zhang WL, Liu Y and Huang ZC:
CXCR4/TGF-β1 mediated hepatic stellate cells differentiation into
carcinoma-associated fibroblasts and promoted liver metastasis of
colon cancer. Cancer Biol Ther. 21:258–268. 2020. View Article : Google Scholar
|
|
70
|
Mukaida N, Zhang D and Sasaki SI:
Emergence of cancer-associated fibroblasts as an indispensable
cellular player in bone metastasis process. Cancers (Basel).
12:28962020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Houthuijzen JM and de Visser KE: The lung
fibroblast as 'soil fertilizer' in breast cancer metastasis.
Immunity. 55:1336–1339. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Chang HY, Chi JT, Dudoit S, Bondre C, van
de Rijn M, Botstein D and Brown PO: Diversity, topographic
differentiation, and positional memory in human fibroblasts. Proc
Natl Acad Sci USA. 99:12877–12882. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Apte MV, Wilson JS, Lugea A and Pandol SJ:
A starring role for stellate cells in the pancreatic cancer
microenvironment. Gastroenterology. 144:1210–1219. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Hessmann E, Patzak MS, Klein L, Chen N,
Kari V, Ramu I, Bapiro TE, Frese KK, Gopinathan A, Richards FM, et
al: Fibroblast drug scavenging increases intratumoural gemcitabine
accumulation in murine pancreas cancer. Gut. 67:497–507. 2018.
View Article : Google Scholar
|
|
75
|
Helms EJ, Berry MW, Chaw RC, DuFort CC,
Sun D, Onate MK, Oon C, Bhattacharyya S, Sanford-Crane H, Horton W,
et al: Mesenchymal lineage heterogeneity underlies nonredundant
functions of pancreatic cancer-associated fibroblasts. Cancer
Discov. 12:484–501. 2022. View Article : Google Scholar
|
|
76
|
Garcia PE, Adoumie M, Kim EC, Zhang Y,
Scales MK, El-Tawil YS, Shaikh AZ, Wen HJ, Bednar F, Allen BL, et
al: Differential contribution of pancreatic fibroblast subsets to
the pancreatic cancer stroma. Cell Mol Gastroenterol Hepatol.
10:581–599. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zhang Y, Bian Y, Wang Y, Wang Y, Duan X,
Han Y, Zhang L, Wang F, Gu Z and Qin Z: HIF-1α is necessary for
activation and tumour-promotion effect of cancer-associated
fibroblasts in lung cancer. J Cell Mol Med. 25:5457–5469. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Shintani Y, Fujiwara A, Kimura T, Kawamura
T, Funaki S, Minami M and Okumura M: IL-6 secreted from
cancer-associated fibroblasts mediates chemoresistance in NSCLC by
increasing epithelial-mesenchymal transition signaling. J Thorac
Oncol. 11:1482–1492. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Gottschling S, Granzow M, Kuner R, Jauch
A, Herpel E, Xu EC, Muley T, Schnabel PA, Herth FJ and Meister M:
Mesenchymal stem cells in non-small cell lung cancer-different from
others? Insights from comparative molecular and functional
analyses. Lung Cancer. 80:19–29. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Wang H, Shui L, Chen R and Chen Y, Guo J
and Chen Y: Occurrence and prognosis of lung cancer metastasis to
major organs: A population-based study. Eur J Cancer Prev.
32:246–253. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Kong J, Tian H, Zhang F, Zhang Z, Li J,
Liu X, Li X, Liu J, Li X, Jin D, et al: Extracellular vesicles of
carcinoma-associated fibroblasts creates a pre-metastatic niche in
the lung through activating fibroblasts. Mol Cancer. 18:1752019.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Duda DG, Duyverman AM, Kohno M, Snuderl M,
Steller EJ, Fukumura D and Jain RK: Malignant cells facilitate lung
metastasis by bringing their own soil. Proc Natl Acad Sci USA.
107:21677–21682. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Buchsbaum RJ and Oh SY: Breast
cancer-associated fibroblasts: Where We Are And Where We Need To
Go. Cancers (Basel). 8:192016. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Hu D, Li Z, Zheng B, Lin X, Pan Y, Gong P,
Zhuo W, Hu Y, Chen C, Chen L, et al: Cancer-associated fibroblasts
in breast cancer: Challenges and opportunities. Cancer Commun
(Lond). 42:401–434. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Friedman G, Levi-Galibov O, David E,
Bornstein C, Giladi A, Dadiani M, Mayo A, Halperin C,
Pevsner-Fischer M, Lavon H, et al: Cancer-associated fibroblast
compositions change with breast cancer progression linking the
ratio of S100A4+ and PDPN+ CAFs to clinical
outcome. Nat Cancer. 1:692–708. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhang XHF, Jin X, Malladi S, Zou Y, Wen
YH, Brogi E, Smid M, Foekens JA and Massagué J: Selection of bone
metastasis seeds by mesenchymal signals in the primary tumor
stroma. Cell. 154:1060–1073. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Kuo MC, Kothari AN, Kuo PC and Mi Z:
Cancer stemness in bone marrow micrometastases of human breast
cancer. Surgery. 163:330–335. 2018. View Article : Google Scholar
|
|
88
|
Ban J, Fock V, Aryee DNT and Kovar H:
Mechanisms, diagnosis and treatment of bone metastases. Cells.
10:29442021. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Haider MT, Smit DJ and Taipaleenmäki H:
The endosteal niche in breast cancer bone metastasis. Front Oncol.
10:3352020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Croucher PI, McDonald MM and Martin TJ:
Bone metastasis: The importance of the neighbourhood. Nat Rev
Cancer. 16:373–386. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Cassell K, Thomas-Lopez D, Kjelsø C and
Uldum S: Provincial trends in Legionnaires' disease are not
explained by population structure in Denmark, 2015 to 2018. Euro
Surveill. 26:20000362021. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Mundim FGL, Pasini FS, Nonogaki S, Rocha
RM, Soares FA, Brentani MM and Logullo AF: Breast
carcinoma-associated fibroblasts share similar biomarker profiles
in matched lymph node metastasis. Appl Immunohistochem Mol Morphol.
24:712–720. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Del Valle PR, Milani C, Brentani MM,
Katayama ML, de Lyra EC, Carraro DM, Brentani H, Puga R, Lima LA,
Rozenchan PB, et al: Transcriptional profile of fibroblasts
obtained from the primary site, lymph node and bone marrow of
breast cancer patients. Genet Mol Biol. 37:480–489. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Puram SV, Tirosh I, Parikh AS, Patel AP,
Yizhak K, Gillespie S, Rodman C, Luo CL, Mroz EA, Emerick KS, et
al: Single-cell transcriptomic analysis of primary and metastatic
tumor ecosystems in head and neck cancer. Cell. 171:1611–1624.e24.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Han L, Wu Y, Fang K, Sweeney S, Roesner
UK, Parrish M, Patel K, Walter T, Piermattei J, Trimboli A, et al:
The splanchnic mesenchyme is the tissue of origin for pancreatic
fibroblasts during homeostasis and tumorigenesis. Nat Commun.
14:12023. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Nielsen SR, Quaranta V, Linford A, Emeagi
P, Rainer C, Santos A, Ireland L, Sakai T, Sakai K, Kim YS, et al:
Macrophage-secreted granulin supports pancreatic cancer metastasis
by inducing liver fibrosis. Nat Cell Biol. 18:549–560. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Zhang C, Wang XY, Zhang P, He TC, Han JH,
Zhang R, Lin J, Fan J, Lu L, Zhu WW, et al: Cancer-derived exosomal
HSPC111 promotes colorectal cancer liver metastasis by
reprogramming lipid metabolism in cancer-associated fibroblasts.
Cell Death Dis. 13:572022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Calon A, Espinet E, Palomo-Ponce S,
Tauriello DV, Iglesias M, Céspedes MV, Sevillano M, Nadal C, Jung
P, Zhang XH, et al: Dependency of colorectal cancer on a
TGF-β-driven program in stromal cells for metastasis initiation.
Cancer Cell. 22:571–584. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Shi M, Zhu J, Wang R, Chen X, Mi L, Walz T
and Springer TA: Latent TGF-β structure and activation. Nature.
474:343–349. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Massagué J: TGFbeta signalling in context.
Nat Rev Mol Cell Biol. 13:616–630. 2012. View Article : Google Scholar
|
|
101
|
Su J, Morgani SM, David CJ, Wang Q, Er EE,
Huang YH, Basnet H, Zou Y, Shu W, Soni RK, et al: TGF-β
orchestrates fibrogenic and developmental EMTs via the RAS effector
RREB1. Nature. 577:566–571. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Kojima Y, Acar A, Eaton EN, Mellody KT,
Scheel C, Ben-Porath I, Onder TT, Wang ZC, Richardson AL, Weinberg
RA and Orimo A: Autocrine TGF-beta and stromal cell-derived
factor-1 (SDF-1) signaling drives the evolution of tumor-promoting
mammary stromal myofibroblasts. Proc Natl Acad Sci USA.
107:20009–20014. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Chen IX, Chauhan VP, Posada J, Ng MR, Wu
MW, Adstamongkonkul P, Huang P, Lindeman N, Langer R and Jain RK:
Blocking CXCR4 alleviates desmoplasia, increases T-lymphocyte
infiltration, and improves immunotherapy in metastatic breast
cancer. Proc Natl Acad Sci USA. 116:4558–4566. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Eckert MA, Coscia F, Chryplewicz A, Chang
JW, Hernandez KM, Pan S, Tienda SM, Nahotko DA, Li G, Blaženović I,
et al: Proteomics reveals NNMT as a master metabolic regulator of
cancer-associated fibroblasts. Nature. 569:723–728. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Biffi G, Oni TE, Spielman B, Hao Y, Elyada
E, Park Y, Preall J and Tuveson DA: IL1-induced JAK/STAT signaling
is antagonized by TGFβ to shape CAF heterogeneity in pancreatic
ductal adenocarcinoma. Cancer Discov. 9:282–301. 2019. View Article : Google Scholar
|
|
106
|
Chen Y, McAndrews KM and Kalluri R:
Clinical and therapeutic relevance of cancer-associated
fibroblasts. Nat Rev Clin Oncol. 18:792–804. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Maehira H, Miyake T, Iida H, Tokuda A,
Mori H, Yasukawa D, Mukaisho KI, Shimizu T and Tani M: Vimentin
expression in tumor microenvironment predicts survival in
pancreatic ductal adenocarcinoma: Heterogeneity in fibroblast
population. Ann Surg Oncol. 26:4791–4804. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Paulsson J and Micke P: Prognostic
relevance of cancer-associated fibroblasts in human cancer. Semin
Cancer Biol. 25:61–68. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Kim HM, Jung WH and Koo JS: Expression of
cancer-associated fibroblast related proteins in metastatic breast
cancer: An immunohistochemical analysis. J Transl Med. 13:2222015.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Koerber SA, Staudinger F, Kratochwil C,
Adeberg S, Haefner MF, Ungerechts G, Rathke H, Winter E, Lindner T,
Syed M, et al: The role of 68Ga-FAPI PET/CT for patients
with malignancies of the lower gastrointestinal tract: First
clinical experience. J Nucl Med. 61:1331–1336. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Altmann A, Haberkorn U and Siveke J: The
latest developments in imaging of fibroblast activation protein. J
Nucl Med. 62:160–167. 2021. View Article : Google Scholar
|
|
112
|
Imlimthan S, Moon ES, Rathke H,
Afshar-Oromieh A, Rösch F, Rominger A and Gourni E: New frontiers
in cancer imaging and therapy based on radiolabeled fibroblast
activation protein inhibitors: A rational review and current
progress. Pharmaceuticals (Basel). 14:10232021. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Zhao L, Chen J, Pang Y, Fu K, Shang Q, Wu
H, Sun L, Lin Q and Chen H: Fibroblast activation protein-based
theranostics in cancer research: A state-of-the-art review.
Theranostics. 12:1557–1569. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Zubaľ M, Výmolová B, Matrasová I, Výmola
P, Vepřková J, Syrůček M, Tomáš R, Vaníčková Z, Křepela E, Konečná
D, et al: Fibroblast activation protein as a potential theranostic
target in brain metastases of diverse solid tumours. Pathology.
55:806–817. 2023. View Article : Google Scholar
|
|
115
|
Peltier A, Seban RD, Buvat I, Bidard FC
and Mechta-Grigoriou F: Fibroblast heterogeneity in solid tumors:
From single cell analysis to whole-body imaging. Semin Cancer Biol.
86:262–272. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Taralli S, Lorusso M, Perrone E, Perotti
G, Zagaria L and Calcagni ML: PET/CT with fibroblast activation
protein inhibitors in breast cancer: Diagnostic and theranostic
application-A literature review. Cancers (Basel). 15:9082023.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Dong Y, Zhou H, Alhaskawi A, Wang Z, Lai
J, Yao C, Liu Z, Hasan Abdullah Ezzi S, Goutham Kota V, Hasan
Abdulla Hasan Abdulla M and Lu H: The superiority of fibroblast
activation protein inhibitor (FAPI) PET/CT versus FDG PET/CT in the
diagnosis of various malignancies. Cancers (Basel). 15:11932023.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Serfling S, Zhi Y, Schirbel A, Lindner T,
Meyer T, Gerhard-Hartmann E, Lapa C, Hagen R, Hackenberg S, Buck AK
and Scherzad A: Improved cancer detection in Waldeyer's tonsillar
ring by 68Ga-FAPI PET/CT imaging. Eur J Nucl Med Mol
Imaging. 48:1178–1187. 2021. View Article : Google Scholar
|
|
119
|
Mona CE, Benz MR, Hikmat F, Grogan TR,
Lueckerath K, Razmaria A, Riahi R, Slavik R, Girgis MD, Carlucci G,
et al: Correlation of 68Ga-FAPi-46 PET biodistribution
with FAP expression by immunohistochemistry in patients with solid
cancers: Interim analysis of a prospective translational
exploratory study. J Nucl Med. 63:1021–1026. 2022. View Article : Google Scholar :
|
|
120
|
Sollini M, Kirienko M, Gelardi F, Fiz F,
Gozzi N and Chiti A: State-of-the-art of FAPI-PET imaging: A
systematic review and meta-analysis. Eur J Nucl Med Mol Imaging.
48:4396–4414. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Yazdani S, Bansal R and Prakash J: Drug
targeting to myofibroblasts: Implications for fibrosis and cancer.
Adv Drug Deliv Rev. 121:101–116. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Becker LM, O'Connell JT, Vo AP, Cain MP,
Tampe D, Bizarro L, Sugimoto H, McGow AK, Asara JM, Lovisa S, et
al: Epigenetic reprogramming of cancer-associated fibroblasts
deregulates glucose metabolism and facilitates progression of
breast cancer. Cell Rep. 31:1077012020. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Muchlińska A, Nagel A, Popęda M, Szade J,
Niemira M, Zieliński J, Skokowski J, Bednarz-Knoll N and Żaczek AJ:
Alpha-smooth muscle actin-positive cancer-associated fibroblasts
secreting osteopontin promote growth of luminal breast cancer. Cell
Mol Biol Lett. 27:452022. View Article : Google Scholar
|
|
124
|
Kwak Y, Lee HE, Kim WH, Kim DW, Kang SB
and Lee HS: The clinical implication of cancer-associated
microvasculature and fibroblast in advanced colorectal cancer
patients with synchronous or metachronous metastases. PLoS One.
9:e918112014. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Itou RA, Uyama N, Hirota S, Kawada N, Wu
S, Miyashita S, Nakamura I, Suzumura K, Sueoka H, Okada T, et al:
Immunohistochemical characterization of cancer-associated
fibroblasts at the primary sites and in the metastatic lymph nodes
of human intrahepatic cholangiocarcinoma. Hum Pathol. 83:77–89.
2019. View Article : Google Scholar
|
|
126
|
Borriello L, Nakata R, Sheard MA,
Fernandez GE, Sposto R, Malvar J, Blavier L, Shimada H, Asgharzadeh
S, Seeger RC and DeClerck YA: Cancer-associated fibroblasts share
characteristics and protumorigenic activity with mesenchymal
stromal cells. Cancer Res. 77:5142–5157. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Zhang J, Chen L, Liu X, Kammertoens T,
Blankenstein T and Qin Z: Fibroblast-specific protein
1/S100A4-positive cells prevent carcinoma through collagen
production and encapsulation of carcinogens. Cancer Res.
73:2770–2781. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Shindo K, Aishima S, Ohuchida K, Fujiwara
K, Fujino M, Mizuuchi Y, Hattori M, Mizumoto K, Tanaka M and Oda Y:
Podoplanin expression in cancer-associated fibroblasts enhances
tumor progression of invasive ductal carcinoma of the pancreas. Mol
Cancer. 12:1682013. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Kubouchi Y, Yurugi Y, Wakahara M, Sakabe
T, Haruki T, Nosaka K, Miwa K, Araki K, Taniguchi Y, Shiomi T, et
al: Podoplanin expression in cancer-associated fibroblasts predicts
unfavourable prognosis in patients with pathological stage IA lung
adenocarcinoma. Histopathology. 72:490–499. 2018. View Article : Google Scholar
|
|
130
|
Zhou Q, Wang Z, Zeng H, Zhang H, Liu Z,
Huang Q, Wang J, Chang Y, Bai Q, Liu L, et al: Identification and
validation of poor prognosis immunoevasive subtype of
muscle-invasive bladder cancer with tumor-infiltrating
podoplanin+ cell abundance. Oncoimmunology.
9:17473332020. View Article : Google Scholar
|
|
131
|
Wang P, Song L, Ge H, Jin P, Jiang Y, Hu W
and Geng N: Crenolanib, a PDGFR inhibitor, suppresses lung cancer
cell proliferation and inhibits tumor growth in vivo. Onco Targets
Ther. 7:1761–1768. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Matsuwaki R, Ishii G, Zenke Y, Neri S,
Aokage K, Hishida T, Yoshida J, Fujii S, Kondo H, Goya T, et al:
Immunophenotypic features of metastatic lymph node tumors to
predict recurrence in N2 lung squamous cell carcinoma. Cancer Sci.
105:905–911. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Lavie D, Ben-Shmuel A, Erez N and
Scherz-Shouval R: Cancer-associated fibroblasts in the single-cell
era. Nat Cancer. 3:793–807. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Zhang X, Zhu R, Yu D, Wang J, Yan Y and Xu
K: Single-cell RNA sequencing to explore cancer-associated
fibroblasts heterogeneity: 'Single' vision for 'heterogeneous'
environment. Cell Prolif. e135922023.Epub ahead of print.
View Article : Google Scholar
|
|
135
|
Li C, Wu H, Guo L, Liu D, Yang S, Li S and
Hua K: Single-cell transcriptomics reveals cellular heterogeneity
and molecular stratification of cervical cancer. Commun Biol.
5:12082022. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Li X, Sun Z, Peng G, Xiao Y, Guo J, Wu B,
Li X, Zhou W, Li J, Li Z, et al: Single-cell RNA sequencing reveals
a pro-invasive cancer-associated fibroblast subgroup associated
with poor clinical outcomes in patients with gastric cancer.
Theranostics. 12:620–638. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Guo W, Zhou B, Yang Z, Liu X, Huai Q, Guo
L, Xue X, Tan F, Li Y, Xue Q, et al: Integrating microarray-based
spatial transcriptomics and single-cell RNA-sequencing reveals
tissue architecture in esophageal squamous cell carcinoma.
EBioMedicine. 84:1042812022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Buechler MB, Pradhan RN, Krishnamurty AT,
Cox C, Calviello AK, Wang AW, Yang YA, Tam L, Caothien R,
Roose-Girma M, et al: Cross-tissue organization of the fibroblast
lineage. Nature. 593:575–579. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Garcia-Recio S, Hinoue T, Wheeler GL,
Kelly BJ, Garrido-Castro AC, Pascual T, De Cubas AA, Xia Y,
Felsheim BM, McClure MB, et al: Multiomics in primary and
metastatic breast tumors from the AURORA US network finds
microenvironment and epigenetic drivers of metastasis. Nat Cancer.
4:128–147. 2023.
|
|
140
|
Liu S, Suhail Y, Novin A, Perpetua L and
Kshitiz: Metastatic transition of pancreatic ductal cell
adenocarcinoma is accompanied by the emergence of pro-invasive
cancer-associated fibroblasts. Cancers (Basel). 14:21972022.
View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Hill M and Tran N: MicroRNAs regulating
MicroRNAs in cancer. Trends Cancer. 4:465–468. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Tkach M and Théry C: Communication by
extracellular vesicles: Where we are and where we need to go. Cell.
164:1226–1232. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Vivacqua A, Muoio MG, Miglietta AM and
Maggiolini M: Differential MicroRNA landscape triggered by
estrogens in cancer associated fibroblasts (CAFs) of primary and
metastatic breast tumors. Cancers (Basel). 11:4122019. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Lee KS, Nam SK, Koh J, Kim DW, Kang SB,
Choe G, Kim WH and Lee HS: Stromal expression of MicroRNA-21 in
advanced colorectal cancer patients with distant metastases. J
Pathol Transl Med. 50:270–277. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Han Q, Tan S, Gong L, Li G, Wu Q, Chen L,
Du S, Li W, Liu X, Cai J and Wang Z: Omental cancer-associated
fibroblast-derived exosomes with low microRNA-29c-3p promote
ovarian cancer peritoneal metastasis. Cancer Sci. 114:1929–1942.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Alsayed RKME, Khan AQ, Ahmad F, Ansari AW,
Alam MA, Buddenkotte J, Steinhoff M, Uddin S and Ahmad A:
Epigenetic regulation of CXCR4 signaling in cancer pathogenesis and
progression. Semin Cancer Biol. 86:697–708. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Petit I, Jin D and Rafii S: The
SDF-1-CXCR4 signaling pathway: A molecular hub modulating
neo-angiogenesis. Trends Immunol. 28:299–307. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Shi Y, Riese DJ II and Shen J: The role of
the CXCL12/CXCR4/CXCR7 chemokine axis in cancer. Front Pharmacol.
11:5746672020. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Dai JM, Sun K, Li C, Cheng M, Guan JH,
Yang LN and Zhang LW: Cancer-associated fibroblasts contribute to
cancer metastasis and apoptosis resistance in human ovarian cancer
via paracrine SDF-1α. Clin Transl Oncol. 25:1606–1616. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Zhang Y, Yang P, Sun T, Li D, Xu X, Rui Y,
Li C, Chong M, Ibrahim T, Mercatali L, et al: miR-126 and miR-126*
repress recruitment of mesenchymal stem cells and inflammatory
monocytes to inhibit breast cancer metastasis. Nat Cell Biol.
15:284–294. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Zhong B, Cheng B, Huang X, Xiao Q, Niu Z,
Chen YF, Yu Q, Wang W and Wu XJ: Colorectal cancer-associated
fibroblasts promote metastasis by up-regulating LRG1 through
stromal IL-6/STAT3 signaling. Cell Death Dis. 13:162021. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Xie H, Lei Y, Mao Y, Lan J, Yang J, Quan H
and Zhang T: FK866 inhibits colorectal cancer metastasis by
reducing NAD+ levels in cancer-associated fibroblasts.
Genes Genomics. 44:1531–1541. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Walterskirchen N, Müller C, Ramos C,
Zeindl S, Stang S, Herzog D, Sachet M, Schimek V, Unger L,
Gerakopoulos V, et al: Metastatic colorectal carcinoma-associated
fibroblasts have immunosuppressive properties related to increased
IGFBP2 expression. Cancer Lett. 540:2157372022. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Mukherjee S, Sakpal A, Mehrotra M, Phadte
P, Rekhi B and Ray P: Homo and heterotypic cellular cross-talk in
epithelial ovarian cancer impart pro-tumorigenic properties through
differential activation of the notch3 pathway. Cancers (Basel).
14:33652022. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Pan X, Zhou J, Xiao Q, Fujiwara K, Zhang
M, Mo G, Gong W and Zheng L: Cancer-associated fibroblast
heterogeneity is associated with organ-specific metastasis in
pancreatic ductal adenocarcinoma. J Hematol Oncol. 14:1842021.
View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Muhl L, Genové G, Leptidis S, Liu J, He L,
Mocci G, Sun Y, Gustafsson S, Buyandelger B, Chivukula IV, et al:
Single-cell analysis uncovers fibroblast heterogeneity and criteria
for fibroblast and mural cell identification and discrimination.
Nat Commun. 11:39532020. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Ewald CY: The matrisome during aging and
longevity: A systems-level approach toward defining matreotypes
promoting healthy aging. Gerontology. 66:266–274. 2020. View Article : Google Scholar
|
|
158
|
Rhim AD, Oberstein PE, Thomas DH, Mirek
ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP,
Tattersall IW, et al: Stromal elements act to restrain, rather than
support, pancreatic ductal adenocarcinoma. Cancer Cell. 25:735–747.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Boyd LNC, Andini KD, Peters GJ, Kazemier G
and Giovannetti E: Heterogeneity and plasticity of
cancer-associated fibroblasts in the pancreatic tumor
microenvironment. Semin Cancer Biol. 82:184–196. 2022. View Article : Google Scholar
|
|
160
|
von Ahrens D, Bhagat TD, Nagrath D, Maitra
A and Verma A: The role of stromal cancer-associated fibroblasts in
pancreatic cancer. J Hematol Oncol. 10:762017. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Deasy SK and Erez N: A glitch in the
matrix: organ-specific matrisomes in metastatic niches. Trends Cell
Biol. 32:110–123. 2022. View Article : Google Scholar
|
|
162
|
Elia I, Rossi M, Stegen S, Broekaert D,
Doglioni G, van Gorsel M, Boon R, Escalona-Noguero C, Torrekens S,
Verfaillie C, et al: Breast cancer cells rely on environmental
pyruvate to shape the metastatic niche. Nature. 568:117–121. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Yuzhalin AE, Gordon-Weeks AN, Tognoli ML,
Jones K, Markelc B, Konietzny R, Fischer R, Muth A, O'Neill E,
Thompson PR, et al: Colorectal cancer liver metastatic growth
depends on PAD4-driven citrullination of the extracellular matrix.
Nat Commun. 9:47832018. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Levental KR, Yu H, Kass L, Lakins JN,
Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, et
al: Matrix crosslinking forces tumor progression by enhancing
integrin signaling. Cell. 139:891–906. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Er EE, Valiente M, Ganesh K, Zou Y,
Agrawal S, Hu J, Griscom B, Rosenblum M, Boire A, Brogi E, et al:
Pericyte-like spreading by disseminated cancer cells activates YAP
and MRTF for metastatic colonization. Nat Cell Biol. 20:966–978.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Che LH, Liu JW, Huo JP, Luo R, Xu RM, He
C, Li YQ, Zhou AJ, Huang P, Chen YY, et al: A single-cell atlas of
liver metastases of colorectal cancer reveals reprogramming of the
tumor microenvironment in response to preoperative chemotherapy.
Cell Discov. 7:802021. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Whatcott CJ, Diep CH, Jiang P, Watanabe A,
LoBello J, Sima C, Hostetter G, Shepard HM, Von Hoff DD and Han H:
Desmoplasia in primary tumors and metastatic lesions of pancreatic
cancer. Clin Cancer Res. 21:3561–3568. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Placencio-Hickok VR, Lauzon M, Moshayedi
N, Guan M, Kim S, Nissen N, Lo S, Pandol S, Larson BK, Gong J, et
al: Hyaluronan heterogeneity in pancreatic ductal adenocarcinoma:
Primary tumors compared to sites of metastasis. Pancreatology.
22:92–97. 2022. View Article : Google Scholar
|
|
169
|
Ueno H, Sekine S, Oshiro T, Kanemitsu Y,
Hamaguchi T, Shida D, Takashima A, Ishiguro M, Ito E, Hashiguchi Y,
et al: Disentangling the prognostic heterogeneity of stage III
colorectal cancer through histologic stromal categorization.
Surgery. 163:777–783. 2018. View Article : Google Scholar
|
|
170
|
Ao T, Kajiwara Y, Yonemura K, Shinto E,
Mochizuki S, Okamoto K, Aosasa S and Ueno H: Prognostic
significance of histological categorization of desmoplastic
reaction in colorectal liver metastases. Virchows Arch.
475:341–348. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Ao T, Kajiwara Y, Yonemura K, Shinto E,
Mochizuki S, Okamoto K, Kishi Y and Ueno H: Morphological
consistency of desmoplastic reactions between the primary
colorectal cancer lesion and associated metastatic lesions.
Virchows Arch. 477:47–55. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Mayorca-Guiliani AE, Madsen CD, Cox TR,
Horton ER, Venning FA and Erler JT: ISDoT: In situ
decellularization of tissues for high-resolution imaging and
proteomic analysis of native extracellular matrix. Nat Med.
23:890–898. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Yang H, Sun B, Fan L, Ma W, Xu K, Hall
SRR, Wang Z, Schmid RA, Peng RW, Marti TM, et al: Multi-scale
integrative analyses identify THBS2+ cancer-associated
fibroblasts as a key orchestrator promoting aggressiveness in
early-stage lung adenocarcinoma. Theranostics. 12:3104–3130. 2022.
View Article : Google Scholar :
|
|
174
|
Irum B, Asif M, Mumtaz B and Aslam N:
Effect of dental proximal restorations on periodontal health in
patients. J Ayub Med Coll Abbottabad. 34(Suppl 1): S987–S990. 2022.
View Article : Google Scholar
|
|
175
|
Machado RB, Aguiar LMS and Silva JMC:
Brazil: Plan for zero vegetation loss in the Cerrado. Nature.
615:2162023. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Dean M, Fojo T and Bates S: Tumour stem
cells and drug resistance. Nat Rev Cancer. 5:275–284. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Brabletz T, Kalluri R, Nieto MA and
Weinberg RA: EMT in cancer. Nat Rev Cancer. 18:128–134. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Belfiore A, Rapicavoli RV, Le Moli R,
Lappano R, Morrione A, De Francesco EM and Vella V: IGF2: A role in
metastasis and tumor evasion from immune surveillance?
Biomedicines. 11:2292023. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Chhabra Y and Weeraratna AT: Fibroblasts
in cancer: Unity in heterogeneity. Cell. 186:1580–1609. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Minchinton AI and Tannock IF: Drug
penetration in solid tumours. Nat Rev Cancer. 6:583–592. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Wong L, Kumar A, Gabela-Zuniga B, Chua J,
Singh G, Happe CL, Engler AJ, Fan Y and McCloskey KE: Substrate
stiffness directs diverging vascular fates. Acta Biomater.
96:321–329. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Engler AJ, Sen S, Sweeney HL and Discher
DE: Matrix elasticity directs stem cell lineage specification.
Cell. 126:677–689. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Ruehle MA, Eastburn EA, LaBelle SA,
Krishnan L, Weiss JA, Boerckel JD, Wood LB, Guldberg RE and Willett
NJ: Extracellular matrix compression temporally regulates
microvascular angiogenesis. Sci Adv. 6:eabb63512020. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Jing X, Yang F, Shao C, Wei K, Xie M, Shen
H and Shu Y: Role of hypoxia in cancer therapy by regulating the
tumor microenvironment. Mol Cancer. 18:1572019. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Alvarez R, Musteanu M, Garcia-Garcia E,
Lopez-Casas PP, Megias D, Guerra C, Muñoz M, Quijano Y, Cubillo A,
Rodriguez-Pascual J, et al: Stromal disrupting effects of
nab-paclitaxel in pancreatic cancer. Br J Cancer. 109:926–933.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Kim H, Samuel S, Lopez-Casas P, Grizzle W,
Hidalgo M, Kovar J, Oelschlager D, Zinn K, Warram J and Buchsbaum
D: SPARC-independent delivery of nab-paclitaxel without depleting
tumor stroma in patient-derived pancreatic cancer xenografts. Mol
Cancer Ther. 15:680–688. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Zhang X, Zeng Y, Zhao L, Xu Q, Miao D and
Yu F: Targeting hepatic stellate cell death to reverse hepatic
fibrosis. Curr Drug Targets. 24:568–583. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Jin H, Lian N, Zhang F, Chen L, Chen Q, Lu
C, Bian M, Shao J, Wu L and Zheng S: Activation of PPARγ/P53
signaling is required for curcumin to induce hepatic stellate cell
senescence. Cell Death Dis. 7:e21892016. View Article : Google Scholar
|
|
189
|
Xia S, Liu Z, Cai J, Ren H, Li Q, Zhang H,
Yue J, Zhou Q, Zhou T, Wang L, et al: Liver fibrosis therapy based
on biomimetic nanoparticles which deplete activated hepatic
stellate cells. J Control Release. 355:54–67. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Zi F, He J, He D, Li Y, Yang L and Cai Z:
Fibroblast activation protein alpha in tumor microenvironment:
Recent progression and implications (review). Mol Med Rep.
11:3203–3211. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Bughda R, Dimou P, D'Souza RR and
Klampatsa A: Fibroblast activation protein (FAP)-targeted CAR-T
cells: Launching an attack on tumor stroma. Immunotargets Ther.
10:313–323. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Claus C, Ferrara C, Xu W, Sam J, Lang S,
Uhlenbrock F, Albrecht R, Herter S, Schlenker R, Hüsser T, et al:
Tumor-targeted 4-1BB agonists for combination with T cell
bispecific antibodies as off-the-shelf therapy. Sci Transl Med.
11:eaav59892019. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Melero I, Tanos T, Bustamante M, Sanmamed
MF, Calvo E, Moreno I, Moreno V, Hernandez T, Martinez Garcia M,
Rodriguez-Vida A, et al: A first-in-human study of the fibroblast
activation protein-targeted, 4-1BB agonist RO7122290 in patients
with advanced solid tumors. Sci Transl Med. 15:eabp92292023.
View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Ballal S, Yadav MP, Kramer V, Moon ES,
Roesch F, Tripathi M, Mallick S, ArunRaj ST and Bal C: A
theranostic approach of [68Ga]Ga-DOTA.SA.FAPi
PET/CT-guided [177Lu]Lu-DOTA. SA.FAPi radionuclide
therapy in an end-stage breast cancer patient: New frontier in
targeted radionuclide therapy. Eur J Nucl Med Mol Imaging.
48:942–944. 2021. View Article : Google Scholar
|
|
195
|
Assadi M, Rekabpour SJ, Jafari E, Divband
G, Nikkholgh B, Amini H, Kamali H, Ebrahimi S, Shakibazad N, Jokar
N, et al: Feasibility and therapeutic potential of 177Lu-fibroblast
activation protein inhibitor-46 for patients with relapsed or
refractory cancers: A preliminary study. Clin Nucl Med.
46:e523–e530. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Baum RP, Schuchardt C, Singh A,
Chantadisai M, Robiller FC, Zhang J, Mueller D, Eismant A, Almaguel
F, Zboralski D, et al: Feasibility, biodistribution, and
preliminary dosimetry in peptide-targeted radionuclide therapy of
diverse adenocarcinomas using 177Lu-FAP-2286:
First-in-humans results. J Nucl Med. 63:415–423. 2022. View Article : Google Scholar :
|
|
197
|
Vallet SD and Ricard-Blum S: Lysyl
oxidases: from enzyme activity to extracellular matrix cross-links.
Essays Biochem. 63:349–364. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Granzow M, Schierwagen R, Klein S,
Kowallick B, Huss S, Linhart M, Mazar IG, Görtzen J, Vogt A,
Schildberg FA, et al: Angiotensin-II type 1 receptor-mediated Janus
kinase 2 activation induces liver fibrosis. Hepatology. 60:334–348.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Takiguchi T, Takahashi-Yanaga F, Ishikane
S, Tetsuo F, Hosoda H, Arioka M, Kitazono T and Sasaguri T:
Angiotensin II promotes primary tumor growth and metastasis
formation of murine TNBC 4T1 cells through the fibroblasts around
cancer cells. Eur J Pharmacol. 909:1744152021. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Murphy JE, Wo JY, Ryan DP, Clark JW, Jiang
W, Yeap BY, Drapek LC, Ly L, Baglini CV, Blaszkowsky LS, et al:
Total neoadjuvant therapy with FOLFIRINOX in combination with
losartan followed by chemoradiotherapy for locally advanced
pancreatic cancer: A phase 2 clinical trial. JAMA Oncol.
5:1020–1027. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Wong KM, Horton KJ, Coveler AL, Hingorani
SR and Harris WP: Targeting the tumor stroma: The biology and
clinical development of pegylated recombinant human hyaluronidase
(PEGPH20). Curr Oncol Rep. 19:472017. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Kudo D, Suto A and Hakamada K: The
development of a novel therapeutic strategy to target hyaluronan in
the extracellular matrix of pancreatic ductal adenocarcinoma. Int J
Mol Sci. 18:6002017. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Ramanathan RK, McDonough SL, Philip PA,
Hingorani SR, Lacy J, Kortmansky JS, Thumar J, Chiorean EG, Shields
AF, Behl D, et al: Phase IB/II randomized study of FOLFIRINOX plus
pegylated recombinant human hyaluronidase versus FOLFIRINOX alone
in patients with metastatic pancreatic adenocarcinoma: SWOG S1313.
J Clin Oncol. 37:1062–1069. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Van Cutsem E, Tempero MA, Sigal D, Oh DY,
Fazio N, Macarulla T, Hitre E, Hammel P, Hendifar AE, Bates SE, et
al: Randomized phase III trial of pegvorhyaluronidase alfa with
nab-paclitaxel plus gemcitabine for patients with hyaluronan-high
metastatic pancreatic adenocarcinoma. J Clin Oncol. 38:3185–3194.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Sakers A, De Siqueira MK, Seale P and
Villanueva CJ: Adipose-tissue plasticity in health and disease.
Cell. 185:419–446. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Koudelka S and Turánek J: Liposomal
paclitaxel formulations. J Control Release. 163:322–334. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Shahriari K, Shen F, Worrede-Mahdi A, Liu
Q, Gong Y, Garcia FU and Fatatis A: Cooperation among heterogeneous
prostate cancer cells in the bone metastatic niche. Oncogene.
36:2846–2856. 2017. View Article : Google Scholar :
|
|
208
|
Nakamura Y, Kinoshita J, Yamaguchi T, Aoki
T, Saito H, Hamabe-Horiike T, Harada S, Nomura S, Inaki N and
Fushida S: Crosstalk between cancer-associated fibroblasts and
immune cells in peritoneal metastasis: Inhibition in the migration
of M2 macrophages and mast cells by Tranilast. Gastric Cancer.
25:515–526. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Suetsugu A, Osawa Y, Nagaki M, Saji S,
Moriwaki H, Bouvet M and Hoffman RM: Imaging the recruitment of
cancer-associated fibroblasts by liver-metastatic colon cancer. J
Cell Biochem. 112:949–953. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Jung Y, Kim JK, Shiozawa Y, Wang J, Mishra
A, Joseph J, Berry JE, McGee S, Lee E, Sun H, et al: Recruitment of
mesenchymal stem cells into prostate tumours promotes metastasis.
Nat Commun. 4:17952013. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Kidd S, Spaeth E, Watson K, Burks J, Lu H,
Klopp A, Andreeff M and Marini FC: Origins of the tumor
microenvironment: Quantitative assessment of adipose-derived and
bone marrow-derived stroma. PLoS One. 7:e305632012. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Tang H, Chu Y, Huang Z, Cai J and Wang Z:
The metastatic phenotype shift toward myofibroblast of
adipose-derived mesenchymal stem cells promotes ovarian cancer
progression. Carcinogenesis. 41:182–193. 2020. View Article : Google Scholar
|
|
213
|
Cho JA, Park H, Lim EH and Lee KW:
Exosomes from breast cancer cells can convert adipose
tissue-derived mesenchymal stem cells into myofibroblast-like
cells. Int J Oncol. 40:130–138. 2012.
|
|
214
|
Karnoub AE, Dash AB, Vo AP, Sullivan A,
Brooks MW, Bell GW, Richardson AL, Polyak K, Tubo R and Weinberg
RA: Mesenchymal stem cells within tumour stroma promote breast
cancer metastasis. Nature. 449:557–563. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Zhang J, Sun D, Fu Q, Cao Q, Zhang H and
Zhang K: Bone mesenchymal stem cells differentiate into
myofibroblasts in the tumor microenvironment. Oncol Lett.
12:644–650. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Bochet L, Lehuédé C, Dauvillier S, Wang
YY, Dirat B, Laurent V, Dray C, Guiet R, Maridonneau-Parini I, Le
Gonidec S, et al: Adipocyte-derived fibroblasts promote tumor
progression and contribute to the desmoplastic reaction in breast
cancer. Cancer Res. 73:5657–5668. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Jotzu C, Alt E, Welte G, Li J, Hennessy
BT, Devarajan E, Krishnappa S, Pinilla S, Droll L and Song YH:
Adipose tissue derived stem cells differentiate into
carcinoma-associated fibroblast-like cells under the influence of
tumor derived factors. Cell Oncol (Dordr). 34:55–67. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Baroni S, Romero-Cordoba S, Plantamura I,
Dugo M, D'Ippolito E, Cataldo A, Cosentino G, Angeloni V, Rossini
A, Daidone MG and Iorio MV: Exosome-mediated delivery of miR-9
induces cancer-associated fibroblast-like properties in human
breast fibroblasts. Cell Death Dis. 7:e23122016. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Arina A, Idel C, Hyjek EM, Alegre ML, Wang
Y, Bindokas VP, Weichselbaum RR and Schreiber H: Tumor-associated
fibroblasts predominantly come from local and not circulating
precursors. Proc Natl Acad Sci USA. 113:7551–7556. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Vicent S, Sayles LC, Vaka D, Khatri P,
Gevaert O, Chen R, Zheng Y, Gillespie AK, Clarke N, Xu Y, et al:
Cross-species functional analysis of cancer-associated fibroblasts
identifies a critical role for CLCF1 and IL-6 in non-small cell
lung cancer in vivo. Cancer Res. 72:5744–5756. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Nair N, Calle AS, Zahra MH, Prieto-Vila M,
Oo AKK, Hurley L, Vaidyanath A, Seno A, Masuda J, Iwasaki Y, et al:
A cancer stem cell model as the point of origin of
cancer-associated fibroblasts in tumor microenvironment. Sci Rep.
7:68382017. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
Sandoval P, Jiménez-Heffernan JA,
Rynne-Vidal Á, Pérez-Lozano ML, Gilsanz Á, Ruiz-Carpio V, Reyes R,
García-Bordas J, Stamatakis K, Dotor J, et al: Carcinoma-associated
fibroblasts derive from mesothelial cells via
mesothelial-to-mesenchymal transition in peritoneal metastasis. J
Pathol. 231:517–531. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
223
|
Zeisberg EM, Potenta S, Xie L, Zeisberg M
and Kalluri R: Discovery of endothelial to mesenchymal transition
as a source for carcinoma-associated fibroblasts. Cancer Res.
67:10123–10128. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
224
|
Xin Y, Li K, Yang M and Tan Y: Fluid shear
stress induces EMT of circulating tumor cells via JNK signaling in
favor of their survival during hematogenous dissemination. Int J
Mol Sci. 21:81152020. View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Kan T, Wang W, Ip PP, Zhou S, Wong AS,
Wang X and Yang M: Single-cell EMT-related transcriptional analysis
revealed intra-cluster heterogeneity of tumor cell clusters in
epithelial ovarian cancer ascites. Oncogene. 39:4227–4240. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
226
|
Yoshimura Y, Suzuki D and Miyahara K:
Measurement accuracy of fat and iron deposits in the liver using
1H-MRS (HISTO). Nihon Hoshasen Gijutsu Gakkai Zasshi.
74:148–153. 2018.In Japanese. View Article : Google Scholar
|
|
227
|
Ringuette Goulet C, Bernard G, Tremblay S,
Chabaud S, Bolduc S and Pouliot F: Exosomes induce fibroblast
differentiation into cancer-associated fibroblasts through TGFbeta
signaling. Mol Cancer Res. 16:1196–1204. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
228
|
Zhang J, Fu L, Yasuda-Yoshihara N,
Yonemura A, Wei F, Bu L, Hu X, Akiyama T, Kitamura F, Yasuda T, et
al: IL-1β derived from mixed-polarized macrophages activates
fibroblasts and synergistically forms a cancer-promoting
microenvironment. Gastric Cancer. 26:187–202. 2023. View Article : Google Scholar
|
|
229
|
Wei LY, Lee JJ, Yeh CY, Yang CJ, Kok SH,
Ko JY, Tsai FC and Chia JS: Reciprocal activation of
cancer-associated fibroblasts and oral squamous carcinoma cells
through CXCL1. Oral Oncol. 88:115–123. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
230
|
Goulet CR, Champagne A, Bernard G, Vandal
D, Chabaud S, Pouliot F and Bolduc S: Cancer-associated fibroblasts
induce epithelial-mesenchymal transition of bladder cancer cells
through paracrine IL-6 signalling. BMC Cancer. 19:1372019.
View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Scognamiglio I, Cocca L, Puoti I, Palma F,
Ingenito F, Quintavalle C, Affinito A, Roscigno G, Nuzzo S,
Chianese RV, et al: Exosomal microRNAs synergistically trigger
stromal fibroblasts in breast cancer. Mol Ther Nucleic Acids.
28:17–31. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
232
|
Qin X, Lu M, Li G, Zhou Y and Liu Z:
Downregulation of tumor-derived exosomal miR-34c induces
cancer-associated fibroblast activation to promote
cholangiocarcinoma progress. Cancer Cell Int. 21:3732021.
View Article : Google Scholar : PubMed/NCBI
|
|
233
|
Zhou X, Yan T, Huang C, Xu Z, Wang L,
Jiang E, Wang H, Chen Y, Liu K, Shao Z and Shang Z: Melanoma
cell-secreted exosomal miR-155-5p induce proangiogenic switch of
cancer-associated fibroblasts via SOCS1/JAK2/STAT3 signaling
pathway. J Exp Clin Cancer Res. 37:2422018. View Article : Google Scholar : PubMed/NCBI
|
|
234
|
Ye B, Duan Y, Zhou M, Wang Y, Lai Q, Yue
K, Cao J, Wu Y, Wang X and Jing C: Hypoxic tumor-derived exosomal
miR-21 induces cancer-associated fibroblast activation to promote
head and neck squamous cell carcinoma metastasis. Cell Signal.
108:1107252023. View Article : Google Scholar : PubMed/NCBI
|
|
235
|
Xu Y, Kuai R, Chu YM, Zhou L, Zhang HQ and
Li J: Hypoxia facilitates the proliferation of colorectal cancer
cells by inducing cancer-associated fibroblast-derived IL6.
Neoplasma. 68:1015–1022. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
236
|
Butti R, Nimma R, Kundu G, Bulbule A,
Kumar TVS, Gunasekaran VP, Tomar D, Kumar D, Mane A, Gill SS, et
al: Tumor-derived osteopontin drives the resident fibroblast to
myofibroblast differentiation through Twist1 to promote breast
cancer progression. Oncogene. 40:2002–2017. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
237
|
Calvo F, Ege N, Grande-Garcia A, Hooper S,
Jenkins RP, Chaudhry SI, Harrington K, Williamson P, Moeendarbary
E, Charras G and Sahai E: Mechanotransduction and YAP-dependent
matrix remodelling is required for the generation and maintenance
of cancer-associated fibroblasts. Nat Cell Biol. 15:637–646. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
238
|
Foster CT, Gualdrini F and Treisman R:
Mutual dependence of the MRTF-SRF and YAP-TEAD pathways in
cancer-associated fibroblasts is indirect and mediated by
cytoskeletal dynamics. Genes Dev. 31:2361–2375. 2017. View Article : Google Scholar
|
|
239
|
Cadamuro M, Nardo G, Indraccolo S,
Dall'olmo L, Sambado L, Moserle L, Franceschet I, Colledan M,
Massani M, Stecca T, et al: Platelet-derived growth factor-D and
Rho GTPases regulate recruitment of cancer-associated fibroblasts
in cholangiocarcinoma. Hepatology. 58:1042–1053. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
240
|
Pietras K, Pahler J, Bergers G and Hanahan
D: Functions of paracrine PDGF signaling in the proangiogenic tumor
stroma revealed by pharmacological targeting. PLoS Med. 5:e192008.
View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Scherz-Shouval R, Santagata S, Mendillo
ML, Sholl LM, Ben-Aharon I, Beck AH, Dias-Santagata D, Koeva M,
Stemmer SM, Whitesell L and Lindquist S: The reprogramming of tumor
stroma by HSF1 is a potent enabler of malignancy. Cell.
158:564–578. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
Ferrari N, Ranftl R, Chicherova I, Slaven
ND, Moeendarbary E, Farrugia AJ, Lam M, Semiannikova M, Westergaard
MCW, Tchou J, et al: Dickkopf-3 links HSF1 and YAP/TAZ signalling
to control aggressive behaviours in cancer-associated fibroblasts.
Nat Commun. 10:1302019. View Article : Google Scholar : PubMed/NCBI
|
|
243
|
Guo Z, Zhang H, Fu Y, Kuang J, Zhao B,
Zhang L, Lin J, Lin S, Wu D and Xie G: Cancer-associated
fibroblasts induce growth and radioresistance of breast cancer
cells through paracrine IL-6. Cell Death Discov. 9:62023.
View Article : Google Scholar : PubMed/NCBI
|
|
244
|
Çermik TF, Ergül N, Yılmaz B and
Mercanoğlu G: Tumor imaging with 68Ga-DOTA-FAPI-04 PET/CT:
Comparison with 18F-FDG PET/CT in 22 different cancer types. Clin
Nucl Med. 47:e333–e339. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Pang Y, Zhao L, Meng T, Xu W, Lin Q, Wu H,
Zhang J, Chen X, Sun L and Chen H: PET imaging of fibroblast
activation protein in various types of cancer using
68Ga-FAP-2286: comparison with 18F-FDG and
68Ga-FAPI-46 in a single-center, prospective study. J
Nucl Med. 64:386–394. 2023. View Article : Google Scholar :
|
|
246
|
Hosein AN, Huang H, Wang Z, Parmar K, Du
W, Huang J, Maitra A, Olson E, Verma U and Brekken RA: Cellular
heterogeneity during mouse pancreatic ductal adenocarcinoma
progression at single-cell resolution. JCI Insight. 5:e1292122019.
View Article : Google Scholar : PubMed/NCBI
|
|
247
|
Neuzillet C, Tijeras-Raballand A, Ragulan
C, Cros J, Patil Y, Martinet M, Erkan M, Kleeff J, Wilson J, Apte
M, et al: Inter- and intra-tumoural heterogeneity in
cancer-associated fibroblasts of human pancreatic ductal
adenocarcinoma. J Pathol. 248:51–65. 2019. View Article : Google Scholar :
|
|
248
|
Lin W, Noel P, Borazanci EH, Lee J, Amini
A, Han IW, Heo JS, Jameson GS, Fraser C, Steinbach M, et al:
Single-cell transcriptome analysis of tumor and stromal
compartments of pancreatic ductal adenocarcinoma primary tumors and
metastatic lesions. Genome Med. 12:802020. View Article : Google Scholar : PubMed/NCBI
|
|
249
|
Sebastian A, Hum NR, Martin KA, Gilmore
SF, Peran I, Byers SW, Wheeler EK, Coleman MA and Loots GG:
Single-cell transcriptomic analysis of tumor-derived fibroblasts
and normal tissue-resident fibroblasts reveals fibroblast
heterogeneity in breast cancer. Cancers (Basel). 12:13072020.
View Article : Google Scholar : PubMed/NCBI
|
|
250
|
Li H, Courtois ET, Sengupta D, Tan Y, Chen
KH, Goh JJL, Kong SL, Chua C, Hon LK, Tan WS, et al: Reference
component analysis of single-cell transcriptomes elucidates
cellular heterogeneity in human colorectal tumors. Nat Genet.
49:708–718. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
251
|
Peng Z, Ye M, Ding H, Feng Z and Hu K:
Spatial transcriptomics atlas reveals the crosstalk between
cancer-associated fibroblasts and tumor microenvironment components
in colorectal cancer. J Transl Med. 20:3022022. View Article : Google Scholar : PubMed/NCBI
|
|
252
|
Lambrechts D, Wauters E, Boeckx B, Aibar
S, Nittner D, Burton O, Bassez A, Decaluwé H, Pircher A, Van den
Eynde K, et al: Phenotype molding of stromal cells in the lung
tumor microenvironment. Nat Med. 24:1277–1289. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
253
|
Hornburg M, Desbois M, Lu S, Guan Y, Lo
AA, Kaufman S, Elrod A, Lotstein A, DesRochers TM, Munoz-Rodriguez
JL, et al: Single-cell dissection of cellular components and
interactions shaping the tumor immune phenotypes in ovarian cancer.
Cancer Cell. 39:928–944.e6. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
254
|
Izar B, Tirosh I, Stover EH, Wakiro I,
Cuoco MS, Alter I, Rodman C, Leeson R, Su MJ, Shah P, et al: A
single-cell landscape of high-grade serous ovarian cancer. Nat Med.
26:1271–1279. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
255
|
Zhang M, Yang H, Wan L, Wang Z, Wang H, Ge
C, Liu Y, Hao Y, Zhang D, Shi G, et al: Single-cell transcriptomic
architecture and intercellular crosstalk of human intrahepatic
cholangiocarcinoma. J Hepatol. 73:1118–1130. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
256
|
Davidson S, Efremova M, Riedel A, Mahata
B, Pramanik J, Huuhtanen J, Kar G, Vento-Tormo R, Hagai T, Chen X,
et al: Single-cell RNA sequencing reveals a dynamic stromal niche
that supports tumor growth. Cell Rep. 31:1076282020. View Article : Google Scholar : PubMed/NCBI
|
|
257
|
Chen Z, Zhou L, Liu L, Hou Y, Xiong M,
Yang Y, Hu J and Chen K: Single-cell RNA sequencing highlights the
role of inflammatory cancer-associated fibroblasts in bladder
urothelial carcinoma. Nat Commun. 11:50772020. View Article : Google Scholar : PubMed/NCBI
|
|
258
|
Kürten CHL, Kulkarni A, Cillo AR, Santos
PM, Roble AK, Onkar S, Reeder C, Lang S, Chen X, Duvvuri U, et al:
Investigating immune and non-immune cell interactions in head and
neck tumors by single-cell RNA sequencing. Nat Commun. 12:73382021.
View Article : Google Scholar : PubMed/NCBI
|