Introduction
According to the World Health Organization
classification system for thyroid tumors, papillary thyroid
microcarcinoma (PTMC) is defined as a papillary thyroid carcinoma
(PTC) measuring ≤10 mm in its greatest dimension (1). The occurrence of PTMC is on the
increase worldwide (2–4), along with the frequent application of
neck ultrasonography (US) (5,6).
PTMC is generally characterized by an indolent clinical course and
has an excellent prognosis, with a disease-specific mortality of
<0.5% (6). However, certain
PTMC cases were found to be clinically aggressive (6,7).
According to the observations of Sugitani et al (7), PTMC patients with bulky lymph node
metastases or extrathyroidal invasion were at the highest risk for
a cancer-specific fatal outcome. Those observations suggested that
there is a group of PTMCs that have already acquired highly
malignant potential. However, the basic mechanism underlying the
development of aggressive characteristics in these tumors has not
yet been identified.
The reported risk factors for PTMC recurrence were
shown to be male gender (8,9),
extent of primary surgery (10),
presence of lymph node metastases at initial diagnosis (3,8–12),
tumor multifocality (3,8,12)
and capsular invasion (9,11–14).
Furthermore, male gender, tumor multifocality and capsular invasion
are considered to be risk factors characteristic of lymph node
metastasis (13,15). Several studies reported that the
presence of clinical lymph node metastasis in PTMC was one of the
most important prognostic indicators, whereas others demonstrated
that pathological lymph node metastasis identified following
prophylactic dissection did not significantly affect patient
prognosis. Pathological lymph node metastasis from PTMC was found
in a range of 26–56% (15–20). The reason(s) for the difference
between clinical and pathological lymph node metastasis have not
been fully elucidated.
In Japan, thyroid function-preserving surgery with
prophylactic lymph node dissection is considered to be the standard
procedure for PTMC. Postoperative follow-up with surgeon-performed
US, without radioactive iodine ablation (RIA) or
thyroid-stimulating hormone (TSH) suppression, is widely applied as
the standard management, due to the strict regulations on
radioisotope use, the shortage of institutes that perform
radioiodine therapy and the difficulties in restricting iodine
intake in the daily diet (21).
Therefore, we were able to enroll a number of PTMC patients who
were diagnosed with pathological lymph node metastasis, with a long
follow-up period.
The required steps for cancer cells to form
metastases are escape from the primary tumor, active migration
toward the vasculature and survival within the systemic
circulation. To successfully undertake these steps, cancer cells
may alter their characteristics from an epithelial- to a
mesenchymal-like form (epithelial-to-mesenchymal transition; EMT)
(22). E-cadherin is a well-known
cellular adhesion molecule in epithelial cells and is known to be
lost during the process of EMT. E-cadherin expression is commonly
observed in differentiated thyroid cancer (23–27)
and loss of its expression was reported to be an independent
prognostic factor for these tumors (27).
In the present study, we investigated the expression
of E-cadherin and Ki-67-index (markers for EMT and cell
proliferation, respectively) in PTMC cases. The results
demonstrated that loss of E-cadherin expression is correlated with
lymph node metastasis, although re-expression of E-cadherin was
commonly detected in the metastatic foci, without observed
acceleration of proliferation, suggesting that the metastatic
cancer cells in the lymph nodes exhibit basically indolent
characteristics, with an innate malignant potential.
Patients and methods
Patients
A consecutive series of 93 patients with PTMC who
were surgically treated in our institute between 2000 and 2010 was
investigated (Table I). The
patients with incidental cancer found following surgery or
concomitant multiple lesions >1 cm in diameter were excluded
from this study. All patients were diagnosed with PTC prior to
surgery by fine-needle aspiration cytology. The postoperative
pathological examination confirmed the absence of a poorly
differentiated carcinoma component. The cases included 10 male and
83 female patients, with a median age of 55 years (range, 24–80
years). A total of 66, 5 and 22 patients underwent lobectomy,
subtotal, or total thyroidectomy, respectively. All patients
underwent lymph node dissection, including at least the central
compartment. A total of 17 patients underwent therapeutic lateral
lymph node dissection. Ipsilateral and bilateral compartment
dissection was performed in 72 and 9 patients, respectively.
Pathological nodal involvement was detected in 57 (61.3%) of the
patients, 26 patients (28.0%) had nodal metastasis in the central
compartment only and 31 (33.3%) had metastatic lymph nodes in the
lateral compartment.
 | Table ICharacteristics of the study
population: patients with papillary microcarcinoma
investigated. |
Table I
Characteristics of the study
population: patients with papillary microcarcinoma
investigated.
| Category | No. of patients | % |
|---|
| Gender
(male:female) | 10:83 | - |
| Age at operation,
years | 24–80; median,
55 | - |
| Extent of
surgery |
| Lobectomy | 66 | 71.0 |
| Subtotal Tx | 5 | 5.4 |
| Total Tx | 22 | 23.7 |
| Extent of
dissection |
| Central | 12 | 12.9 |
| Lateral |
| Ipsilateral | 72 | 77.4 |
| Bilateral | 9 | 9.7 |
RIA and TSH suppression were performed in 11 and 10
patients, respectively, including 1 patient with lung metastasis,
whereas 6 patients received both treatments. All patients were
followed-up at our institute for 30–136 months (median, 78 months)
by annual US and thyroid function tests. Iodine scintigraphy or
computed tomography were performed when considered necessary. Two
patients had a recurrence in the lymph nodes at the ipsilateral
submandibular compartment and required additional dissection. No
other patients developed lymph node or distant metastases.
Immunohistochemistry
The 93 primary tumors and the metastatic lesions in
the lymph nodes from 57 patients were immunohistochemically stained
as described previously (28).
Briefly, the specimens were fixed in 10% formaldehyde solution and
embedded in paraffin. The specimens were then cut in 4-μm sections
and deparaffinized in xylene. The tissues were heated for 20 min at
105°C by autoclave in Target Retrieval solution (Dako, Carpinteria,
CA, USA). Following blocking of the endogenous peroxidase activity,
the sections were incubated in normal goat serum. The M3612 and
M7240 primary antibodies (DakoCytomation, Glostrup, Denmark) were
used to detect E-cadherin and Ki-67, respectively. The tissue
sections were incubated with each antibody for 60 min at room
temperature or overnight at 4°C, followed by incubation with a
secondary antibody and treatment with streptavidin-peroxidase
reagent [Histofine SAB-PO (M) kit; Nichirei, Tokyo, Japan].
Diaminobenzidine was added as a chromogen, followed by
counterstaining with Mayer’s hematoxylin.
The specific immune reactivity of E-cadherin was
detected on the membranous surface of the cancer cells. The
membranous staining of the follicular cells in adjacent normal
thyroid tissue was used as positive control. Positive staining was
defined as >10% of the cancer cells showing specific immune
reactivity at the center of the tumor. Seven tumors were surrounded
by a thick fibrous capsule and the immune reactivity of E-cadherin
at the invasive front was investigated in the remaining 86 tumors.
The invasive front was defined as the interface (<0.1 cm)
between the tumor and the adjacent non-neoplastic tissue (29).
The Ki-67 index was defined as the percentage of
cancer cells with positive nuclear staining for Ki-67.
Statistical analysis
Statistical analysis was performed using SPSS 13.0
statistical software (SPSS, Inc., Chicago, IL, USA). The
Chi-squared test was used to compare the differences in the
positivity rate for immunostaining and the clinicopathological
factors and P<0.05 was considered to indicate a statistically
significant difference.
Results
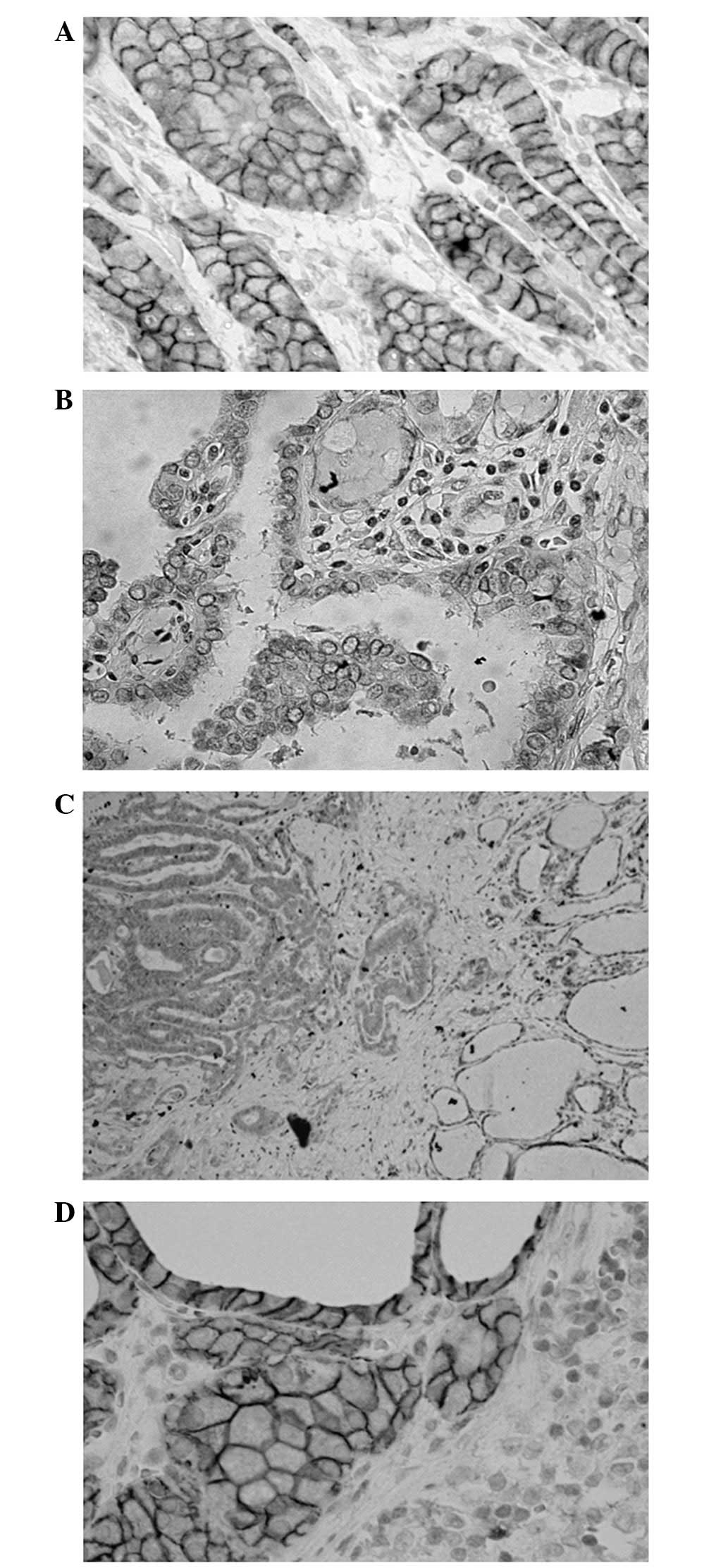
A total of 73 of the 93 tumors (78.5%) exhibited
specific membranous staining for E-cadherin (Fig. 1). E-cadherin expression was
detected in the 12 smaller tumors (≤5 mm) and was significantly
more commonly expressed in the smaller compared with the 81 larger
tumors. There was no observed correlation between E-cadherin
expression and gender, age, or other pathological factors,
including nodal involvement (Table
II).
 | Table IIAssociation of clinicopathological
characteristics of the patients with E-cadherin expression and
Ki-67 index of the tumor. |
Table II
Association of clinicopathological
characteristics of the patients with E-cadherin expression and
Ki-67 index of the tumor.
| | E-cadherin
expression | | | |
|---|
| |
| | | |
|---|
|
Characteristics | n | (−) | (+) | % | P-value | Ki-67 index
(%) |
|---|
| Gender |
| Male | 10 | 1 | 9 | 90.0 | 0.317 | 1.19 |
| Female | 83 | 19 | 64 | 77.1 | | 1.28 |
| Age at operation,
years |
| <45 | 23 | 7 | 16 | 69.6 | 0.230 | 1.44 |
| ≥45 | 70 | 13 | 57 | 81.4 | | 1.21 |
| Tumor diameter,
mm |
| 1–5 | 12 | 0 | 12 | 100.0 | 0.044 | 1.67 |
| 6–10 | 81 | 20 | 61 | 75.3 | | 1.29 |
| Capsular
invasion |
| Negative | 56 | 13 | 43 | 76.8 | 0.622 | 1.39 |
| Positive | 37 | 7 | 30 | 81.1 | | 1.05 |
| pT |
| 1a | 56 | 13 | 43 | 76.8 | 0.622 | 1.39 |
| 3 | 35 | 7 | 28 | 80.0 | | 1.07 |
| 4 | 2 | 0 | 2 | 100.0 | | 0.50 |
| pN |
| 0 | 36 | 9 | 27 | 75.0 | 0.514 | 1.31 |
| 1a | 26 | 6 | 20 | 76.9 | | 1.74 |
| 1b | 31 | 5 | 26 | 83.9 | | 0.88 |
| M |
| 0 | 92 | 20 | 72 | 78.3 | 0.785 | 1.27 |
| 1 | 1 | 0 | 1 | 100.0 | - | |
| pStage |
| I | 39 | 11 | 28 | 71.8 | 0.181 | 1.24 |
| II | 1 | 0 | 1 | 100.0 | - | |
| III | 29 | 7 | 22 | 75.9 | | 1.63 |
| IV | 24 | 2 | 22 | 91.7 | | 0.89 |
| E-cadherin |
| Negative | - | - | - | - | - | 2.27 (1.00a) |
| Positive | - | - | - | - | | 1.09 |
| Total | 93 | 20 | 73 | 78.4 | | 1.27 |
A total of 17 (25.4%) of the 67 evaluable
E-cadherin-positive tumors had lost E-cadherin expression at the
invasive front. By contrast, no E-cadherin-negative tumor gained
its expression at the invasive front. Therefore, E-cadherin
expression was significantly less commonly found at the invasive
front compared to the center of the tumor (58.1%, P<0.01,
Table III). Of the 17 patients
with tumors that had lost E-cadherin expression at the invasive
front, 12 (70.6%) presented with nodal involvement. This frequency
of nodal involvement was higher compared to that in cases that
retained E-cadherin expression at the invasive front (28/50; 56.0%)
or had not expressed E-cadherin in the primary tumor (11/19;
57.9%).
 | Table IIIE-cadherin expression in the tumor
and comparison of expression at the center with that at the
invasive front of the tumor. |
Table III
E-cadherin expression in the tumor
and comparison of expression at the center with that at the
invasive front of the tumor.
| At the invasive
front | | | |
|---|
|
| | | |
|---|
| At the center | Negative (%) | Positive (%) | Subtotal (%) | Encapsulated
tumors | Total (%) |
|---|
| Negative | 19 | 0 | 19 | 1 | 20 (21.5) |
| Positive | 17 | 50 | 67 | 6 | 73 (78.5) |
| Total | 36 (41.9) | 50 (58.1) | 86 (100) | 7 | 93 (100) |
E-cadherin expression was frequently found in the
metastatic foci in the involved lymph nodes (49 of 57 nodes,
86.0%). Ten of the 11 cases with E-cadherin-negative tumors
exhibited E-cadherin expression in the metastatic foci in the
involved lymph nodes. There was no correlation between the
E-cadherin expression status at the center of the primary tumor and
that at the metastatic foci. However, there was a positive
correlation between the E-cadherin expression status at the
invasive front and that at the metastatic foci (P=0.024, Table IV). A total of 8 lymph node
metastatic foci did not express E-cadherin. Although one of these
lesions recurred in the neck, no remarkable clinical
characteristics were observed in the other cases. Five of these 8
cases (62.5%) exhibited loss of E-cadherin expression at the
invasive front of the primary tumor. The rate of
E-cadherin-negative metastatic foci was significantly higher among
cases in which the tumor had lost E-cadherin expression at the
invasive front compared to those in which its expression at the
invasive front of the primary tumor was retained (Table V, P<0.005).
 | Table IVCorrelation between E-cadherin
expression in the tumor and that in the metastatic foci in the
involved lymph nodes. |
Table IV
Correlation between E-cadherin
expression in the tumor and that in the metastatic foci in the
involved lymph nodes.
| In the metastatic
lymph nodes | | |
|---|
|
| | |
|---|
| In the primary
tumor | Negative (%) | Positive (%) | Total (%) | P-value |
|---|
| At the center | 8 (14.0) | 49 (86.0) | 57 (100) | |
| Negative | 1 | 10 | 11 (19.3) | 0.538 |
| Positive | 7 | 39 | 46 (80.7) | |
| At the invasive
front | 8 (14.0) | 49 (86.0) | 57 (100) | |
| Negative | 6 | 17 | 23 (40.3) | 0.024 |
| Positive | 1 | 28 | 29 (50.9) | |
| Encapsulated | 1 | 4 | 5 (8.8) | |
 | Table VCorrelation between loss of
E-cadherin expression at the invasive front of the tumor and at the
metastatic foci in the involved lymph nodes. |
Table V
Correlation between loss of
E-cadherin expression at the invasive front of the tumor and at the
metastatic foci in the involved lymph nodes.
| In the primary
tumor | In the metastatic
lymph nodes | |
|---|
|
| |
|---|
| At the center | At the invasive
front | Negative (%) | Positive (%) | Total (%) |
|---|
| Negative | Negative | 1 | 10 | 11 (19.3) |
| Positive | 0 | 0 | 0 |
| Positive | Negative | 5a | 7 | 12 (21.1) |
| Positive | 1 | 28 | 29 (50.9) |
| Encapsulated | 1 | 4 | 5 (8.8) |
| Total | | 8 (41.9) | 49 (58.1) | 57 (100) |
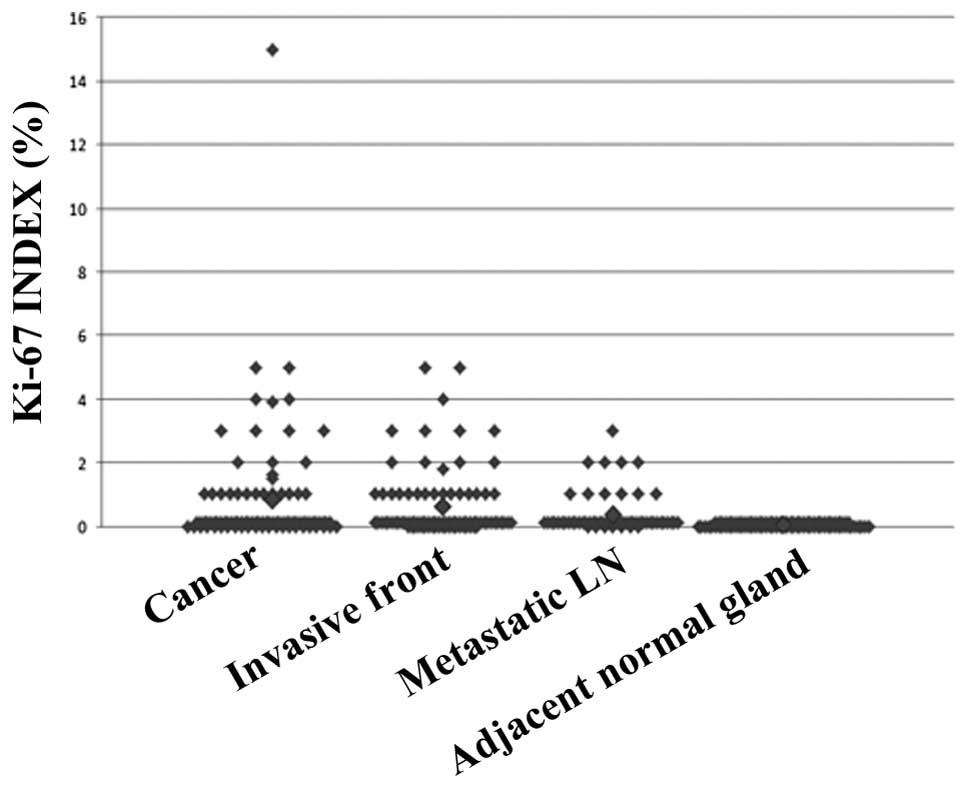
The Ki-67 index ranged between 0 and 15% in the
tumors, with only one primary tumor scoring >5%. Thus, the Ki-67
index was almost universally ≤5% in the tumors and did not
demonstrate any significant differences according to the
clinicopathological characteristics of the patients or the
E-cadherin expression of the tumors (Table II). There was no difference in the
Ki-67 index at the invasive front (mean ± standard deviation,
1.03±0.86%) compared to that at the center of the tumor
(2.27±4.29%). The Ki-67 index in the metastatic foci was
universally ≤3% (0.83±0.83%) (Fig.
2). Two cases that developed recurrence during the follow-up
period did not exhibit high Ki-67 indices (<1%). The only
patient with a Ki-67 index of 15% had a single 6 mm-diameter tumor,
without capsular invasion (T1a, N1a, M0, stage III) and remains
alive and disease-free for >5 years.
Discussion
Total thyroidectomy followed by RIA is often
performed as initial treatment for patients with PTMC (8,30).
However, there has been accumulating information justifying a less
invasive treatment for PTMC, due to its excellent prognosis
following less extensive surgery (4,16,17,31–33),
or even observation without surgery (34,35).
Indeed, only a few fatal PTMC cases have been recorded among a
small proportion of high-risk patients. The optimal management
strategy for patients with PTMC should be further investigated
(32,36), as there is lack of sufficient
information regarding the basic characteristics of PTMC.
In the present study, we detected frequent and
stable expression of E-cadherin in PTMCs. These results are in
accordance with those of previous studies investigating E-cadherin
expression in PTCs of all stages (23–27).
Certain studies demonstrated a correlation between the loss of
E-cadherin expression and disease progression or poorer prognosis
in PTC (27,29); however, the results of the present
study did not verify the clinical significance of E-cadherin
expression in PTMC. The majority of PTMCs exhibited low Ki-67
indices, suggesting a low level of proliferation. There were no
cases with fatal outcome or highest-risk factors for
cancer-specific mortality. However, it may be necessary to include
aggressive PTMC cases in future studies, in order to determine the
clinical significance of the loss of E-cadherin expression,
although such cases are rare.
In a quarter of the cases with E-cadherin-positive
tumors included in the present study, we observed a decrease in
E-cadherin expression at the invasive front. This phenomenon was
also reported by Liu et al (29) in larger PTCs. The authors of that
study also demonstrated that E-cadherin loss was associated with a
loss of cohesiveness and polarity, which was similar to our
findings. These phenotypical and morphological changes are
characteristic of EMT (29).
Furthermore, we observed that the tumors that had lost E-cadherin
expression at the invasive front, commonly presented with lymph
node involvement, suggesting clinical characteristics of EMT. It is
therefore indicated that, even in small PTMCs, the process of
cancer cell dispersion has already been initiated and parts of the
tumor may have acquired aggressive characteristics.
It was also observed that E-cadherin was frequently
re-expressed in the cancer cells that formed metastatic foci in the
involved lymph nodes. A similar observation was described as the
‘re-expression of E-cadherin’ in a previous study investigating PTC
and follicular carcinoma of all stages (27). According to recent findings, this
re-expression step of E-cadherin is considered to represent a
mesenchymal-to-epithelial transformation (MET), the reversal of
EMT. This phenotypical reversal is considered to be a step toward
creating suitable conditions for cancer cells under which they may
survive and form metastatic foci within an environment other than
that of the primary site (37).
Re-expression of E-cadherin in metastatic lymph nodes was commonly
observed in patients with E-cadherin-negative primary PTMC in the
present study, suggesting that MET is crucial for the formation of
metastatic lesions. There was no upregulation of proliferative
activity at the metastatic site, as demonstrated by the low Ki-67
indices in these cancer cells, indicating that the majority of the
PTMC metastatic foci in the involved lymph nodes exhibited an
indolent phenotype, similar to that of the primary site.
The loss of E-cadherin expression was one of several
profiles that indicated phenotypical characteristics suggesting EMT
in PTC (38). Several other
factors are also known to be involved in this process (39). The expression of transforming
growth factor-β (TGF-β) in PTMC was shown to be associated with
high proliferative potential and clinically aggressive
characteristics (14). A previous
study by Knauf et al (40)
suggested that PTC with B-raf mutation has the potential to acquire
aggressive characteristics through EMT by the stimulation of TGF-β.
B-raf mutations are frequently found in PTMCs and are associated
with distinctive morphology and aggressive behaviour (12,41).
It is hypothesized that a certain type of
stimulation may irreversibly alter the phenotype of cancer cells
when they have already acquired the ability to transform. RIA may
be effective in eradicating cancer cells in metastatic lymph nodes,
due to their characteristics regarding iodine uptake (42). However, the indication and efficacy
of RIA in low-risk PTMC cases remains questionable (4,43).
We still need to determine how indolent PTMC cells respond to
stimulation inducing cell proliferation, by TSH or other factors
that induce EMT, prior to the application of RIA in low-risk
patients.
In conclusion, this study demonstrated that cancer
cells in the metastatic lymph nodes exhibited indolent
characteristics, similar to those of the primary PTMC. However, the
metastatic cancer cells may have already completed the processes of
EMT and MET, suggesting an innate malignant potential. Further
studies are required to identify the trigger that initiates the
change of indolent PTMC cancer cells to the aggressive
phenotype.
Acknowledgements
This study was supported in part by a Grant-in-Aid
for Scientific Research (Kakenhi no. 25461992).
References
|
1
|
LiVolsi VA, Albores-Saavedra J, Asa SL, et
al: Papillary carcinoma. World Health Organization Classification
of Tumours: Pathology and Genetics. Tumours of the Endocrine
Organs. De Lellis RA, Lloyd RV, Heitz PU and Eng C: 8. IARC Press
International Agency for Research on Cancer; Lyon: pp. 57–66.
2004
|
|
2
|
Leenhardt L, Grosclaude P and
Chérié-Challine L; Thyroid Cancer Committee. Increased incidence of
thyroid carcinoma in France: a true epidemic or thyroid nodule
management effects? Report from the French Thyroid Cancer
Committee. Thyroid. 14:1056–1060. 2004. View Article : Google Scholar
|
|
3
|
Chow SM, Law SC, Chan JK, et al: Papillary
microcarcinoma of the thyroid - Prognostic significance of lymph
node metastasis and multifocality. Cancer. 98:31–40. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hay ID, Hutchinson ME, Gonzalez-Losada T,
et al: Papillary thyroid microcarcinoma: a study of 900 cases
observed in a 60-year period. Surgery. 144:980–988. 2008.PubMed/NCBI
|
|
5
|
Karatzas T, Vasileiadis I, Kapetanakis S,
et al: Risk factors contributing to the difference in prognosis for
papillary versus micropapillary thyroid carcinoma. Am J Surg.
206:586–593. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Roti E, degli Uberti EC, Bondanelli M and
Braverman LE: Thyroid papillary microcarcinoma: a descriptive and
meta-analysis study. Eur J Endocrinol. 159:659–673. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sugitani I, Toda K, Yamada K, et al: Three
distinctly different kinds of papillary thyroid microcarcinoma
should be recognized: our treatment strategies and outcomes. World
J Surg. 34:1222–1231. 2010. View Article : Google Scholar
|
|
8
|
Buffet C, Golmard JL, Hoang C, et al:
Scoring system for predicting recurrences in patients with
papillary thyroid microcarcinoma. Eur J Endocrinol. 167:267–275.
2012.PubMed/NCBI
|
|
9
|
Riss JC, Peyrottes I, Chamorey E, et al:
Prognostic impact of tumour multifocality in thyroid papillary
microcarcinoma based on a series of 160 cases. Eur Ann
Otorhinolaryngol Head Neck Dis. 129:175–178. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hay ID, Grant CS, van Heerden JA, et al:
Papillary thyroid microcarcinoma: a study of 535 cases observed in
a 50-year period. Surgery. 112:1139–1147. 1992.PubMed/NCBI
|
|
11
|
Pisanu A, Reccia I, Nardello O and
Uccheddu A: Risk factors for nodal metastasis and recurrence among
patients with papillary thyroid microcarcinoma: differences in
clinical relevance between nonincidental and incidental tumors.
World J Surg. 33:460–468. 2009. View Article : Google Scholar
|
|
12
|
Zheng X, Wei S, Han Y, et al: Papillary
microcarcinoma of the thyroid: clinical characteristics and
BRAF(V600E) mutational status of 977 cases. Ann Surg Oncol.
20:2266–2273. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gulben K, Berberoglu U, Celen O and Mersin
HH: Incidental papillary microcarcinoma of the thyroid - factors
affecting lymph node metastasis. Langenbecks Arch Surg. 393:25–29.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sugitani I, Yanagisawa A, Shimizu A, Kato
M and Fujimoto Y: Clinicopathologic and immunohistochemical studies
of papillary thyroid microcarcinoma presenting with cervical
lymphadenopathy. World J Surg. 22:731–737. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang L, Wei WJ, Ji QH, et al: Risk
factors for neck nodal metastasis in papillary thyroid
microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab.
97:1250–1257. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hyun SM, Song HY, Kim SY, et al: Impact of
combined prophylactic unilateral central neck dissection and
hemithyroidectomy in patients with papillary thyroid
microcarcinoma. Ann Surg Oncol. 19:591–596. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Caliskan M, Park JH, Jeong JS, et al: Role
of prophylactic ipsilateral central compartment lymph node
dissection in papillary thyroid microcarcinoma. Endocr J.
59:305–311. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zeng RC, Li Q, Lin KL, et al: Predicting
the factors of lateral lymph node metastasis in papillary
microcarcinoma of the thyroid in eastern China. Clin Transl Oncol.
14:842–847. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhou YL, Gao EL, Zhang W, et al: Factors
predictive of papillary thyroid micro-carcinoma with bilateral
involvement and central lymph node metastasis: a retrospective
study. World J Surg Oncol. 10:672012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim BY, Jung CH, Kim JW, et al: Impact of
clinicopathologic factors on subclinical central lymph node
metastasis in papillary thyroid microcarcinoma. Yonsei Med J.
53:924–930. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sugitani I and Fujimoto Y: Management of
low-risk papillary thyroid carcinoma: unique conventional policy in
Japan and our efforts to improve the level of evidence. Surg Today.
40:199–215. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kalluri R and Weinberg RA: The basics of
epithelial-mesenchymal transition. J Clin Invest. 119:1420–1428.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Batistatou A, Charalabopoulos K, Nakanishi
Y, et al: Differential expression of dysadherin in papillary
thyroid carcinoma and microcarcinoma: correlation with E-cadherin.
Endocr Pathol. 19:197–202. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Choi YL, Kim MK, Suh JW, et al:
Immunoexpression of HBME-1, high molecular weight cytokeratin,
cytokeratin 19, thyroid transcription factor-1, and E-cadherin in
thyroid carcinomas. J Korean Med Sci. 20:853–859. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Naito A, Iwase H, Kuzushima T, Nakamura T
and Kobayashi S: Clinical significance of E-cadherin expression in
thyroid neoplasms. J Surg Oncol. 76:176–180. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kapran Y, Ozbey N, Molvalilar S, et al:
Immunohistochemical detection of E-cadherin, alpha- and
beta-catenins in papillary thyroid carcinoma. J Endocrinol Invest.
25:578–585. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
von Wasielewski R, Rhein A, Werner M, et
al: Immunohistochemical detection of E-cadherin in differentiated
thyroid carcinomas correlates with clinical outcome. Cancer Res.
57:2501–2507. 1997.PubMed/NCBI
|
|
28
|
Kashiwagi S, Yashiro M, Takashima T, et
al: c-Kit expression as a prognostic molecular marker in patients
with basal-like breast cancer. Br J Surg. 100:490–496. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu Z, Kakudo K, Bai Y, et al: Loss of
cellular polarity/cohesiveness in the invasive front of papillary
thyroid carcinoma, a novel predictor for lymph node metastasis;
possible morphological indicator of epithelial mesenchymal
transition. J Clin Pathol. 64:325–329. 2011. View Article : Google Scholar
|
|
30
|
Pelizzo MR, Boschin IM, Toniato A, et al:
Natural history, diagnosis, treatment and outcome of papillary
thyroid microcarcinoma (PTMC): a mono-institutional 12-year
experience. Nucl Med Commun. 25:547–552. 2004.PubMed/NCBI
|
|
31
|
Lee J, Park JH, Lee CR, Chung WY and Park
CS: Long-term outcomes of total thyroidectomy versus thyroid
lobectomy for papillary thyroid microcarcinoma: comparative
analysis after propensity score matching. Thyroid. 23:1408–1415.
2013. View Article : Google Scholar
|
|
32
|
Pacini F: Management of papillary thyroid
microcarcinoma: primum non nocere! J Clin Endocrinol Metab.
98:1391–1393. 2013.PubMed/NCBI
|
|
33
|
Ito Y, Tomoda C, Uruno T, et al: Papillary
microcarcinoma of the thyroid: how should it be treated? World J
Surg. 28:1115–1121. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ito Y, Uruno T, Nakano K, et al: An
observation trial without surgical treatment in patients with
papillary microcarcinoma of the thyroid. Thyroid. 13:381–387. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sugitani I and Fujimoto Y: Symptomatic
versus asymptomatic papillary thyroid microcarcinoma: a
retrospective analysis of surgical outcome and prognostic factors.
Endocr J. 46:209–216. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yu XM, Wan Y, Sippel RS and Chen H: Should
all papillary thyroid microcarcinomas be aggressively treated? An
analysis of 18,445 cases. Ann Surg. 254:653–660. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hugo H, Ackland ML, Blick T, et al:
Epithelial - mesenchymal and mesenchymal - epithelial transitions
in carcinoma progression. J Cell Physiol. 213:374–383. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Vasko V, Espinosa AV, Scouten W, et al:
Gene expression and functional evidence of
epithelial-to-mesenchymal transition in papillary thyroid carcinoma
invasion. Proc Natl Acad Sci USA. 104:2803–2808. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zeisberg M and Neilson EG: Biomarkers for
epithelial-mesenchymal transitions. J Clin Invest. 119:1429–1437.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
40
|
Knauf JA, Sartor MA, Medvedovic M, et al:
Progression of BRAF-induced thyroid cancer is associated with
epithelial-mesenchymal transition requiring concomitant MAP kinase
and TGFβ signaling. Oncogene. 30:3153–3162. 2011.PubMed/NCBI
|
|
41
|
Virk RK, Van Dyke AL, Finkelstein A, et
al: BRAFV600E mutation in papillary thyroid microcarcinoma: a
genotype-phenotype correlation. Mod Pathol. 26:62–70. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
So YK, Son YI, Baek CH, et al: Expression
of sodium-iodide symporter and TSH receptor in subclinical
metastatic lymph nodes of papillary thyroid microcarcinoma. Ann
Surg Oncol. 19:990–995. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kim HJ, Kim NK, Choi JH, et al:
Radioactive iodine ablation does not prevent recurrences in
patients with papillary thyroid microcarcinoma. Clin Endocrinol
(Oxf). 78:614–620. 2012. View Article : Google Scholar : PubMed/NCBI
|