Introduction
Trichilemmal carcinoma (TC) is a rare malignancy,
commonly located on the scalp, forehead and neck, trunk or the
upper extremities (1). It is known
to develop from the external root sheath of the hair follicle,
affecting predominantly the sun-exposed areas of the skin.
(1). TC is also characterized by
an indolent clinical course, and is usually considered to be
curable following surgical treatment in the form of wide surgical
excision (2). TC clinical
characteristics are usually not taken into consideration, while an
onset of an abrupt growth phase leads to medical evaluation in the
late stage of disease progression (3). A limited number of studies
investigating TC are available, thus, the tumor behavior and
prognosis are difficult to be estimated (4). Although TC has a low metastatic
potential and does not usually recur, no long-term follow-up data
have been collected on patients with this neoplasm, rendering deep
invasion and local recurrence possible (5). In addition, no optimal treatment for
TC with metastasis has been suggested and no established
chemotherapy regimen for metastatic TC has been reported in the
medical literature. Therefore, TC patients with metastasis have a
poor prognosis (6). Although
supported by limited data, the risk of recurrence and lymph node
metastasis is potentially similar to that of squamous cell
carcinoma (4).
However, since most of the previously published
studies are case reports, only a limited number of studies have
investigated the potential treatment strategies for this unique
population (1,3–5). In
the present study, to investigate this aspect, we performed a
retrospective analysis of data obtained from the Sun Yat-sen
University Cancer Center (Guangzhou, China). We evaluated the
survival rate, clinical features and prognostic factors in 26
patients who developed TC. The aim of this study was to
comprehensively identify the optimal therapeutic strategy for
TC.
Patients and methods
Patient data
This retrospective study comprised consecutive
patients admitted to the Sun Yat-sen University Cancer Center
between February, 1998 and February, 2012, who were diagnosed with
TC. Informed consent was obtained from the patients, while ethics
approval was obtained from the Institutional Research Ethics
Committee of the Sun Yat-sen University Cancer Center. In total, 26
TC patients were eligible to be included in this study (12 males
and 14 females). The male/female ratio was 0.85. The average age of
patients with TC was 42.5 years.
The cumulative risk of the TC patients was estimated
using the Kaplan-Meier method. Cox’s proportional-hazard regression
model was used to estimate the relative risk of survival following
treatment. P<0.05 was considered to indicate a statistically
significant difference.
Clinical data
Most of the TC patients included in this study had a
history of significant lifetime sun exposure. The pathological
diagnosis of the patients was confirmed to be TC. Patients (12/26)
were initially treated elsewhere and presented at the reported
center at the time of the locoregional recurrence development. The
most common tumor sites were areas of sun-exposed skin, including
14 cases located on the occipitalis, 6 on the scalp, 2 on the
temporal region, 2 on the ear, 1 on the napex and 1 on the lower
lip. Macroscopically, the neoplasms were described as exophytic,
polypoid, ulcerated or nodular lesions, with or without malodor or
bleeding. The size of the tumors ranged from 1 to 8 cm (mean size,
2.8 cm). Twenty cases were characterized by non-invasive, and 6
cases by invasive boundary. In most of the TC patients, the lesion
was present for a long time prior to diagnosis and a recent rapid
growth phase occurred.
Follow-up data were collected from the outpatient
service and complementary data were obtained by telephone inquiry
and follow-up letters. The follow-up deadline was set for February
29, 2012. The median follow-up period was 63.8 months (range, 1–147
months).
Treatment
The patients were treated with surgery alone, and
complete surgical excision with documented non-invasive intra- and
postoperative margins were recommended for the patients. Eleven
patients underwent direct suture after surgery, five reconstruction
with rotation flap, and the remaining 10 patients underwent local
rotation flap reconstruction and skin-grafting. Split skin was
obtained from the abdomen (7 cases) and anterolateral (3 cases),
meshed 1:1.5, and transplanted onto the dermal template.
Postoperative course was uneventful for the patients. However, two
patients who underwent expand resection and neck dissection
developed lymph node metastasis and far recurrence after the
initial surgery. Patients received chemotherapy treatment after
surgery.
Statistical analysis
Univariate analysis was conducted using the
Kaplan-Meier method and log-rank test. P<0.05 was considered to
indicate a statistically significant difference.
Results
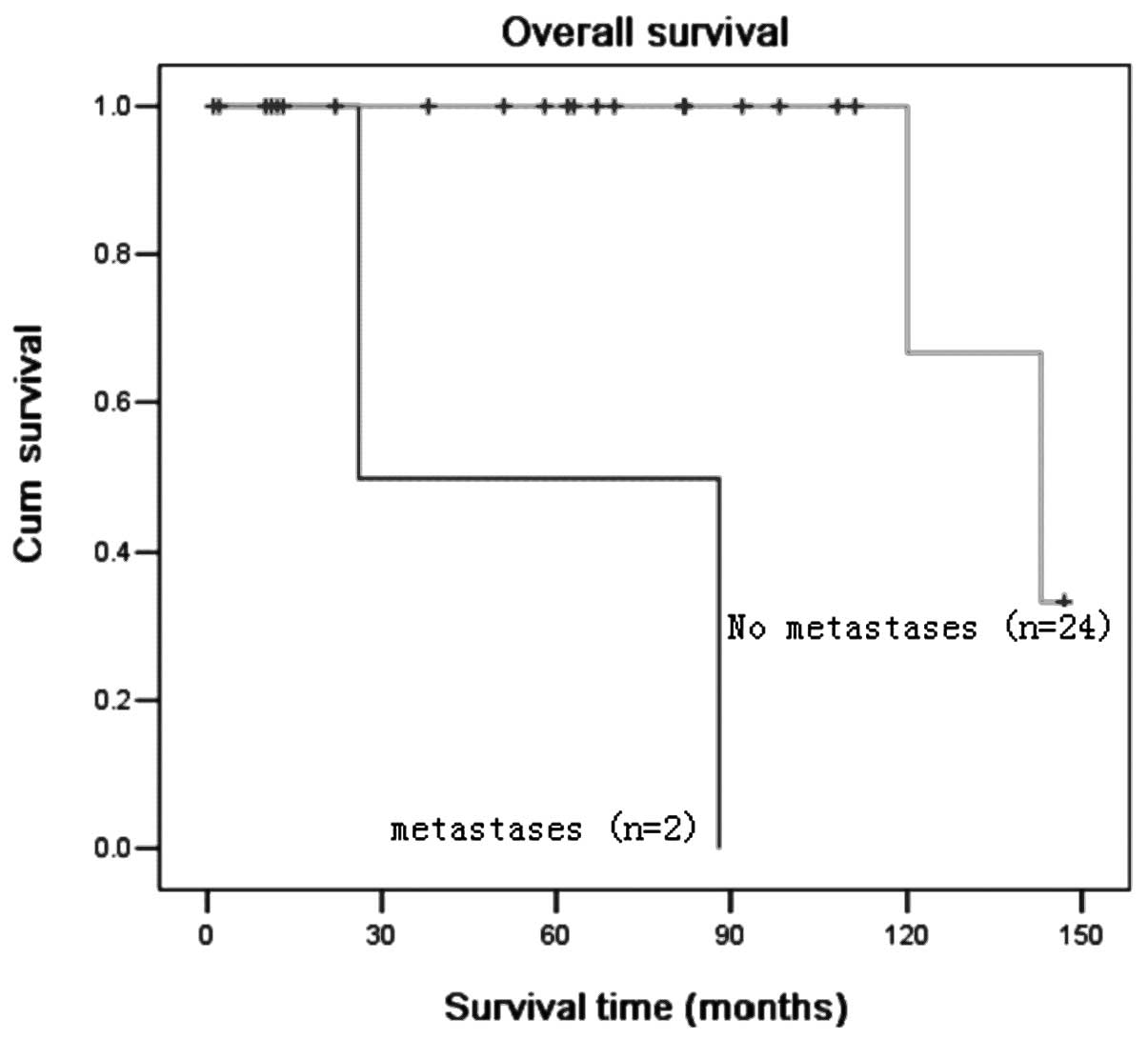
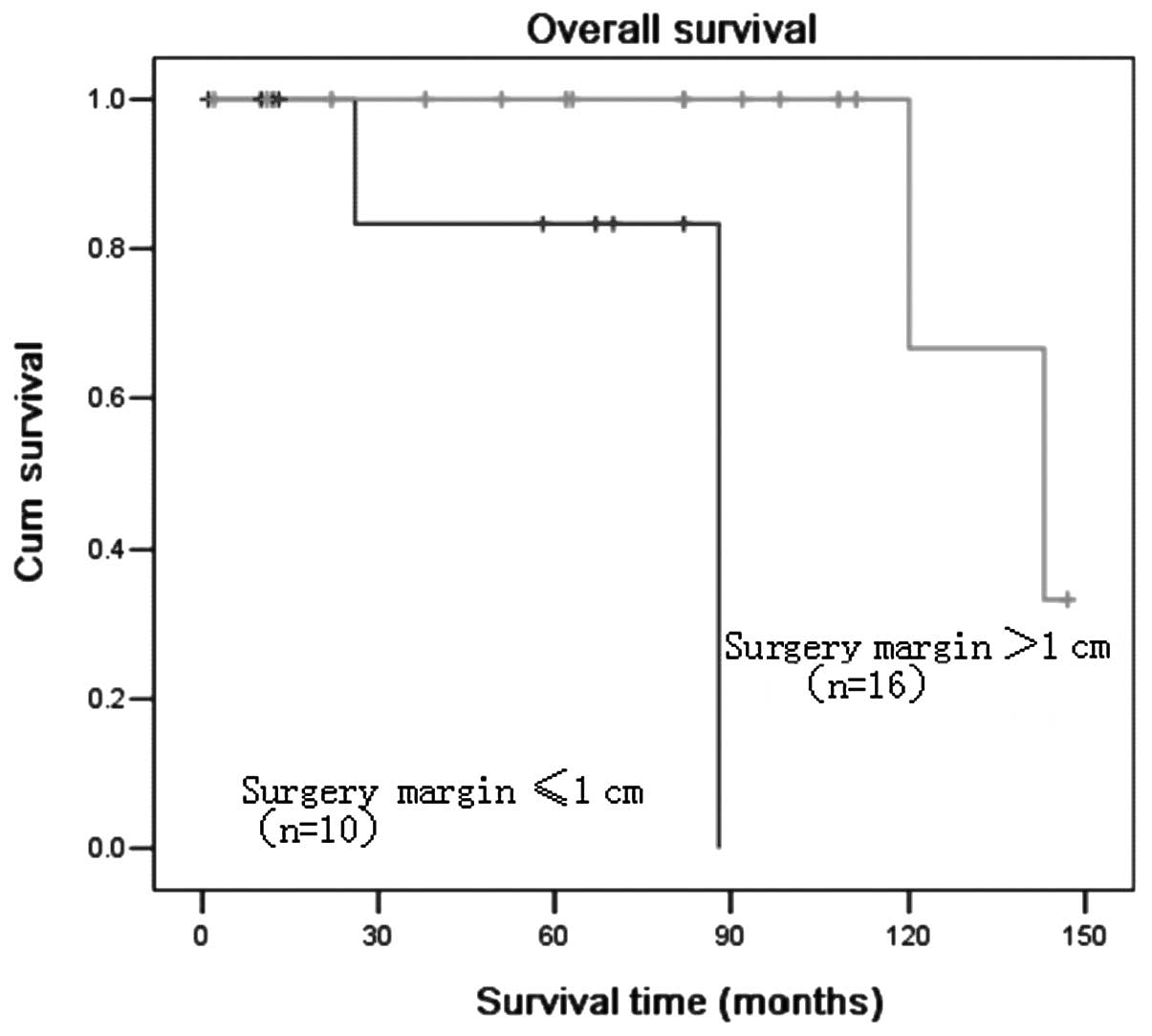
Four of the 26 patients succumbed to the disease.
The overall 5-year survival rate of the patients was 89.2%.
Univariate analysis demonstrated that the key prognostic factors
influencing the survival of these patients were lymph node
metastasis and surgery margin (Figs.
1 and 2). There was no
statistically significant correlation between TC and gender, tumor
size, age and locoregional recurrence (Table I).
 | Table IEffect of clinicopathological
characteristics on the survival of 26 trichilemmal carcinoma
patients, using the log-rank test. |
Table I
Effect of clinicopathological
characteristics on the survival of 26 trichilemmal carcinoma
patients, using the log-rank test.
| Characteristics | Cases (n) | 5-year survival
(months) |
χ2-value | P-value |
|---|
| Gender | | | 0.253 | 0.615 |
| Male | 12 | 88.9 | | |
| Female | 14 | 88.9 | | |
| Age (years) | | | 0.031 | 0.859 |
| >40 | 15 | 90.9 | | |
| ≤40 | 11 | 87.5 | | |
| Tumor size (cm) | | | 0.027 | 0.869 |
| D≤2.5 | 12 | 88.9 | | |
| D>2.5 | 14 | 90.0 | | |
| N classification | | | 22.539 | 0.000 |
| N+ | 2 | 00.0 | | |
| N0 | 24 | 87.5 | | |
| Local recurrence | | | 2.793 | 0.095 |
| Yes | 12 | 77.8 | | |
| No | 14 | 100 | | |
| Surgery margin
(cm) | | | 8.131 | 0.004 |
| ≤1.0 | 10 | 71.4 | | |
| >1.0 | 16 | 100 | | |
In the Cox proportional hazard regression model,
there was no risk factor affecting the survival of TC patients.
Discussion
TC is a rare, cutaneous adnexal malignant tumor
deriving from the outer root sheath of hair follicles usually
affecting the sun-exposed areas of the skin in elderly people
(1,7). TC is usually a solitary indolent
lesion, although it can appear as multiple lesions on
non-sun-exposed skin (8).
Clinically, it may be misdiagnosed as squamous or basal cell
carcinoma, nodular melanoma or keratoacanthoma. TC has been shown
to be a malignant form of a trichilemmoma (9). The diagnosis is established following
histopathological examination using hematoxylin and eosin (H&E)
staining which, when necessary, is complemented by
immunohistochemical staining of the lesions (10).
Generally, TC has a non-aggressive course. In their
study, Boscaino et al(7)
reported that after excision of the lesions in seven patients,
there was no recurrence of the tumor within a 2-month to 4-year
follow-up period. The clinical findings of this study were similar
to those previously described (1,3,5,7,8–10).
First, the duration of the lesion prior to diagnosis ranged from 2
months to 50 years. In some cases, rapid growth of tumor was noted
prior to presentation after a long period of time and these tumors
were frequently misdiagnosed as benign lesions. Most of the TC
patients had a history of significant lifetime sun exposure. The
distribution of the lesions suggest that sunlight is important in
the development of this malignancy (11). However, TC is an adnexal tumor,
thus its regional distribution may simply reflect its appendageal
origin which favors the head and neck region. Moreover, TC has been
reported in burn scars, as well as in an elderly man who received
50–60 diagnostic chest radiographs for the management of pulmonary
tuberculosis (12,13). However, the pathogenesis of TC
remains poorly understood.
Although TC is known to be an unusual malignant
lesion with its histological characteristics suggesting an
intermediate- to high-grade malignancy, it is generally
characterized by a benign neoplasm process and can be treated with
complete excision (9). Routine
care for this tumor has been surgical excision with the
demonstration of non-invasive margins (14). Histologically, non-invasive margins
are crucial for locally aggressive growth pattern and local
recurrence potential (9,14,17). In this study, despite the wide
local excision with tumor-free margins, the tumor recurred in two
cases, while 24/26 patients underwent surgical excision with a
satisfactory outcome. Surgery is considered to be the treatment of
choice for TC, and periodic surveillance without adjuvant therapy
is generally sufficient (12).
Local cervical lymph node and distant metastases of
this neoplasm have rarely been reported in the medical literature
(3,9,14).
In this study, a total of two patients succumbed to the disease one
year and six months after surgery and chemotherapy (cisplatin,
bleomycin and vindesine), due to regional lymph node and presented
distant metastases. No optimal treatment for TC with metastases has
been suggested and there is no established chemotherapy regimen
reported in the medical literature. In their study, Yi et
al(6) reported that a patient
was treated with four cycles of cisplatin plus cyclophosphamide
combination chemotherapy and a partial remission was achieved. The
cisplatin plus cyclophosphamide treatment was not curative, but
controlled tumor growth. In their study, Roismann et
al(10) described a TC case
where 4 cycles of chemotherapy (5 fluorouracil combined with
cisplatin) were administered in case of poor prognosis (10). Moreover, Hayashi et
al(15) and Ikegawa et
al(16) administered
chemotherapy [cisplatin, adriamycin and vindesine (CAV) treatment]
similar to the regimen used for highly advanced cases of squamous
cell carcinoma. The present study shows a recurrent TC case that
was difficult to treat, which presented distant metastases
(4,6,10,15,16).
In summary, after the investigation of the
clinicopathological characteristics of 26 TC patients, the
treatment of TC is suggested to be exclusively surgical. Simple
excision with 1-cm margins is believed to be safe, cost-efficient
and effective for the treatment of TC. Moreover, postoperative
follow-up of the patient in order to facilitate early diagnosis of
the recurrence and distant metastasis is necessary. Systemic
chemotherapy should be considered when distant tumor metastasis is
confirmed, which is potentially useful for the monitoring of
disease progression.
References
|
1.
|
Reis JP, Tellechea O, Cunha MF and
Baptista AP: Trichilemmal carcinoma: a review of eight cases. J
Cutan Pathol. 20:44–49. 1993. View Article : Google Scholar
|
|
2.
|
Maize JC and Snider RL: Nonmelanoma skin
cancers in association with seborrheic keratoses. Clinicopathologic
correlations. Dermatol Surg. 21:960–962. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Swanson PE, Marrogi AJ, Williams DJ,
Chewitz DL and Wick MR: Trichilemmal carcinoma: clinicopathologic
study of 10 cases. J Cutan Pathol. 19:100–109. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Van Zele D, Arrese JE, Heymans O, et al:
Invasive tricholemmal carcinoma of the nose. Dermatology.
204:315–317. 2002.PubMed/NCBI
|
|
5.
|
Dailey JR, Helm KF and Goldberg SH:
Tricholemmal carcinoma of the eyelid. Am J Ophthalmol. 115:118–119.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Yi HS, Sym SJ, Park J, Cho EK, Ha SY, Shin
DB and Lee JH: Recurrent and metastatic trichilemmal carcinoma of
the skin over the thigh: a case report. Cancer Res Treat.
42:176–179. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Boscaino A, Terracciano LM, Donofrio V, et
al: Tricholemmal carcinoma: a study of seven cases. J Cutan Pathol.
19:94–99. 1992. View Article : Google Scholar
|
|
8.
|
Garrett AB and Scott KA: Trichilemmal
carcinoma: a case report of a rare skin cancer occurring in a renal
transplant patient. Transplantation. 76:11312003. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Garrett AB, Azmi FH and Ogburia KS:
Trichilemmal carcinoma: a rare cutaneous malignancy: a report of
two cases. Dermatol Surg. 30:113–115. 2004.PubMed/NCBI
|
|
10.
|
Roismann M, Freitas RR, Ribeiro LC,
Montenegro MF, Biasi LJ and Jung JE: Trichilemmal carcinoma: case
report. An Bras Dermatol. 86:991–994. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Laochumroonvorapong P, Kokta V and Quan
MB: Trichilemmal carcinoma in an African American. Dermatol Surg.
28:284–286. 2002.PubMed/NCBI
|
|
12.
|
Ko T, Tada H, Hatoko M, Muramatsu T and
Shirai T: Trichilemmal carcinoma developing in a burn scar: a
report of two cases. J Dermatol. 23:463–468. 1996.PubMed/NCBI
|
|
13.
|
Chan KO, Lim IJ, Baladas HG and Tan WT:
Multiple tumour presentation of trichilemmal carcinoma. Br J Plast
Surg. 52:665–667. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Wong TY and Suster S: Tricholemmal
carcinoma. A clinicopathologic study of 13 cases. Am J
Dermatopathol. 16:463–473. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Hayashi I, Harada T, Muraoka M and Ishii
M: Malignant proliferating trichilemmal tumour and CAV (cisplatin,
adriamycin, vindesine) treatment. Br J Dermatol. 150:156–157. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Ikegawa S, Saida T, Obayashi H, Sasaki A,
Esumi H, Ikeda S, et al: Cisplatin combination chemotherapy in
squamous cell carcinoma and adenoid cystic carcinoma of the skin. J
Dermatol. 16:227–230. 1989.PubMed/NCBI
|