Introduction
In 2012, >400,000 patients in Europe were
diagnosed with lung cancer (1).
Historically, it has been reported that approximately one-third of
these individuals will develop bone metastases (2,3).
However, recent advances in treatment, such as the use of
inhibitors of the epidermal growth factor receptor and anaplastic
lymphoma kinase oncogenes (4),
have extended the life expectancy of patients with lung cancer,
suggesting that bone metastases and their associated complications
have become more clinically relevant (5).
Metastatic bone complications, otherwise known as
skeletal-related events (SREs), are common in patients with lung
cancer; a large, randomised, placebo-controlled, phase 3 study
demonstrated that the rate of SREs in patients with lung cancer and
other solid tumours (excluding breast and prostate cancer) was 46%
over a 21-month period (6). SREs
are typically defined as radiation to bone, pathological fractures,
surgery to bone and spinal cord compression. SREs may cause
debilitating pain and reduced mobility, resulting in a reduction in
the quality of life and significant decreases in physical
well-being and functional independence (7,8).
Radiation to bone, often used to treat pain, may itself cause
transient increases in pain (‘pain flare’) (9), while opioids, also commonly used to
alleviate pain, are associated with severe side effects, including
nausea and constipation (10), as
well as psychological association and fears (11). In addition to causing persistent
pain, pathological fractures reduce load-bearing capacity and
restrict movement. Furthermore, spinal cord compression is a
serious complication, which may even lead to paralysis (2,12).
Surgery to bone often requires lengthy inpatient stays, which may
be traumatic for patients and their families (13). Thus, SREs impose a substantial
burden on patients.
In addition to the clinical and patient impact, SREs
place a considerable burden onto healthcare systems. Several
retrospective studies have highlighted the increase in treatment
costs as patients with lung cancer progress to metastatic bone
disease and experience associated SREs (14–18).
A prospective study in France also highlighted the high cost of
care of patients with SREs, with 50% of the cost for the treatment
of patients with lung cancer who have bone metastases being linked
to the occurrence of SREs (19).
Although these data provide some insight into the impact that lung
cancer-associated SREs have on healthcare systems, there is
generally a lack of prospective data from a broader European
population. Increasing awareness of the burden of these bone
complications will highlight the need for appropriate patient
management and aid healthcare planning through a better
understanding of the resources commonly required in treating
SREs.
A prospective, observational, multinational study
was conducted to evaluate the health resource utilisation (HRU)
associated with SREs in patients with bone metastases secondary to
cancer of the prostate, breast or lung and multiple myeloma in
Canada, Germany, Italy, Spain, the United Kingdom (UK) and the
United States of America. Data on the HRU associated with all
tumour types in Europe and the financial cost of SREs associated
with solid tumours in Europe have previously been reported
(20,21). In the present study, we assessed
the data for the subset of patients with lung cancer from Germany,
Italy, Spain and the UK, since the European approach to patient
management is fairly congruent.
Materials and methods
Patients
Eligible patients were aged ≥18 years, with bone
metastases secondary to lung cancer and a life expectancy of ≥6
months (as judged by the treating physician). Patients were
required to have an Eastern Cooperative Oncology Group (ECOG)
performance status of 0, 1 or 2 and to have experienced ≥1 SRE in
the 97 days prior to enrolment (index SRE). For patients who had
experienced >1 SRE in the 97 days prior to enrolment, the index
SRE was classified based on the following hierarchy: spinal cord
compression, surgery to bone, pathological fracture and radiation
to bone. Patients who were already enrolled into an investigational
drug trial for the treatment of bone metastases or prevention of
SREs were excluded from this study.
Study design
Patient demographics and medical history (including
time since bone metastasis detection) were collected at enrolment.
Data were collected both retrospectively and prospectively: HRU
data for each patient were collected retrospectively through chart
review for all SREs occurring in the 97-day period prior to
enrolment and prospectively for the duration of each participant’s
involvement in the study. Treating physicians independently
attributed HRU to SREs. If radiation or surgery to bone was
performed as a result of another SRE (i.e., to treat a primary
SRE), the physicians had the option of attributing the HRU to the
primary SRE. However, in these cases, the inclusion of radiation or
surgery to bone as discrete SREs with no associated HRU in the
analysis would result in an underestimation of the mean HRU for
these two types of SREs. Thus, in such cases, these SREs were
excluded from the analysis. Physicians were required to report all
SRE-related HRU data at least every 90 days during the prospective
data collection period.
The planned follow-up period was 18–21 months. The
HRU outcome measures recorded were as follows: number, duration and
facility type of inpatient stays; number and facility type of
outpatient visits; number and specific type of procedures (e.g.,
imaging, radiation therapy or outpatient procedures, such as
surgery); number of emergency department visits; number of home
health visits; and previous bisphosphonate use and duration of
use.
Informed consent was required prior to the
collection of patient data. The study was performed in compliance
with the Helsinki Declaration.
Statistical analyses
HRU was summarised by SRE type; the details have
been previously described (20).
The mean HRU per SRE type was calculated by dividing the total HRU
attributed to a specific SRE type by the total number of SREs of
the same type. The mean duration of inpatient stay per SRE was
calculated as the total number of inpatient days divided by the
total number of SREs that were associated with at least one
inpatient stay (if a SRE contributed multiple inpatient stays, the
total duration of all these inpatient stays was used).
The data are primarily reported as both mean and
median values, where appropriate. The mean values describe the
total resources used at a population level: information that is
required for healthcare policy decisions (20). The median values are also reported
to illustrate the distribution of data when sample sizes are small
and to describe the typical HRU for an individual patient.
Results
Study cohort
A total of 135 patients with a primary diagnosis of
lung cancer were enrolled (Table
I). Of the 135 patients, 34 were from Germany, 43 from Italy,
41 from Spain and 17 from the UK. Baseline characteristics were
generally similar across the four countries. The mean age ±
standard deviation (SD) ranged from 60.3±10.3 to 66.6±11.4 years
across all countries. Data on the number of patients who had
received bisphosphonates at any point prior to enrolment revealed
that, compared with patients from the other countries, patients in
the UK were less likely to have received bisphosphonate treatment.
This may be associated with the fact that fewer patients in the UK
had previously experienced SREs prior to the 97-day period
preceding the signing of informed consent. The median time to
enrolment since primary cancer diagnosis ranged from 2.2 to 3.5
months across all countries and was similar to the median time
since the detection of bone metastasis (range, 1.7–2.5 months).
This suggests that, in a large proportion of patients, diagnoses
were made at a late stage of the disease, with patients likely to
have metastases at the time of diagnosis. The median length of the
follow-up was 1.5–5.6 months across the four countries.
 | Table IBaseline demographics and disease
history. |
Table I
Baseline demographics and disease
history.
| Germany (n=34) | Italy (n=43) | Spain (n=41) | UK (n=17) |
|---|
| Follow-up time,
months | | | | |
| Mean (SD) | 5.5 (4.1) | 5.6 (4.2) | 3.7 (3.8) | 3.2 (4.2) |
| Median (Q1, Q3) | 5.6 (2.0, 8.2) | 4.8 (1.9, 8.0) | 2.6 (1.2, 4.4) | 1.5 (0.7, 3.3) |
| Male, n (%) | 24 (70.6) | 26 (60.5) | 28 (68.3) | 10 (58.8) |
| Ethnic group, n
(%) | | | | |
| White or
Caucasian | 33 (97.1) | 43 (100.0) | 40 (97.6) | 17 (100.0) |
| Other | 1 (2.9) | 0 (0.0) | 1 (2.4) | 0 (0.0) |
| Age, years | | | | |
| Mean (SD) | 63.0 (10.6) | 64.1 (9.1) | 60.3 (10.3) | 66.6 (11.4) |
| ≥65, n (%) | 15 (44.1) | 24 (55.8) | 15 (36.6) | 10 (58.8) |
| ECOG performance
status, n (%) | | | | |
| 0 | 4 (11.8) | 12 (27.9) | 7 (17.0) | 0 (0.0) |
| 1 | 18 (52.9) | 17 (39.5) | 17 (41.5) | 5 (29.4) |
| 2 | 12 (35.3) | 14 (32.6) | 17 (41.5) | 12 (70.6) |
| History of
SREsa, n (%) | 22 (64.7) | 24 (55.8) | 27 (65.9) | 2 (11.8) |
| Time to enrolment
since primary cancer diagnosis, months | | | | |
| Mean (SD) | 7.8 (15.0) | 7.0 (9.5) | 8.1 (10.8) | 14.2 (32.3) |
| Median (Q1, Q3) | 3.2 (1.2, 6.5) | 2.6 (1.4, 8.5) | 3.5 (1.5,
10.4) | 2.2 (1.2, 5.2) |
| Time since bone
metastasis detection, months | | | | |
| Mean (SD) | 4.5 (12.9) | 4.2 (4.2) | 4.6 (7.3) | 2.6 (2.3) |
| Median (Q1,
Q3) | 1.9 (0.85,
3.4) | 2.5 (1.4, 6.7) | 1.8 (1.2, 4.4) | 1.7 (1.2, 3.2) |
| Previous
bisphosphonate useb, n (%) | 22 (64.7) | 21 (48.8) | 16 (39.0) | 5 (29.4) |
| Duration of
previous bisphosphonate useb,
months | | | | |
| Mean (SD) | 5.0 (16.1) | 2.7 (3.7) | 3.3 (7.8) | 1.0 (0.8) |
| Median (Q1,
Q3) | 1.2 (0.4, 2.0) | 1.7 (0.2, 3.1) | 0.9 (0.4, 1.7) | 0.9 (0.6, 1.1) |
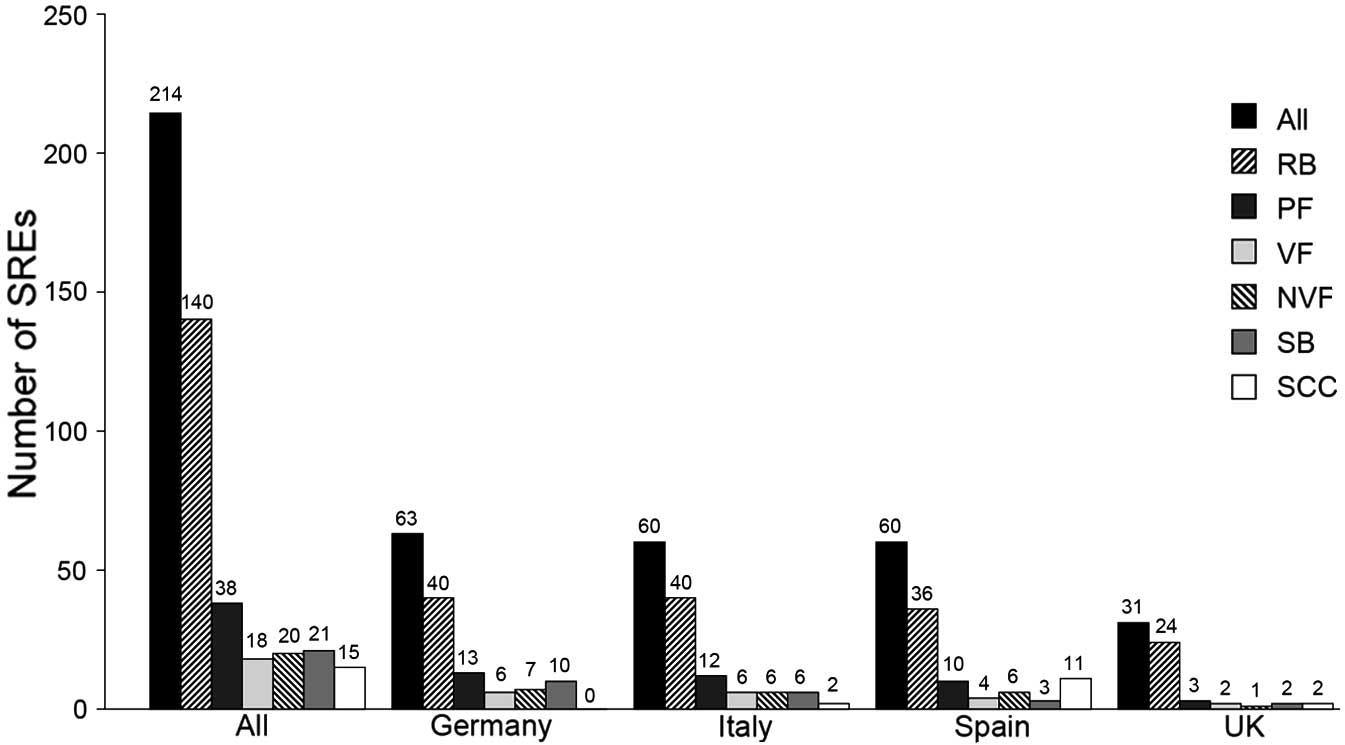
Skeletal-related events
Eligible patients experienced a total of 239 SREs.
Analysis of the crude SRE data (including SREs that were excluded
from the HRU analysis) found the number of SREs per patient-year
varied by country (2.8 for Germany, 2.1 for Italy, 3.2 for Spain
and 3.9 for the UK). Following removal of the SREs for which HRU
was attributed to another (primary) SRE, 214 SREs were included in
the study (Fig. 1). Radiation to
bone was the most common SRE (140 events); pathological fractures,
surgery to bone and spinal cord compression were less common (38,
21 and 15 events, respectively).
Health resource utilisation
Inpatient stays
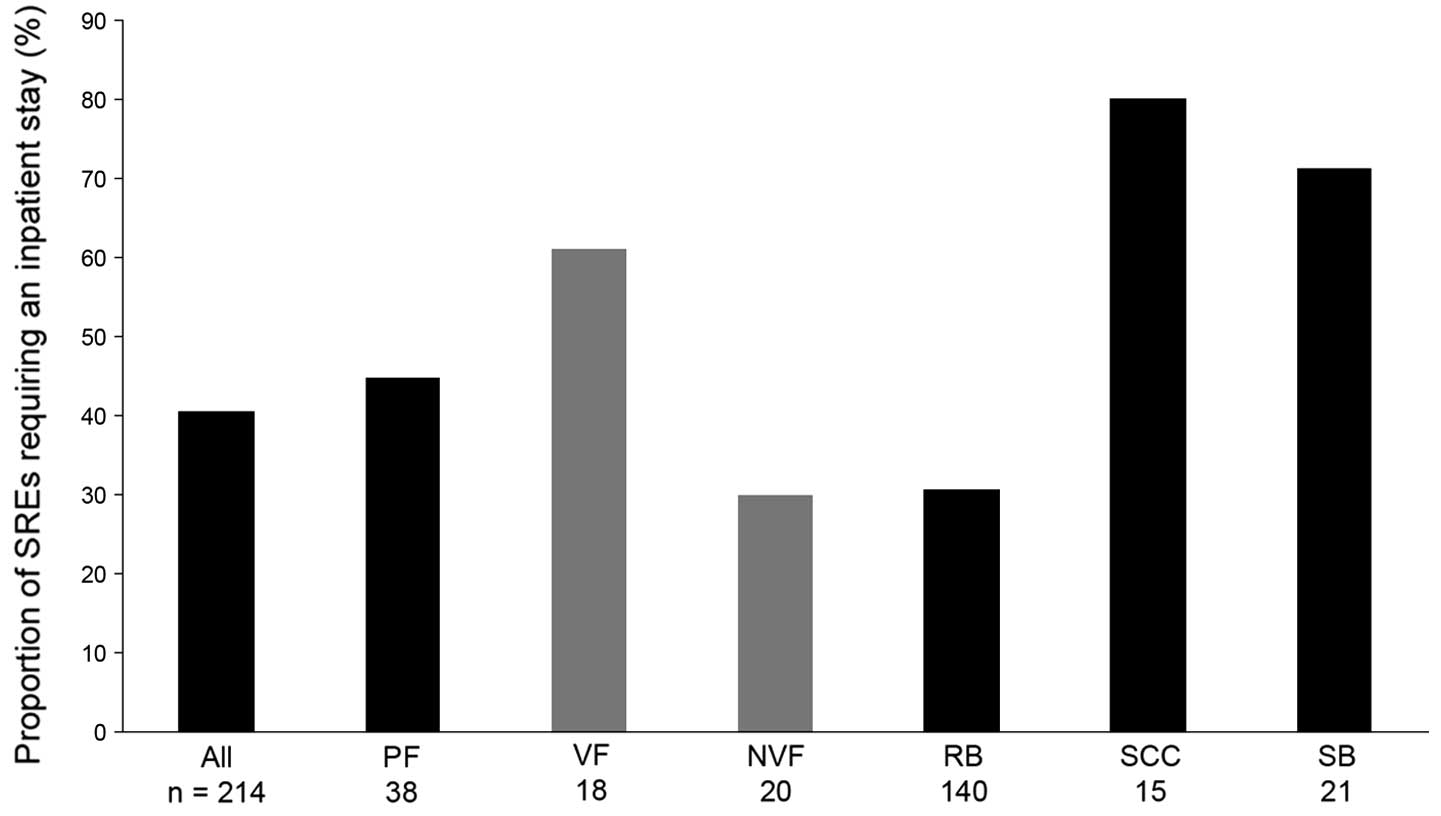
Overall, 4 in every 10 SREs (87 of 214 SREs)
required an inpatient stay (Fig.
2). Inpatient stays were slightly less frequent in the
UK, being required in approximately 3 in every 10 SREs. Spinal cord
compression and surgery to bone were the SREs most likely to result
in an inpatient stay (80.0 and 71.4% of SREs, respectively). In
Germany, hospitalisation for radiation to bone was also relatively
common, with 1 in 2 SREs requiring an inpatient stay (50.0%). In
Spain and Italy, patients were more likely to be hospitalised for
pathological fractures compared with the other countries (60.0 and
58.3%, respectively, compared with the overall mean of 44.7% for
all the countries), although the data should be interpreted with
caution due to the small number of pathological fracture events in
total.
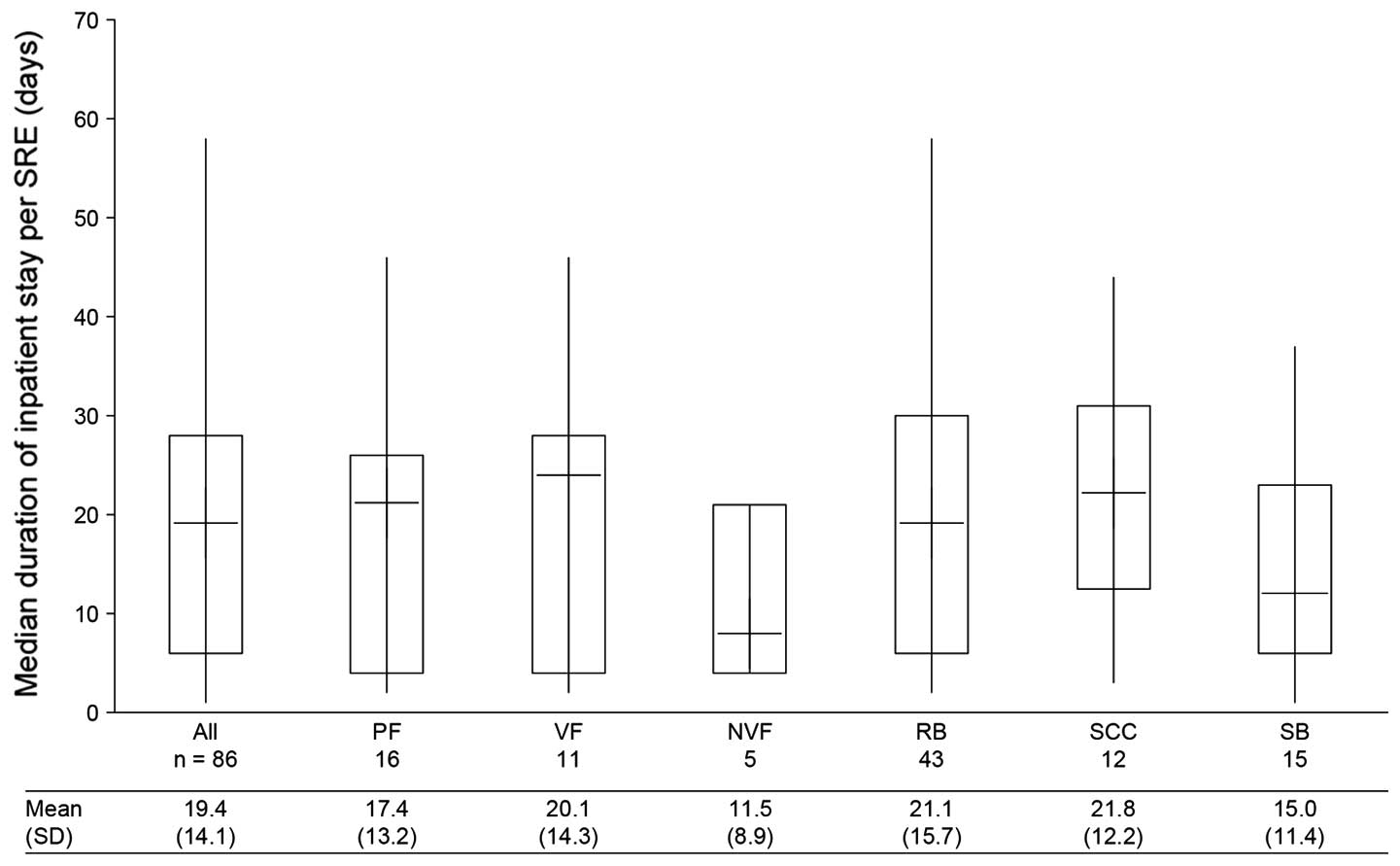
Data on the duration of inpatient stays were
collected for 86 of the 87 SREs that required hospitalisation. The
median [quartile (Q)1, Q3] length of stay per SRE that resulted in
hospitalisation was 19.0 (6.0, 28.0) days (Fig. 3). Across all countries, spinal cord
compression and pathological fracture had the longest median length
of stays [22.0 (12.5, 31.0) and 21.0 (4.0, 26.0) days,
respectively] and surgery to bone the shortest [12.0 (6.0, 23.0)
days]. Patients were most likely to be treated in oncology units;
general, radiation and surgical units were also frequently used
(data not shown).
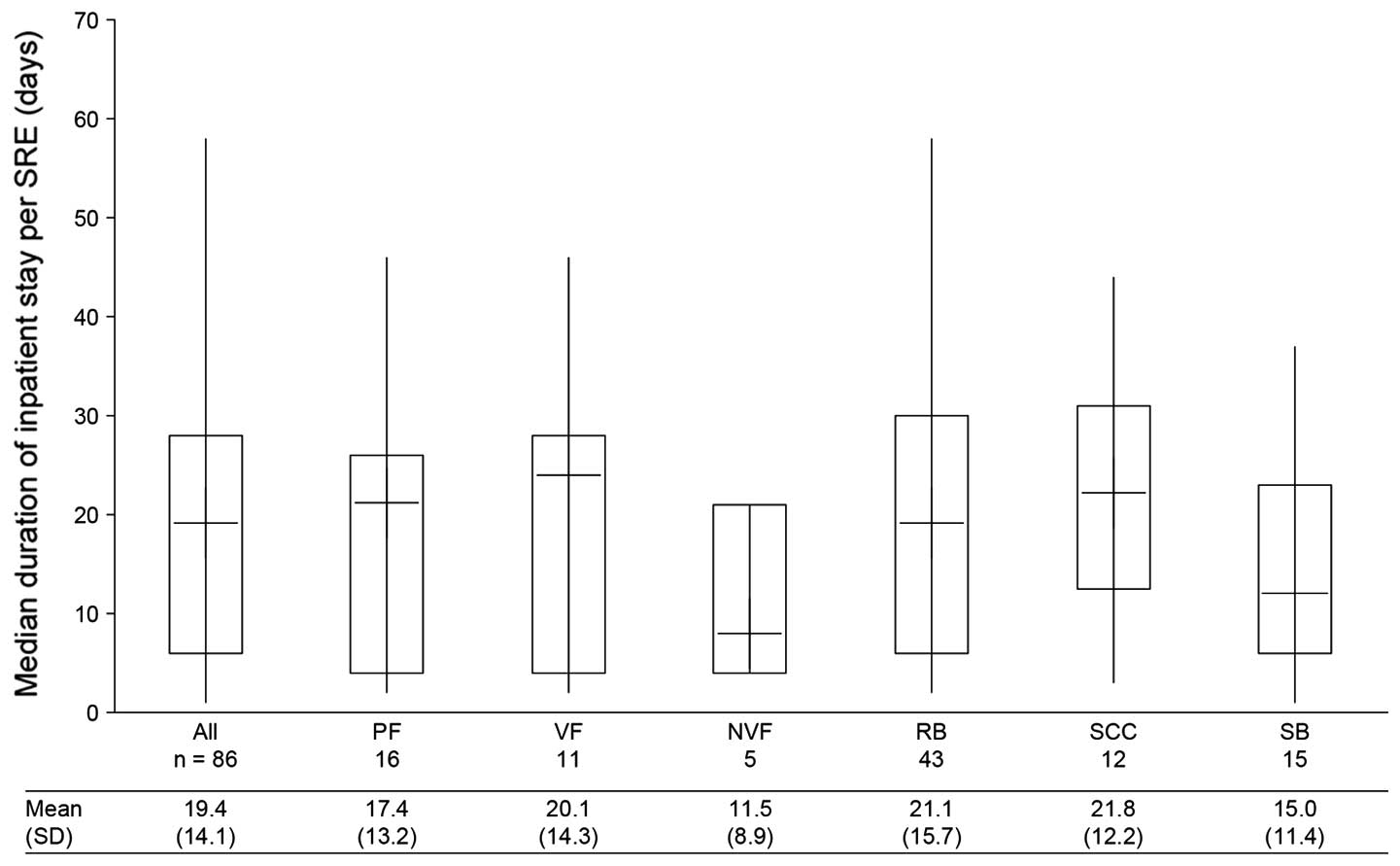 | Figure 3Duration of inpatient stay per SRE.
Data in the box and whisker plot are shown as median (horizontal
line within box) + interquartile range (box) + range (whiskers) and
include only SREs requiring an inpatient stay. If a SRE resulted in
multiple inpatient stays, the total duration of all the inpatient
stays was used. VF and NVF are subsets of PF. SRE, skeletal-related
event; SD, standard deviation; n, number of SREs; PF, pathological
fracture; VF, vertebral fracture; NVF, non-vertebral fracture; RB,
radiation to the bone; SCC, spinal cord compression; SB, surgery to
the bone. |
Outpatient visits
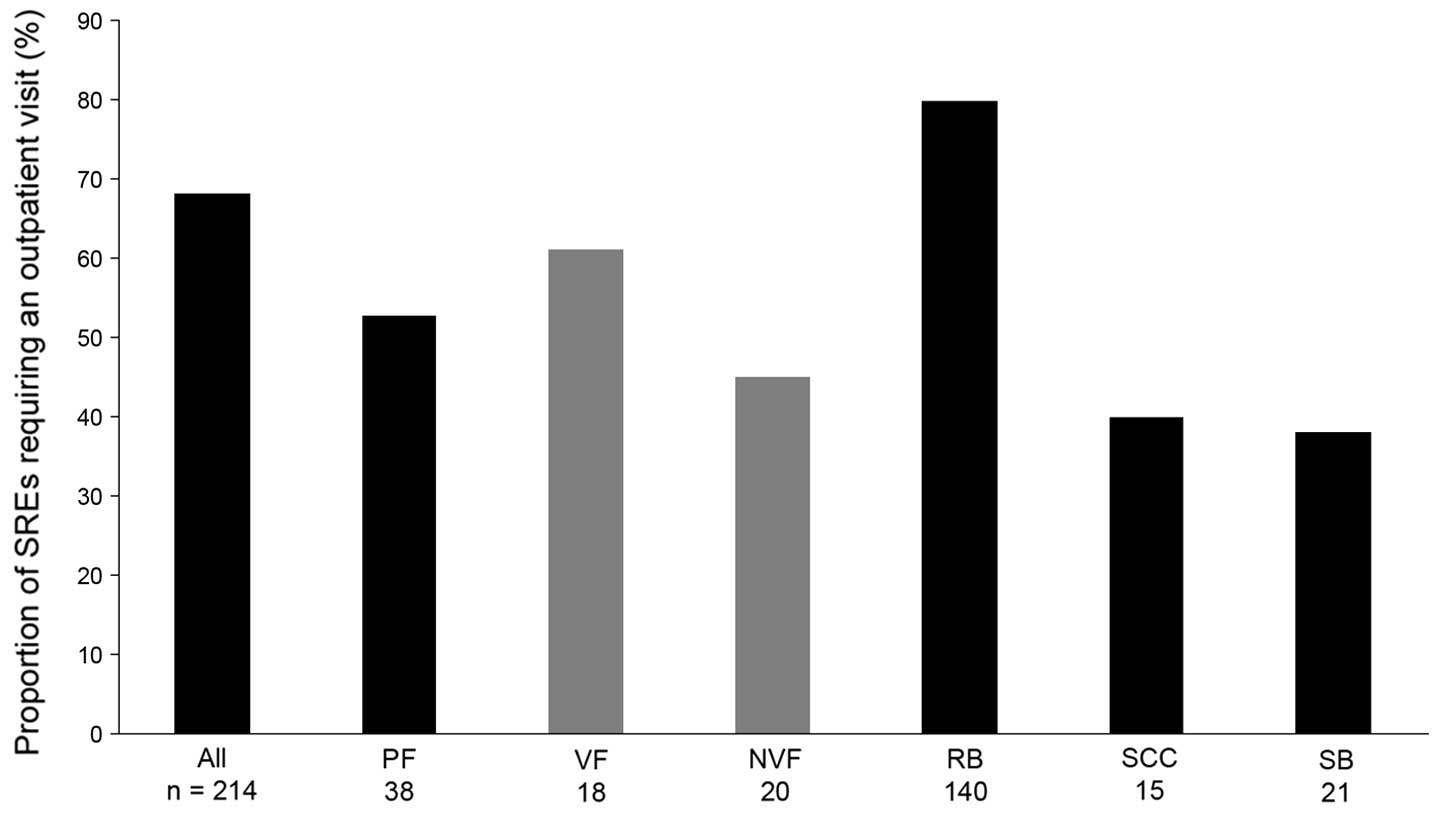
Across the four countries, two-thirds (mean 68.2%)
of SREs required an outpatient visit (Fig. 4). The rates were higher in Italy
and the UK (80.0 and 83.9% of events, respectively) compared with
those in Germany or Spain (58.7 and 58.3%, respectively). Radiation
to bone most frequently required outpatient visits (80.0% of
events), while surgery to bone required the fewest visits (38.1% of
events). This pattern was consistent across the countries, with the
exception of Germany, where pathological fractures were least
likely to require a visit (23.1%) and was low vs. the mean of the
overall study population (52.6%).
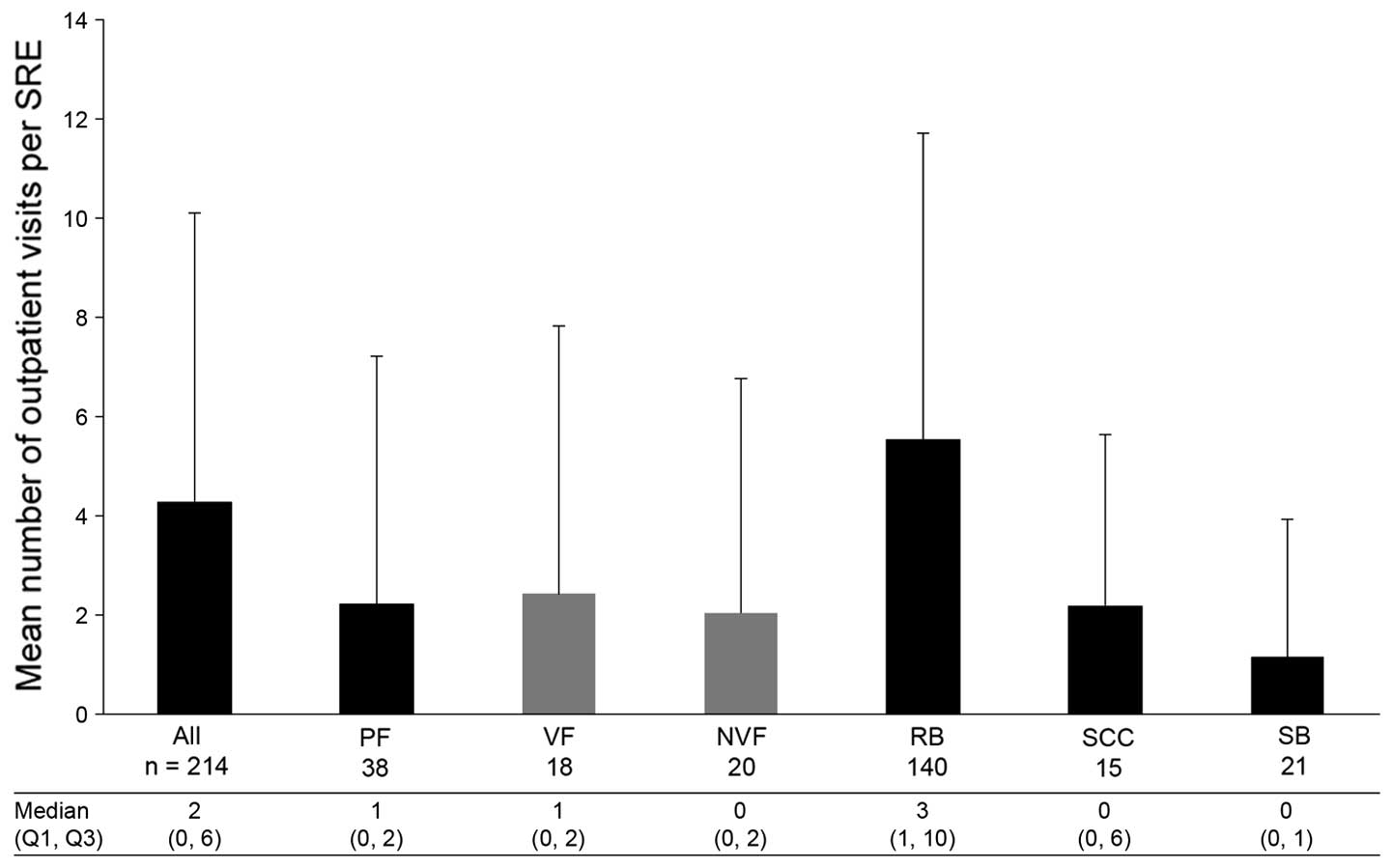
The mean number (± SD) of outpatient visits required
per SRE was 4.3 (±5.8), with radiation to bone requiring the most
[5.6 (±6.1)] and surgery to bone the fewest [1.2 (±2.8)] visits
(Fig. 5). Patients in Germany had
the highest mean number of outpatient visits per SRE [6.3 (±8.1)]
and patients in the UK had the lowest [2.9 (±3.0)]. Patients in the
UK had far fewer visits per radiation to bone event [mean, 2.6
(±2.6)] compared with those in the other three countries [ranging
between 4.5 (±4.4) and 8.6 (±8.1)].
 | Figure 5Number of outpatient visits per SRE.
Data in the bar chart are shown as mean + standard deviation. VF
and NVF are subsets of PF. SRE, skeletal-related event; Q1, first
quartile; Q3, third quartile; n, number of SREs; PF, pathological
fracture; VF, vertebral fracture; NVF, non-vertebral fracture; RB,
radiation to the bone; SCC, spinal cord compression; SB, surgery to
the bone. |
Procedures
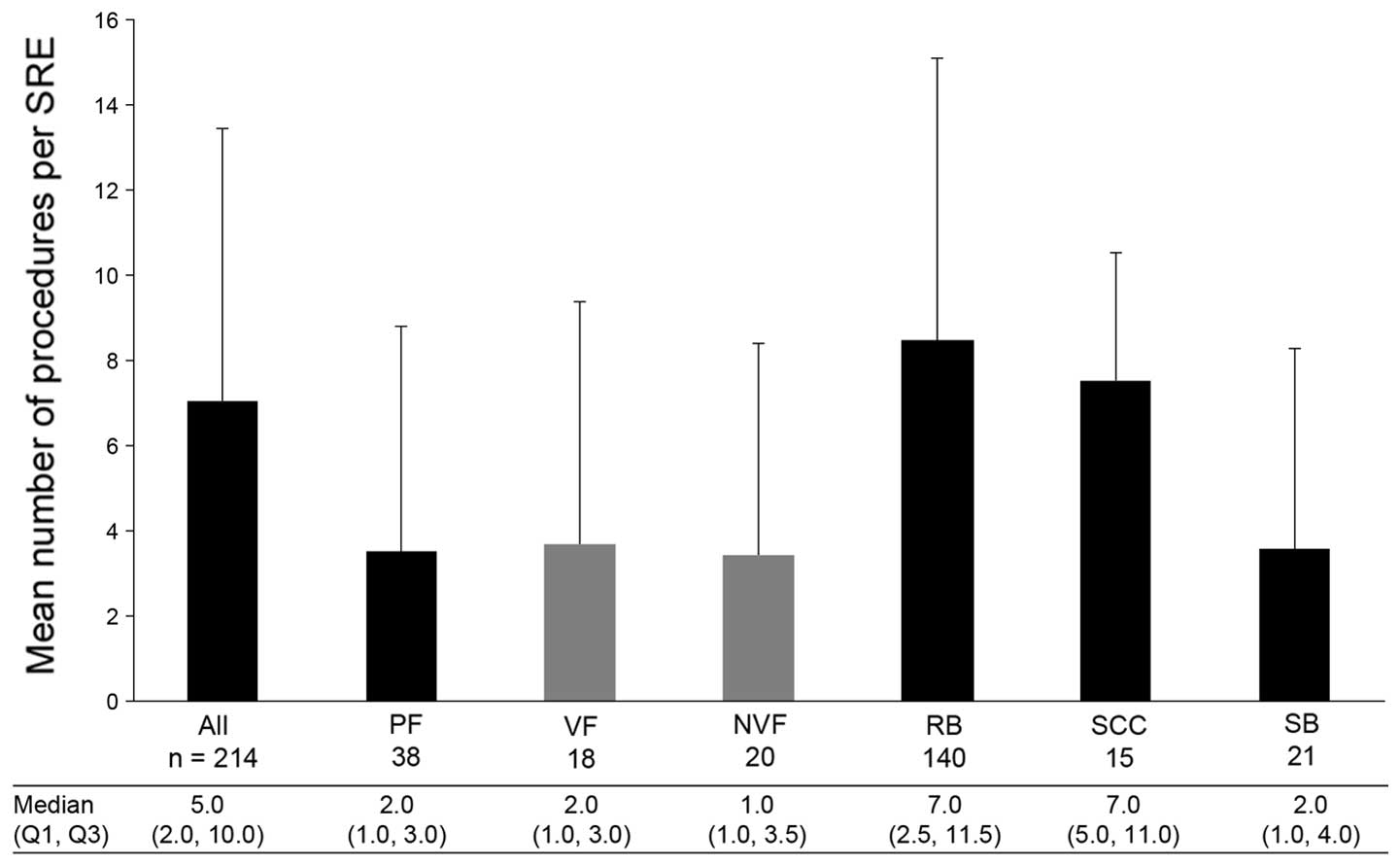
Almost all of the SREs required at least one
procedure (96.7%). Across all the SRE types and countries, a mean
(± SD) of 7.1 (±6.4) procedures were required per SRE (Fig. 6). The most common type of procedure
was external beam radiation, with a mean (±SD) of 4.1 (±6.0)
procedures per SRE, followed by intensity-modulated radiotherapy
[1.6 (±4.4)] and computed tomography [0.3 (±0.5)]. In all countries
apart from the UK, radiation to bone required the highest number of
procedures per SRE. In Germany, a mean of 13.9 (±7.1) procedures
were required per radiation to bone event; in the UK, only 3.4
(±2.4) procedures were performed per radiation to bone event. The
majority of the procedures were performed in the outpatient setting
[4.4 (±5.8) per SRE], with radiation to bone being the main
contributor to this mean value [5.7 (±6.1) procedures in the
outpatient setting per SRE]. The procedures were a major
contributor to SRE-related inpatient stays, with a mean (±SD) of
2.5 (±4.4) procedures requiring hospitalisation per SRE, with
spinal cord compression was the most significant contributor
(5.1±3.7 procedures resulting in an overnight stay per SRE).
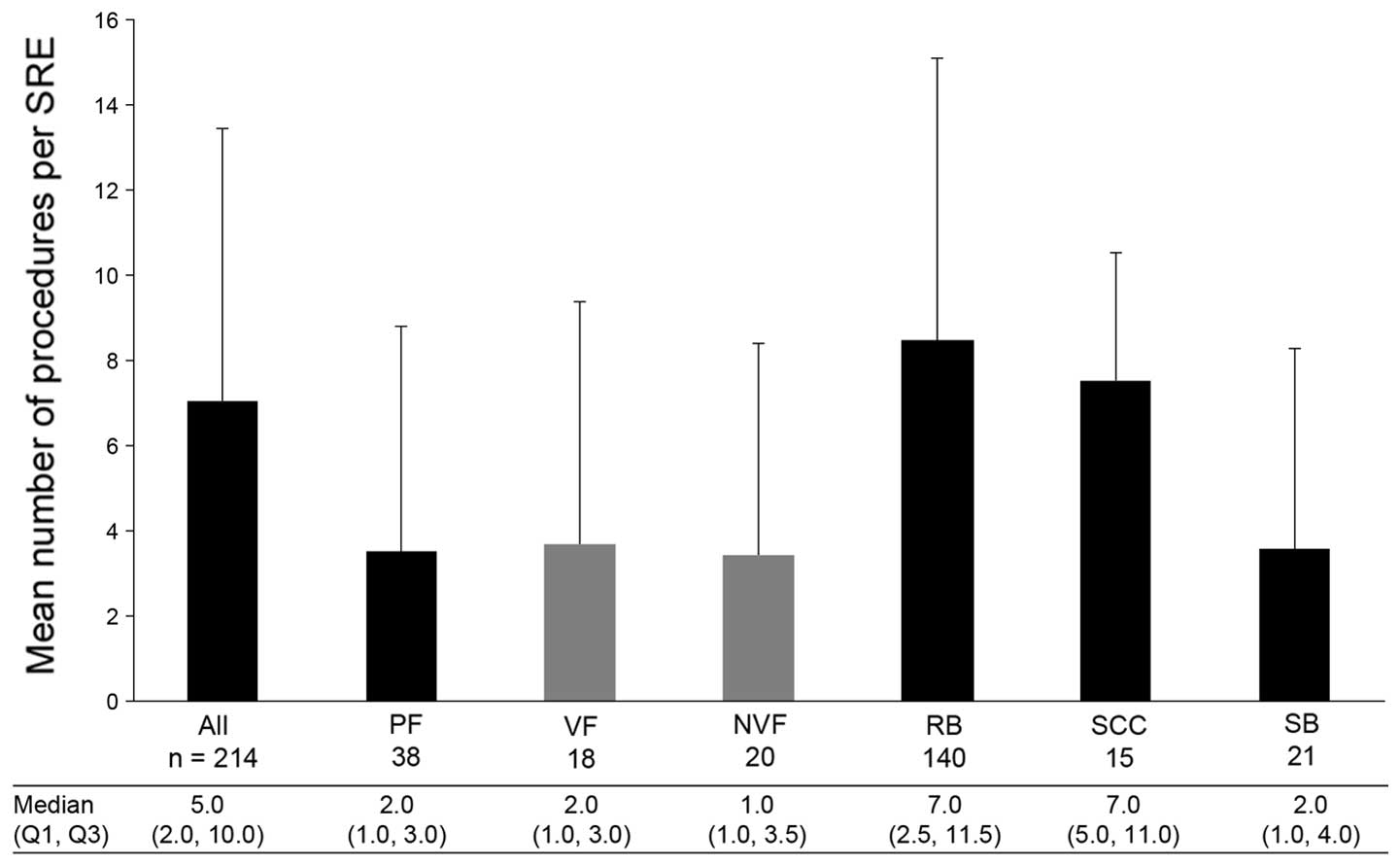 | Figure 6Number of procedures performed per
SRE. Data are presented as mean + standard deviation. VF and NVF
are subsets of PF. SRE, skeletal-related event; Q1, first quartile;
Q3, third quartile; n, number of SREs; PF, pathological fracture;
VF, vertebral fracture; NVF, non-vertebral fracture; RB, radiation
to the bone; SCC, spinal cord compression; SB, surgery to the
bone. |
Emergency department and home health
visits
Emergency department visits and home health visits
were less frequently reported compared to other measures of HRU
(3.3 and 0.9% of SREs, respectively).
Discussion
To the best of our knowledge, this is the first
combined retrospective and prospective study to investigate HRU
associated with SREs in patients with advanced lung cancer in
Europe. Furthermore, this is the first study in which HRU was
assigned to specific SREs independently by investigators.
Therefore, HRU was recorded only when the treating physician
considered it to be a direct result of a SRE, as opposed to the
underlying disease. In line with other previous studies (22,23),
all the SREs resulting from bone metastases secondary to lung
cancer were associated with substantial HRU.
Inpatient stays were common (40.7% of SREs), with
hospitalisations lasting a median of ~3 weeks. The proportion of
patients with lung cancer requiring an inpatient stay was
significantly higher compared to that of patients with breast or
prostate cancer (23,24). The patients were also more likely
to have a worse performance status, which may contribute to an
increased need for hospitalisation on experiencing a SRE. In
addition, outpatient visits were necessary for the majority of SREs
(68.2%), with several patients requiring multiple visits.
Similarly, almost every SRE required a procedure and multiple
procedures were common.
Although spinal cord compression and surgery to the
bone reportedly occur less frequently compared with the other SREs
(6), the results of this analysis
demonstrated that they were more likely to be associated with
inpatient stays; spinal cord compression was associated with the
longest stays among all SREs (median of 22.0 days). Conversely,
although radiation to bone was the SRE least likely to be
associated with an inpatient stay, this SRE occurs frequently
(6). Therefore, the associated HRU
is also likely to be substantial. Inpatient stays required for
radiation to bone were also lengthy, indicating that radiation to
bone may impose a significant burden on healthcare resources.
Radiation to bone also required the highest number of outpatient
visits and procedures per SRE, suggesting it is a major contributor
to HRU.
The patterns of HRU were generally similar across
countries, although certain exceptions were noted. In the UK,
radiation to bone was less likely to require multiple outpatient
visits and procedures compared to the other countries, possibly
reflecting a preference for single- as opposed to multiple-fraction
radiotherapy (25,26). Overall, the proportion of SREs
requiring an outpatient visit was highest in the UK and Italy.
Patients in these countries were also less likely to be
hospitalised, suggesting a preference for outpatient management of
SREs.
In our study, the incidence of previous treatment
with bisphosphonates for the prevention of SREs was low,
particularly in the UK. This reflects the lower percentage of
patients in the UK who had a history of SREs compared with the
other countries. In addition, the length of time over which
patients had been treated with bisphosphonates was short. The
general lack of treatment observed in all the countries may have
resulted in a high SRE incidence, contributing to the high levels
of HRU required by these patients.
Undertreatment with bone-targeted agents in patients
with bone metastases has been observed across a number of solid
tumour types (27) and appears to
be a particular problem in lung cancer. A study focusing on
patients with lung cancer reported that as few as 38% of the
patients received the bisphosphonate zoledronic acid, which was the
most commonly used bone-targeted agent at the time (28). A prospective chart audit
investigating bisphosphonate use in individuals with lung cancer
revealed that 44% of the patients were not receiving treatment at
the time of the study (29). These
trends may be due to the perceived short life expectancy of
patients with lung cancer (29)
and may also reflect the concern of adding nephrotoxic
bone-targeted agents to the nephrotoxic platinum-based chemotherapy
that is commonly used in the treatment of lung cancer. However,
SREs have been shown to commonly occur within the first 2 months of
diagnosis (15), with individuals
experiencing events every 3–6 months thereafter (2). Given that the median survival of
patients with advanced lung cancer is currently ~12 months
(5), a short life expectancy
should no longer constitute a reason for not prescribing treatment
with bone-targeted agents. Furthermore, avoiding SREs and their
associated complications, including increased requirements for
medical care and lengthy hospitalisations, may be of particular
concern to patients with a limited expected lifespan.
The timing of the initiation of treatment with
bone-targeted agents in patients with lung cancer may also be an
area of concern, considering that these patients are often
diagnosed at an advanced stage. The similar values reported in this
study for time since primary cancer diagnosis and time since bone
metastasis detection suggest that several patients presented with
metastatic bone disease at the time of primary cancer diagnosis.
This may also suggest that, up to that point, the patients had not
received treatment with bone-targeted agents and may already have
been experiencing pain associated with bone complications.
There were a number of limitations associated with
this study, as previously reported by Hoefeler et al
(20). The key considerations
included the limited duration of the follow-up. In addition, the
numbers of patients enrolled were also limited, leading to small
sample sizes in the majority of the SRE subsets, i.e., spinal cord
compression, surgery to bone and pathological fractures. It should
be noted that the relative proportions of SREs reported in this
study are not representative of the real-world distribution of SRE
types, as they are affected by the index SRE recruitment target
(i.e., prespecified numbers of each SRE type) and inclusion
criteria. Additionally, although pain was not defined as an SRE, it
is a common problem in patients with poorly treated bone metastases
and may contribute to additional HRU. In general, these limitations
may be expected to result in the underestimation of the overall HRU
associated with SREs and thus suggest that our data are
conservative.
This study highlights the considerable resource
requirements imposed on healthcare services by SREs in patients
with lung cancer and bone metastases. In addition to lowering the
burden on patients, preventing SREs in patients with bone
metastases secondary to lung cancer through better access to
effective and appropriate treatment may substantially reduce
HRU.
Acknowledgements
The authors would like to thank Dr Kim Allcott (PhD)
of Oxford PharmaGenesis™ Ltd., (Oxford, UK), who provided editorial
support. Funding for this support was provided by Amgen (Europe)
GmbH. Additional statistical analysis and support was provided by
Prayashi Ghelani, who is an employee of Amgen. Ignacio Duran has
acted as a member of advisory boards for Amgen. Cristina
Garzon-Rodriguez has acted as a member of advisory boards for
Amgen. Diana Lüftner has received honoraria for presentations and
has acted as a member of advisory boards for Amgen. Amit Bahl has
acted as a member of advisory boards for Amgen and has received
honoraria for presentations. John Ashcroft has acted as a member of
advisory boards for Amgen and Novartis. Guy Hechmati is an employee
of Amgen and holds stock. Rachel Wei is an employee of Amgen and
holds stock. Emma Thomas is an employee of Amgen and holds stock.
Herbert Hoefeler has acted as a member of advisory boards for
Amgen. This study was funded by Amgen.
References
|
1
|
Steliarova-Foucher E, O’Callaghan M,
Ferlay J, et al: European Cancer Observatory: Cancer Incidence,
Mortality, Prevalence and Survival in Europe. Version 1.0.
September. 2012, European Network of Cancer Registries,
International Agency for Research on Cancer. http://eco.iarc.fr.
Accessed June 18, 2013
|
|
2
|
Coleman RE: Clinical features of
metastatic bone disease and risk of skeletal morbidity. Clin Cancer
Res. 12:6243s–6249s. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Galasko C: The anatomy and pathways of
skeletal metastases. Bone Metastases. Weiss L and Gilbert A: GK
Hall; Boston: pp. 49–63. 1981
|
|
4
|
Mok TS: Personalized medicine in lung
cancer: what we need to know. Nat Rev Clin Oncol. 8:661–668. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brodowicz T, O’Byrne K and Manegold C:
Bone matters in lung cancer. Ann Oncol. 23:2215–2222. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosen LS, Gordon D, Tchekmedyian NS, et
al: Long-term efficacy and safety of zoledronic acid in the
treatment of skeletal metastases in patients with nonsmall cell
lung carcinoma and other solid tumors: a randomized, phase III,
double-blind, placebo-controlled trial. Cancer. 100:2613–2621.
2004. View Article : Google Scholar
|
|
7
|
Costa L, Badia X, Chow E, Lipton A and
Wardley A: Impact of skeletal complications on patients’ quality of
life, mobility, and functional independence. Support Care Cancer.
16:879–889. 2008.
|
|
8
|
Mercadante S: Malignant bone pain:
pathophysiology and treatment. Pain. 69:1–18. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Loblaw DA, Wu JS, Kirkbride P, et al: Pain
flare in patients with bone metastases after palliative
radiotherapy - a nested randomized control trial. Support Care
Cancer. 15:451–455. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Coleman RE: Skeletal complications of
malignancy. Cancer. 80(Suppl 8): 1588–1594. 1997. View Article : Google Scholar
|
|
11
|
National Collaborating Centre for Cancer
(UK). Opioids in palliative care: safe and effective prescribing of
strong opioids for pain in palliative care of adults. Full
guideline. May;2012.PubMed/NCBI
|
|
12
|
Loblaw DA, Perry J, Chambers A and
Laperriere NJ: Systematic review of the diagnosis and management of
malignant extradural spinal cord compression: the Cancer Care
Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease
Site Group. J Clin Oncol. 23:2028–2037. 2005.
|
|
13
|
Katzer A, Meenen NM, Grabbe F and Rueger
JM: Surgery of skeletal metastases. Arch Orthop Trauma Surg.
122:251–258. 2002. View Article : Google Scholar
|
|
14
|
Body JJ, Chevalier P, Gunther O, Hechmati
G and Lamotte M: The economic burden associated with
skeletal-related events in patients with bone metastases secondary
to solid tumors in Belgium. J Med Econ. 16:539–546. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Delea T, Langer C, McKiernan J, et al: The
cost of treatment of skeletal-related events in patients with bone
metastases from lung cancer. Oncology. 67:390–396. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Delea T, McKiernan J, Brandman J, et al:
Retrospective study of the effect of skeletal complications on
total medical care costs in patients with bone metastases of breast
cancer seen in typical clinical practice. J Support Oncol.
4:341–347. 2006.PubMed/NCBI
|
|
17
|
Pockett RD, Castellano D, McEwan P,
Oglesby A, Barber BL and Chung K: The hospital burden of disease
associated with bone metastases and skeletal-related events in
patients with breast cancer, lung cancer, or prostate cancer in
Spain. Eur J Cancer Care (Engl). 19:755–760. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schulman KL and Kohles J: Economic burden
of metastatic bone disease in the U.S. Cancer. 109:2334–2342. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Decroisette C, Monnet I, Berard H, et al:
Epidemiology and treatment costs of bone metastases from lung
cancer: a French prospective, observational, multicenter study
(GFPC 0601). J Thorac Oncol. 6:576–582. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hoefeler H, Duran I, Hechmati G, et al:
Health resource utilization associated with skeletal-related events
in patients with bone metastases: results from a multinational
retrospective - prospective observational study - a cohort from 4
European countries. J Bone Oncol. (In press).
|
|
21
|
Hechmati G, Cure S, Gouepo A, et al: Cost
of skeletal-related events in European patients with solid tumours
and bone metastases: data from a prospective multinational
observational study. J Med Econ. 16:691–700. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lüftner D, Lorusso V, Duran I, et al:
Health resource utilization associated with skeletal-related events
in patients with advanced breast cancer: results from a
prospective, multinational observational study. Submitted for
publication. 2013.
|
|
23
|
Hoefeler H, Duran I, Hechmati G, et al:
Health resource utilization (HRU) associated with skeletal-related
events (SREs) by tumour type in patients with bone
metastases/lesions: European analysis of a prospective
multinational observational study. Eur J Cancer. 47:S262–S263.
2011.
|
|
24
|
Lüftner D, Lorusso V, Duran I, et al:
Health resource utilization (HRU) associated with skeletal-related
events (SREs) in advanced breast cancer patients with bone
metastases: results from a prospective multinational observational
study. Cancer Res. 71(24 Suppl): abstract P4-16-09. 2011.
|
|
25
|
Royal College of Radiologists. Single
fraction radiotherapy for bone metastases. http://www.rcr.ac.uk/docs/oncology/pdf/bonemetsreport.pdf.
Accessed June 27, 2013
|
|
26
|
Williams MV, Summers ET, Drinkwater K and
Barrett A: Radiotherapy dose fractionation, access and waiting
times in the countries of the UK in 2005. Clin Oncol (R Coll
Radiol). 19:273–286. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Casas A, Lebret T, Cavo M, et al: Insights
into the management of bone metastases: a comprehensive European
survey. Support Care Cancer. 20:S882012.
|
|
28
|
Calderone R, Nimako K, Leary A, Popat S
and O’Brien ME: Under usage of zoledronic acid in non-small cell
lung cancer patients with metastatic bone disease - a short
communication. Eur J Cancer. 47:1603–1605. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Woll PJ, Flinois A, Schoen P, Shepherd S
and Haynes I: Insights into the management of bone metastases in
patients with lung cancer: A comprehensive European survey. Eur J
Cancer. 49:abstract 3473. 2013.
|