Introduction
The majority of the mesenchymal tumors of the
gastrointestinal tract are currently referred to as
gastrointestinal stromal tumors (GISTs). The immunohistochemical
examination commonly reveals a positive expression for CD117.
Extragastrointestinal stromal tumors (EGISTs) are mesenchymal
tumors occurring outside the gastrointestinal tract, with
histological, immunohistochemical and molecular genetic
characteristics very similar to those of GISTs (1). EGISTs are a rare clinical entity and,
to date, there has been no report of bladder EGIST in non-adult
patients. In this report, we present a mesenchymal tumor removed
from the bladder of a 15-year-old female. The patient remains alive
and disease-free 35 months after the surgery.
Case study
A 15-year-old adolescent female patient was
hospitalized following 2 weeks of painless gross hematuria with
clots. On admission, the patient had stable vital signs, a pale
appearance and no positive abdominal signs. On routine blood
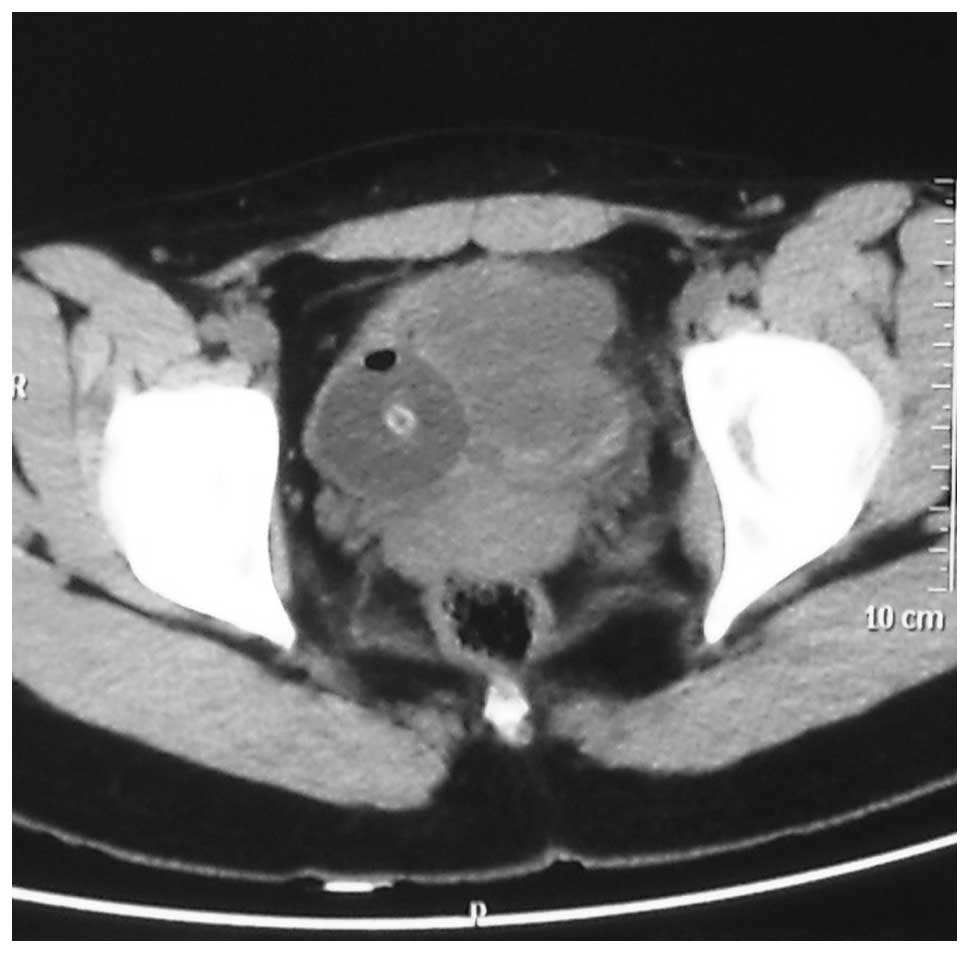
examination, the concentration of hemoglobin was 69 g/l. A B-mode
ultrasound image indicated a urinary bladder neoplasm and pelvic
computed tomography (CT) revealed an irregular soft tissue density
mass, sized 5.7×4.8 cm, in the bladder, which exhibited uneven
density and obscure boundaries (Fig.
1). The patient was subjected to partial cystectomy and the
intraoperative exploration identified a sessile tumor, sized
5.7×4.8×3 cm, in the upper wall of the bladder, which grew along
the muscular layer and broke through the mucous layer with
associated bleeding. There was no macroscopic invasion of the
ureteral opening. The remaining bladder wall was smooth and
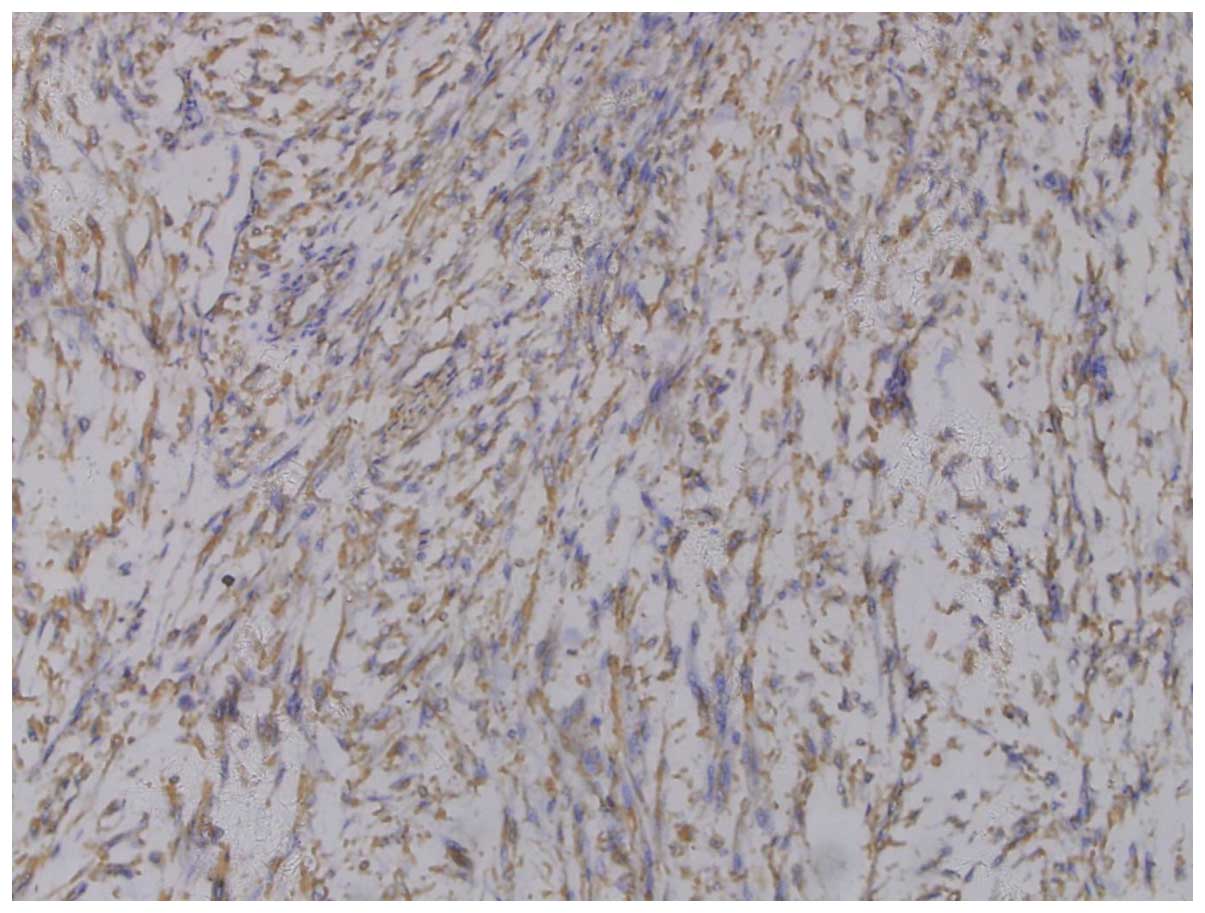
exhibited no signs of neoplasia. On postoperative pathological
examination, the tumor was composed of fusiform cells with abundant
acidophilic cytoplasm and clavate nuclei, with both ends round and
mostly blunt. The cells were mainly arranged in interwoven bundles
or swirls and were mildly atypical (Fig. 2). The mitotic count was 5 per 50
high-power fields (HPFs). Immunohistochemically, the tumor cells
strongly expressed CD117 (Fig. 3),
vimentin and smooth muscle actin, but were negative for CD34,
desmin and S-100 protein. The tumor was diagnosed as an EGIST. The
patient in this study did not receive any molecular-targeted drugs
due to financial difficulties. During follow-up, transabdoninal
ultrasonography and cystoscopic examination identified no evidence
of recurrence over the following 35 months.
Discussion
GISTs are mesenchymal tumors occurring in the
gastrointestinal tract and their development is driven by mutant
c-kit or platelet-derived growth factor receptor α genes. On
mmunohistochemical examination, GISTs exhibit positive expression
for CD117 or DOG-1. EGISTs are mesenchymal tumors occurring outside
the gastrointestinal tract, with morphological, immunophenotypic
and molecular biological characteristics very similar to those of
GISTs (1). EGISTs are a rare
clinical entity, accounting for <5% of soft tissue tumors
(2–4). Furthermore, EGISTs are even more rare
in the urinary bladder. Following a literature review, we found 5
cases of patients with bladder EGISTs, including 3 men and 2 women,
aged 34–78 years (5–9). To the best of our knowledge, the
patient in this study, aged 15 years, is the first non-adult
patient presenting with EGIST, indicating that the occurrence of
EGISTs is not limited to adults.
The clinical manifestations of EGISTs are
non-specific. EGISTs of the bladder are characterized by larger
tumor size and are mainly manifested by gross hematuria, which is
often caused by bleeding due to tumor invasion of the mucous layer.
EGISTs have no specific tumor markers. Furthermore, there are no
specific diagnostic criteria for EGISTs on imaging examinations,
such as B-mode ultrasound, CT, magnetic resonance imaging and
position emission tomography/computed tomography. The current
diagnostic criteria for EGISTs were developed according to the
immunohistochemical diagnostic criteria for GISTs, i.e.,
mesenchymal tumors occurring outside the gastrointestinal tract,
histologically consisting of fusiform, epithelioid or,
occasionally, pleomorphic cells, in a bundle-like or diffuse
arrangement; on immunohistochemical examination, the tumor cells
are usually positive for CD117 or DOG-1 expression. The main
clinical manifestation in our patient was hematuria and the lesion,
which was located in the upper wall of the urinary bladder, was
relatively large-sized and exhibited typical GIST histological
morphology. The immunohistochemical examination revealed positive
CD117 expression. Therefore, the diagnosis of EGIST was
confirmed.
EGISTs are rare and their pathogenesis has not been
fully elucidated. In this study, prompted by the GIST origin from
pacemaker cells, also referred to as the interstitial cells of
Cajal (ICC), which surround the gastrointestinal nerve plexus, we
identified ICC cells in the gastrointestinal tract, as well as
several other abdominal organs, extensively involving the bladder.
Thus, we hypothesized that ICC carcinogenesis in the bladder is a
primary cause of this disease. ICCs express the c-kit protein. The
c-kit proto-oncogene is located on human chromosome 4q11-12, of
which the product is the growth factor receptor tyrosine kinase
type III, a member of the immunoglobulin superfamily, also known as
CD117. It was previously demonstrated that c-kit is expressed at
relatively high levels in GISTs (up to 81–100%) and is more
sensitive compared to CD34 (10–12).
However, in GISTs harbouring c-kit gene mutations, the positive
rate of DOG-1 is 92% and that of CD117 is 81%, making DOG-1
comparatively a more sensitive and specific indicator. Therefore,
in cases of tumors morphologically suspicious for EGIST and
negative for CD117 expression, DOG-1 is recommended for diagnosis
(13,14).
The prognosis of EGIST appears to be related to
morphological characteristics. Generally, compared to GISTs, a
tumor may be determined as having malignant potential if it
exhibits one of the following characteristics: i) Significantly
atypical tumor cells, tumor necrosis, muscular layer invasion,
ancient coin-like growth around the vessels and mitotic count
≥10/50 HPFs; or ii) mucosal invasion, perineural invasion, fatty
infiltration, vascular invasion and lymph node metastasis. The more
common the abovementioned findings, the higher the degree of
malignancy (15,16). However, these findings are derived
from scattered onset locations and rare cases; therefore, the
association between morphological characteristics and biological
behavior requires further documentation for substantiation,
particularly evidence-based medicine.
EGISTs are considered to be refractory to
conventional radiotherapy and chemotherapy and resection is
currently the preferred treatment option. The thoroughness of
surgical treatment is closely associated with cure; therefore, a
complete excision of the tumor by properly expanding the surgical
scope is the key to EGIST treatment (17). By administering molecular-targeted
drugs, such as imatinib, as neoadjuvant and adjuvant therapy for
GISTs, small-scale clinical studies have achieved some clinical
efficacy (18). However, in
EGISTs, imatinib has been used in fewer cases; thus, our clinical
experience is limited. The majority of these drugs are used for the
prevention of EGIST relapse following surgery. The patient in our
study did not receive any molecular-targeted drugs due to financial
difficulties and there was no evidence of recurrence during
follow-up over the next 35 months. The efficacy of
molecular-targeted drugs, such as imatinib, in the treatment of
EGISTs requires further support by clinical cases in the
future.
References
|
1
|
Llenas-Garcia J, Guerra-Vales JM, Moreno
A, Ibarrola C, Castelbon FJ, Fernandez-Ruiz M, Meneu JC, Ballestin
C and Moreno E: Primary extragastrointestinal stromal tumors in the
omentum and mesentery: a clinicopathological and
immunohistochemical study. Hepatogastroenterology. 55:1002–1005.
2008.PubMed/NCBI
|
|
2
|
Miettinen M, Monihan JM, Sarlomo-Rikala M,
Kovatich AJ, Carr NJ, Emory TS and Sobin LH: Gastrointestinal
stromal tumors/smooth muscle tumors (GISTs) primary in the omentum
and mesentery: clinicopathologic and immunohistochemical study of
26 cases. Am J Surg Pathol. 23:1109–1118. 1999. View Article : Google Scholar
|
|
3
|
Reith JD, Goldblum JR, Lyles RH and Weiss
SW: Extragastrointestinal (soft tissue) stromal tumors: an analysis
of 48 cases with emphasis on histologic predictors of outcome. Mod
Pathol. 13:577–585. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fletcher CD, Berman JJ, Corless C, et al:
Diagnosis of gastrointestinal stromal tumors: A consensus approach.
Hum Pathol. 33:459–465. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lasota J, Carlson JA and Miettinen M:
Spindle cell tumor of urinary bladder serosa with phenotypic and
genotypic features of gastrointestinal stromal tumor. Arch Pathol
Lab Med. 124:894–897. 2000.PubMed/NCBI
|
|
6
|
Krokowski M, Jocham D, Choi H, Feller AC
and Horny HP: Malignant extragastrointestinal stromal tumor of
bladder. J Urol. 169:1790–1791. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mekni A, Chelly I, Azzouz H, Ben Ghorbel
I, Bellil S, Haouet S, Kchir N, Zitouna M and Bellil K:
Extragastrointestinal stromal tumor of the urinary wall bladder:
case report and review of the literature. Pathologica. 100:173–175.
2008.PubMed/NCBI
|
|
8
|
Garcia-Segui A and Gascon M:
Gastrointestinal stromal tumour in the urinary bladder. Actas Urol
Esp. 35:124–125. 2011.(In Spanish).
|
|
9
|
Shin HS, Cho CH and Kum YS:
Extragastrointestinal stromal tumor of the urinary bladder: a case
report. Urol J. 8:165–167. 2011.PubMed/NCBI
|
|
10
|
Kindblom LG, Remotti HE, Aldenborg F and
Meis-Kindblom JM: Gastrointestinal pacemaker cell tumor (GIPACT):
gastrointestinal stromal tumors show phenotypic characteristics of
the interstitial cells of Cajal. Am J Pathol. 152:1259–1269.
1998.
|
|
11
|
Hirota S, Isozaki K, Moriyama Y, et al:
Gain-of-function mutations of c-kit in human gastrointestinal
stromal tumors. Science. 279:577–580. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sircar K, Hewlett BR, Huizinga JD,
Chorneyko K, Berezin I and Riddell RH: Interstitial cells of Cajal
as precursors of gastrointestinal stromal tumors. Am J Surg Pathol.
23:377–389. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Espinosa I, Lee CH, Kim MK, et al: A novel
monoclonal antibody against DOG1 is a sensitive and specific marker
for gastrointestinal stromal tumors. Am J Surg Pathol. 32:210–218.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Long KB, Butrynski JE, Blank SD, Ebrahim
KS, Dressel DM, Heinrich MC, Corless CL and Hornick JL: Primary
extragastrointestinal stromal tumor of the pleura: report of a
unique case with genetic confirmation. Am J Surg Pathol.
34:907–912. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors: pathology and prognosis at different sites. Semin
Diagn Pathol. 23:70–83. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Joensuu H: Risk stratification of patients
diagnosed with gastrointestinal stromal tumor. Hum Pathol.
39:1411–1419. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Badalamenti G, Rodolico V, Fulfaro F, et
al: Gastrointestinal stromal tumors (GISTs): focus on
histopathological diagnosis and biomolecular features. Ann Oncol.
18(Suppl 6): vi136–vi140. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dematteo RP, Ballman KV, Antonescu CR, et
al; American College of Surgeons Oncology Group (ACOSOG) Intergroup
Adjuvant GIST Study Team. Adjuvant imatinib mesylate after
resection of localised, primary gastrointestinal stromal tumour: a
randomised, double-blind, placebo-controlled trial. Lancet.
373:1097–1104. 2009. View Article : Google Scholar
|