Introduction
Hepatocellular carcinoma (HCC) is one of the leading
causes of cancer-related mortality worldwide, with a continuously
increasing incidence (1). Surgery
and ablation and liver transplantation are the only potentially
curative treatments for HCC; however, liver transplantation is
restricted by a shortage of liver donors, with surgery and ablation
currently being the mainstay of treatment. The tumor recurrence
rate is high following liver resection or tumor ablation.
Postoperative chemoprevention with vitamin E or vitamin K2 and
intervention with 131I are used to reduce tumor
recurrence following curative treatment (2); however, there is currently no widely
accepted effective adjuvant therapy.
Recurrence may be classified as early, with 1
(3) or 2 years (4) as the cut-off point, or late
recurrence (5). Early recurrence
may be associated with dissemination of the primary HCC, whereas
late recurrence mainly results from de novo tumors arising
from the ‘field effect’ in the diseased liver (6,7).
Variables associated with metastasis are associated with early
recurrence, whereas those associated with increased carcinogenesis
contribute to late recurrence (8).
Antitumor treatment may be important in reducing early recurrence,
whereas pre- and postoperative antiviral and anti-inflammatory
treatments may be crucial in reducing both early and late
recurrence (9). The recurrence
patterns differ between hepatitis B virus (HBV) associated with HCC
(HBV-HCC) and hepatitis C virus (HCV) associated with HCC (HCV-HCC)
cases. HBV-HCC tends to involve more early recurrence due to
micrometastases not identified during surgery and HCV-HCC tends to
involve multicentric late recurrence arising from the cirrhotic
liver. The mechanisms of carcinogenesis also differ between HBV-HCC
and HCV-HCC; in HBV patients, HCC may occur without cirrhosis,
whereas cirrhosis is consistently present in patients with HCV-HCC
(10). Therefore, multistep and
multicentric HCC develops most frequently in patients with HCV
infection (11).
Interferons (IFNs) are cytokines possessing a
variety of biological properties, including antiviral,
immunomodulatory, antiproliferative and antiangiogenic effects
(12,13). IFN is effective in suppressing the
replication of HBV and was the first agent to be approved for the
treatment of chronic HBV infection (13). IFN has long been used for HCV
infection and has effectively decreased progression to liver
cirrhosis and development of HCC (14). However, the use of IFN following
curative treatment for HCC was not found to be consistently
effective and IFN is not considered as the standard adjuvant
treatment for HCC following curative treatment. Previous
meta-analyses demonstrated that IFN decreased disease recurrence
and mortality and prolonged recurrence-free survival (15–17);
however, no study has compared the different efficacies of IFN in
HBV-HCC and HCV-HCC. The present study focuses on the effect of
adjuvant IFN therapy on early and late recurrence of HCC with
different hepatitis backgrounds.
Materials and methods
Databases and searches
An electronic search was conducted through Medline,
Embase, the Cochrane Central Register of Controlled Trials
(Central) and the Database of Abstracts of Reviewers of
Effectiveness (DARE). The search was limited to the period between
January, 1998 and June, 2013, as IFN had not been approved for the
treatment of viral hepatitis prior to the late 1990s.
‘Hepatocellular carcinoma’, ‘interferon’, ‘adjuvant’, ‘resection
and ablation’ and ‘recurrence’ were used as keywords. All the
included studies were also entered in the PubMed ‘related articles’
application and the Science Citation Index to cross-search for
similarly indexed studies. Additional studies were identified from
article citations.
Data extraction and synthesis
The literature search, data extraction, evaluation
and summary were performed independently. Any disagreement was
resolved through discussion. The primary efficacy indicator was
mortality rate between the IFN treatment and the control groups,
whereas the second indicator was recurrence rate, including early
and late recurrence. Data regarding the following potential
prognostic factors, if available, were extracted from the published
reports: patient age, etiology of underlying liver disease (HBV or
HCV), types of curative therapy (surgery or ablation), tumor
characteristics, liver cirrhosis and type, dosage and duration of
IFN treatment, including cumulative dosage and average dosage per
week. We used early and late recurrence to evaluate the effect of
IFN on the tumor or the liver. Since early recurrence was defined
as 1 or 2 years postoperatively, we analyzed both 1- and 2-year
recurrence; late recurrence was defined as recurrence occurring
after 2 years. As HCC mainly develops in hepatitis virus-infected
liver, we performed a comparison between studies that enrolled
HBV-HCC and those that enrolled HCV-HCC patients.
Statistical analysis
Meta-analyses were conducted using the fixed-effects
and random-effects models and treatment effects were expressed as
risk ratios (RRs) with corresponding 95% confidence intervals (95%
CIs). If the fixed- and random-effects models produced the same
result, only the fixed-effects estimate was reported. Heterogeneity
was assessed using the χ2 statistic and the proportion
of variation attributable to heterogeneity was expressed as
I2. In the presence of significant heterogeneity
(P<0.05 for χ2), defined sources of heterogeneity
were used, which included the type of IFN (α or β), type of viral
hepatitis (HCV or HBV) and other factors. All the analyses were
conducted with Review Manager 5.2 software (Cochrane Collaboration,
Oxford, UK).
Results
Study selection and characteristics
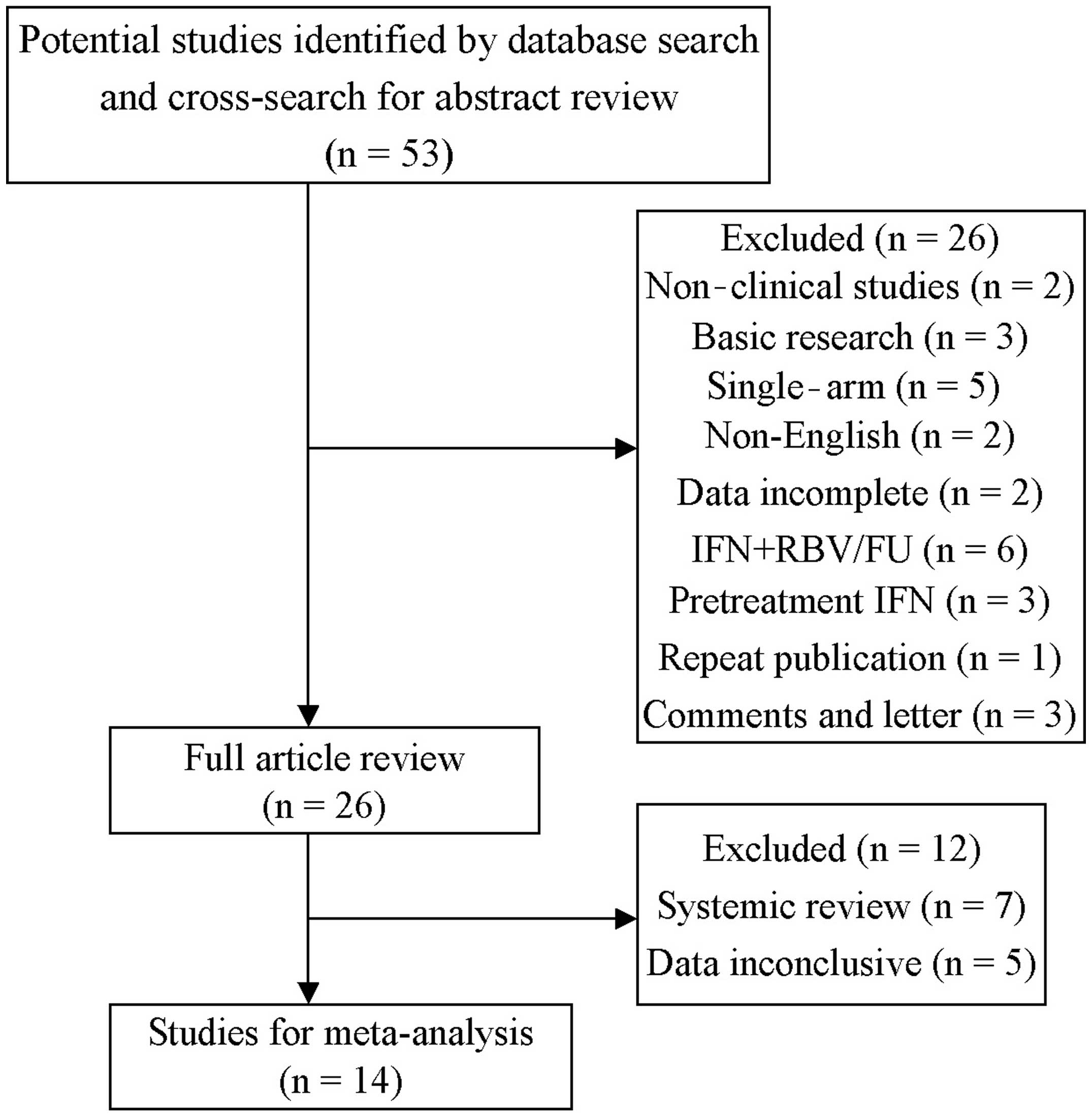
The data extraction process and the selection of
studies are outlined in Fig. 1. We
also assessed all the systemic reviews on IFN as adjuvant therapy
for HCC following curative treatment and studies that were not
initially enrolled were added. Finally, we included 14 studies,
namely 9 randomized controlled trials (RCT) and 5 case-control
studies, including a total of 1,385 patients, comparing the
recurrence and mortality rates of HCC following curative treatment,
including resection (n=5), ablation (n=5), or resection plus
ablation (n=4).
The characteristics of the studies are summarized in
Tables I and II. The sample size for each study varied
between 20 and 268 patients, with the median age varying between 49
and 68.5 years. IFN treatment included IFNα-2a, IFNα-2b, IFNα-1b,
IFNβ and pegylated IFN (PEG-IFN). The median tumor size varied
between 1.5 and 5.7 cm and the proportion of multiple tumors varied
between 0.0 and 43.8%. The incidence of vessel invasion varied
between 19.7 and 76.2% and the proportion of cirrhosis varied
between 47.0 and 100.0%. The median follow-up time was 25–85 months
(Table II).
 | Table IStudy characteristics and interferon
regimens. |
Table I
Study characteristics and interferon
regimens.
| Author (year) | Patient number
(IFN/Ctrl) | Study type | Primary
treatment | Viral
hepatitis | Type | IFN schedule | Cum. dose (MU) | Weeks | Dose/week (MU) | Median follow-up
(mo) | (Refs.) |
|---|
| Ikeda et al
(2000) | 10/10 | RCT | S/A | HCV | IFNβ | 6 MU biw × 36
wk | 432 | 36 | 12 | 25/25 | (27) |
| Kubo et al
(2002) | 15/15 | RCT | Surgery | HCV | IFNα | 6 MU qd × 2 wk+ 6
MU tiw × 14 wk+ 6 MU biw × 88 wk | 1,392 | 104 | 13 | 36/30 | (22) |
| Suou et al
(2001) | 18/22 | CS | S/A | HCV | IFNα | 6 MU qd × 2 wk+ 6
MU tiw × 22 wk | 480 | 24 | 20 | NA/NA | (37) |
| Miyaguchi et
al (2002) | 16/16 | RCT | TACE+ PEI | HCV | IFNα-2b | 3 MU tiw × 16
wk | 104 | 16 | 7 | NA | (38) |
| Shiratori et
al (2003) | 49/25 | RCT | Ablation | HCV | IFNα | 6 MU tiw × 48
wk | 864 | 48 | 18 | 85/85 | (39) |
| Lin et al
(2007) | 20/10 | RCT | Ablation |
HBV(17)/HCV(13) | IFNα-2b | 3 MU tiw × >24
wk or 3×10/mo × 6 mo+ 3×10/3 mo × 18 mo | 212/360 | 24/96 | 9/4 | 27/27 | (14) |
| Chen et al
(2012) | 133/135 | RCT | Surgery | HBV
(215)/HCV(53) | IFNα-2b | 1–5/1 wk+5 qd × 4
wk+ 5 MU tiw × 48 wk | 835 | 53 | 16 | 63.8/63.8 | (19) |
| Mazzaferro et
al (2006) | 76/74 | RCT | Surgery | HCV | IFNα-2b | 3 MU tiw × 48
wk | 432 | 48 | 9 | 45/45 | (4) |
| Sun et al
(2006) | 118/118 | RCT | Surgery | HBV | IFNα-1b | 5 MU qd × 2+ tiw ×
72 wk | 1,092 | 74 | 15 | 36.5/36.5 | (18) |
| Lo et al
(2007) | 40/40 | RCT | Surgery | HBV
(77)/HCV(3) | IFNα-2b | 10 MU/m2
tiw × 16 wk or 30 MU/m2 tiw × 16 wk | 480/1,440 | 16/16 | 30/90 | >36/>36 | (13) |
| Jeong et al
(2007a) | 42/42 | CS | S/A | HCV | IFNα | 6 MU qd × 2 wk+ 6
MU tiw × 22 wk | 480 | 24 | 20 | 37/37 | (40) |
| Jeong et al
(2007b) | 16/16 | CS | S/A | HCV | IFNα | 3 MU tiw × 48
wk | 432 | 48 | 9 | 32/31 | (20) |
| Kudo et al
(2007) | 43/84 | CS | Ablation | HCV |
IFNα-2b/PEG-IFNα-2a | Maintenance 3 MU/90
μg qw/q2wk | NA | NA | NA | NA | (21) |
| Hagihara et
al (2011) | 37/145 | CS | S/A | HCV | PEG-IFNα-2a/2 | 90–180 μg qw ×
24–48 wk (60–100 μg qw × 24–48 wk) | NA | 48 | NA | 44/44 | (41) |
 | Table IITumor characteristics and patient’
follow-up in the interferon treatment/control groups. |
Table II
Tumor characteristics and patient’
follow-up in the interferon treatment/control groups.
| Author (year) | Median age
(years) | Median size
(cm) | Multiple (%) | Vessel invasion
(%) | Cirrhosis (%) | Median follow-up
(months) | 1-year rec.
(n) | 2-year rec.
(n) | >2-year rec.
(n) | No. of deaths | Mortality rate
(%) | (Refs.) |
|---|
| Ikeda et al
(2000) | 60/64.5 | 2.2/2 | 10/10 | 0/0 | 80/90 | 25/25 | 0/5 | 0/7 | 1/0 | 0/0 | 0.0/0.0 | (27) |
| Kubo et al
(2002) | 61.9/60 | 2.5/2.6 | 0/0 | NA | 47/53 | 36/30 | 1/3 | 5/6 | 0/6 | 8/10 | 53.3/66.7 | (22) |
| Suou et al
(2001) | 61/62 | 2/2.1 | 0/0 | NA | NA | NA | 1/3 | 2/7 | 2/8 | 0/6 | 0.0/27.3 | (37) |
| Miyaguchi et
al (2002) | 66.2/65 | 2.8/2.4 | 27.2/33 | NA | 100/100 | NA | 3/10 | 3/14 | 1/0 | NA | NA | (38) |
| Shiratori et
al (2003) | 61/63 | 2.2/2.3 | 34.7/36 | NA | 100/100 | 85/85 | 12/6 | 25/17 | 15/6 | 19/13 | 38.8/52.0 | (39) |
| Lin et al
(2007) | 61.3/59 | 2/2.5 | 15/20 | NA | 90/100 | 27/27 | 56/4 | 5/6 | 3/3 | 4/5 | 20.0/50.0 | (14) |
| Chen et al
(2012) | 50/49 | 3.5/3 | 21.5/14.8 | 30.8/24.4 | 53.8/55.2 | 63.8/63.8 | 37/35 | 51/55 | 27/21 | 43/41 | 32.3/30.4 | (19) |
| Mazzaferro et
al (2006) | 65/67 | 3.4/3.2 | 22.4/25.7 | 19.7/23.0 | 94/88 | 45/45 | 25/24 | 40/39 | 4/8 | 17/23 | 22.4/31.1 | (4) |
| Sun et al
(2006) | 52.2/50.4 | 4.3/4.9 | 13.6/12.7 | 76.2/75.4 | 83/88.1 | 36.5/36.5 | 32/49 | 52/62 | 15/9 | 38/60 | 32.2/50.8 | (18) |
| Lo et al
(2007) | 52/51 | 5.5/5.7 | 17/27 | 48/35 | 48/83 | >36/>36 | 2/6 | 17/20 | 4/2 | 8/13 | 20.0/32.5 | (13) |
| Jeong et al
(2007a) | 62/63 | 2/1.5 | 28.6/14.3 | NA | 70.2/75.8 | 37/37 | 0/2 | 9/13 | 11/17 | 2/12 | 4.8/28.6 | (19) |
| Jeong et al
(2007b) | 68.5/67.5 | 1.5/1.8 | 43.8/37.5 | NA | 100/100 | 32/31 | 2/1 | 7/11 | 1/2 | 1/6 | 6.3/37.5 | (40) |
| Kudo et al
(2007) | 65/66 | 1.8/1.5 | 19/23 | NA | 70.2/75.8 | NA | 2/6 | 12/13 | 12/17 | 6/37 | 14.0/44.0 | (21) |
| Hagihara et
al (2011) | 63/67 | 1.8/2 | 28/28 | NA | NA | 44/44 | 5/33 | 17/76 | 1/25 | 2/49 | 5.4/33.8 | (41) |
IFN regimen
A total of 12 studies used IFNα (6 studies used
IFNα-2b, 1 used IFNα-1b and 5 used what was only referred to as
IFNα), 1 study used IFNβ, 2 used PEG-IFNα-2a and 1 used
PEG-IFNα-2b. The schedules of IFN administration were also
distinct, ranging between 1 and 3 times per week. The cumulative
dosage of IFN varied between 104 and 1,440 million units (MU), the
duration of IFN treatment varied from 16 to 104 weeks and some
studies used IFN without discontinuation. The average dosage per
week varied between 4 and 90 MU (Table
I).
Treatment efficacy
In all the studies investigating HBV-HCC and
HCV-HCC, we analyzed mortality rates and 1- and 2-year recurrence
rates. For mortality rate analysis, data from one study were
unavailable; therefore, a total of 14 studies with 1,385 patients
were finally included. IFN treatment significantly reduced the risk
of mortality (pooled RR=0.60; 95% CI: 0.50–0.71; P<0.00001)
(Fig. 2A). The statistical
heterogeneity (I2=54%; P=0.01 for χ2) may be
partly explained by the study of Chen et al (19), which is the only study reporting
that IFN did not reduce the mortality rate for HCC. When this study
was excluded from the analysis, the heterogeneity was not
statistically significant (I2=36%; P=0.10 for
χ2) (data not shown) and the efficacy of IFN was similar
among studies.
HCC recurrence was classified as early and late,
with the cut-off point for early recurrence varying between 1 and 2
years. We analyzed early (1- and 2-year) and late recurrence (>2
years). A total of 14 studies, including 1,385 patients, were used
for the assessment of early and late recurrence and IFN treatment
was found to significantly reduce the risk of 1-year recurrence
(pooled RR=0.76; 95% CI: 0.62–0.92; P=0.005). The heterogeneity was
not significant (I2=3%; P=0.42 for χ2)
(Fig. 2B).
IFN treatment significantly reduced the risk of
2-year recurrence (pooled RR=0.77; 95% CI: 0.68–0.87; P<0.0001).
The heterogeneity was not statistically significant
(I2=33%; P=0.11 for χ2) (Fig. 2C).
IFN treatment did not significantly reduce the risk
of late recurrence (recurrence >2 years; pooled RR=0.91; 95% CI:
0.71–1.17; P=0.45). The heterogeneity was marginally statistically
significant (I2=35%; P=0.09 for χ2) (Fig. 2D).
Subgroup analysis according to type of
hepatitis virus
As HBV-HCC and HCV-HCC exhibited different
characteristics in the carcinogenesis of HCC, we performed a
subgroup analysis according to different types of hepatitis. In
studies that enrolled only patients with HCV-HCC, IFN reduced the
mortality and recurrence rates, including both early and late
recurrence (Fig. 3). IFN reduced
mortality rate (pooled RR=0.44; 95% CI: 0.34–0.58; P<0.00001)
and the heterogeneity was not significant (I2=48%;
P=0.05 for χ2) (Fig.
3A). IFN also decreased 1-year early recurrence rate (pooled
RR=0.69; 95% CI: 0.51–0.93; P=0.02) (Fig. 3B) and 2-year recurrence rate
(pooled RR=0.69; 95% CI: 0.58–0.82; P<0.0001) (Fig. 3C). Moreover, late recurrence rate
was also significantly decreased (pooled RR=0.68; 95% CI:
0.49–0.94; P=0.02) (Fig. 3D).
In studies enrolling only patients with HBV-HCC, IFN
only reduced the mortality rate (pooled RR=0.79; 95% CI: 0.63–0.98;
P=0.03). However, early recurrence rates were not significantly
reduced at 1-year (pooled RR=0.82; 95% CI: 0.64–1.05; P=0.12) or at
2-years (pooled RR=0.89; 95% CI: 0.74–1.08; P=0.24). Additionally,
the late recurrence rate was not reduced with IFN treatment (pooled
RR=1.45; 95% CI: 0.96–2.20; P=0.08) (Fig. 4).
We further compared the clinicopathological data for
HBV-HCC and HCV-HCC patients and found that patients with HBV-HCC
had larger tumors, a higher proportion of single tumors and more
tumors with vascular invasion; however, these patients had less
severe liver cirrhosis, indicating that HBV-HCC was more aggressive
and that liver cirrhosis in HBV-HCC was less severe compared to
that in HCV-HCC (Table III).
 | Table IIIComparison of clinicopathological
characteristics between HBV-HCC and HCV-HCC cases. |
Table III
Comparison of clinicopathological
characteristics between HBV-HCC and HCV-HCC cases.
|
Characteristics | Group | HBV-HCCa, median (range) | HCV-HCCb, median (range) |
|---|
| Tumor size
(cm) | IFN | 3.9 (2.5–5.5) | 2 (1.5–3.4) |
| Control | 3.95 (2.1–5.7) | 2.1 (1.5–2.6) |
| Multiple tumors
(%) | IFN | 17.5 (17–21.5) | 27.2 (10–43.8) |
| Control | 15.9 (12.7–27) | 25.7 (10–37.5) |
| Vascular invasion
(%) | IFN | 48 (30.8–76.2) | 19.7b |
| Control | 35 (24.4–75.4) | 23b |
| Cirrhosis (%) | IFN | 53.8 (48–83) | 90 (47–100) |
| Control | 83 (44.2–88.1) | 90 (53–100) |
Since IFN did not reduce the recurrence rate in
HBV-HCC, we performed further analyses of individual studies and
found that in the study by Lo et al (13), IFN significantly reduced the
recurrence rate in patients with TNM stage III/IVA, indicating the
direct antitumor effect of IFN. In the study by Sun et al
(18), IFN significantly prolonged
disease-free survival, although the tumor recurrence rate was not
decreased. However, in the study by Chen et al (19), IFN neither prolonged survival nor
reduced the mortality or recurrence rates, which may be
attributable to the obvious bias in that study, with the IFN group
exhibiting more unfavorable tumor characteristics, such as larger
tumors (3.5 vs. 3.0 cm), multiple tumors (21.5 vs. 14.8%) and high
incidence of microvascular invasion (30.8 vs. 24.4%). Liver traits,
such as hepatitis activity, were also more severe in the IFN group
(hepatitis activity, 63.9 vs. 51.1%). However, information
regarding TNM staging for both groups was unavailable, making
subset analysis of TNM staging impossible.
Second recurrence and prognosis of
patients with recurrent tumors
The reduction in mortality rate by IFN is associated
with its inhibition of recurrence; a number of studies have
reported that recurrent tumors after adjuvant IFN therapy are more
likely to receive potentially curative treatment. Jeong et
al (20) demonstrated that the
second recurrence rate was significantly lower in the IFN compared
to that in the non-IFN group. Kudo et al (21) also demonstrated that, in
IFN-treated patients, all the recurrent tumors were single and
<2.0 cm in diameter and could be completely retreated by
radiofrequency ablation in all the cases. However, in the control
group, recurrent tumors tended to be multiple and the majority were
incurable by local therapy. Kubo et al (22) reported that recurrent tumors in the
IFN group were mostly single, but in the control group multiple
tumors were more common. Sun et al (18) demonstrated that the median overall
survival rate of patients with tumor recurrence was longer in the
IFNα compared to that in the control group.
Bias analysis
One study used IFNβ, whereas other studies
exclusively used IFNα, including IFNα in 6, IFNα-2b in 6, IFNα-2a
in 2, IFNα-1b in 1 and PEG-IFNα in 2 studies. The cumulative dosage
varied between 104 and 1,440 MU, the duration of the IFN treatment
varied from 4 months to 2 years. We also calculated dosage per
week, which varied 4–90 MU/week. The withdrawal rate varied between
0 and 17.1% and adverse effects were common in the IFN group. We
did not analyze side effects, due to the heterogeneity of the data.
In the study by Mazzaferro et al (4), only 28 of the 76 patients in the IFN
group were adherent to the protocol according to definition,
reflecting poor compliance.
Other systemic reviews or
meta-analyses
Breitenstein et al (23) reported that IFN significantly
reduced the 2-year mortality rate following curative treatment of
HCC (pooled RR=0.65; 95% CI: 0.52–0.80; P<0.001) in the absence
of any significant heterogeneity (I2=0%; P=0.823 for
χ2). The effect on reduction of tumor recurrence was
less pronounced, but still significant (pooled RR=0.86; 95% CI:
0.76–0.97; P=0.013). Zhang et al (24) reported that IFN significantly
reduced early recurrence (1–1.5 years after surgery) and 1-year
survival. Zhong et al (2)
reported that IFN significantly reduced 2-year recurrence and
2-year overall survival. Shen et al (16) demonstrated that adjuvant IFN
prolonged 1-, 2- and 3-year recurrence-free survival rates of
patients with HCC. However, all the meta-analyses included patients
with HBV-HCC and patients with HCV-HCC and stratification according
to different types of hepatitis was lacking.
Discussion
The present study systematically reviewed the
published RCTs and cohort studies on adjuvant IFN therapy for HCC
and found that IFN significantly reduced the mortality and early
recurrence rates (1- and 2-year) of HCC following curative
treatment; however, IFN treatment did not reduce late (>2 years)
recurrence. Furthermore, the effect of IFN on HCC with a different
hepatitis background varied. In HCV-HCC cases, IFN reduced the
mortality and recurrence rates, including both early and late
recurrence. However, in HBV-HCC cases, IFN only reduced the
mortality rate, whereas neither early nor late recurrence rates
were reduced. Further analysis demonstrated that tumors associated
with HBV-HCC were more aggressive compared to tumors associated
with HCV-HCC and HCV-HCC was associated with more severe cirrhosis
compared to HBV-HCC.
The effects of IFN on HCC are affected by several
factors, including antitumor, antiviral, antiangiogenic and
modulatory inflammatory factors or hepatic stellate cells in the
tumor microenvironment (12,23).
IFN is currently the standard therapy for HCV infection and has
also been proven to inhibit HCC development in HCV patients through
clearance of HCV RNA, improving the degree of inflammation and
preventing worsening of compensated cirrhosis (25). However, the preferred treatment
option for the majority of patients with HBV infection is not IFN,
but rather nucleotide/nucleoside analogs (NA). A previous
meta-analysis demonstrated that NA treatment achieved a more
profound reduction in HCC risk compared to IFN, which produced only
a modest effect (78 vs. 34%, repectively) (26). Since a high viral load is the most
important factor leading to cirrhosis and cancer development in the
liver, the more effective reduction in HCC risk may be associated
with the more profound effects of viral suppression with oral
antiviral agents compared to IFN.
IFN in HCV-HCC reduced both early and late
recurrence. IFN reduced early recurrence by directly inhibiting
tumor metastasis. Ikeda et al (27) found that IFNβ significantly reduced
early recurrence of pure HCV-HCC through a direct antitumor effect.
Both IFNα and IFNβ are type I IFNs, share the same IFN receptors
and have several similar biological functions, although the direct
antitumor effect of IFNα is weaker. However, the efficacy of IFN in
reducing early recurrence of HCV-HCC may also be associated with
its antiviral and anti-inflammatory effects, as microenvironmental
factors (28) have been found to
contribute to tumor micrometastasis and IFN may reduce early
recurrence by improving the microenvironment. IFN improves liver
function and relieves liver cirrhosis, which lead to a decrease in
late recurrence. IFN was found to reduce transaminase levels and to
improve liver function and liver cirrhosis. In the present study,
liver cirrhosis was more severe in HCV-HCC compared to that in
HBV-HCC patients. The benefits of antiviral therapy for reducing
late recurrence of HCC have already been accepted by several
investigators, as there are data suggesting that antiviral therapy
may modulate the pro-oncogenic field effect in the liver. Kubo
et al (22) reported
increased albumin and decreased alanine transaminase and total
bilirubin levels in IFN-treated patients, indicating improved liver
function. In the study by Mazzaferro et al (4), early (within 2 years) and late
recurrences were analyzed separately and the only significant
result was observed for late recurrences among HCV-pure patients
(P=0.032). Huang et al (29) proved the feasibility of
PEG-IFN/ribavirin therapy with current treatment guidelines in
chronic HVC patients after successful eradication of HCC.
IFN did not reduce recurrence rates in HBV-HCC for
two main reasons. First, IFN is not the preferred antiviral
treatment option for the majority of patients with HBV infection.
High viral load is recognized as one of the key risk factors for
HBV-HCC recurrence following resection (30) and antiviral treatment with NA has
been proven to significantly decrease early recurrence of HBV-HCC
(31). Since early HBV-DNA
suppression with antiviral treatment improved the prognosis of
patients with HBV-HCC (32) and
since IFN has been reported to be more effective in responders
compared to non-responders, it is important to monitor serum HBV
DNA levels prior to and following surgery and/or ablation of HCC
and to evaluate its association with recurrence. IFN plus NA
administered in an adjuvant setting may be more promising. Second,
there may be subgroups of patients who are sensitive to IFN
therapy. Evidence has demonstrated that IFN exerts direct antitumor
effects. IFNα/β exerted direct antitumor effects on HBV-HCC
independent of hepatitis status and liver inflammation (33,34).
Lo et al (13) reported
that IFN was more effective in TNM stage III/IVA patients,
indicating that IFN exerts direct antitumor effects. Moreover, Qian
et al (35) reported that
IFN only reduced tumor recurrence in patients with P48-positive
tumors. More recently, Ji et al (36) observed that patients whose tumors
exhibited low miR-26 expression had shorter overall survival, but a
better response to IFN therapy compared to patients whose tumors
exhibited a high expression of miR-26. Therefore, personalized
treatment should be administered to HBV-HCC patients according to
specific tumor markers, such as P48 or miR-26.
Subset analyses of individual studies suggested that
IFN should be administered for longer periods of time, as it may
not only reduce recurrence rates, but also increase the possibility
of receiving curative treatment after tumor recurrence. In the
study by Sun et al (18),
during the first 18 months after resection (the planned duration
for IFNα treatment), the recurrence rate in the control group was
higher compared to that in the IFNα treatment group [49.2% (58/118)
vs. 36.4% (43/118)]; P=0.0485 for χ2], but the
recurrence rates after the first 18 months were not significantly
different between the two groups [23.2% (13/56) vs. 32.9% (24/73);
P=0.2292 for χ2]. Lo et al (13) used high-dose IFN for 6 months after
surgery and recorded 10 recurrence events in the control group and
3 recurrence events in the IFN group during 6 months of treatment,
12 recurrence events in the control group during 12 months of
treatment and 9 recurrence events in the IFN group after 12 months
of treatment. Thereafter, after another 6 months, there were 12
recurrence events in the control and 12 recurrence events in the
IFN group, indicating that IFN should be administered over a longer
period of time.
This study has several limitations. The included
studies used surgery, ablation or surgery and ablation.
Furthermore, there were only a few RCTs, they were all from a
single center instead of multiple centers and most of the published
studies had small sample sizes. The types of IFN and IFN regimens
used in the published studies varied widely regarding total dosage,
average dosage per week and treatment duration. Long-term IFN, such
as PEG-IFN, as well as short-term IFN, were used and certain
studies used IFNα or IFNβ or IFNα-1b and IFNα-2b. Further clinical
trials should use a standardized IFN regimen to yield more
comparable results. Other limitations are that the side effects of
IFN were not investigated and the dropout ratio was not described.
The side-effects of IFNα are dose-dependent and may be severe. Lo
et al (13) reported that
minor influenza-like side effects were so frequent that double
blinding in their study was not possible. In the study by
Mazzaferro et al (4), the
withdrawal rate was extremely high, which may be the reason for its
negative results. In addition, the quantification and monitoring of
the serum levels of HBV DNA and HCV RNA were unavailable in the
majority of the studies and we were unable to evaluate the
association between viral inhibition and the efficacy of IFN.
Finally, study-related bias was significant in certain studies.
In conclusion, our study demonstrated that the
effect of adjuvant IFN following curative treatment for HCC
differed between HBV-HCC and HCV-HCC; therefore, different
strategies with IFN in an adjuvant setting should be used to treat
HCCs with different hepatitis backgrounds. For HCV-HCC, IFN with an
additional antiviral treatment, such as ribavirin, may be
promising. However, in HBV-HCC, individualized therapy according to
specific molecular markers may be necessary prior to IFN treatment,
while antiviral drugs combinations may be required for patients
with high viral loads.
Acknowledgements
This study was funded by a grant from the National
Natural Science Foundation of China (no. 81101871).
References
|
1
|
Jemal A, Bray F, Center MM, et al: Global
cancer statistics. CA Cancer J Clin. 61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Zhong JH, Li H, Li LQ, et al: Adjuvant
therapy options following curative treatment of hepatocellular
carcinoma: a systematic review of randomized trials. Eur J Surg
Oncol. 38:286–295. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Poon RT, Fan ST, Ng IO, et al: Different
risk factors and prognosis for early and late intrahepatic
recurrence after resection of hepatocellular carcinoma. Cancer.
89:500–507. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mazzaferro V, Romito R, Schiavo M, et al:
Prevention of hepatocellular carcinoma recurrence with
alpha-interferon after liver resection in HCV cirrhosis.
Hepatology. 44:1543–1554. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Llovet JM, Burroughs A and Bruix J:
Hepatocellular carcinoma. Lancet. 362:1907–1917. 2003. View Article : Google Scholar
|
|
6
|
Chen L, Zhang Q, Chang W, et al: Viral and
host inflammation-related factors that can predict the prognosis of
hepatocellular carcinoma. Eur J Cancer. 48:1977–1987. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wu JC, Huang YH, Chau GY, et al: Risk
factors for early and late recurrence in hepatitis B-related
hepatocellular carcinoma. J Hepatol. 51:890–897. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Imamura H, Matsuyama Y, Tanaka E, et al:
Risk factors contributing to early and late phase intrahepatic
recurrence of hepatocellular carcinoma after hepatectomy. J
Hepatol. 38:200–207. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hoshida Y: Risk of recurrence in hepatitis
B-related hepatocellular carcinoma: impact of viral load in late
recurrence. J Hepatol. 51:842–844. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Clavien PA: Interferon: the magic bullet
to prevent hepatocellular carcinoma recurrence after resection? Ann
Surg. 245:843–845. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oikawa T, Ojima H, Yamasaki S, et al:
Multistep and multicentric development of hepatocellular carcinoma:
histological analysis of 980 resected nodules. J Hepatol.
42:225–229. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang L, Wu WZ, Sun HC, et al: Mechanism of
interferon alpha on inhibition of metastasis and angiogenesis of
hepatocellular carcinoma after curative resection in nude mice. J
Gastrointest Surg. 7:587–594. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lo CM, Liu CL, Chan SC, et al: A
randomized, controlled trial of postoperative adjuvant interferon
therapy after resection of hepatocellular carcinoma. Ann Surg.
245:831–842. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lin SM, Yu ML, Lee CM, et al: Interferon
therapy in HBeAg positive chronic hepatitis reduces progression to
cirrhosis and hepatocellular carcinoma. J Hepatol. 46:45–52. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miyake Y, Takaki A, Iwasaki Y and Yamamoto
K: Meta-analysis: interferon-alpha prevents the recurrence after
curative treatment of hepatitis C virus-related hepatocellular
carcinoma. J Viral Hepat. 17:287–292. 2010. View Article : Google Scholar
|
|
16
|
Shen YC, Hsu C, Chen LT, et al: Adjuvant
interferon therapy after curative therapy for hepatocellular
carcinoma (HCC): a meta-regression approach. J Hepatol. 52:889–894.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Singal AK, Salameh H, Kuo YF and Fontana
RJ: Meta-analysis: the impact of oral anti-viral agents on the
incidence of hepatocellular carcinoma in chronic hepatitis B.
Aliment Pharmacol Ther. 38:98–106. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sun HC, Tang ZY, Wang L, et al:
Postoperative interferon alpha treatment postponed recurrence and
improved overall survival in patients after curative resection of
HBV-related hepatocellular carcinoma: a randomized clinical trial.
J Cancer Res Clin Oncol. 132:458–465. 2006. View Article : Google Scholar
|
|
19
|
Chen LT, Chen MF, Li LA, et al: Long-term
results of a randomized, observation-controlled, phase III trial of
adjuvant interferon alpha-2b in hepatocellular carcinoma after
curative resection. Ann Surg. 255:8–17. 2012. View Article : Google Scholar
|
|
20
|
Jeong S, Aikata H, Katamura Y, et al:
Low-dose intermittent interferon-alpha therapy for HCV-related
liver cirrhosis after curative treatment of hepatocellular
carcinoma. World J Gastroenterol. 13:5188–5195. 2007. View Article : Google Scholar
|
|
21
|
Kudo M, Sakaguchi Y, Chung H, et al:
Long-term interferon maintenance therapy improves survival in
patients with HCV-related hepatocellular carcinoma after curative
radiofrequency ablation. A matched case-control study. Oncology.
72(Suppl 1): 132–138. 2007. View Article : Google Scholar
|
|
22
|
Kubo S, Nishiguchi S, Hirohashi K, et al:
Randomized clinical trial of long-term outcome after resection of
hepatitis C virus-related hepatocellular carcinoma by postoperative
interferon therapy. Br J Surg. 89:418–422. 2002. View Article : Google Scholar
|
|
23
|
Breitenstein S, Dimitroulis D, Petrowsky
H, et al: Systematic review and meta-analysis of interferon after
curative treatment of hepatocellular carcinoma in patients with
viral hepatitis. Br J Surg. 96:975–981. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang CH, Xu GL, Jia WD and Ge YS: Effects
of interferon alpha treatment on recurrence and survival after
complete resection or ablation of hepatocellular carcinoma: a
meta-analysis of randomized controlled trials. Int J Cancer.
124:2982–2988. 2009. View Article : Google Scholar
|
|
25
|
Nishiguchi S, Kuroki T, Nakatani S, et al:
Randomised trial of effects of interferon-alpha on incidence of
hepatocellular carcinoma in chronic active hepatitis C with
cirrhosis. Lancet. 346:1051–1055. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sung JJ, Tsoi KK, Wong VW, et al:
Meta-analysis: treatment of hepatitis B infection reduces risk of
hepatocellular carcinoma. Aliment Pharmacol Ther. 28:1067–1077.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ikeda K, Arase Y, Saitoh S, et al:
Interferon beta prevents recurrence of hepatocellular carcinoma
after complete resection or ablation of the primary tumor-A
prospective randomized study of hepatitis C virus-related liver
cancer. Hepatology. 32:228–232. 2000. View Article : Google Scholar
|
|
28
|
Budhu A, Forgues M, Ye QH, et al:
Prediction of venous metastases, recurrence, and prognosis in
hepatocellular carcinoma based on a unique immune response
signature of the liver microenvironment. Cancer Cell. 10:99–111.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Huang JF, Yu ML, Huang CF, et al: The
efficacy and safety of pegylated interferon plus ribavirin
combination therapy in chronic hepatitis C patients with
hepatocellular carcinoma post curative therapies - a multicenter
prospective trial. J Hepatol. 54:219–226. 2011. View Article : Google Scholar
|
|
30
|
Hung IF, Poon RT, Lai CL, et al:
Recurrence of hepatitis B-related hepatocellular carcinoma is
associated with high viral load at the time of resection. Am J
Gastroenterol. 103:1663–1673. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yin J, Li N, Han Y, et al: Effect of
antiviral treatment with nucleotide/nucleoside analogs on
postoperative prognosis of hepatitis B virus-related hepatocellular
carcinoma: a two-stage longitudinal clinical study. J Clin Oncol.
31:3647–3655. 2013. View Article : Google Scholar
|
|
32
|
Huang G, Yang Y, Shen F, et al: Early
viral suppression predicts good postoperative survivals in patients
with hepatocellular carcinoma with a high baseline HBV-DNA load.
Ann Surg Oncol. 20:1482–1490. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yang JQ, Pan GD, Chu GP, et al:
Interferon-alpha restrains growth and invasive potential of
hepatocellular carcinoma induced by hepatitis B virus X protein.
World J Gastroenterol. 14:5564–5569. 2008. View Article : Google Scholar
|
|
34
|
Yamazaki K, Suzuki K, Ohkoshi S, et al:
Temporal treatment with interferon-beta prevents hepatocellular
carcinoma in hepatitis B virus X gene transgenic mice. J Hepatol.
48:255–265. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Qian YB, Zhang JB, Wu WZ, et al: P48 is a
predictive marker for outcome of postoperative interferon-alpha
treatment in patients with hepatitis B virus infection-related
hepatocellular carcinoma. Cancer. 107:1562–1569. 2006. View Article : Google Scholar
|
|
36
|
Ji J, Shi J, Budhu A, et al: MicroRNA
expression, survival, and response to interferon in liver cancer. N
Engl J Med. 361:1437–1447. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Suou T, Mitsuda A, Koda M, et al:
Interferon alpha inhibits intrahepatic recurrence in hepatocellular
carcinoma with chronic hepatitis C: a pilot study. Hepatol Res.
20:301–311. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Miyaguchi S, Watanabe T, Takahashi H, et
al: Interferon therapy for hepatocellular carcinoma patients with
low HCV-RNA levels. Hepatogastroenterology. 49:724–729.
2002.PubMed/NCBI
|
|
39
|
Shiratori Y, Shiina S, Teratani T, et al:
Interferon therapy after tumor ablation improves prognosis in
patients with hepatocellular carcinoma associated with hepatitis C
virus. Ann Intern Med. 138:299–306. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jeong SC, Aikata H, Katamura Y, et al:
Effects of a 24-week course of interferon-alpha therapy after
curative treatment of hepatitis C virus-associated hepatocellular
carcinoma. World J Gastroenterol. 13:5343–5350. 2007. View Article : Google Scholar
|
|
41
|
Hagihara H, Nouso K, Kobayashi Y, et al:
Effect of pegylated interferon therapy on intrahepatic recurrence
after curative treatment of hepatitis C virus-related
hepatocellular carcinoma. Int J Clin Oncol. 16:210–220. 2011.
View Article : Google Scholar
|