Introduction
The word parotid is derived from the greek word
‘parotis’, which means para (near) and otis (ear). The parotid
gland has been extensively investigated and there are numerous
published studies on the pathology of this gland worldwide. It was
estimated that salivary gland tumours comprise ~3–10% of all
neoplasms of the head and neck (1), with an incidence estimated at
0.4–13.5% annually per 100,000 individuals worldwide (2). The majority (80%) of these tumours
originate in the parotid gland, with an incidence of 66–80% for
benign and 20–34% for malignant lesions. A recent study conducted
by Shrestha et al (3) at
B.P. Koirala Memorial Cancer Hospital in Nepal, reported these new
statistics on salivary gland tumours based on a total of 34,978
biopsies. The highest incidence for benign lesions was in the
3rd-4th and for malignant lesions in the 4th-5th decades of life,
with a male predominance (63.6% of all cases). Mucoepidermoid
carcinoma was the most common malignant tumour of the parotid
gland, accounting for 23.6% of all malignant salivary gland tumours
in that series, followed by adenoid cystic carcinoma (9%), acinic
cell carcinoma (7.2%), adenocarcinoma not otherwise specified
(6.3%), carcinoma ex pleomorphic adenoma (5.4%), unclassified
tumours (4.5%), squamous cell carcinoma (3.6%), basal cell
carcinoma (1.8%), polymorphous low-grade adenocarcinoma (1.8%) and
metastatic undifferentiated carcinoma (1.8%). Survival as quoted by
the American Cancer Society varies depending on stage, with a
5-year survival rate of 91% for stage I, 75% for stage II, 65% for
stage III and 39% for stage IV disease (4). The prognosis is extremely good in
children, with a survival rate of ~100%. As regards the available
literature in the Caribbean region, there are only a few studies
from Jamaica, South America and Cuba. To the best of our knowledge,
this is the first study on parotid gland pathology from Trinidad
and Tobago and it may serve as a platform for further research and
development in this area.
Materials and methods
Data collection
Retrospective data on all the cases of parotid
tumour surgery between October, 2003 and February, 2012 were
collected from the electronic records of the Department of
Pathology at the Port-of-Spain General Hospital (POSGH), Trinidad
and Tobago. Demographic information regarding date of surgery,
patient age and gender, hospital of origin, morphological and
histological characteristics of the specimen, were collected and
retrospectively analyzed. Pathological data from POSGH, Sangre
Grande District General Hospital (SGH) and Scarborough Regional
Hospital (SRH) in Tobago were also included in this study.
Ethics approval was granted from the relevant
authorities and the data were analyzed using SPSS® statistics,
version 20 (IBM SPSS, Armonk, NY, USA).
Types of tumours
Histological information was collected and
classified by type of tumour. The benign lesions included
pleomorphic adenoma, Warthin's tumour (adenolymphoma) and
monomorphic adenoma and the malignant tumours included
mucoepidermoid carcinoma, adenocarcinoma, acinic cell carcinoma and
squamous cell carcinoma.
Results
Patients
Data from 60 parotid tumour patients between
October, 2003 and February, 2012 were retrospectively collected
from the pathology records at POSGH, Trinidad and Tobago. Our
sample comprised 56 primary lesions, 1 basal cell carcinoma of the
skin infiltrating the gland and 3 metastatic tumours. The patients
included 31 men and 29 women, with a mean age of 48.7 years, a
median of 51.5 years and a mode of 56 years (range, 21–73
years).
Age distribution and annual
incidence
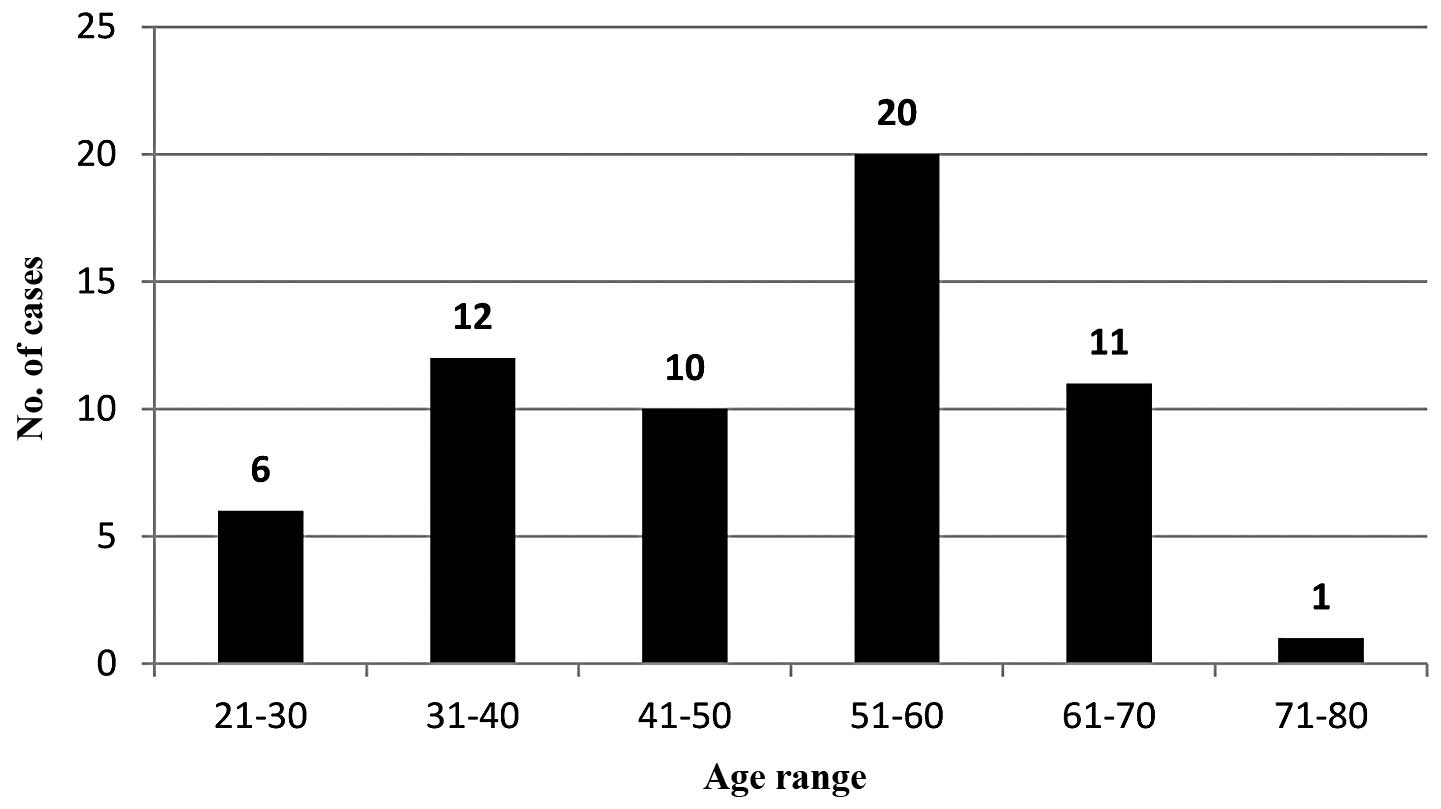
The age range distribution was as follows: 21–30, 6
(10%); 31–40, 12 (20%); 41–50, 10 (13.3%); 51–60, 20 (33.3%);
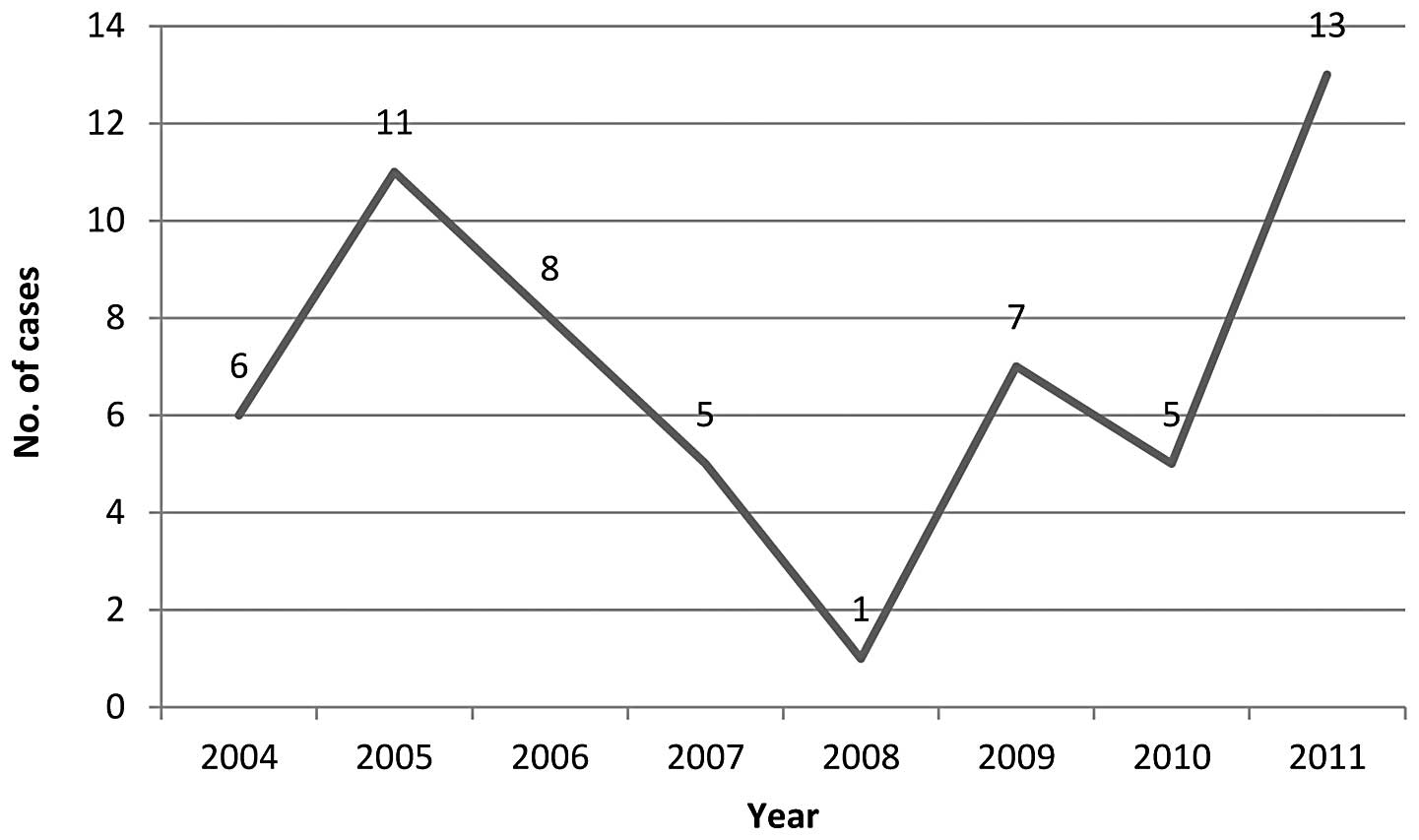
61–70, 11 (18.3%); and 71–80, 1 (1.7%) (Fig. 1). The number of new primary cases
per year was as follows: 2004, 6; 2005, 11; 2006, 8; 2007, 5; 2008,
1; 2009, 7; 2010, 5; and 2011, 13 (Fig. 2).
Surgical approach and tumour
types
Of the 60 cases, 53 (88.3%) were from POSGH and 7
from SGH, whereas there were no cases from SRH. The surgical
procedures included 53 superficial parotidectomies, 6 radical
parotidectomies and 1 parotid biopsy. The primary tumours comprised
56 cases in total, excluding 1 basal cell carcinoma and 3
metastatic lesions. The benign lesions included 34 pleomorphic
adenomas and 7 Warthin's tumours, accounting for 73.2% of the 56
primary tumours.
Benign lesions
For pleomorphic adenomas, the mean patient age was
47 years (range, 27–73 years). The peak age groups affected
included the 3rd and 5th decades of life, accounting for 29 and 32%
of patients, respectively, with female patients accounting for 65%
of these cases.
As regards Warthin's tumours, the age range was
44–68 years, with a mean of 55 years. The peak age groups affected
included the 4th, 5th and 6th decades of life, accounting for 28.6%
of cases per decade. Males were predominantly affected, accounting
for 86% of these cases.
Malignant lesions
The malignant lesions included 6 squamous cell
carcinomas, 3 mucoepidermoid carcinomas, 2 acinic cell carcinomas,
2 adenoid cystic carcinomas, 1 anaplastic carcinoma and 1 papillary
carcinoma, accounting for 26.8% of all the lesions.
Discussion
Parotid gland pathology has been well described and
documented in the literature, with 80% of all primary tumours being
benign and 20% malignant. Of the benign lesions, pleomorphic
adenomas account for 80% and Warthin's tumours for 20% of the
cases. These figures may vary in different regions, but are
generally confined within a certain range. The most common
malignant parotid tumours worldwide are reportedly mucoepidermoid
and adenoid cystic carcinomas (5–7).
Other malignant tumours of the parotid gland include acinic cell
carcinoma, carcinoma ex pleomorphic adenoma, adenocarcinoma
(arising from the ductal epithelium of the parotid gland), squamous
cell carcinoma (arising from the parenchyma of the parotid gland)
and undifferentiated carcinoma.
A study conducted by Catania et al (8) in Italy investigated 336 patients, 239
of whom had benign and 65 malignant lesions. Of the benign lesions,
55% were pleomorphic adenomas and 36% were Warthin's tumours,
whereas the majority of the malignant lesions (29%) were
mucoepidermoid carcinomas.
A study conducted by Chung et al (9) in Singapore documented the
epidemiology of parotid gland tumours in an Asian population over a
period of 10 years. A total of 289 patients were investigated, of
whom 136 had pleomorphic adenomas and 73 (25%) Warthin's tumours (7
bilateral), with a ratio of Warthin's tumours to pleomorphic
adenomas of 1:9. The racial distribution of Warthin's tumours
exhibited an increased incidence among Chinese patients and a
reduced incidence among Malays and Indians. It was hypothesized
that the lower incidence among ethnic groups with darker skin
suggested that concomitant genetic factors other than environmental
factors alone affected tumorigenesis. Smokers exhibited a 40-fold
higher risk of developing a Warthin's tumour compared to
non-smokers.
Another study conducted by Gunn et al
(10) in Northumberland
investigated 376 new cases of parotid tumours over a period of 5
years, with 28 recurrent cases. The incidence of new parotid
tumours was 2.4 per 100,000 and of pleomorphic adenomas 1.5 per
100,000 cases per annum.
An interesting study, conducted by Massoud et
al (11) in Lebanon, reported
on the etiological aspects of 175 parotidectomies. The authors
reported that 80% of the lesions were benign and 20% were
malignant, with an increase in malignancy rates with increasing
age. The mixed tumour rate was 31%, with 69% of the cases
comprising haemangiomas, tuberculomas, salivary cysts, chronic
parotiditis and Warthin's tumours.
Of note, Manifold et al (12) conducted a study on parotid gland
tumours in children and reported that 50% of all tumours were
malignant; therefore, all parotid lumps in children should be
considered as malignant until proven otherwise. There was also a
report by McShane et al (13) on adenoid cystic carcinoma arising
in the context of AIDS-related complex; this type of tumour is
currently more commonly encountered, due to the increasing
incidence of HIV infection.
As regards local data, very few studies have been
published within the West Indies, with no documented data from
Trinidad and Tobago. A literature search identified an article by
Shah et al (14) published
in the West Indian Medical Journal in 1990. Between 1958 and 1989,
the Jamaica Cancer Registry recorded 491 cases of benign and
malignant salivary gland tumours, including 18 cases of Warthin's
tumour (3.7%), with a male:female ratio of 5:1. Obbenson et
al (15) also conducted an
analysis on fine-needle aspiration cytology in 2001. Additionally,
there have been 3 studies from Cuba detailing the pathology of the
parotid and other salivary glands (16–18).
The present study on 60 patients with parotid gland
tumours in a mixed West Indian population, composed of 40% East
Indians, 38% Afro-Caribbeans, 20% mixed and <2% Caucasians,
Chinese and Arabs, revealed an interesting profile for these
tumours.
There were 56 primary and 4 secondary lesions (1
basal cell carcinoma and 3 metastatic tumours). The male:female
ratio was 1:1, with a mean age of 48.7 years, a median of 51.5
years and a mode of 56 years (range, 21–73 years). There were no
pediatric cases and no definitive confirmation of AIDS-related
complex, although this condition may have been present but
overlooked.
The benign lesions included 34 pleomorphic adenomas,
and 7 Warthin's tumours, accounting for 73.2% of the 56 primary
tumours. The malignant lesions included 6 squamous cell carcinomas,
3 mucoepidermoid carcinomas, 2 acinic cell carcinomas, 2 adenoid
cystic carcinomas, 1 anaplastic carcinoma and 1 papillary
carcinoma, accounting for 26.8% of all the primary lesions. The
most common carcinomas are reportedly the mucoepidermoid and
adenoid cystic types; however, squamous cell carcinomas were the
most commonly encountered malignant parotid tumours in our
series.
This study may provide useful information on parotid
gland pathology in Trinidad and Tobago and, by extension, the West
Indies, encouraging further research in this field.
Acknowledgements
We herein acknowledge the tireless efforts of Dr
Neville Jankey FRCPath, the Senior Pathologist at POSGH over
several decades and one of the main contributors to this database.
This study received no specific grant from any funding agency in
the public, commercial or not-for-profit sectors.
References
|
1
|
Ansari MH: Salivary gland tumors in an
Iranian population: a retrospective study of 130 cases. J Oral
Maxillofac Surg. 65:2187–2194. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jones AV, Craig GT, Speight PM and
Franklin CD: The range and demographics of salivary gland tumours
diagnosed in a UK population. Oral Oncol. 44:407–417. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shrestha S, Pandey GK, Pun CB, Bhatta R
and Shahi R: Histopathological pattern of salivary gland tumors. J
Pathol Nepal. 4:520–524. 2014. View Article : Google Scholar
|
|
4
|
American Cancer Society and salivary gland
cancer. http://www.cancer.org/cancer/salivaryglandcancer/detailedguide/Accessed.
September 16–2014
|
|
5
|
Gore DO, Annamunthodo H and Harland A:
Tumours of salivary gland origin. Surg Gynecol Obstet.
119:1290–1296. 1964.PubMed/NCBI
|
|
6
|
Gardner AF, Siegler HR and Spire ED: A
study of one hundred and seventy-three instances of pleomorphic
adenomas of the salivary glands. Am Surg. 30:539–548.
1964.PubMed/NCBI
|
|
7
|
Butler EC: The management of tumours of
the parotid gland, based on 373 cases seen at the London Hospital
between 1943–1958. Bull Soc Int Chir. 23:10–16. 1964.PubMed/NCBI
|
|
8
|
Catania A, Falvo L, D'Andrea V, et al:
Parotid gland tumours. Our experience and a review of the
literature. Chir Ital. 55:857–864. 2003.PubMed/NCBI
|
|
9
|
Chung YF, Khoo ML, Heng MK, et al:
Epidemiology of Warthin's tumour of the parotid gland in an Asian
population. Br J Surg. 86:661–664. 1999.
|
|
10
|
Gunn A and Parrott NR: Parotid tumours: a
review of parotid tumour surgery in the Northern Regional Health
Authority of the United Kingdom 1978–1982. Br J Surg. 75:1144–1146.
1988.PubMed/NCBI
|
|
11
|
Massoud E and Tarabay F: Parotid tumours.
Only 31% of mixed tumours in one hundred and seventy-five
parotidectomies. Sem Hop. 58:1448–1455. 1982.(In French).
|
|
12
|
Manifold DK and Thomas JM: Parotidectomy
in childhood - with a review of the literature. Eur J Surg Oncol.
20:549–552. 1994.PubMed/NCBI
|
|
13
|
McShane DP, Vellend H and Dayal VS: AIDS,
otolaryngology and a case of adenoid cystic carcinoma of the
parotid arising in a patient with the AIDS-related complex. J
Otolaryngol. 16:10–15. 1987.PubMed/NCBI
|
|
14
|
Shah D, Williams E and Brooks SE:
Warthin's tumour in Jamaica. Incidence, electron microscopy and
immunoenzyme studies. West Indian Med J. 39:225–232. 1990.
|
|
15
|
Obenson K and East J: Fine needle
aspiration biopsy in Western Jamaica: preliminary observations.
Cytopathology. 12:129–130. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Juarbe C, Longo F, Riera I and Urdaz V:
Parotidectomy in an urban community hospital. Bol Asoc Med PR.
81:427–429. 1989.PubMed/NCBI
|
|
17
|
Estrada Sarmiento M and Pinilla González
R: Tumors of the parotid gland. Rev Cubana Estomatol. 23:221–227.
1986.(In Spanish).
|
|
18
|
Urbizo Velez J and Moreira Diaz E:
Salivary gland tumors. A study of 155 cases. Rev Cubana Estomatol.
12:137–143. 1975.(In Spanish).
|