Introduction
Rectal cancer is a widespread malignancy with a high
incidence rate. Advances in surgical techniques have decreased the
frequency of postoperative rectal cancer recurrence (1,2), although
the rate remains high. In Japan, the reported disease recurrence
rates are 7.3% for hepatic metastasis, 7.5% for lung metastasis and
8.8% for locally recurrent rectal cancer (LRRC) (3).
Surgical resection is considered the most effective
curative treatment for postoperative LRRC in the pelvis. However,
resection is less commonly performed for LRRC compared to liver or
lung metastases. A recent meta-analysis (4) concluded that the primary goal of LRRC
treatment is to achieve radical resection. However, such surgical
resection often requires a highly aggressive approach, such as
total pelvic exenteration, and is associated with a high risk of
postoperative complications, including massive hemorrhage and
severe sepsis. Additionally, postoperative fibrosis and adhesions
are often indistinguishable from the recurrent tumor, making
curative resection even more difficult (5,6).
Particle beams utilizing protons and carbon ions
(C-ions) provide a more favorable dose distribution compared with
those involving photons. Furthermore, C-ions are heavier compared
to protons and, thus, have greater biological effectiveness. C-ion
radiotherapy (RT) was first utilized in 1994 by the National
Institute of Radiological Sciences. C-ion RT was tested on a
variety of tumor types in clinical trials and was approved as a
highly advanced medical technology by the Japanese Ministry of
Health in 2003. The main types of cancer that have been treated
with C-ion RT include bone and soft tissue sarcoma, prostate, head
and neck and non-small-cell lung cancer. Particle beam RT,
including C-ion RT, has also been investigated as a potential novel
tool for controlling LRRC. This is the report of three cases of
LRRC treated using particle beam RT.
Case reports
Patient selection criteria
Particle beam RT treatment for LRRC was indicated
for patients who refused to undergo surgery and who were able to
cover the high treatment cost (~three million yen). Additionally,
the recurrent tumors should not be closely adjacent to the
intestine or colon and rectum. Particle beam RT was performed at
the Hyogo Ion Beam Medical Center, the first institute in Japan to
provide both proton and C-ion therapy.
Therapeutic planning
Computed tomography (CT) scans were performed for
therapeutic planning. The specific therapy technique was as
previously described (7–9). Briefly, the CT imaging data were
transferred to the treatment planning system. Irradiation
parameters, in terms of the number of irradiation portals and their
directions, were determined in conjunction with target volume
delineation. A 5-mm safety margin was usually added to the clinical
target volume to create the planning target volume. The dose in
Gray equivalents (GyE = carbon physical dose in gray x relative
biological effectiveness) was calculated for the target volume and
any nearby critical structures, such as skin, urinary bladder and
intestines.
Written informed consent was obtained from the
patient or their family for publication of this manuscript and
accompanying images.
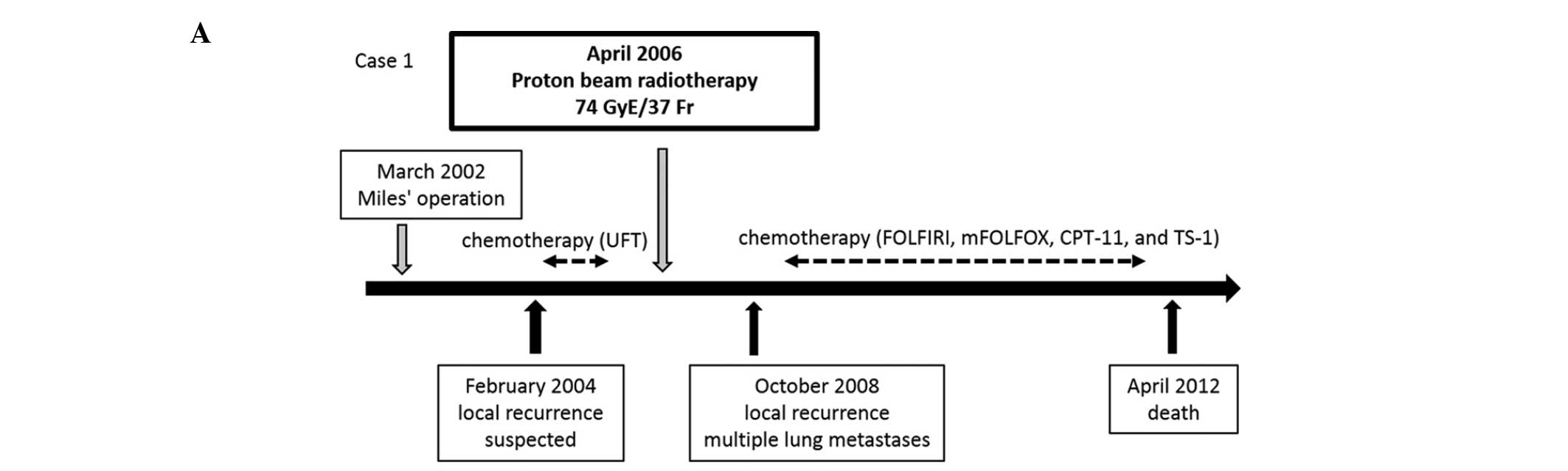
Case 1
A 56-year-old man with lower rectal cancer and lymph
node metastasis (stage IIIA according to the Union for
International Cancer Control tumor-node-metastasis classification)
underwent curative abdominoperineal excision (Miles' operation) in
March, 2002 (Fig. 1A). The
histological evaluation established the diagnosis of moderately
differentiated adenocarcinoma. At the patient's request, no
postsurgical adjuvant chemotherapy was administered. In February,
2004, CT and positron emission tomography (PET) scans revealed LRRC
in the patient's pelvis (Figs. 1B and
C). Tegafur-uracil was orally administered for 2 years. In
April, 2006, a magnetic resonance imaging scan showed that the LRRC
lesion had increased in size (Fig.
1D) and the patient underwent proton beam RT. During RT, the
patient exhibited only grade 1 dermatitis and he completed the
entire course of treatment (74 GyE/37 Fr). In October, 2008, the
patient exhibited multiple lung metastases and reappearance of the
LRRC. In March, 2010, the LRRC invaded the sacrum and the patient
was initiated on pain control medication due to sacral nerve
invasion. The patient underwent a series of chemotherapy
treatments, including FOLFIRI (fluorouracil, leucovorin and
irinotecan), mFOLFOX (modified leucovorin, fluorouracil and
oxaliplatin), irinotecan and TS-1 (tegafur, gimeracil and oteracil
potassium), but succumbed to the disease in April, 2012.
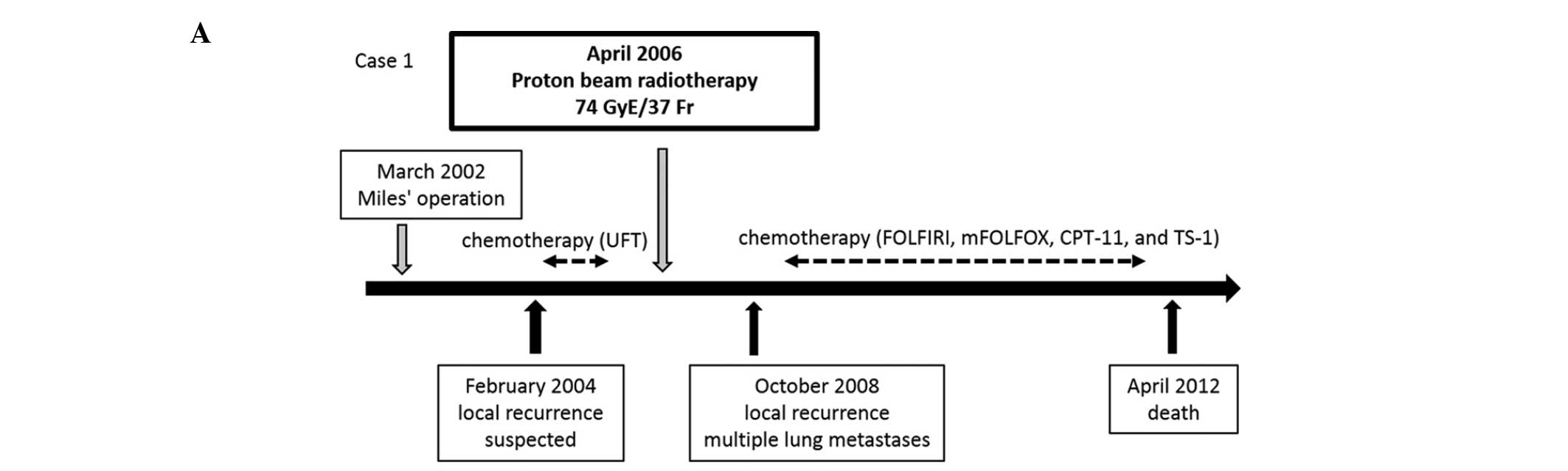 | Figure 1.Summary of case 1. (A) Course of
treatment following surgical resection. (B) Computed tomography
(CT) image from February, 2004. (C) Positron emission tomography-CT
scans from February, 2004 showing faint fluorodeoxyglucose uptake
in soft tissues (arrowheads) in accordance with the CT images. (D)
Magnetic resonance image from March, 2006 showing tumor invasion of
the caudal space (arrows). UFT, tegafur-uracil; FOLFIRI,
fluorouracil, leucovorin and irinotecan; mFOLFOX, modified
leucovorin, fluorouracil and oxaliplatin; CPT-11, irinotecan; TS-1,
tegafur, gimeracil and oteracil potassium. |
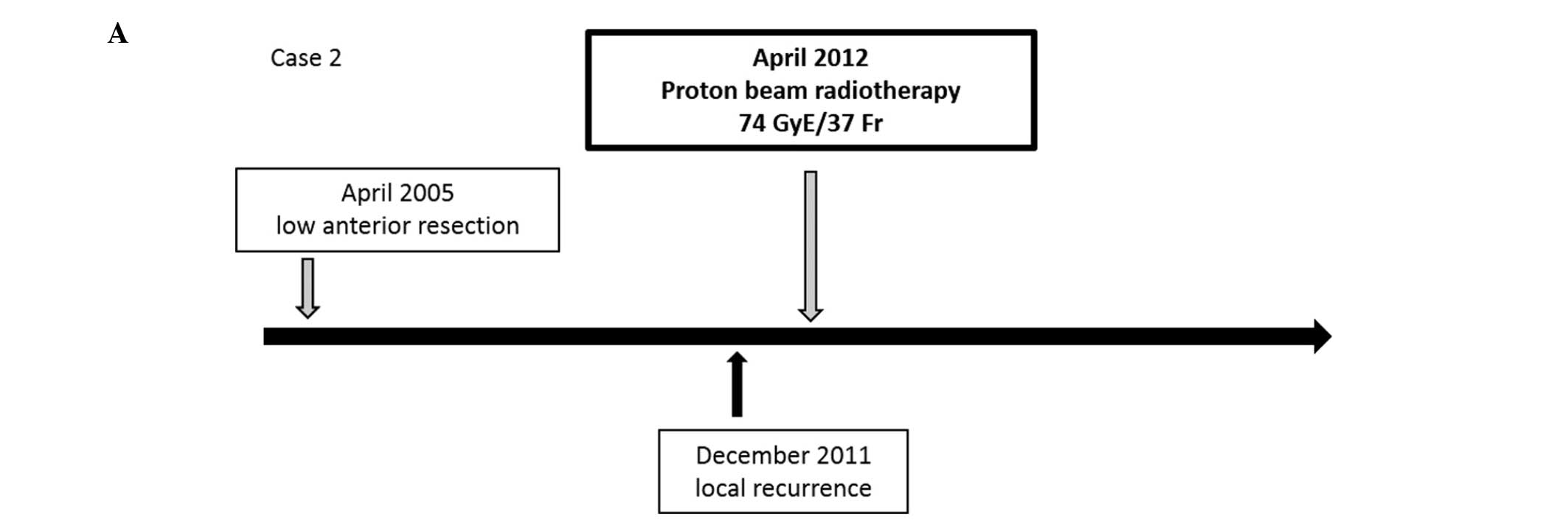
Case 2
In April, 2005, a 70-year-old man with lower rectal
cancer and lymph node metastasis (stage IIIA) underwent low
anterior resection with curative intent (Fig. 2A). The histological evaluation
established the diagnosis of moderately differentiated
adenocarcinoma. No postoperative adjuvant chemotherapy was
administered due to the patient's advanced age and chronic heart
disease. Six years after the surgery, in December, 2011, LRRC was
detected by CT (Fig. 2B) and PET
(Fig. 2C) scans. Proton beam RT was
performed in April, 2012 (Fig. 2D).
During RT, the patient experienced no adverse events and the
treatment was completed (74 GyE/37 fr). The patient has remained
tumor recurrence-free for >2.5 years.
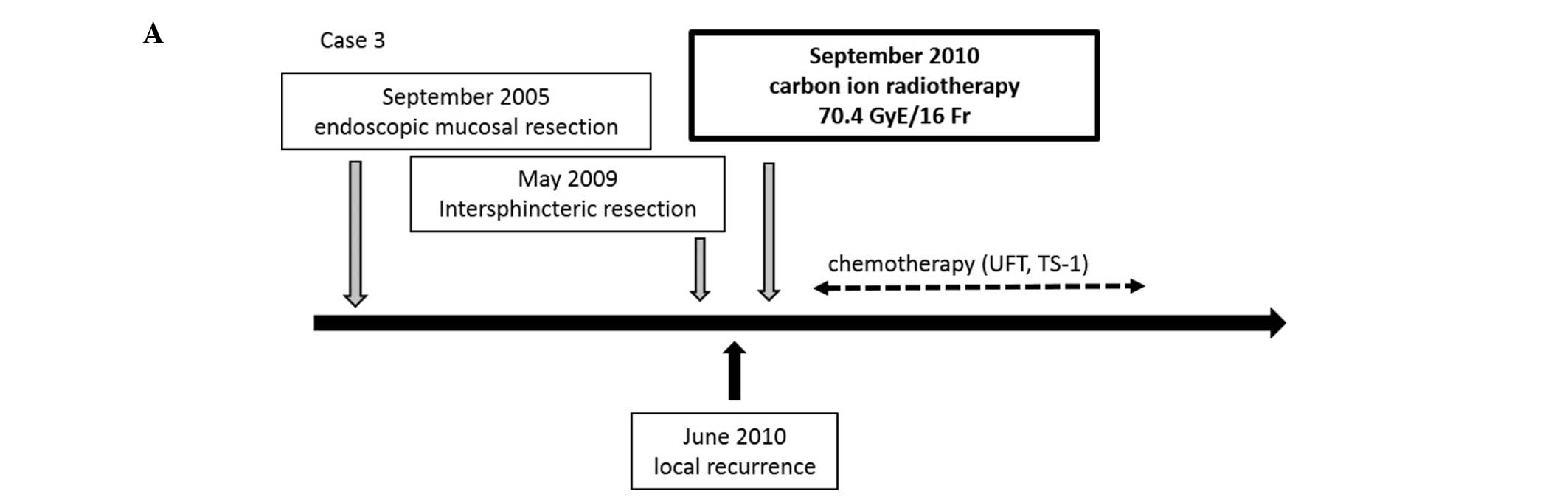
Case 3
In September 2005, a 71-year-old man with lower
rectal cancer underwent endoscopic mucosal resection (EMR)
(Fig. 3A). The histological
evaluation revealed vessel invasion and deep invasion into the
submucosal layer, necessitating additional surgical treatment.
However, the patient firmly declined additional surgery; therefore,
he underwent periodic CT scans, colonoscopy and blood tests to
monitor disease recurrence or distant metastasis. Four years later,
the patient exhibited rectal cancer recurrence on the EMR site.
Intersphincteric resection was performed in May, 2009. The
histological examination revealed that the tumor was a
well-differentiated adenocarcinoma (stage I). In June, 2010, PET-CT
scans revealed LRRC in the patient's pelvis and C-ion RT was
performed in September, 2010. No adverse events were observed
during the RT and the patient completed the treatment (70.4 GyE/16
fr). To date, there has been no LRRC; however, the patient has had
disease recurrence at different sites in the pelvis. The patient
remained symptom-free until December, 2014, but he currently
requires medication with oral morphine for severe perianal
pain.
Discussion
To date, surgical resection remains the standard
therapy for LRRC, with continuous advances in the surgical
techniques. However, the 5-year survival rate following surgical
treatment for LRRC remains 17–36% (5,6,10,11).
Furthermore, surgical treatment often requires the creation of two
stomas, which significantly compromises the patient's quality of
life. Additionally, sacral nerve damage caused by high sacral
resection may lead to walking disorders and severe lower limb pain.
Particle beam RT may be a potentially useful alternative treatment
option in certain cases of LRRC.
Particle beams possess several unique physical and
biological properties, such as the sharp, narrow Bragg peak created
by the energy deposition (high-dose peak) at the end of the beam
path. In contrast with photons and fast neutrons, the peak of a
particle beam is narrower, providing a dosage at the peak that is
several times higher compared with the dose in the plateau. A flow
of hydrogen nuclei is referred to as a proton beam, while a flow of
carbon nuclei is called a C-ion beam. The particle range is
controlled by the energy of the incoming particles. Photons,
electrons and protons are referred to as low-linear energy transfer
(LTE) radiations, while a C-ion is considered ionizing high-LTE
radiation. High-LTE radiation may cause cellular damage, regardless
of cell cycle phase and oxygenation status (8). The C-ion beam is a minimally invasive
radiation technology that delivers a large dose of highly focused
ionizing radiation to the target tumor, thus reducing toxicity to
normal tissues.
The use of C-ion RT to treat postoperative pelvic
recurrence of rectal cancer has been previously reported. Yamada
et al (12) performed a
dose-escalation study and demonstrated that the local control and
survival rates correlated to the total dose delivered. They
reported 5-year survival rates of 24, 27.5 and 42.3% for patients
treated with 67.2, 70.4 and 73.6 GyE/16 fr, respectively. Their
study design did not restrict other treatments, including
chemotherapy and molecularly targeted therapy; however, their
results were compatible with the surgical outcomes. No adverse
events were reported in the acute phase with C-ion RT of 73.6
GyE/16 fr; therefore, the survival rate at this dose is acceptable
as compared with that of surgical resection of LRRC.
In the present study, LRRC was treated using
irradiation with proton beam RT of 74 GyE/37 fr for cases 1 and 2
and with C-ion RT of 70.4 GyE/16 fr for case 3. In each case,
treatment was determined considering the tumor size and the
patient's basal complications. In cases 2 and 3, treatment
successfully led to long-term control of LRRC, with survival over a
follow-up period of 2–4 years. The patient in case 1 eventually
succumbed to the disease, but the local recurrence remained stable
for 2 years following RT and he survived for 6 years after the
treatment. None of the treated patients experienced severe adverse
events during the therapy, although two patients were aged >75
years. Our results did not reveal significant differences between
the proton beam RT and the C-ion RT with regard to controlling
LRRC. It is possible that sequential therapy and chemotherapy or
surgery may improve the curative rate of LRRC. Tomokuni et
al (13) previously reported a
case of LRRC treated with curative surgery and preoperative C-ion
RT.
In case 1, the patient developed inflammation of the
pelvic dead space following surgery, as well as long-lasting
discharge from the perineal wound. LRRC was first suspected in
February, 2004. However, we could not definitively differentiate
between inflammatory changes and disease recurrence until the tumor
marker carcinoembryonic antigen levels increased to >100 ng/ml
in 2005. Although there is no consensus regarding the optimal time
to initiate RT, it is possible that earlier induction would have
improved the prognosis in case 1.
In conclusion, particle beam RT is an effective
treatment for local control of LRRC in patients for whom surgical
resection is not considered the optimal choice. Particle beam RT
represents a promising alternative to surgery. However, the
long-term safety of this approach requires further
investigation.
Abbreviations:
|
LRRC
|
locally recurrent rectal cancer
|
|
C-ion RT
|
carbon ion radiotherapy
|
|
TPE
|
total pelvic exenteration
|
|
CT
|
computed tomography
|
|
LTE
|
linear energy transfer
|
|
NIRS
|
National Institute of Radiological
Sciences
|
References
|
1
|
Dias AR and Nahas SC: Modified
supralevator pelvic exenteration for the treatment of locally
advanced rectal cancer with vaginal and uterine invasion. Surg
Today. 43:702–704. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Seishima R, Okabayashi K, Hasegawa H,
Sugiyama D, Ishii Y, Tsuruta M, Takebayashi T and Kitagawa Y:
Obesity was associated with a decreased postoperative recurrence of
rectal cancer in a Japanese population. Surg Today. 44:2324–2331.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Watanabe T, Itabashi M, Shimada Y, et al:
Japanese Society for Cancer of the Colon and Rectum: Japanese
Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010
for the treatment of colorectal cancer. Int J Clin Oncol. 17:1–29.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bhangu A, Ali SM, Darzi A, Brown G and
Tekkis P: Meta-analysis of survival based on resection margin
status following surgery for recurrent rectal cancer. Colorectal
Dis. 14:1457–1466. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ike H, Shimada H, Ohki S, Yamaguchi S,
Ichikawa Y and Fujii S: Outcome of total pelvic exenteration for
locally recurrent rectal cancer. Hepatogastroenterology.
50:700–703. 2003.PubMed/NCBI
|
|
6
|
Nielsen MB, Rasmussen PC, Lindegaard JC
and Laurberg S: A 10-year experience of total pelvic exenteration
for primary advanced and locally recurrent rectal cancer based on a
prospective database. Colorectal Dis. 14:1076–1083. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kamada T: Clinical evidence of particle
beam therapy (carbon). Int J Clin Oncol. 17:85–88. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tsujii H and Kamada T: A review of update
clinical results of carbon ion radiotherapy. Jpn J Clin Oncol.
42:670–685. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Okada T, Kamada T, Tsuji H, et al: Carbon
ion radiotherapy: Clinical experiences at National Institute of
Radiological Science (NIRS). J Radiat Res (Tokyo). 51:355–364.
2010. View Article : Google Scholar
|
|
10
|
Bosman SJ, Vermeer TA, Dudink RL, de Hingh
IH, Nieuwenhuijzen GA and Rutten HJ: Abdominosacral resection:
Long-term outcome in 86 patients with locally advanced or locally
recurrent rectal cancer. Eur J Surg Oncol. 40:699–705. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Moriya Y, Akasu T, Fujita S and Yamamoto
S: Total pelvic exenteration with distal sacrectomy for fixed
recurrent rectal cancer in the pelvis. Dis Colon Rectum.
47:2047–2053; discussion 2053-4. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yamada S, Shinoto M and Endo S: Carbon ion
radiotherapy for patients with locally recurrent rectal cancer.
Proceedings of NIRS-ETOILE 2nd Joint Symposium on Carbon Ion
Radiotherapy 2011. NIRS-M-243:54–59. 2011.
|
|
13
|
Tomokuni A, Takahashi H, Ikeda M,
Mizushima T, Takemasa I, Yamamoto H, Sekimoto M, Yamada S, Doki Y
and Mori M: A case of locally recurrent rectal cancer resected in
combination with preoperative carbon ion radiotherapy. Jpn J
Gastroenterol Surg. 43:595–600. 2010. View Article : Google Scholar
|