Introduction
Cancer and its treatment are frequently complicated
by pulmonary disorders, mainly thromboembolic disease, although
infections and drug toxicity may also develop. Diagnosis is usually
based on clinical and radiological manifestations.
Permanent central venous catheters (CVC), such as
Port-a-Cath® and Hickmann®, are widely used in oncology patients
for cancer treatment. The most commonly reported complications of
CVCs are infections and thrombosis. The incidence of CVC-related
thrombosis was reported to be ~30% in adults (1). The clinical manifestations sometimes are
obvious, with congestion of the collateral veins of the shoulder
and chest wall on the affected side; however, thrombosis of the
deep veins may occasionally be asymptomatic or present with mild
symptoms. Rarely, CVC may be associated with the development of an
atrial mass as a consequence of a CVC-related organized thrombus
located inside the atrial cavity (1).
Herein, we report the case of a patient with colon
cancer and a CVC who developed severe hemodynamic complications
associated with an atrial thrombotic mass.
Case report
A 43-year-old man was admitted to the hospital due
to severe and progressive shortness of breath and platypnea. The
patient was on chemotherapy for colon cancer and a liver metastasis
had been resected 1 month earlier. The patient was receiving FOLFOX
as a perioperative regimen and had received the sixth course of
chemotherapy several days prior to his admission. The patient's
medical record included dyslipidemia and first-degree relatives
with cancer (mother, colon and breast cancer; and father, bladder
cancer).
A few days after his fifth course of chemotherapy,
the patient developed rapidly progressive dyspnea on exertion. The
dyspnea improved in the supine position (platypnea); the oxygen
saturation while breathing room air was 75% and it also improved in
the supine position (orthodeoxia).
An arterial blood gas analysis while breathing room
air revealed a pH of 7.54, PaCO2 of 19 mmHg and
PaO2 of 45 mmHg. The patient was admitted to the
emergency room due to worsening of the respiratory symptoms and was
transferred to the intensive care unit due to severe respiratory
distress and very low oxygen saturation. The laboratory analysis
did not show relevant data, apart from elevated levels of D-dimers.
On electrocardiography, there was sinus rhythm with no
abnormalities. The chest X-ray was normal and a chest computed
tomography (CT) excluded pulmonary embolism and revealed no airway
or parenchymal pathological findings, thus excluding infection and
drug toxicity. The tip of the CVC was inside the right atrial
cavity, in close proximity to the tricuspid valve. A transthoracic
echocardiogram revealed a mild interventricular septal hypertrophy
and normal biventricular systolic function. The patient was treated
with high fraction of inspired oxygen and low-molecular weight
heparin and exhibited progressive improvement. On discharge, the
patient had an oxygen saturation of 93% while breathing room air in
the supine position, which was reduced to 88% while sitting
(orthodeoxia). In addition to the hypoxemia, the blood gas analysis
revealed a respiratory alkalosis (pH=7.49, PaCO2=28,
PaCO2=65 and HCO3=24). The abdominal CT
revealed post-hepatectomy and -hemicolectomy surgical alterations.
No portal hypertension was detected. Due to the suspicion of a
right-to-left intracardiac shunt, a transcranial Doppler ultrasound
of the left medial cerebral artery was performed with the infusion
of an agitated saline solution through the right arm, which
revealed a ‘shower-curtain effect’, suggesting a massive
intracardiac shunt. A transesophageal echocardiography confirmed a
right-to-left shunt through a patent foramen ovale (PFO) and
detected a fixed mass in the right atrium in close proximity to the
mouth of the superior cava, causing an obstruction of the entry
flow, which was directed towards the foramen ovale. The distal end
of the CVC was seen inside the right atrium, but the mass did not
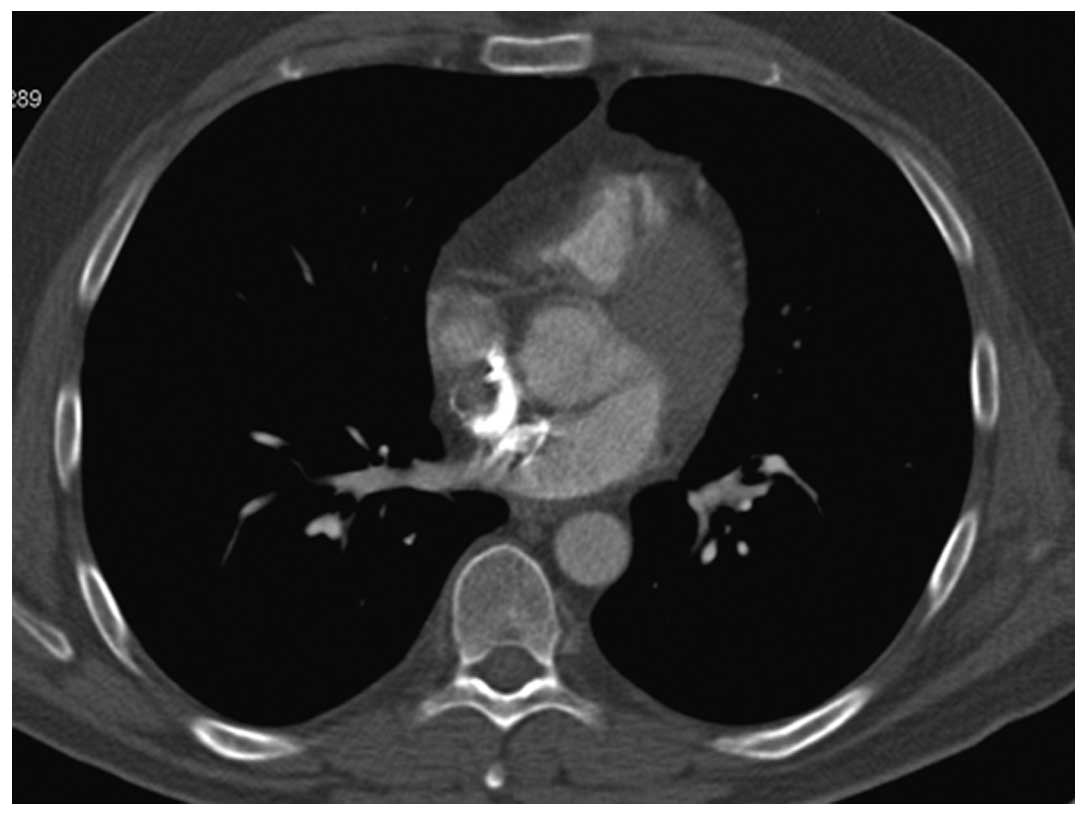
appear to be attached to it. Magnetic resonance imaging (MRI) of
the heart and a new CT revealed a mass inside the right atrium
(Figs. 1 and 2). Considering all these findings, the
patient continued to receive low-molecular weight heparin and was
referred for cardiac surgery.
The right atrium was opened and a large mass (6×5
cm) was identified, which filled the entire atrium. The mass was
intimately attached to the free atrial wall and obstructed the
tricuspid valve. The entire free wall of the right atrium was
resected along with the mass and the atrium was reconstructed with
autologous pericardium. The PFO was closed and the CVC was moved in
place. Several hours after surgery, the patient suffered a
pericardial tamponade requiring a pericardial window.
The pathological examination revealed a section of
resected cardiac wall with a fibrous pericardium and a mass
composed of fibrin and thrombotic hyaline, with isolated lymphocyte
aggregates. No neoplastic cells were identified. Following surgery,
the patient exhibited a significant improvement of the dyspnea,
whereas the oxygen saturation while breathing room air increased to
95–98%. The patient is currently on chemotherapy with FOLFOX, with
acceptable tolerance, apart from progressive cumulative peripheral
neuropathy secondary to oxaliplatin.
Discussion
We herein described a rare complication in colon
cancer: A right-to-left shunt with moderate-to-severe hypoxemia
associated with a right atrial mass. Several differential diagnoses
are possible when a right atrial mass is detected in a cancer
patient. Myxomas are the most common atrial tumors and are
classically described as arising on the left side, although a
significant proportion of these tumors occur on the right side.
Cardiac metastases from primary colorectal carcinomas are extremely
rare (2). However, metastatic
involvement of the heart is relatively common in melanoma, lung
cancer, breast cancer and renal cell carcinoma. Klatt and Heitz
(2) examined a total of 1,029
autopsies from patients diagnosed with malignancies and found
cardiac involvement in 10.4% of all cases, 36.4% of which
originated from adenocarcinomas of the lung, gastrointestinal
tract, female genitourinary tract, breast or pancreas.
CVC-related thrombosis is another cause of atrial
masses and it may be a complication and frequent cause of death in
cancer patients (3). The incidence of
CVC-related thrombosis has changed over the last few decades, being
reported by more recent studies as ~14–18% in asymptomatic and 5%
in symptomatic patients (4). Several
authors have suggested that, when the tip of the catheter is
located in the right atrium, the risk of thrombosis is higher
(5). Several mechanisms may underlie
this complication, mainly direct endocardial injury by the tip of
the catheter, although antitumor drugs and their action on
endothelial cells may also be involved. Maney et al
(6) reported that certain antitumor
agents may induce apoptosis of endocardial endothelial cells when
these cells are directly exposed to the chemotherapeutic
agents.
As we have previously mentioned, the differential
diagnoses of intracardiac masses include vegetations, thrombi or
tumors. Echocardiography has become the gold standard for the
diagnosis of intracardiac masses and the transesophageal approach
has improved the overall accuracy (7). MRI may be suitable for tissue
characterization, identifying the amount of fat with a high degree
of specificity and may be used to diagnose cardiac lipomas and
cardiac thrombi, which usually exhibit delayed enhancement. Cardiac
MRI may also reveal in detail the location, insertion site and size
of the mass, facilitating surgical resection. However, although all
these tests are very useful, they are frequently unable to
distinguish with certainty between a solid organized thrombus and a
tumor.
Systemic thrombolysis may be suitable for pulmonary
thromboembolism or free-floating emboli in the right atrium (type A
thrombi) (5). Giant thrombi (type B)
(5), which develop within the heart
chambers, are usually fixed, well-organized and fibrotic,
intimately associated with the atrial wall and very unlikely to
respond to thrombolytic therapy; in fact, in such cases,
thrombolytic therapy is often ineffective and unsafe. The few cases
of giant atrial thrombi reported in the literature suggest open
surgical removal as the procedure of choice (8).
Gas exchange impairment with normal thoracic
radiology and pulmonary function tests should suggest a
right-to-left shunt, either intrapulmonary or intracardiac; both
are typically associated with platypnea and orthodeoxia. In
addition to PFO, which is as frequent as 27% in some autopsy series
(9–14), other causes have been described, such
as other interatrial defects, pericardial effusion, constrictive
pericarditis and non-cardiac disorders, including emphysema,
amiodarone-related pulmonary toxicity and cirrhosis (15,16). In
cancer patients, conditions such as pneumonectomy and primary
benign and malignant cardiac tumors may be associated with a PFO
(17). Latif et al (18) described a patient with a right-to-left
shunt secondary to intracardiac metastasis from a nasopharyngeal
epidermoid carcinoma diagnosed 2 years earlier. We hypothesized
that, in our patient, the right atrial mass redirected the flow
from the superior vena cava to the interatrial septum, opening a
PFO that had caused no hemodynamic consequences up to that
point.
One possible explanation for the development of an
organized thrombus inside the right atrium may be that the tip of
the catheter was moved inside the atrial cavitity, coming into
direct contact with the endocardium, initiating a fibrotic reaction
and inducing the release of several prothrombotic proteins, leading
to the formation of an atrial thrombotic mass and the subsequent
complications.
Although several examinations (ultrasound and MRI)
did not reveal that the chemotherapy infusion directly over the
endocardium induced a reaction leading to the development of an
organized thrombus, Maney et al (6) reported that certain antitumor agents may
induce apoptosis of endocardial endothelial cells when these cells
are directly exposed to the chemotherapeutic agents.
The need for an etiological diagnosis of the atrial
mass and the increased risk of embolization using a percutaneous
procedure made a surgical approach mandatory. In addition, our
patient exhibited symptoms and signs of valvular obstruction.
Surgery is the procedure of choice in cases of valvular
obstruction, since it may resolve the obstruction and prolong life
expectancy in such patients. Several authors have reported cases of
obstructive cardiac metastasis that have been successfully treated
with surgery (18,19). The majority of authors consider that
organized thrombi require a surgical approach, as conservative
treatment with low-molecular weight heparin or dicumarins cannot
resolve the thrombus or reverse its hemodynamic consequences.
Although there is not enough evidence to establish the optimal
treatment approach to intracardiac thrombosis, surgery is preferred
in the majority of the cases (19,20).
Another reason for surgery in such patients is the closure of the
atrial septal defect (20).
In conclusion, although gas exchange impairment in
oncology patients is most frequently due to pulmonary emboli
secondary to thrombosis unrelated to CVC, pulmonary infections or
pulmonary drug toxicity, other infrequent causes should be
considered, including an intracardiac shunt, particularly if the
radiological findings are normal. CVC-related thrombosis is a
frequent complication that should be ruled out due to the
potentially severe hemodynamic consequences, particularly if the
tip of the catheter is located inside the atrium.
References
|
1
|
Lordick F, Hentrich M, Decker T, Hennig M,
Pohlmann H, Hartenstein R and Peschel C: Ultrasound screening for
internal jugular vein thrombosis aids the detection of central
venous catheter-related infections in patients with
haemato-oncological diseases: A prospective observational study. Br
J Haematol. 120:1073–1078. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Klatt EC and Heitz DR: Cardiac metastases.
Cancer. 65:1456–1459. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee AY and Kamphuisen PW: Epidemiology and
prevention of catheter-related thrombosis in patients with cancer.
J Thromb Haemost. 10:1491–1499. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Murray J, Precious E and Alikhan R:
Catheter-related thrombosis in cancer patients. Br J Haematol.
162:748–757. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Egolum UO, Stover DG, Anthony R, Wasserman
AM, Lenihan D and Damp JB: Intracardiac thrombus: Diagnosis,
complications and management. Am J Med Sci. 345:391–395. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maney SK, Johnson AM, Sampath Kumar A,
Nair V, Santhosh Kumar TR and Kartha CC: Effect of
apoptosis-inducing antitumor agents on endocardial endothelial
cells. Cardiovasc Toxicol. 11:253–262. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cakal S, Cakal B, Alıcı G, Ozkan B, Bulut
M and Esen AM: Different imaging modalities in detection of a huge
intracardiac mass. Heart Lung Circ. 20:773–774. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shankarappa RK, Math RS, Papaiah S,
Channabasappa YM, Karur S and Nanjappa MC: Free floating right
atrial thrombus with massive pulmonary embolism: Near catastrophic
course following thrombolytic therapy. Indian Heart J. 65:460–463.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ando T, Abe H, Nagata T, Sakurai Y,
Chikada M, Kobayashi T and Makuuchi H: Reports of four surgical
treatments of acute pulmonary embolism with a floating thrombus in
the right atrium. Gen Thorac Cardiovasc Surg. 59:705–708. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Roche L, Rioufol G, Piszker G, Genety C,
Ritz B, Ferrini M, Finet G and Aupetit JF: Platypnea-orthodeoxia
syndrome: A case report. Ann Cardiol Angeiol (Paris). 62:354–357.
2013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Amao E, Val E and Michel F:
Platypnea-orthodeoxia syndrome. Rev Clin Esp (Barc). 213:120–121.
2013.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hagen PT, Scholz DG and Edwards WD:
Incidence and size of patent foramen ovale during the first 10
decades of life: An autopsy study of 965 normal hearts. Mayo Clin
Proc. 59:17–20. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mühling O, Koller M, Langbein A, Fröhner
S, Schumacher B and Kerber S: Hypoxemia 4 month after right-sided
pneumonectomy. Internist (Berl). 52:1002–1005. 2011.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bhattacharya K, Birla R, Northridge D and
Zamvar V: Platypnea-orthodeoxia syndrome: A rare complication after
right pneumonectomy. Ann Thorac Surg. 88:2018–2019. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chartier L, Béra J, Delomez M, Asseman P,
Beregi JP, Bauchart JJ, Warembourg H and Théry C: Free-floating
thrombi in the right heart: Diagnosis, management and prognostic
indexes in 38 consecutive patients. Circulation. 99:2779–2783.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nicolaou N, Becker A, Mc Michael G and
Nicolaou V: Giant atrial thrombus presenting as a tumor. Int J Surg
Case Rep. 4:62–64. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Funt S, Lerakis S, McLean DS, Willis P,
Book W and Martin RP: A right atrial mass, patent foramen ovale and
indwelling central venous catheter in a patient with a malignancy:
A diagnostic and therapeutic dilemma. J Am Soc Echocardiogr.
23:457.e1–3. 2010.PubMed/NCBI
|
|
18
|
Latif T, Steiman DM and Gagaoudakis P:
Massive right atrial thrombosis due to Hickman catheter requiring
open heart surgery - a case report. Angiology. 52:425–428. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Erkut B, Ates A, Dag O, et al: Surgical
removal of dialysis catheter related atrial thrombus. J Vasc
Access. 11:175–176. 2010.PubMed/NCBI
|
|
20
|
Hussain N, Shattuck PE, Senussi MH, et al:
Large right atrial thrombus associated with central venous catheter
requiring open heart surgery. Case Rep Med.
2012:5013032012.PubMed/NCBI
|