Introduction
Multiport laparoscopic colectomy (MLC) is being
increasingly adopted worldwide for treating colon disease. MLC has
been associated with less pain, quicker recovery of
gastrointestinal function, better pulmonary function, shorter
hospital stay and a better postoperative quality of life compared
with open surgery (1).
Single-incision laparoscopic colectomy (SLC) was recently
successfully introduced for colon cancer (2–6). As SLC is
becoming a more frequently used surgical option for the treatment
of colon cancer, the technical demands and lack of surgical
experience may limit a resident's opportunity to be trained in this
laparoscopic technique, similar to the early days of MLC. The
number of studies that have been conducted on resident training in
SLC is very limited and it has only been evaluated in a total of 31
patients, including 13 cancer patients and 18 patients with other
benign conditions (7); it appears
that SLC training for the residents has not been evaluated in
patients undergoing colon cancer resection, including
lymphadenectomy. The aim of the present study was to evaluate
resident performance and outcomes in patients undergoing SLC
performed by residents vs. staff colorectal surgeons, and
demonstrate the feasibility and safety of surgical residents
performing SLC under the supervision of colorectal surgeons
experienced in this technique.
Patients and methods
Surgeon selection
The resident group included 3 residents, each with
experience in a gastrointestinal surgery department, with the most
junior in the third year and the most senior in the fifth year of
residency. The staff group consisted of 2 staff surgeons with ≥10
years of experience in colorectal cancer surgery. One of the
surgeons is registered as a ‘qualified surgeon’ according to the
endoscopic surgical skill qualification system of the Japan Society
for Endoscopic Surgery. The operator and the assistants were
randomly selected.
Cases and procedures
First, a retrospective investigation of the peri-
and postoperative short-term results for the 141 MLC cases (staff
group, n=77; and resident group, n=64) was performed, to assess the
MLC surgical skills of the residents.
Next, we performed a retrospective case-control
study of 79 patients undergoing elective SLC for colon cancer by a
staff surgeon (staff group, n=49) or a resident (resident group,
n=30) over a 12-month period at the Yao Municipal Hospital (Yao,
Japan). All the cases were directly supervised by the staff
surgeons. Data on patient demographics, body mass index (BMI),
American Society of Anesthesiologists (ASA) class, tumor location
and size, personal history of prior surgery, operative time,
estimated blood loss, length of the incision, number of harvested
lymph nodes, length of the resected margin, conversion to open
surgery, insertion of an additional port, perioperative
complications, morbidity and length of hospital stay, were
compared. To investigate issues regarding the surgical procedures,
the video recordings of the operations for all the patients were
reviewed. The entire surgical process for the right colon was
divided into 4 procedures as follows: i) From camera insertion to
the start of mesenteric incision, ii) from the start of mesenteric
incision and separation and identification of the origin of the
mesenteric artery to clip insertion, iii) from clip insertion to
blood vessel dissection and iv) from blood vessel dissection to the
closure of the mesentery of the dissected colon. In addition to
these 4 procedures, 2 further steps were added for the left colon:
v) From the closure of the mesentery of the dissected intestine to
colon dissection and vi) from camera insertion via a
pneumoperitoneum to the removal of an automatic anastomosis. Each
procedure was measured in seconds.
Surgical technique
For SLC, a lap protector (Hakko Co., Ltd., Chikuma,
Japan) was inserted through a 30-mm incision in the umbilicus.
Subsequently, an EZ-access (Hakko Co., Ltd.) was mounted on the lap
protector and three 5-mm ports were placed in the EZ-access. The
operative procedures and instruments were identical to those used
for standard laparoscopic surgery with a flexible 5-mm scope
(Olympus Medical Systems Corp., Tokyo, Japan). An additional
incision or trocar port was placed without hesitation, if
necessary, to complete the procedure, whereas conversion to open
laparotomy was maintained as an option. The decision of additional
trocar placement or conversion to open laparotomy depended on the
staff surgeons. For lymphadenectomy, complete mesocolic excision
(CME) with central vascular ligation (CVL) was performed (8–10). The
final incision was extended to a length comparable to the size of
the specimen.
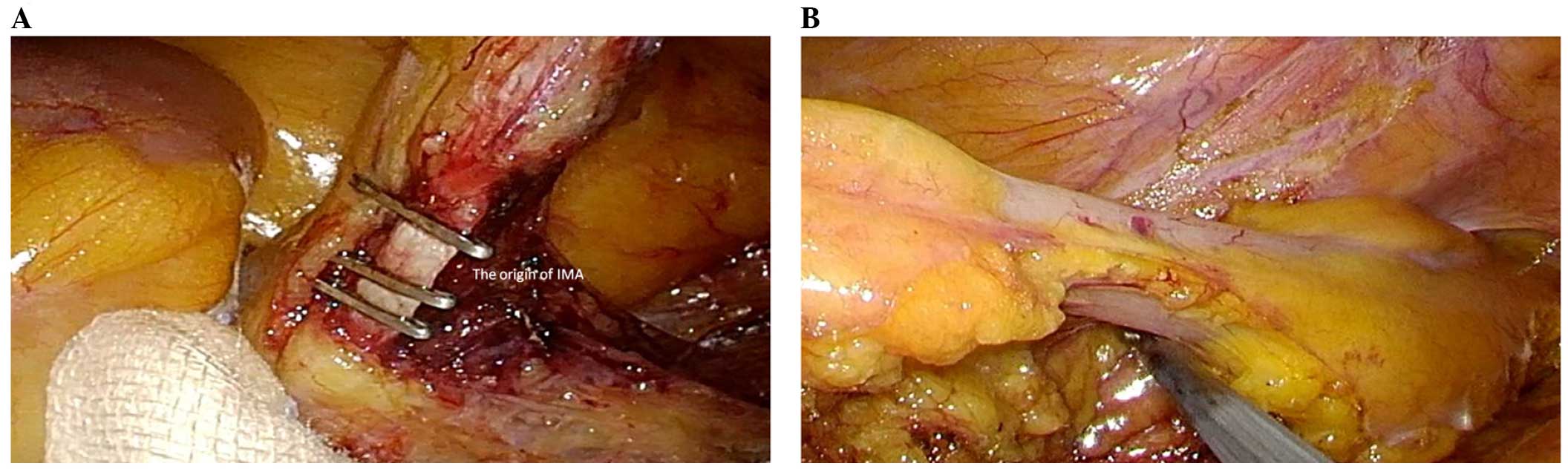
Right hemicolectomy
The patient was placed in the Trendelenburg
semi-left lateral position. The surgeon and camera operator stood
on the left side of the patient. In case of MLC, the assistant
stood between the patient's legs. In both groups, the procedure was
performed via an inferior approach, with initial peritoneal
dissection between the mesoileum and the retroperitoneum. Following
mesocolic plane resection, the duodenum and pancreas were
sufficiently exposed and the ileocolic, right (if necessary) and
middle colic vessels were ligated and dissected between the clips
at their origin to allow complete dissection of the right mesocolon
and lymph nodes (Fig. 1. Following
dissection of the greater omentum, the hepatic flexure was
mobilized. The specimen was retrieved through the incision of the
umbilicus, followed by extracorporeal functional end-to-end
anastomosis.
Sigmoidectomy and anterior
resection
The patient was placed in the Trendelenburg
semi-right lateral position. The surgeon and camera operator stood
on the right side of the patient. In case of MLC, the assistant
stood between the patient's legs or on the left side. In both
groups, the procedure was performed via a standard
medial-to-lateral approach. The inferior mesenteric artery and vein
were skeletonized, clipped and divided (Fig. 2. Subsequently, we dissected downwards
from the mesenteric window to the pelvis. The next step was
mobilization of the sigmoid colon up to the splenic flexure. The
descending and sigmoid colon was pulled anteromedially to ensure
preservation of the left ureter and gonadal vessels. The fat
surrounding the rectum at least 50 mm distal to the lesion was
dissected and then normally transected using an endoscopic linear
stapler (Endo GIA™; Covidien LLC, Mansfield, MA, USA) with a purple
cartridge inserted from the umbilical port with a 12-mm EZ link
(Hakko Co., Ltd.). The specimen was retrieved through the incision
in the umbilicus and the double stapling technique was applied for
anastomosis.
Statistical analysis
Statistical analysis was performed using
commercially available software (SPSS for Windows v14.0; SPSS,
Chicago, IL, USA). All the variables were evaluated using the
Chi-square test or the Student's t-test when appropriate. A P-value
of <0.05 was considered to indicate statistically significant
differences.
Results
Characteristics of patients undergoing
MLC
For MLC, the total patient characteristics did not
differ significantly between the staff and resident groups (age,
69.8±10.6 vs. 67.0±11.0 years, respectively; P=0.14; BMI, 22.9±3.4
kg/m2 vs. 22.6±3.5 kg/m2, respectively;
P=0.60). No other clinical variables, i.e., ASA class, tumor
location and history of prior surgery, differed significantly
between the two groups, apart from gender. Comparing these
variables between the groups on the basis of tumor location (right-
vs. left-sided colon cancer), no significant differences were
observed (Table I).
 | Table I.Characteristics of patients who
underwent multiport laparoscopic colectomy. |
Table I.
Characteristics of patients who
underwent multiport laparoscopic colectomy.
|
| Total | Righta | Leftb |
|---|
|
|
|
|
|
|---|
| Characteristics | Staff (n=77) | Resident (n=64) | P-value | Staff (n=29) | Resident (n=26) | P-value | Staff (n=48) | Resident (n=38) | P-value |
|---|
| Age, years | 69.8±10.6 | 67.0±11.0 | 0.14 | 71.5±9.9 | 67.8±12.2 | 0.22 | 66.8±11.0 | 66.4±10.3 | 0.33 |
| Gender |
|
|
|
|
|
|
|
|
|
| Male | 40 | 23 | 0.06 | 18 | 11 | 0.14 | 22 | 30 | <0.01 |
|
Female | 37 | 41 |
| 11 | 15 |
| 26 | 8 |
|
| BMI,
kg/m2 | 22.9±3.4 | 22.6±3.5 | 0.60 | 21.7±4.1 | 21.7±4.1 | 0.44 | 23.2±2.9 | 23.3±2.9 | 0.89 |
| ASA class |
|
|
|
|
|
|
|
|
|
| 1 | 7 | 8 | 0.36 | 3 | 2 | 0.93 | 4 | 6 | 0.25 |
| 2 | 60 | 52 |
| 23 | 22 |
| 37 | 30 |
|
| 3 | 10 | 4 |
| 3 | 2 |
| 7 | 2 |
|
| Prior surgery | 20 | 15 | 0.73 | 6 | 6 | 0.37 | 14 | 9 | 0.57 |
| Tumor location |
|
| 0.94 |
|
|
|
|
|
|
|
Cecum | 9 | 6 |
|
|
|
|
|
|
|
| Ascending
colon | 13 | 12 |
|
|
|
|
|
|
|
|
Transverse colon | 7 | 8 |
|
|
|
|
|
|
|
|
Descending colon | 6 | 5 |
|
|
|
|
|
|
|
| Sigmoid
colon | 30 | 26 |
|
|
|
|
|
|
|
|
Rectosigmoid colon | 12 | 7 |
|
|
|
|
|
|
|
Surgical outcomes of patients
undergoing MLC
The operative statistics are listed in Table II. Total surgical outcomes, including
blood loss, hospital stay, number of harvested lymph nodes, margin
of the resected specimen and tumor size, were similar between the
staff and resident groups. For right-sided colon cancer, the
operative time tended to be longer in the resident compared with
that in the staff group, but the difference was not significant
(223.2±72.0 vs. 200.7±49.7 min, respectively; P=0.08). The
operative complications were comparable between the two groups
(staff group, n=7; and resident group, n=8; P=0.51). There was no
mortality in either group and there was no readmission within 30
days after the MLC procedure. These results indicate that the
residents were able to perform MLC safely under the guidance of the
staff surgeons.
 | Table II.Surgical outcomes of patients who
underwent multiport laparoscopic colectomy. |
Table II.
Surgical outcomes of patients who
underwent multiport laparoscopic colectomy.
|
| Total | Righta | Leftb |
|---|
|
|
|
|
|
|---|
| Variables | Staff (n=77) | Resident (n=64) | P-value | Staff (n=29) | Resident (n=26) | P-value | Staff (n=48) | Resident (n=38) | P-value |
|---|
| Operative time,
min | 194.0±46.7 | 214.1±59.5 | 0.10 | 200.7±49.7 | 223.2±72.0 | 0.08 | 190.6±44.6 | 202.5±47.6 | 0.24 |
| Estimated blood
loss, ml | 19.7±58.0 | 27.2±35.4 | 0.15 | 25.2±32.6 | 20.0±34.0 | 0.56 | 19.6±70.2 | 39.6±62.9 | 0.27 |
| Conversion to
laparotomy | 4 | 0 | – | 3 | 0 | – | 1 | 0 | – |
| Length of hospital
stay, days | 9.9±7.2 | 9.9±8.4 | 0.99 | 11.0±10.7 | 9.3±6.5 | 0.49 | 9.3±3.6 | 10.4±9.6 | 0.46 |
| Days to bowel
movement after surgery | 3.9±3.6 | 3.8±1.9 | 0.75 | 2.3±0.9 | 2.7±0.9 | 0.14 | 3.7±1.7 | 3.5±1.9 | 0.71 |
| Complications | 7 | 8 | 0.51 | 4 | 3 | 0.80 | 3 | 5 | 0.27 |
| Wound
infection | 2 | 0 |
| 1 | 0 |
| 1 | 0 |
|
|
Anastomotic leakage | 3 | 4 |
| 2 | 1 |
| 1 | 3 |
|
|
Ileus | 2 | 2 |
| 1 | 1 |
| 1 | 1 |
|
|
Urinary | 0 | 1 |
| 0 | 0 |
| 0 | 1 |
|
|
Other | 0 | 1c |
| 0 | 1c |
| 0 | 0 | – |
| Readmission within
30 days after surgery | 0 | 0 | – | 0 | 0 | – | 0 | 0 | – |
| No. of harvested
lymph nodes | 19.9±10.2 | 23.0±13.0 | 0.11 | 22.8±10.3 | 26.3±16.9 | 0.36 | 19.4±9.4 | 20.9±9.2 | 0.66 |
| Margin of specimen,
mm |
|
|
|
|
|
|
|
|
|
|
Proximal | 106.8±75.1 | 110.2±62.3 | 0.71 | 156.3±89.7 | 137.6±74.9 | 0.41 | 77.0±43.7 | 93.2±44.7 | 0.09 |
|
Distal | 80.6±45.5 | 74.0±32.3 | 0.33 | 82.1±35.9 | 175.5±34.7 | 0.49 | 79.6±50.2 | 73.0±31.0 | 0.48 |
| Tumor size, mm | 40.6±20.8 | 42.5±22.6 | 0.60 | 46.3±22.1 | 44.9±26.8 | 0.84 | 37.1±19.5 | 40.8±19.4 | 0.38 |
Characteristics of patients undergoing
SLC
Next, an investigation was performed to determine
whether the residents who were able to perform MLC successfully
were similarly able to perform SLC.
For SLC, the total patient characteristics did not
differ significantly between the staff and resident groups (age,
69.5±10.7 vs. 69.1±9.9 years, respectively; P=0.88; and BMI,
23.5±3.8 kg/m2 vs. 23.1±4.0 kg/m2,
respectively; P=0.66). For left-sided colon cancer, prior surgery
differed significantly between the staff and resident groups
(P=0.01). No other clinical variables, i.e., ASA class and tumor
location, differed significantly between the two groups. When
comparing these variables between the groups on the basis of tumor
location (right- vs. left-sided colon cancer), no significant
differences were observed (Table
III).
 | Table III.Characteristics of patients who
underwent single-incision laparoscopic colectomy. |
Table III.
Characteristics of patients who
underwent single-incision laparoscopic colectomy.
|
| Total | Righta | Leftb |
|---|
|
|
|
|
|
|---|
|
Characteristics | Staff (n=49) | Resident
(n=30) | P-value | Staff (n=18) | Resident (n=9) | P-value | Staff (n=31) | Resident
(n=21) | P-value |
|---|
| Age, years | 69.5±10.7 | 69.1±9.9 | 0.88 | 72.6±10.4 | 77.7±7.5 | 0.15 | 66.6±10.9 | 66.9±8.5 | 0.92 |
| Gender |
|
|
|
|
|
|
|
|
|
|
Male | 24 | 16 | 0.89 | 7 | 4 | 0.78 | 17 | 10 | 0.82 |
|
Female | 25 | 14 |
| 11 | 5 |
| 14 | 11 |
|
| BMI,
kg/m2 | 23.5±3.8 | 23.1±4.0 | 0.66 | 24.2±3.9 | 22.6±3.2 | 0.98 | 23.1±3.6 | 23.4±5.3 | 0.84 |
| ASA class |
|
|
|
|
|
|
|
|
|
| 1 | 4 | 2 | 0.96 | 0 | 1 | 0.3 | 4 | 1 | 0.59 |
| 2 | 39 | 24 |
| 17 | 7 |
| 22 | 17 |
|
| 3 | 6 | 4 |
| 1 | 1 |
| 5 | 3 |
|
| Prior surgery | 8 | 12 | 0.04 | 6 | 4 | 0.89 | 2 | 8 | 0.01 |
| Tumor location |
|
| 0.61 |
|
|
|
|
|
|
|
Cecum | 7 | 2 |
|
|
|
|
|
|
|
|
Ascending colon | 11 | 7 |
|
|
|
|
|
|
|
|
Descending colon | 0 | 1 |
|
|
|
|
|
|
|
| Sigmoid
colon | 22 | 15 |
|
|
|
|
|
|
|
|
Rectosigmoid colon | 9 | 5 |
|
|
|
|
|
|
|
Surgical outcomes of patients
undergoing SLC
The operative statistics are listed in Table IV. Total surgical outcomes, including
operative time, blood loss, hospital stay, number of harvested
lymph nodes, margin of the resected specimen and tumor size, were
similar between the staff and resident groups. The operative
complications were comparable between the two groups (staff group,
n=4; and resident group, n=4; P=0.46). There was no mortality in
either group; however, there was 1 readmission within 30 days after
surgery in the resident group, due to the development of an
intra-abdominal abscess.
 | Table IV.Surgical outcomes of patients who
underwent single-incision laparoscopic colectomy. |
Table IV.
Surgical outcomes of patients who
underwent single-incision laparoscopic colectomy.
|
| Total | Righta | Leftb |
|---|
|
|
|
|
|
|---|
| Variables | Staff (n=49) | Resident
(n=30) | P-value | Staff (n=18) | Resident (n=9) | P-value | Staff (n=31) | Resident
(n=21) | P-value |
|---|
| Operative time,
min | 192.5±58.9 | 217.5±199.0 | 0.88 | 195.5±62.5 | 174.1±69.6 | 0.47 | 188.5±41.7 | 247.6±107.4 | 0.03 |
| Estimated blood
loss, ml | 57.7±161.7 | 22.0±57.7 | 0.32 | 128.8±243.9 | 31.7±62.5 | 0.25 | 24.2±69.7 | 15.4±55.5 | 0.71 |
| Final incision,
mm | 34.9±5.6 | 34.3±8.1 | 0.76 | 36.6±5.7 | 32.8±7.1 | 0.15 | 33.9±5.4 | 35.4±8.8 | 0.57 |
| Conversion to
laparotomy | 1 | 0 | – | 0 | 0 | – | 1 | 0 | – |
| Length of hospital
stay, days | 9.0±7.3 | 7.7±3.8 | 0.44 | 9.4±0.5 | 6.2±1.0 | 0.32 | 8.7±5.4 | 8.7±4.8 | 0.98 |
| Complications | 4 | 4 | 0.46 | 1 | 0 | – | 3 | 4 | 0.33 |
| Wound
infection | 1 | 0 |
| 0 | 0 |
| 1 | 0 |
|
|
Anastomotic leakage | 0 | 0 |
| 0 | 0 |
| 0 | 0 |
|
|
Ileus | 2 | 2 |
| 0 | 0 |
| 2 | 2 |
|
|
Urinary | 0 | 0 |
| 0 | 0 |
| 0 | 0 |
|
|
Incisional hernia | 0 | 0 |
| 0 | 0 |
| 0 | 0 |
|
|
Other | 1c | 1d |
| 1c | 0 |
| 0 | 1d |
|
| Readmission within
30 days after surgery | 0 | 1 | – | 0 | 0 | – | 0 | 1 | – |
| No. of harvested
lymph nodes | 21.1±7.4 | 23.6±10.2 | 0.20 | 21.6±8.8 | 23.9±11.1 | 0.57 | 20.4±6.4 | 22.2±10.0 | 0.21 |
| Margin of specimen,
mm |
|
|
|
|
|
|
|
|
|
| Proximal | 79.2±55.7 | 84.4±37.8 | 0.69 | 116.3±62.7 | 93.1±42.3 | 0.33 | 48.0±18.5 | 68.5±34.9 | 0.11 |
| Distal | 67.1±34.5 | 69.8±56.9 | 0.82 | 72.3±30.5 | 80.3±84.6 | 0.74 | 62.4±37.7 | 62.5±27.5 | 0.99 |
| Tumor size, mm | 43.5±27.5 | 36.2±18.4 | 0.27 | 50.2±31.4 | 38.1±20.3 | 0.31 | 37.8±23.1 | 34.8±17.7 | 0.70 |
For right-sided colon cancer, the operative time was
marginally longer in the staff group compared with that in the
resident group (195.5±62.5 vs. 174.1±69.6 min, respectively;
P=0.47), whereas it was significantly shorter in the staff group
compared with that in the resident group for left-sided colon
cancer (188.5±41.7 vs. 247.6±107.4 min, respectively; P=0.03;
Table IV). For right- and left-sided
colon cancer, the estimated blood loss, length of surgical margin
and number of harvested lymph nodes were similar between the two
groups. All the procedures performed by the residents were
successfully completed, whereas one procedure in the staff group
was converted to open surgery due to rectal injury. No patient
required additional ports in either group. Postoperative ileus
occurred in left-sided colon cancer (staff group, n=2; and resident
group, n=2) and 1 incisional infection occurred in the staff group.
There was no anastomotic leakage in either group (Table IV).
Time analysis of SLC
When the surgical process was examined in seconds,
no significant differences were found in all 4 procedures for the
right colon between the staff and resident groups; however, for the
left colon, the residents required a significantly longer time to
complete the procedure from blood vessel dissection to the closure
of the mesentery of the dissected intestine compared with the staff
surgeons (3,470.1±1,258.5 vs. 5,218.6±2,341.2 sec; P=0.01)
(Table V).
 | Table V.Time analysis of the surgical
procedure in patients who underwent single-incision laparoscopic
colectomy. |
Table V.
Time analysis of the surgical
procedure in patients who underwent single-incision laparoscopic
colectomy.
|
| Righta | Leftb |
|---|
|
|
|
|
|---|
| Procedures | Staff (n=18) | Resident (n=9) | P-value | Staff (n=31) | Resident
(n=21) | P-value |
|---|
| i) From camera
insertion to start of mesenteric incision | 880.0±73.2 | 1,287.8±239.6 | 0.55 | 616.8±348.2 | 609.6±223.3 | 0.95 |
| ii) From start of
mesenteric incision and identification of the origin of the
mesenteric artery to clip insertion |
2,539.1±1,353.9 |
1,889.4±1,128.4 | 0.24 | 1,707±732.7 | 1,837.3±774.4 | 0.65 |
| iii) From clip
insertion to vessel dissection | 2,370.9±403.5 | 767.8±242.8 | 0.25 | 1,114.8±362.4 | 1,064.2±536.1 | 0.76 |
| iv) From vessel
dissection to exposure of colon resection margin |
2,521.6±1,585.5 |
2,436.7±1,434.1 | 0.89 |
3,470.1±1,258.5 |
5,218.6±2,341.2 | 0.01 |
| v) From exposure of
colon resection margin to colon dissection |
|
|
| 324.2±224.5 | 451.9±354.6 | 0.24 |
| vi) From camera
insertion to anastomosis |
|
|
| 936.8±258.2 | 798.7±309.8 | 0.71 |
Discussion
SLC is potentially accompanied by the advantages of
a minimally invasive surgical procedure. Reduced-port surgery aims
to reduce the size and number of ports for preserving the view
afforded by the laparoscope, while making the surgery less
invasive. Previous studies have reported the advantages of reducing
the number of laparoscopic ports, including better cosmetic
results, reduced postoperative pain and shorter recovery time;
however, there are associated technical complexities, such as
instrument crowding and insufficient counter traction (11–15). In
addition, SLC has the limitation of a learning curve and an
advanced skill of laparoscopic surgery. For widespread utilization,
early introduction of the SLC techniques in surgical residency is
required. This study demonstrated the feasibility and safety of
surgical residents performing SLC under the guidance of colorectal
surgeons experienced in this technique.
For MLC, no significant difference was observed
between staff and resident surgeons in terms of peri- or
postoperative short-term results. This suggests that, under
supervision by a surgeon specializing in colorectal cancer,
residents were able to perform surgery for colon cancer with a
satisfactory level of safety. We formulated the hypothesis that
residents who were able to perform MLC satisfactorily in this
manner were also able to perform SLC to a level comparable to that
of staff members, and this hypothesis was retrospectively
investigated.
In this study, residents experienced in MLC
performed the surgical procedures. In addition, no limitations in
terms of patient age, BMI, ASA class or tumor diameter were
imposed, as restricting patient selection cannot reconstruct the
actual conditions in medical practice; however, the performance of
the residents is likely to have been accurately represented in this
study, as no restrictions were imposed regarding patient
demographics.
The examination of surgical outcomes revealed that
the operative time of the residents was 174.1±69.6 min for the
right colon and 247.6±107.4 min for the left colon for SLC
(Table IV). The operative time for
both right- and left-colon surgery has been reported to be in the
range of 66–502 min (7). In that
study, 13 of 31 patients had cancer, but no detailed information
was provided on lymphadenectomy, such as CVL and CME (8–10);
therefore, it was not feasible to directly compare that study to
our findings. However, our results appear to be consistent. The
number of harvested lymph nodes is crucial in cancer surgery and
there was no significant difference in the number of harvested
nodes between the staff and resident groups (Table IV). The median number of harvested
lymph nodes has been reported to be 17 (range, 10–30) in
right-sided colon cancer and 14 (range, 6–16) in left-sided colon
cancer; our results are consistent with that report (16).
A comparison of the operative time revealed no
significant differences in most procedures between the staff and
resident groups; however, in left-sided colon surgery, the
residents required a significantly longer time to complete the
procedure from blood vessel dissection to the closure of the
mesentery of the dissected colon compared with the staff surgeons
(3,470.1±1,258.5 vs. 5,218.6±2,341.2 sec; P=0.01) (Table V). This appears to be due to the
difficulty of separation procedures to be followed when exposing
the colon along with a dissection line. The grasping position is
critical to successful SLC, since a surgeon tries to preserve the
view using a pair of forceps and gravity and applies tension to the
tissue. When video recordings of the operations performed by the
staff and residents were compared, the residents picked up the
colon several times and they appeared to find it difficult to
preserve the operative view. This may be the cause of the longer
operative time in patients undergoing resident-performed SLC for
left-sided colon cancer. By contrast, no significant difference was
observed for right-sided colon cancer (Table IV); one of the reasons for this is
that fewer steps are required to perform laparoscopic surgery for
right-sided compared with left-sided colon cancer, whereas another
reason is that the supervising staff surgeon may act as an
operator's eye during resident-performed SLC, providing a good
operative field in a stable manner, which is important for
laparoscopic surgery. By contrast, the residents take operative
view during staff surgeon-performed SLC, which causes several
problems, such as unstable surgical field and mutual interference
of the camera and forceps.
Our study demonstrated that SLC was safely performed
with the support of the residents, apart from 1 patient in the
staff group, who required additional port placement due to rectal
injury from the insertion of an automatic anastomosis and 1 patient
in the resident group requiring hospital readmission for
intra-abdominal abscess. Our examination of all surgical outcomes
revealed that they are similar to those reported by a recent
systematic review (17), which
included 23 studies, involving a total of 378 patients undergoing
SLC. In a highly selected cohort with low BMIs, the authors found
operative times ranging between 83 and 225 min, a mean estimated
blood loss of 0–115 ml, a 6.9% conversion rate, additional port
placement in 5% of the cases and low rates of morbidity (13%) and
mortality (0.5%). The oncological outcomes in that review were
adequate, with lymph node yields varying from 13.5 to 27, and
negative margins reported in all the cases. The hospital stay
varied between 1.9 and 9.8 days. When comparing with these results
of oncological outcomes, our results appear to be acceptable
(Table IV).
SLC is likely to be widely used in the future;
however, certain surgeons suggest that only experts are able to
perform this procedure, which may deprive young surgeons of the
opportunity to receive education and training and play an active
role in surgery, as SLC is likely to become a widely applied
surgical procedure. An active involvement of the residents in
surgery is important for a long-term, widespread use of SLC. The
results of our study indicated that residents experienced in MLC
were able to perform SLC with the same level of safety as the staff
surgeons. Our study results also demonstrated that it is easier for
the residents to perform SLC for right-sided colon cancer, whereas
the closure of the mesentery of the dissected intestine in
left-sided colon cancer was the main challenge.
In conclusion, the results of this study indicated
that the residents were able to perform SLC safely under the
guidance of the staff surgeons and that it was easier for the
residents to perform SLC for right-sided colon cancer. Therefore,
this may prove useful for a widespread application of SLC in the
surgical medical practice and resident education and we hope that
more residents will be actively involved in SLC.
References
|
1
|
Yasuda K, Sonoda K, Shiroshita H, Inomata
M, Shiraishi N and Kitano S: Laparoscopically assisted distal
gastrectomy for early gastric cancer in the elderly. Br J Surg.
91:1061–1065. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choi SI, Lee KY, Park SJ and Lee SH:
Single port laparoscopic right hemicolectomy with D3 dissection for
advanced colon cancer. World J Gastroenterol. 16:275–278. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ramos-Valadez DI, Patel CB, Ragupathi M,
Bartley Pickron T and Haas EM: Single-incision laparoscopic right
hemicolectomy: Safety and feasibility in a series of consecutive
cases. Surg Endosc. 24:2613–2616. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hamzaoglu I, Karahasanoglu T, Baca B,
Karatas A, Aytac E and Kahya AS: Single-port laparoscopic
sphincter-saving mesorectal excision for rectal cancer: Report of
the first 4 human cases. Arch Surg. 146:75–81. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Merchant AM and Lin E: Single-incision
laparoscopic right hemicolectomy for a colon mass. Dis Colon
Rectum. 52:1021–1024. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Uematsu D, Akiyama G, Matsuura M and Hotta
K: Single-access laparoscopic colectomy with a novel multiport
device in sigmoid colectomy for colon cancer. Dis Colon Rectum.
53:496–501. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miller S, Causey MW, Damle A, Maykel J and
Steele S: Single-incision laparoscopic colectomy: Training the next
generation. Surg Endosc. 27:1784–1790. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hohenberger W, Weber K, Matzel K,
Papadopoulos T and Merkel S: Standardized surgery for colonic
cancer: Complete mesocolic excision and central ligation-technical
notes and outcome. Colorectal Dis. 11:354–364; discussion.
364-365.2009. View Article : Google Scholar
|
|
9
|
West NP, Hohenberger W, Weber K, Perrakis
A, Finan PJ and Quirke P: Complete mesocolic excision with central
vascular ligation produces an oncologically superior specimen
compared with standard surgery for carcinoma of the colon. J Clin
Oncol. 28:272–278. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
West NP, Kobayashi H, Takahashi K, et al:
Understanding optimal colonic cancer surgery: Comparison of
Japanese D3 resection and European complete mesocolic excision with
central vascular ligation. J Clin Oncol. 30:1763–1769. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen WT, Chang SC, Chiang HC, et al:
Single-incision laparoscopic vs. conventional laparoscopic right
hemicolectomy: A comparison of short-term surgical results. Surg
Endosc. 25:1887–1892. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ramos-Valadez DI, Ragupathi M, et al:
Single-incision vs. conventional laparoscopic sigmoid colectomy: A
case-matched series. Surg Endosc. 26:96–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Champagne BJ, Lee EC, Leblanc F, Stein SL
and Delaney CP: Single-incision vs. straight laparoscopic segmental
colectomy: A case-controlled study. Dis Colon Rectum. 54:183–186.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Champagne BJ, Papaconstantinou HT, Parmar
SS, et al: Single-incision vs. standard multiport laparoscopic
colectomy: A multicenter, case-controlled comparison. Ann Surg.
255:66–69. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Poon JT, Cheung CW, Fan JK, Lo OS and Law
WL: Single-incision vs. conventional laparoscopic colectomy for
colonic neoplasm: A randomized, controlled trial. Surg Endosc.
26:2729–2734. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chew MH, Wong MT, Lim BY, Ng KH and Eu KW:
Evaluation of current devices in single-incision laparoscopic
colorectal surgery: A preliminary experience in 32 consecutive
cases. World J Surg. 35:873–880. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Makino T, Milsom JW and Lee SW:
Feasibility and safety of single-incision laparoscopic colectomy: A
systematic review. Ann Surg. 255:667–676. 2012. View Article : Google Scholar : PubMed/NCBI
|