Introduction
Pyomyoma (suppurative leiomyoma) is a rare, but
life-threatening, condition resulting from infarction and infection
of uterine leiomyoma (1,2). Incidence of pyomyoma has decreased due
to the development of antibiotics. Since 1945, only 50 pyomyoma
cases have been documented in the literature, with a mortality rate
of 6% (3/50) (3–5). The most likely cause of mortality was
delayed and difficult diagnosis. Although the triad of pyomyoma are
sepsis, leiomyoma, and no other source of infection (5), it may present with silent or
non-specific symptoms, which results in delayed diagnosis and
treatment. Visualization of intratumoral gas formation may be
suggestive of pyomyoma, but has not been consistently reported in
all cases. Furthermore, large abdominal complex masses are likely
to be first suspected as pelvic malignancies if found incidentally
in perimenopausal women.
The present study experienced a rare case of large
uterine pyomyoma in a perimenopausal woman who presented with
anemia gravis, severe inflammatory reaction and cachexia. A total
of 50 reported cases of pyomyoma in the literature since 1945 were
also studied.
Case report
A 53-year-old multigravida woman with 7 months of
amenorrhea was referred to the Department of Obstetrics and
Gynecology (Wakayama Medical University, Wakayama, Japan) due to
gradual abdominal distension starting 2 years previously. The
patient exhibited muscle weakness and walking difficulty, but no
fever, abdominal pain or metrorrhagia. Her abdomen was swollen to
the size of a beach ball, with a 126 cm abdominal circumference and
body weight of 84.1 kg. An intrauterine device (IUD) had been
inserted following her third birth, and no history of any lower
abdominal or pelvic discomfort, leiomyoma, pelvic surgery, or other
predisposing factors were known. The present study was unable to
determine the uterine cervix with pelvic examination due to its
deviation, and was unable to acquire cytopathological findings of
the cervix and endometrium. Transvaginal and transabdominal
ultrasound examinations revealed a large abdominal mass with
heterogeneous echogenicity. Computed tomography (CT) and magnetic
resonance imaging (MRI) revealed a large unilocular mass with an
irregular surface and thickened wall, occupying the abdominal
cavity without gas formation (Fig.
1). Contrast CT revealed an expanded branch of the left
internal iliac artery, which was suspected to be the uterine
artery, surrounding the mass (Fig.
1B). Hemoglobin levels were 5.7 g/dl, white blood cell count
was 57,300/µl and C-reactive protein was elevated to 20.24 mg/dl.
Cancer antigen (CA)125 was also elevated to 200 U/ml. Blood and
vaginal cultures were negative. Possible diagnoses of the large
abdominal mass included gynecologic tumor types (benign or
malignant ovarian tumor, uterine sarcoma or pyometra) and
gastrointestinal stromal tumor or mucocele of the appendix.
Gastroscopy revealed no specific findings and colonoscopy revealed
difficulty of insertion above the sigmoid colon due to pressure
from the mass. Due to the finding of the uterine artery by contrast
CT, the origin of the mass was suspected to be the uterus.
Following antibiotic medication and blood transfusion, the patient
underwent a total abdominal hysterectomy and bilateral
salpingo-oophorectomy. Ureteral stents were indwelled in each side
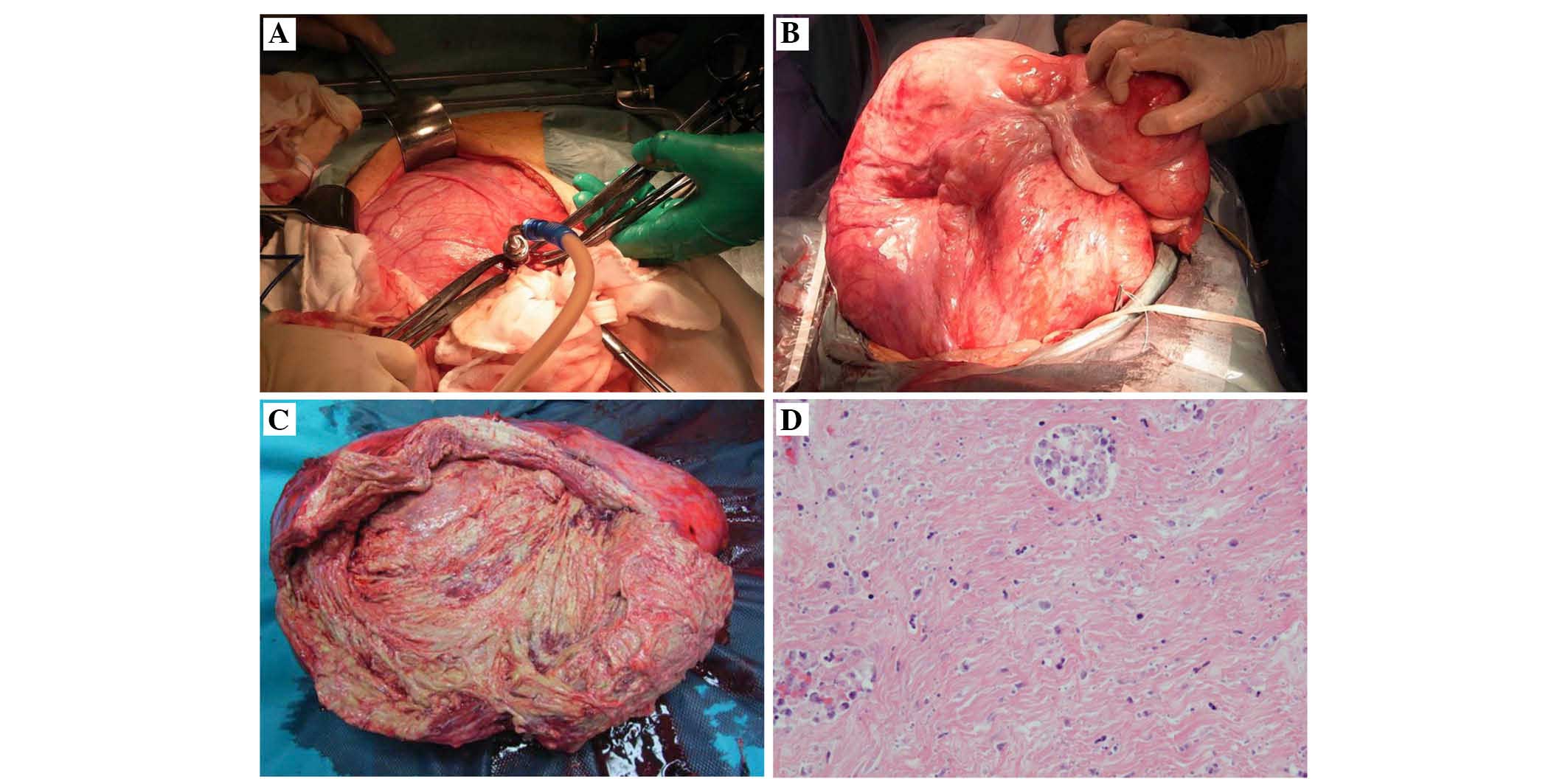
pre-operatively. Intraoperative findings demonstrated a solid tumor
arising from the back of the uterine body with normal bilateral
adnexa. Prior to removal, 12.4 liters of purulent, malodorous fluid
was drained from the tumor (Fig. 2A and
B). The resected mass was 50×37×20 cm in size and 13.5 kg in
weight. The surrounding myometrium appeared normal and measured 3
cm in thickness, and the cut surface of the mass was
purple-yellowish (Fig. 2C). Cultures
of the pus in the tumor revealed the presence of Streptococcus
agalactiae. An IUD was identified near the cervix, however
culture was negative. The pathological diagnosis was leiomyoma with
marked necrosis and chronic inflammation, with no evidence of
malignancy (Fig. 2D). Following
resection of the tumor, the patient's weight decreased to 55 kg.
The post-operative course was uneventful and the patient was
discharged from the hospital on post-operative day 14. At 4 months
follow-up, the patient's weight had increased to 62 kg due to a
good appetite.
Discussion
Pyomyoma occurs in both post-and pre-menopausal
women, however, the risk of suppurative myoma is increased by
pregnancy (1,2). For post-menopausal patients, systemic
vascular changes have been suggested to be the likely underlying
cause of pyomyoma (6). Necrosis of
the leiomyoma caused by vascular flow insufficiency in the uterus
following menopause is also a possible cause. A history of uterine
leiomyoma, pregnancy, abortion, menopause, uterine artery
embolization (UAE), IUD, vascular insufficiency (diabetes,
hypertension and atherosclerosis) and systemic disease or infection
may be predisposing factors for pyomyoma; however, definitive
diagnoses remain difficult. Although rapid clinical diagnosis for
pyomyoma is often difficult due to its low incidence and the
requirement to rule out the possibility of malignancy, mortality
has decreased due to the improvement in surgical treatments,
including myomectomy and hysterectomy, and broad-spectrum
antibiotics.
A MEDLINE search since 1945 revealed only 50
reported cases of pyomyoma: 27 were non-pregnant woman (mean age,
51.8 years; range, 36–69-years-old; Table I) (3–29) and 23
cases were associated with pregnancy or abortion (mean age, 33.6
years; range, 28–44-years-old). The mean pyomyoma size in
non-pregnancy and pregnancy-associated cases were 16.2 cm (3–38 cm)
and 13.5 cm (5–58 cm), respectively. Non-pregnancy pyomyoma tended
to be larger compared with pregnancy-associated pyomyoma, and the
present case was the largest among all reported cases of
non-pregnancy-associated pyomyoma. Severe anemia gravis and
inflammatory reaction were described in numerous pyomyoma cases,
including the present study. The presentation and complications of
pyomyoma vary. It has been shown that 2/50 cases had a history of
IUD usage (7,30), 5/50 cases had UAE (8–12), 6/50
cases had vascular insufficiency (4,13–17) and
8/50 cases demonstrated gas production (6,8–10,12,31–33).
Notably, gas production was observed in 4/5 UAE cases (8–10,12).
Although pyomyoma arises spontaneously, post-partum,
post-instrumentation or post-surgery have been reported in the
literature, only two cases include a IUD, and only one case has
been previously reported in a non-pregnant woman (7). Knowledge of IUD history may be helpful
in the diagnosis of pyomyoma.
 | Table I.Previously reported cases of pyomyoma
without pregnancy, since 1945. |
Table I.
Previously reported cases of pyomyoma
without pregnancy, since 1945.
| Author, year | Age | Key points | Laboratory data | Size |
Treatmenta | Refs. |
|---|
| Miller et al,
1945 | 51 | STM | WBC 38,700/µl | 35×25 cm | Subtotal hysterectomy
+ BSO | (3) |
| Kaufmann et
al, 1974 | 58 | STM, HT, DM | WBC 28,800/µl, Hb 7.3
g/dl | ns | No treatment | (4) |
| Greenspoon et
al, 1990 | 49 | STM | WBC 21,200/µl, Hb 7.4
g/dl | 11.5×9×11 cm, 2.5
kg | No treatment | (5) |
| Chen et al,
2014 | 67 | Gas production | WBC 12,300/µl, CA125
29.98 U/ml | 25×20×15 cm | TAH + BSO | (6) |
| Manchana et
al, 2007 | 42 | IUD | WBC 29,380/µl, Hb 8.7
g/dl, CA125 65.2 U/ml | 15×15 cm | TAH + BSO | (8) |
| Kitamura et
al, 2005 | ns | UAE, gas
production | ns | ns | TAH | (9) |
| Abulafia et
al, 2010 | 48 | UAE, gas
production | WBC 22,600/µl, Hb 8.1
g/dl | 11×10×6 cm | TAH | (10) |
| Shukla et al,
2012 | 65 | UAE, gas
production | WBC 7,900/µl | 12×10 cm | TAH + BSO | (11) |
| Pinto et al,
2012 | 36 | UAE | WBC normal, Hb 9.5
g/dl | 6.8×5.6×5.5 cm | Laparoscopic
drainage | (12) |
| Rosen et al,
2013 | 47 | UAE, gas
production | WBC 15,900/µl | ns | Supracervical
hysterectomy + RSO | (13) |
| Weiss et al,
1976 | 59 | DM | ns | 15 cm | TAH + BSO | (14) |
| Genta et al,
2001 | 60 | DM, DVT | WBC 14,100/µl, Hb 7.7
g/dl, CA125 109.7 U/ml | 25×20 cm | TAH + BSO +
omentectomy | (15) |
| Fletcher et
al, 2009 | 44 | DM | WBC 22,500/µl, Hb 7.8
g/dl, CA125 17.5 U/ml | 15.5×16×9 cm | TAH + BSO | (16) |
| Ono et al,
2014 | 69 | DM | WBC 10,710/µl, CRP
2.71 mg/dl, Hb 7.6 g/dl | ns | TAH | (17) |
| Goyal et al,
2015 | 42 | DM | WBC 10,200/µl, Hb
9.5 g/dl | 6 cm | Subtotal
hysterectomy + | (18) |
| Lee et al,
2010 | 46 | FDG-PET | WBC 10,100/µl, Hb
8.8 g/dl, CA125 59.2 U/ml | 38×30×10 cm, 3
kg | LSO +TAH | (22) |
| Bedrosin et
al, 1956 | 50 | N/A | WBC 12,800/µl, Hb
11.0 g/dl | 7 cm | TAH + BSO | (23) |
| Fuller et
al, 1985 | 68 | N/A | WBC 24,000/µl | 10 cm | TAH + BSO | (24) |
| Yang and Wang,
1999 | 46 | N/A | WBC 45,400/µl, Hb
7.0 g/dl | 13×12 cm | TAH + BSO | (25) |
| Gupta et al,
1999 | 60 | N/A | WBC 14,000/µl | 30×25 cm, 4.3
kg | TAH + BSO | (26) |
| Sah et al,
2005 | 64 | N/A | WBC 15,000/µl, Hb
8.0 g/dl | 22×23×10 cm, 3.5
kg | TAH + BSO | (27) |
| Yeat et al,
2005 | 53 | N/A | WBC 52,600/µl, CRP
42.4 mg/dl, Hb 8.6 g/dl | 12×12×10 cm, 1,020
g | TAH + BSO | (28) |
| Patwardhan and
Bulmer, 2007 | 38 | N/A | WBC 18,500/µl, CRP
22.5 mg/dl | ns | Myomectomy | (29) |
| Chen et al,
2010 | 46 | N/A | WBC 13,000/µl, Hb
7.9 g/dl | 14.3×12×8 cm | TAH | (30) |
| Kuriyama et
al, 2010 | 51 | N/A | WBC 15,900/µl, CRP
13.1 mg/dl | ns | TAH | (31) |
| Zangeneh et
al, 2010 | 47 | N/A | WBC normal, Hb 10.3
g/dl | 3×5 cm | TAH + BSO | (32) |
| Liu and Chen,
2011 | 42 | N/A | WBC 42,880/µl | 9.0×8.0×6.5 cm | Open drainage | (33) |
| Present report | 53 | IUD | WBC 57,300/µl, CRP
20.24 mg/dl, Hb 5.7g/dl, CA125 200.2 U/ml | 50×37×20 cm, 13.5
kg | TAH + BSO | – |
Pyomyoma was often associated with polymicrobial
infection. Among the 50 reported cases, infection by
Staphylococcus species was reported in 8 cases,
Streptococcus species in 7 cases, Escherichia coli in
6 cases, Enterococcus faecalis in 5 cases,
Clostridium species in 3 cases, Proteus species in 2
cases and Candida species in 2 cases. In the present case,
Streptococcus agalactiae was cultured from the pus and
tumor, however, not from the blood and vagina, suggesting the
infection existed focally within the tumor. Therefore, conservative
management with pre-operative broad-spectrum antibiotics and
appropriate surgery was performed successfully. For surgical
treatment, hysterectomy was performed in 32 cases, myomectomy in 10
cases and drainage in 6 cases.
Diagnosis of large pyomyoma is difficult since
surgery is required for a definitive diagnosis. A malignant tumor,
in particular ovarian cancer, was initially suspected due to the
findings of a large abdominal mass with signs of necrosis in a
cachexic perimenopausal woman with an elevated CA125 level. In a
previous report, imaging analysis was shown to identify only
non-specific results (6). MRI and
positron emission tomography did not improve the specificity of
pyomyoma diagnosis. Although intratumoral gas formation is markedly
suggestive of pyomyoma on ultrasound and CT imaging, gas formation
is not consistently observed, as with the present case. In the
present case, contrast CT contributed to the diagnosis of pyomyoma
due to the identification of the uterine artery location.
CA125 has been observed to be increased in other
gynecologic and non-gynecologic malignancies, as well as in a
variety of benign disorders, including leiomyoma. Among the
previously reported cases of pyomyoma, 5 cases reported CA125
levels (6,7,14,15,18),
with a mean level of 56.3 U/ml (29.98–109.7 U/ml). CA125 was
measured only in non-pregnancy-associated cases, possibly due to
suspicion of gynecological malignancy based on the age of the
patient and size of tumor. Furthermore, in pregnancy-associated
cases, diagnosis of myoma was likely during pre-natal examination
prior to the onset of the symptom, which may have contributed to
the identification of the tumor origin. In the present case, CA125
level was the highest compared with the previously reported
cases.
To the best of our knowledge, this is the third
IUD-associated case of pyomyoma, with the largest tumor size and
highest CA125 level compared with previously reported non-pregnancy
cases. A large pyomyoma is difficult to distinguish from a
gynecological malignant tumor, particularly in perimenopausal,
cachectic women with non-specific clinical presentation and without
a history of leiomyoma. A history of IUD usage and contrast CT may
be helpful in the diagnosis of pyomyoma. Gynecologists and general
surgeons must be aware of the possibility of pyomyoma when
presented with a large abdominal tumor, and in certain cases,
surgery in combination with broad spectrum antibiotics may result
in a good outcome.
References
|
1
|
Mason TC, Adair J and Lee YC: Postpartum
pyomyoma. J Natl Med Assoc. 97:826–828. 2005.PubMed/NCBI
|
|
2
|
Kobayashi F, Kondoh E, Hamanishi J,
Kawamura Y, Tatsumi K and Konishi I: Pyomayoma during pregnancy: A
case report and review of the literature. J Obstet Gynaecol Res.
39:383–389. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miller I: Suppurating fibromyomas. Report
of a case with a review of the literature. Am J Obstet Gynecol.
50:522–526. 1945.
|
|
4
|
Kaufmann BN, Cooper VM and Cookson P:
Clostridium perfringens septicemia complicating degenerating
uterine leiomyomas. Am J Obstet Gynecol. 118:877–878. 1974.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Greenspoon JS, Ault M, James BA and Kaplan
L: Pyomyoma associated with polymicrobial bacteremia and fatal
septic shock: Case report and review of the literature. Obstet
Gynecol Surv. 45:563–569. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen JR, Yang TL, Lan FH and Lin TW:
Pyomyoma mimicking advanced ovarian cancer: A rare manifestation in
a postmenopausal virgin. Taiwan J Obstet Gynecol. 53:101–103. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Manchana T, Sirisabya N, Triratanachat S,
Niruthisard S and Tannirandorn Y: Pyomyoma in a perimenopausal
woman with intrauterine device. Gynecol Obstet Invest. 63:170–172.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kitamura Y, Ascher SM, Cooper C, Allison
SJ, Jha RC, Flick PA and Spies JB: Imaging manifestations of
complications associated with uterine artery embolization.
Radiographics. 25:(Suppl 1). S119–S132. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Abulafia O, Shah T, Salame G, Miller MJ,
Serur E, Zinn HL, Sokolovski M and Sherer DM: Sonographic features
associated with post-uterine artery embolization pyomyoma. J
Ultrasound Med. 29:839–842. 2010.PubMed/NCBI
|
|
10
|
Shukla PA, Kumar A, Klyde D and Contractor
S: Pyomyoma after uterine artery embolization. J Vasc Interv
Radiol. 23:423–424. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pinto E, Trovão A, Leitão S, Pina C, Mak
Fk and Lanhoso A: Conservative laparoscopic approach to a
perforated pyomyoma after uterine artery embolization. J Minim
Invasive Gynecol. 19:775–779. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rosen ML, Anderson ML and Hawkins SM:
Pyomyoma after uterine artery embolization. Obstet Gynecol. 121:(2
Pt 2 Suppl 1). S431–S433. 2013.
|
|
13
|
Weiss G, Shenker L and Gorstein F:
Suppurating myoma with spontaneous drainage through abdominal wall.
N Y State J Med. 76:572–573. 1976.PubMed/NCBI
|
|
14
|
Genta PR, Dias ML, Janiszewski TA,
Carvalho JP, Arai MH and Meireles LP: Streptococcus agalactiae
endocarditis and giant pyomyoma stimulating ovarian cancer. South
Med J. 94:508–511. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fletcher H, Gibson R, Williams N, Wharfe
G, Nicholson A and Soares D: A woman with diabetes presenting with
pyomyoma and treated with subtotal hysterectomy: A case report. J
Med Case Rep. 3:74392009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ono H, Kanematsu M, Kato H, Toyoki H,
Hayasaki Y, Furui T, Morishige K and Hatano Y: MR imaging findings
of uterine pyomyoma: Radiologic-pathologic correlation. Abdom
Imaging. 39:797–801. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Goyal S, Mohan H, Punia RS and Tandon R:
Subserosal pyomyoma and tubo-ovarian abscess in a diabetic patient.
J Obstet Gynaecol. 35:101–102. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee SR, Kim BS and Moon HS: Magnetic
resonance imaging and positron emission tomography of a giant
multiseptated pyomyoma simulating an ovarian cancer. Fertil Steril.
94:1900–1902. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bedrosian L, Gabriels AG Jr and Hengerer
AD: Ruptured suppurating myoma; a surgical emergency. Am J Obstet
Gynecol. 71:1145–1147. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fuller AF Jr and Lawrence WD: Case records
of the Massachusetts General Hospital. Case 23-1985. N Engl J Med.
312:1505–1511. 1985.PubMed/NCBI
|
|
21
|
Yang CH and Wang CK: Edwardsiella tarda
bacteraemia-complicated by acute pancreatitis and pyomyoma. J
Infect. 38:124–126. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gupta B, Sehgal A, Kaur R and Malhotra S:
Pyomyoma: A case report. Aust N Z J Obstet Gynecol. 39:520–521.
1999. View Article : Google Scholar
|
|
23
|
Sah SP, Rayamajhi AK and Bhadani PP:
Pyomyoma in a postmenopausal woman: A case report. Southeast Asian
J Trop Med Public Health. 36:979–981. 2005.PubMed/NCBI
|
|
24
|
Yeat SK, Chong KM, Pan HS, Cheng WC, Hwang
JL and Lee CC: Impending sepsis due to a ruptured pyomyoma with
purulent peritonitis: A case report and literature review. Taiwan J
Obstet Gynecol. 44:75–79. 2005. View Article : Google Scholar
|
|
25
|
Patwardhan A and Bulmer P: Pyomyoma as a
complication of uterine fibroids. J Obstet Gynaecol. 27:444–445.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chen ZH, Tsai HD and Sun MJ: Pyomyoma: A
rare and life-threatening complication of uterine leiomyoma. Taiwan
J Obstet Gynecol. 49:351–356. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kuriyama K, Makiishi T, Maeda S, Konishi T
and Hirose K: Acute bilateral renal cortical necrosis complicating
pyomyoma. Intern Med. 49:511–512. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zangeneh M, Alsadat Mahdavi A, Amini E,
Davar Siadat S and Karimian L: Pyomyoma in a premenopausal woman
with fever of unknown origin. Obstet Gynecol. 116:(Suppl 2).
S526–S528. 2010. View Article : Google Scholar
|
|
29
|
Liu HS and Chen CH: Subserosal pyomyoma in
a virgin female: Sonographic and computed tomographic imaging
features. Ultrasound Obstet Gynecol. 37:247–248. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wong TC, Bard DS and Pearce LW: Unusual
case of IUD associated postabortal sepsis complicated by an
infected necrotic leiomyoma, suppurative pelvic thrombophlebitis,
ovarian vein thrombosis, hematoperitoneum and drug fever. J Ark Med
Soc. 83:138–147. 1986.PubMed/NCBI
|
|
31
|
Karcaaltincaba M and Sudakoff GS: CT of a
ruptured pyomyoma. AJR Am J Roentgenol. 181:1375–1377. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nguyen QH and Gruenewald SM: Sonographic
appearance of a postpartum pyomyoma with gas production. J Clin
Ultrasound. 36:186–188. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Stroumsa D, Ben-David E, Hiller N and
Hochner-Celnikier D: Severe clostridial pyomyoma following an
abortion does not always require surgical intervention. Case Rep
Obstet Gynecol. 2011:3646412011.PubMed/NCBI
|