Introduction
Penicillium marneffei is the only
Penicillium that is a dimorphic fungus in China and
South-Eastern Asia. In 1956, P. marneffei was first time
isolated from the hepatic lesions of a bamboo-rat (Rhizomys
sinensis). The disease can occur in healthy individuals;
however, is more commonly detected in immunodeficient or
immunnosuppressed patients. With the recently increasing incidence
of HIV infection, reports of P. marneffei infection are
increasing. It was one of the top three AIDS-defining opportunistic
infections, alongside tuberculosis and cryptococcosis.
Penicillium marneffei often violates multiple body organs,
causes immune deficiency or immune suppression, and is becoming
more common in recent years (1–3), and
this trend will continue to deteriorate. Since the clinical
manifestation is complicated and does not have very high
specificity, this often leads to improper diagnosis, mistakes when
deciding the correct treatment duration, and therefore, the
infection is associated with a high mortality rate (4). Diagnosis of Penicillium fungal
disease is predominantly isolated from clinical specimens of
Penicillium marneffei, and after a thorough treatment it can
be cured. Itraconazole and ketoconazole is the best choice for mild
and moderate infection with P. marneffei, and amphotericin B
may be effective in the treatment of severe infection with P.
marneffei. To date, no cases of P. marneffei infection
recurrence following treatment have been reported. The present
study described the first case, to the best of our knowledge, of a
non-acquired immune deficiency syndrome patient, who is not
immunocompromised, with complications following P. marneffei
infection without any strict treatment, causing disease recurrence.
The present study described the details of the case with emphasis
on the importance of standard treatment. Increased clinician and
patient attention to the disease is essential to prevent any
recurrence, even in non-immunocompromised patients.
Case report
A 36-year-old female, a native of Hunan province in
central China, had a 2 month history of subcutaneous abscess and a
1 month history of intermittent fever, cough and anhelation. The
patient was informed that she had been infected with P.
marneffei 1 year previously. Since then, the masses had
gradually increased both in size and numbers. Despite the use of
therapy with various antibacterial antibiotics for tuberculosis,
the granulomatous lesions in the left upper lobe of the lungs
persisted, the condition failed to improve and gradually
deteriorated. For further treatment, the patient was admitted to
The Second Xiangya Hospital of Central South University (Changsha,
China) on February 25th 2015. Physical examination revealed a body
temperature of 39.1°C, a pulse rate of 140 beats/min. Routine blood
examination revealed the following: White blood cell count,
15.13×10−9/l (normal level, 3.5–9.5×109/l),
red blood cell count, 3.39×1012/l (normal level,
4.3–5.8×1012/l) and hemoglobin level, 88 g/l (normal
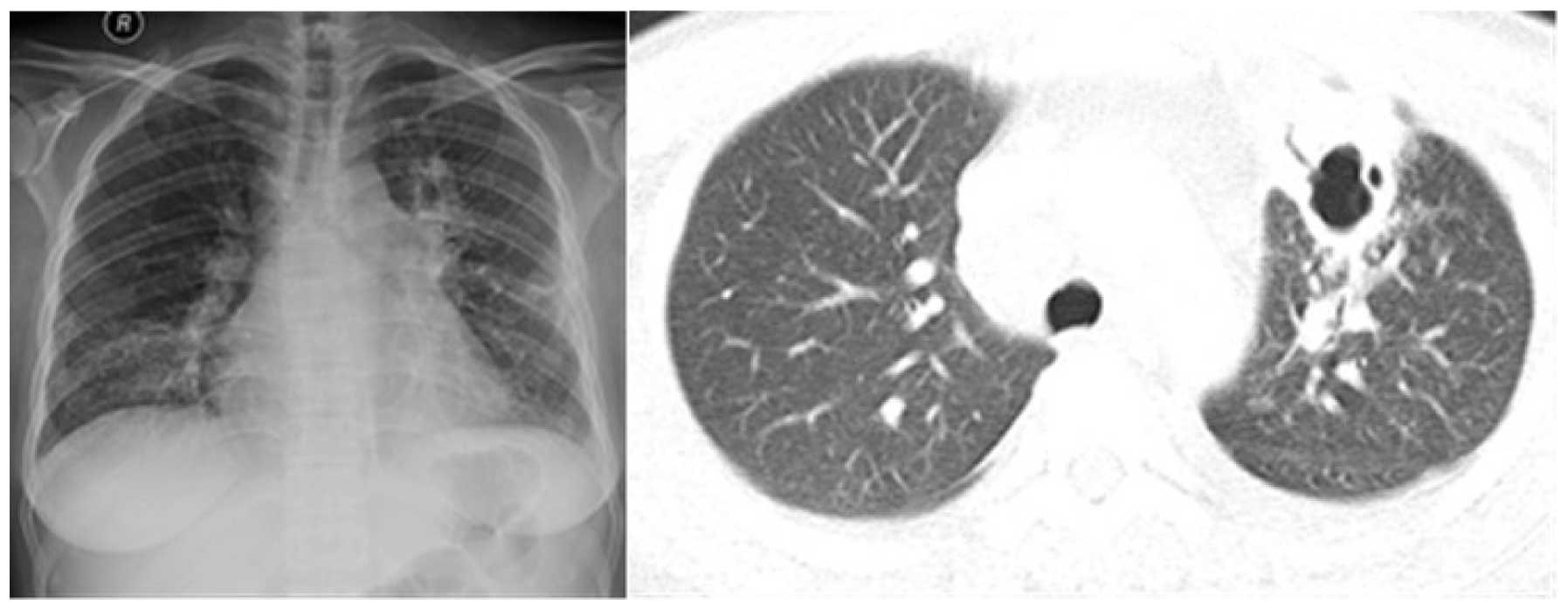
level, 130–175 g/l). Chest radiographs and chest computed
tomography revealed multiple patchy exudative shadows, thick-walled
hollow inner part of the visible lesions, bilateral pleural and
pericardial effusion in the lungs (Fig.
1).
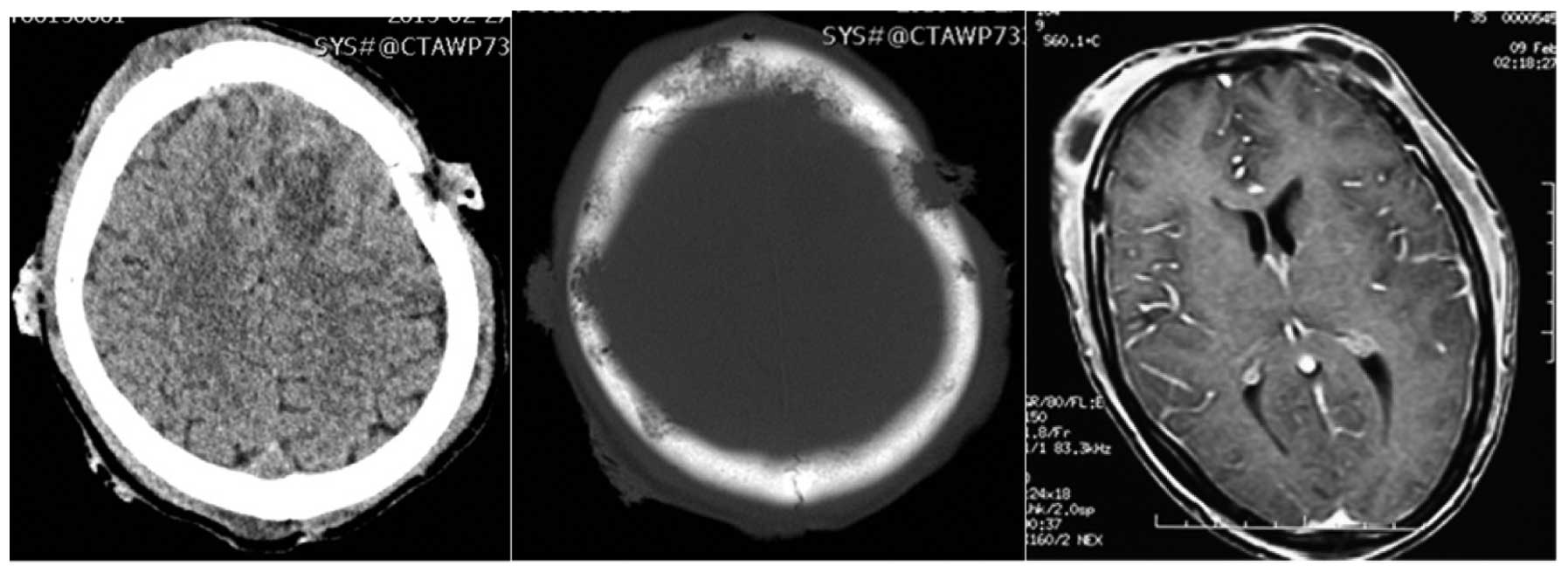
The CT and enhanced MR show multiple bone
destruction and masses in skull, with ring-enhanced abscesses in
scalp (Fig. 2), and bilateral neck,
bilateral upper arm, head and face have multiple visible purulent
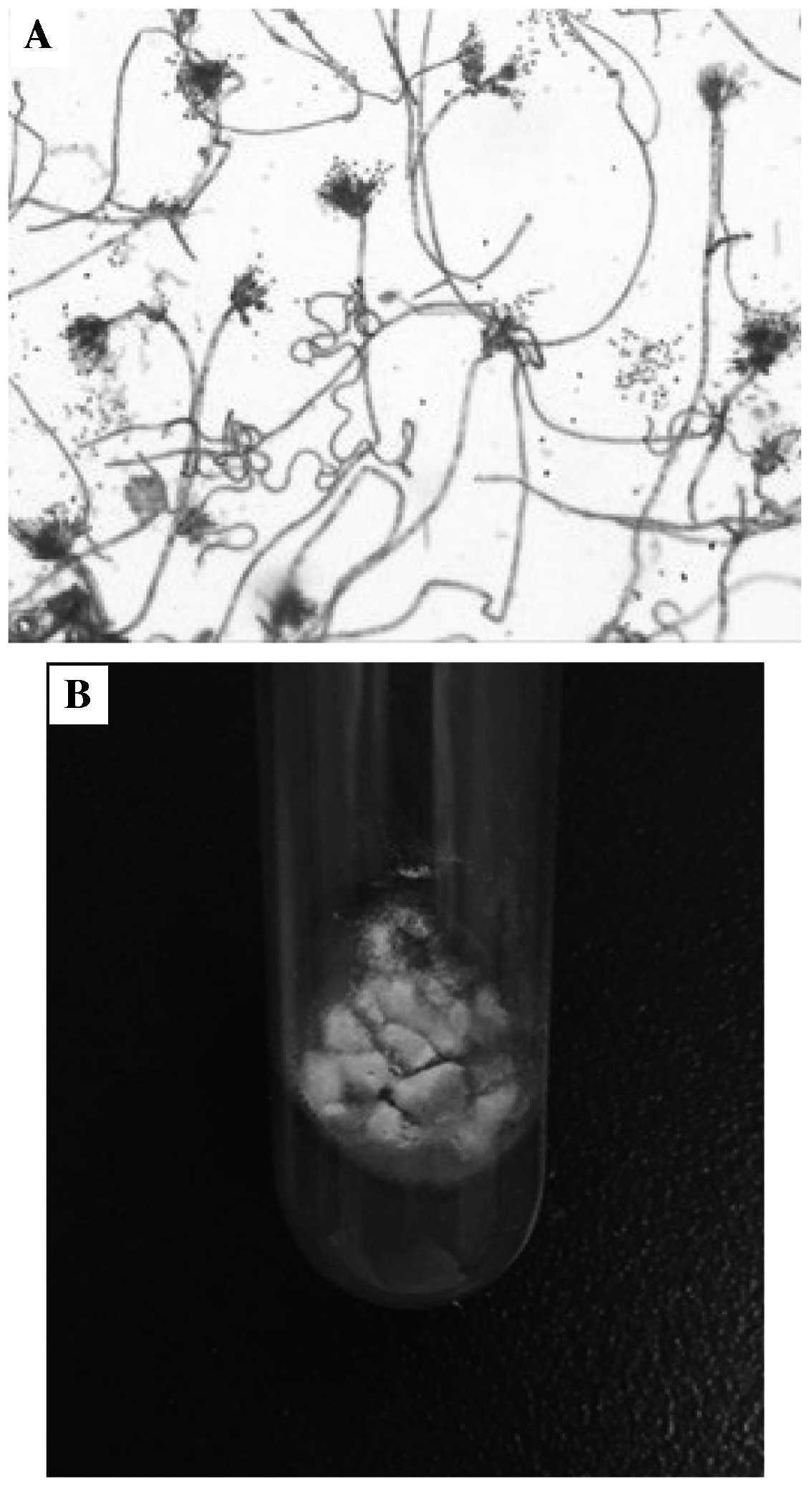
mass. A culture of blood and cyst fluid revealed P.
marneffei infection (Fig. 3).
The patient was administered 2 weeks of antifungal therapy, and the
patient's condition was markedly improved. The exudative lesions
significantly improved absorption and systemic multiple pustule
subsided. Patients and families must consider the costs of
treatment. It was recommended that the patient return to the local
hospital for follow-up treatment following discharge from The
Second Xiangya Hospital of Central South University on March 10th
2015. Following discharge, liposomal amphotericin B was used
(initial dose, 25 mg/day for 4 days, increasing to 150 mg/day for
12 days, then the total applications of amphotericin B liposome was
up to 2,000 mg). After three months of treatment, the abscesses of
the head, face and other body parts disappeared and the enlarged
lymph nodes disappeared. The sizes and number of lesions in the
chest and abdomen were significantly reduced. The symptoms of the
patient were significantly improved, so she decided to stop
antifungal treatment without medical advice. At 10 months after
stopping treatment, the abscesses in the head and neck, the left
breast, and right leg reappeared. After the anti-tuberculosis
treatment at the local hospital, the condition gradually
deteriorated, and pleural and pericardial effusion was observed.
The patient was re-admitted to The Second Xiangya Hospital of
Central South University again. A culture of the systemic lesion
abscess pus once again confirmed P. marneffei infection.
After a period of antifungal therapy with amphotericin B (daily 0.6
mg/kg) for 2 weeks of treatment, followed by oral itraconazole (400
mg/day) maintenance therapy, disappearance of the abscesses were
confirmed, body temperature returned to normal, and pleural and
pericardial effusion disappeared. To date, recurrent disease has
not been detected.
Discussion
The penicillium genus Marneffei is a
dimorphic fungus. P. marneffei does not cause serious human
health problems, but it can cause disease. This bacteria can be
found widespread in nature (5).
During the past few years, the incidence of penicilliosis infection
has markedly increased, paralleling the incidence of human
immunodeficiency virus infection. In China, the endemic of P.
marneffei infection in South China, particularly in Guangdong,
Guangxi, Yunnan and other regions (6). The source of infection is most likely
decaying vegetative material or soil from natural habitat. In
previous years, reports of immunocompromised patients infected with
P. marneffei has gradually increased.
P. marneffei can cause three chemical
reactions in tissues: Granulomatous reaction, purulent reaction and
non-reactive necrosis. It can affect the body's major organs, the
most common organs being the trachea, lung parenchyma,
hematopoietic and lymphoid system, skin, mucous membranes, bone and
soft tissue (7). As a result of a
lack of specific clinical manifestations, misdiagnosis often
occurs. P. marneffei diagnosis using tissue culture of bone
marrow and lymph node specimens have a high positive rate and the
highest reliability. Due to its histological culture lag, the
treatment of patients is often delayed. The patients presented with
fever, cough, multiple abscesses on the body surface and bone
destruction. Antifungal therapy provides a period of rapid relief
of clinical symptoms. However, this relief does not continue if the
patient does not present for follow-up review and they voluntarily
decide to stop taking the drug and return to factory jobs, as
demonstrated in the present study. In February 2016, the present
patient presented with abscesses of the head, neck and left breast.
A culture of blood and cyst fluid revealed infection with P.
marneffei once again. Treatment options were intravenous
amphotericin B (daily 0.6 mg/kg) for 2 weeks of treatment, followed
by oral itraconazole (400 mg/day) maintenance therapy. To date,
this patient with recurrent disease has not exhibited any
recurrence (8).
Disseminated P. marneffei infection is
relatively rare, with no reported cases ofrelapse until now. For
immunocompromised patients, a lack of strict antifungal treatment
and timely follow-up will result in repeated systemic multiple
abscess and bone destruction. The disease development is rapid and
often causes a high rate of mortality. If patients fail to maintain
strict antifungal treatment and timely follow-up, it easily causes
deterioration and even patient mortality. Therefore, Carlyle
marneyfe penicillium consolidation treatment is necessary (9).
In conclusion, when a patient presents with systemic
infection, P. marneffei infection must be considered,
particularly due to the increase in incidence of P.
marneffei in both immunocompromised and immunecompetent hosts.
Increased attention by the clinician and patient is essential to
manage the infection, and antifungal treatment is of great
importance. To prevent recurrence, long-term effective antifungal
therapy is notably important; therapy withdrawal requires strict
and systemic evaluation. Treatment follow-up after the review is
essential.
References
|
1
|
Saadiah S, Jeffrey AH and Mohamed AL:
Penicillium marneffei infection in a non aids patient: First case
report from Malaysia. Med J Malaysia. 54:264–266. 1999.PubMed/NCBI
|
|
2
|
Yousukh A, Jutavijittum P, Pisetpongsa P,
Chitapanarux T, Thongsawat S, Senba M and Toriyama K:
Clinicopathologic study of hepatic Penicillium marneffei in
Northern Thailand. Arch Pathol Lab Med. 128:191–194.
2004.PubMed/NCBI
|
|
3
|
Cao C, Liang L, Wang W, Luo H, Huang S,
Liu D, Xu J, Henk DA and Fisher MC: Common reservoirs for
Penicillium marneffei infection in humans and rodents, China. Emerg
Infect Dis. 17:209–214. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Skalski JH and Limper AH: Fungal, viral
and parasitic pneumonias associated with human immunodeficiency
virus. Semin Respir Crit Care Med. 37:257–266. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li X, Yang Y, Zhang X, Zhou X, Lu S, Ma L,
Lu C and Xi L: Isolation of Penicillium marneffei from soil and
wild rodents in Guangdong, SE China. Mycopathologia. 172:447–451.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hu Y, Zhang J, Li X, Yang Y, Zhang Y, Ma J
and Xi L: Penicillium marneffei infection: An emerging disease in
mainland China. Mycopathologia. 175:57–67. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Duong TA: Infection due to Penicillium
marneffei, an emerging pathogen: Review of 155 reported cases. Clin
Infect Dis. 23:125–130. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Patassi AA, Saka B, Landoh DE, Kotosso A,
Mawu K, Halatoko WA, Wateba MI, Adjoh K, Tidjani O, Salmon D and
Pitché P: First observation in a non-endemic country (Togo) of
Penicillium marneffei infection in a human immunodeficiency
virus-infected patient: A case report. BMC Res Notes. 6:5062013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kawila R, Chaiwarith R and Supparatpinyo
K: Clinical and laboratory characteristics of penicilliosis
marneffei among patients with and without HIV infection in Northern
Thailand: A retrospective study. Bmc Infect Dis. 13:4642013.
View Article : Google Scholar : PubMed/NCBI
|