Introduction
There are several types of nasopharyngeal
malignancies, including carcinomas and hematolymphoid, mesenchymal
and neurogenic tumours; carcinomas, including non-keratinizing and
keratinizing squamous cell types, are the most common type of
nasopharyngeal malignancy. Primary nasopharyngeal adenocarcinoma is
particularly rare, comprising <0.5% of the cases of malignant
nasopharyngeal neoplasms. These tumours are generally
heterogeneous, displaying various histological subtypes and diverse
biological behaviours, although they may be broadly classified into
two subtypes, namely the conventional/surface origin-type and the
salivary gland-type (1). The former
are usually low-grade malignancies with papillary configurations,
i.e., low-grade nasopharyngeal papillary adenocarcinomas (LGNPPAs),
which likely originate from the nasopharyngeal surface mucosa,
whereas the latter include tumours such as mucoepidermoid
adenocarcinomas, adenoid cystic carcinomas and polymorphous
low-grade adenocarcinomas (1,2). LGNPPA
was first described and characterized by Wenig et al in
1988, and since then the published case reports have been scarce
(2).
Thyroid-like LGNPPAs (TL-LGNPPAs) represent a small
minority of LGNPPAs and they are characterised by abnormal
expression of thyroid transcription factor-1 (TTF-1), mimicking
papillary thyroid carcinoma. TL-LGNPPA was first described by
Carrizo et al in 2005 (3)
and, to the best of our knowledge, only 12 cases have been reported
to date (3–12). We herein present a novel case of a
TL-LGNPPA in a 25-year-old woman, followed by a brief discussion on
this rare entity.
Case report
A 25-year-old Japanese woman with a 2-year history
of fever of unknown origin was referred to the Department of
Endocrinology, Metabolism and Nephrology, Kochi Medical School
(Nankoku, Japan). There were no remarkable physical findings and
the laboratory tests, including C-reactive protein levels, were
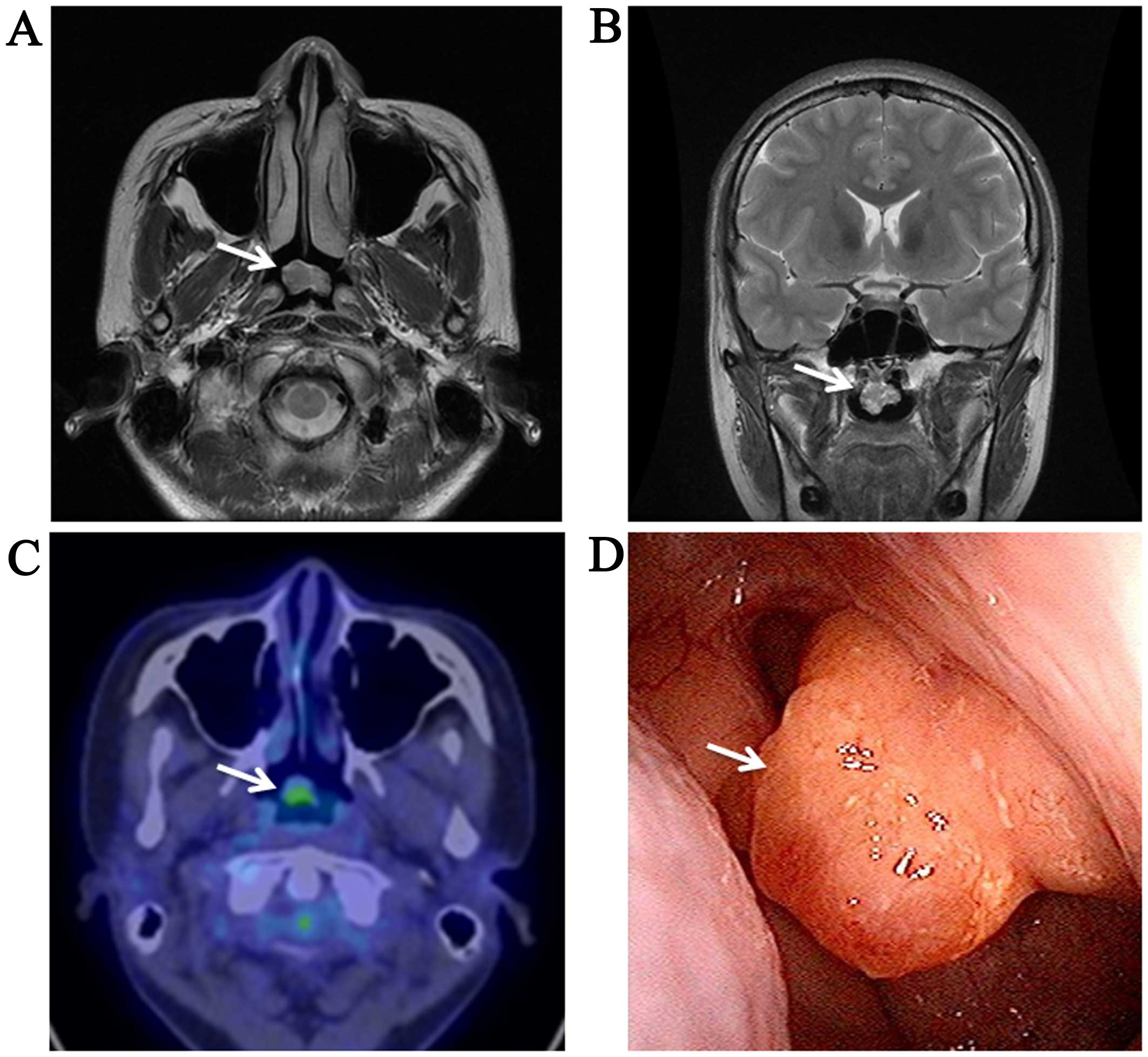
normal. Thorough diagnostic imaging (Fig. 1A-D), which included magnetic
resonance imaging, revealed a 1.7×1.2-cm tumour in the nasopharynx
(Fig. 1A and B). To further
characterise the tumour, 18Fludeoxyglucose-positron
emission tomography-computed tomography was performed, and the
tumour displayed abnormal uptake and accumulation of the tracer
(Fig. 1C). The cervical lymph nodes
and thyroid gland were checked by computed tomography and
ultrasonography, and no abnormalities were detected. Thyroid
function tests confirmed that the patient was euthyroid. Further
systemic radiological imaging studies confirmed that there were no
metastatic lesions. On laryngoscopy, the tumour was described as a
pedunculated mass arising from the roof of the nasopharynx
(Fig. 1D). Finally, the patient
underwent complete resection of the tumour.
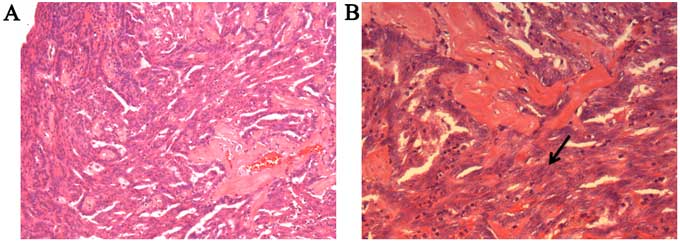
The histopathological examination confirmed negative
margins. Microscopically, the tumour exhibited a papillary
configuration with fibrovascular cores (Fig. 2A). Each papilla was covered with
cuboidal or columnar epithelial cells containing round to ovoid
nuclei. There were foci of tubular architecture, and a spindle cell
component was observed (Fig. 2B). On
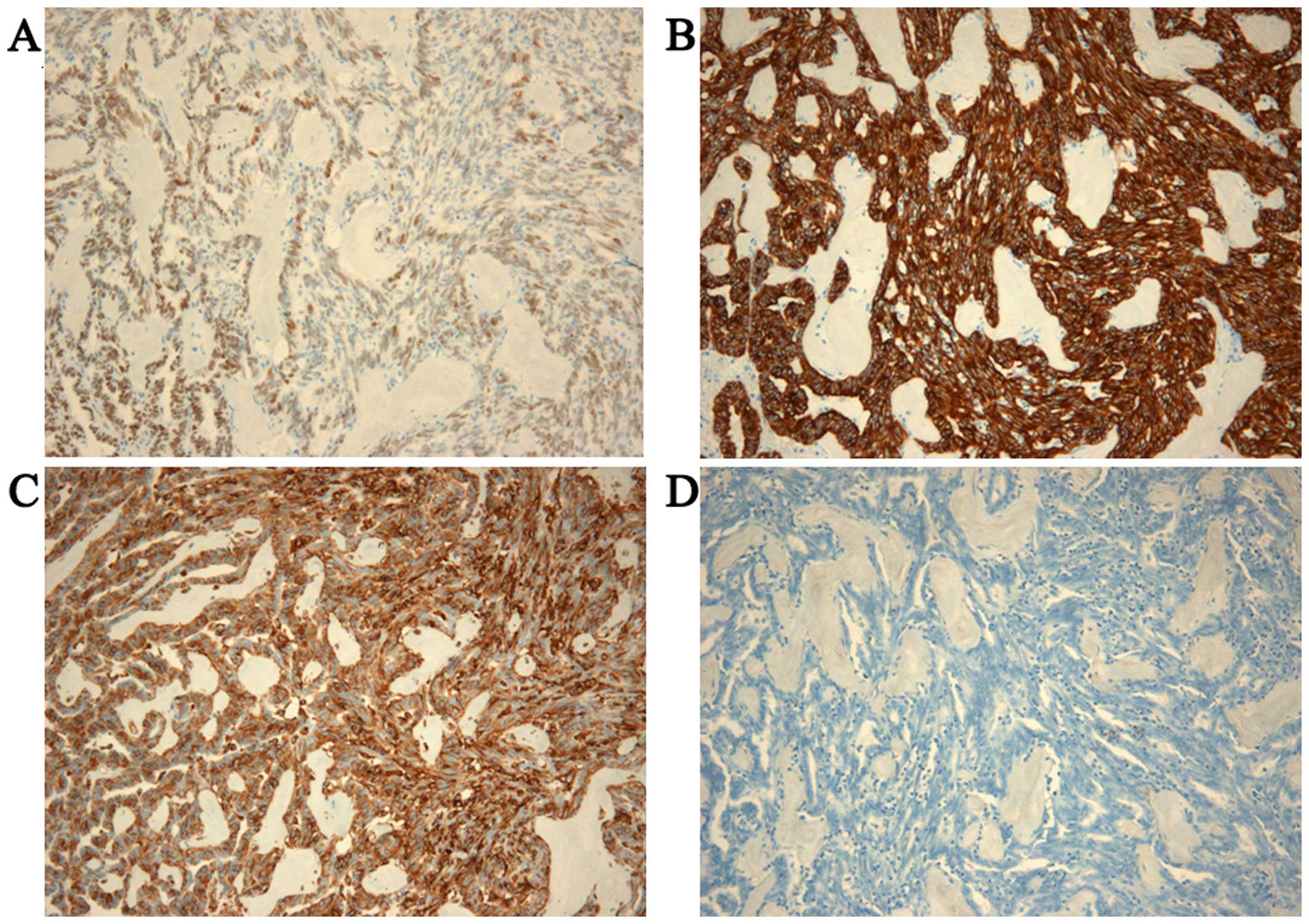
immunohistochemical examination, the tumour cells were diffusely
positive for TTF-1 (Fig. 3A),
whereas they were negative for other thyroid-related proteins,
including thyroglobulin (TG) (Fig.
3D). The neoplastic cells were also positive for cytokeratin
(CK)7 (Fig. 3B) and vimentin
(Fig. 3C), and negative for CK5/6,
CK20, smooth muscle actin, p63 and S-100. The Ki-67 labelling index
(MIB-1 index) reached 5% in the area of greatest concentration.
Based on the histological and immunohistochemical findings, the
diagnosis of TL-LGNPPA was established.
Two days after surgery, the patient's fever
disappeared and she exhibited no other symptoms, so she was
discharged from the hospital. Adjuvant therapy was not recommended,
and the patient has remained afebrile and free of local recurrence
and distant metastasis during the 3 years of postoperative
follow-up.
Discussion
TL-LGNPPA is an extremely rare neoplasm
characterized by morphological analogy to papillary thyroid
carcinoma and aberrant TTF-1 expression. Only 12 cases of TL-LGNPPA
have been reported to date (3–12). In a
review of the clinical characteristics of these tumours described
in the previously published cases, Oishi et al (11) reported that the age of the patients
ranged from 9 to 68 years (median, 34 years), with a male:female
ratio of 1:1. TL-LGNPPA predominantly occurs in the roof of the
nasopharynx and at the posterior edge of the nasal septum. The
prognosis is excellent, as all cases reported to date have been
cured by local excision, whereas local recurrence or metastasis
have not been reported in any of the cases. The most common
immunohistochemical characteristic of TL-LGNPPA is TTF-1
positivity, which has been noted in every reported case. TL-LGNPPA
and papillary thyroid carcinoma share certain immunohistochemical
characteristics, such as expression of CK7 and vimentin; however,
TL-LGNPPA is usually negative for TG, while papillary thyroid
carcinoma is diffusely positive for TG. This finding strongly
emphasizes the importance of immunostaining for TG in order to
differentiate TL-LGNPPA from papillary thyroid carcinoma. All the
findings in our case were compatible with the previously reported
clinical and pathological characteristics of TL-LGNPPA.
However, while the majority of the tumours that have
been previously reported were incidentally discovered or diagnosed
in patients with nasal symptoms including epistaxis and nasal
obstruction, our case was diagnosed during a comprehensive
evaluation of long-term fever of unknown origin. The central
nervous system provides thermoregulatory control of somatic
motoneurons, resulting in shivering, and of the sympathetic outflow
mediating cutaneous vasoconstriction, which is one of the primary
thermoeffector mechanisms conserving heat in the body core and
limiting heat loss to the environment; brown adipose tissue,
another effector of thermogenesis, acts through parallel, but
distinct, effector-specific, integrative/efferent circuits that
share common peripheral thermal sensory inputs (13). The hypothalamus is the coordinating
or central integration centre for thermoregulation, as it contains
the primary integrative and rostral efferent components of these
circuits (13,14). The neurons in the hypothalamus,
particularly in the preoptic area, are the primary site for the
organization and maintenance of febrile response to inflammation
and infection, which includes the stimulation of cutaneous
vasoconstriction, shivering and brown adipose tissue thermogenesis
mediated by prostaglandin E2 on prostaglandin EP3 receptors in the
preoptic area (15–18). Pyrogenic cytokines, tumour necrosis
factor α, interleukin (IL-1β and IL-6 induce cyclooxygenase 2 via
the activation pathways of nuclear factor-κB or signal transducer
and activator of transcription 3, leading to prostaglandin E2
synthesis (19). A previous report
documented that, in the lung, TTF-1 increased the expression of
IL-6, resulting in pulmonary inflammation (20). In our case, although we cannot
confirm that the fever was caused by the tumour, we hypothesize
that the overexpression of TTF-1 in the tumour may have induced
local expression of IL-6, which may have then stimulated the
hypothalamus, which was in close proximity to the tumour, thereby
leading to fever. As mentioned above, we suspect that TL-LGNPPA in
our patient may have been the cause of the fever of unknown origin.
However, this theory is poorly evidenced, and it would be
interesting to see whether future cases of TL-LGNPPA present in a
similar manner.
We herein present a case of TL-LGNPPA in a
25-year-old female patient, exhibiting all the previously reported
clinical, morphological and immunohistochemical characteristics of
this rare tumour, but presented only as a fever of unknown origin.
Our findings and our review of the literature suggest that
physicians should be aware of this novel entity and include it in
the differential diagnosis of fever of unknown origin.
Glossary
Abbreviations
Abbreviations:
|
TL-LGNPPA
|
thyroid-like low-grade nasopharyngeal
papillary adenocarcinoma
|
|
TTF-1
|
thyroid transcription factor-1
|
References
|
1
|
Barnes L, Eveson JW, Reichart P and
Sidransky D: World health organization classification of tumours:
Pathology and genetics of head and neck tumors. Lyon: IARC Press;
2005
|
|
2
|
Wenig BM, Hyams VJ and Heffner DK:
Nasopharyngeal papillary adenocarcinoma. A clinicopathologic study
of a low-grade carcinoma. Am J Surg Pathol. 12:946–953. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carrizo F and Luna MA: Thyroid
transcription factor-1 expression in thyroid-like nasopharyngeal
papillary adenocarcinoma: Report of 2 cases. Ann Diagn Pathol.
9:189–192. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bansal A, Pradeep KE and Gumparthy KP: An
unusual case of low-grade tubulopapillary adenocarcinoma of the
sinonasal tract. World J Surg Oncol. 6:542008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fu CH, Chang KP, Ueng SH, Wu CC and Hao
SP: Primary thyroid-like papillary adenocarcinoma of the
nasopharynx. Auris Nasus Larynx. 35:579–582. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ohe C, Sakaida N, Tadokoro C, Fukui H,
Asako M, Tomoda K, Tomoda K and Uemura Y: Thyroid-like low-grade
nasopharyngeal papillary adenocarcinoma: Report of two cases.
Pathol Int. 60:107–111. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ozer S, Kayahan B, Cabbarzade C, Bugdayci
M, Kosemehmetoglu K and Yucel OT: Thyroid-like papillary
adenocarcinoma of the nasopharynx with focal thyroglobulin
expression. Pathology. 45:622–624. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Petersson F, Pang B, Loke D, Hao L and Yan
B: Biphasic low-grade nasopharyngeal papillary adenocarcinoma with
a prominent spindle cell component: Report of a case localized to
the posterior nasal septum. Head Neck Pathol. 5:306–313. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sillings CN, Weathers DR and Delgaudio JM:
Thyroid-like papillary adenocarcinoma of the nasopharynx: A case
report in a 19-year-old male. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 110:e25–e28. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu PY, Huang CC, Chen HK and Chien CY:
Adult thyroid-like low-grade nasopharyngeal papillary
adenocarcinoma with thyroid transcription factor-1 expression.
Otolaryngol Head Neck Surg. 137:837–838. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oishi N, Kondo T, Nakazawa T, Mochizuki K,
Kasai K, Inoue T, Yamamoto T, Watanabe H, Hatsushika K, Masuyama K
and Katoh R: Thyroid-like low-grade nasopharyngeal papillary
adenocarcinoma: Case report and literature review. Pathol Res
Pract. 210:1142–1145. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang CH, Chang YL, Wang CP and Wu HP:
Positive immunostaining of thyroid transcription factor-1 in
primary nasopharyngeal papillary adenocarcinoma. J Formos Med
Assoc. 114:473–474. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morrison SF: Central control of body
temperature. F1000Res. 5(pii): F1000 Faculty Rev-880.
2016.PubMed/NCBI
|
|
14
|
Tansey EA and Johnson CD: Recent advances
in thermoregulation. Adv Physiol Educ. 39:139–148. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Scammell TE, Elmquist JK, Griffin JD and
Saper CB: Ventromedial preoptic prostaglandin E2 activates
fever-producing autonomic pathways. J Neurosci. 16:6246–6254.
1996.PubMed/NCBI
|
|
16
|
Nakamura K, Kaneko T, Yamashita Y,
Hasegawa H, Katoh H and Negishi M: Immunohistochemical localization
of prostaglandin EP3 receptor in the rat nervous system. J Comp
Neurol. 42:543–569. 2000. View Article : Google Scholar
|
|
17
|
Nakamura K, Matsumura K, Kaneko T,
Kobayashi S, Katoh H and Negishi M: The rostral raphe pallidus
nucleus mediates pyrogenic transmission from the preoptic area. J
Neurosci. 22:4600–4610. 2002.PubMed/NCBI
|
|
18
|
Lazarus M, Yoshida K, Coppari R, Bass CE,
Mochizuki T, Lowell BB and Saper CB: EP3 prostaglandin receptors in
the median preoptic nucleus are critical for fever responses. Nat
Neurosci. 10:1131–1133. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Inoue W, Somay G, Poole S and Luheshi GN:
Immune-to-brain signaling and central prostaglandin E2 synthesis in
fasted rats with altered lipopolysaccharide-induced fever. Am J
Physiol Regul Integr Comp Physiol. 295:R133–R143. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wert SE, Dey CR, Blair PA, Kimura S and
Whitsett JA: Increased expression of thyroid transcription factor-1
(TTF-1) in respiratory epithelial cells inhibits alveolarization
and causes pulmonary inflammation. Dev Biol. 242:75–87. 2002.
View Article : Google Scholar : PubMed/NCBI
|