Introduction
Diffuse large B cell lymphoma (DLBCL) is an
aggressive B-cell lymphoma, histologically characterized by diffuse
proliferation of large neoplastic B lymphoid cells with a nuclear
size equal to or exceeding normal histiocyte nuclei (1). DLBCL is the most common type of
lymphoma, accounting for 30–40% of adult non-Hodgkin lymphomas
(NHLs) worldwide, generally encountered in the 6th and 7th decades
of life (2). Prognostic factors in
DLBCL are age, performance score, stage, proliferation fraction and
gene expression profiles (3,4). DLBCLs are clinically and pathologically
diverse. Over the last decade, the standard of care for DLBCL
patients has been the addition of the anti-CD20 antibody rituximab
to classic cytotoxic chemotherapy. Generally, lymphoma is a
malignant neoplasm commonly occurring in the head and neck that may
occur in multiple locations with variable presentations.
Approximately 23–30% of patients with NHL present with extranodal
involvement of the head and neck, with involvement of the Waldeyer
ring in ~50% of the cases. Other sites of extranodal involvement
include the orbit, parotid gland, brain, nasopharynx, hypopharynx,
larynx, paranasal sinuses and uvula (5,6). We
herein report what is, to the best of our knowledge, the first case
of a patient with DLBCL involving the carotid space unilaterally.
As the disease manifested without previously reported signs or
symptoms, this may pose a diagnostic challenge for clinicians and
pathologists.
Case report
An 84-year-old man presented with a history of
repeated syncope and decreased heart rate and blood pressure over
the last month. There was no apparent cause for the syncope and the
decreased heart rate and blood pressure. The patient had been
emergently admitted to the local community hospital with paleness
and sweating nearly 1 month prior to admission. Following chest
compressions and intravenous injection of atropine and dopamine,
the symptoms were relieved. On physical examination, a mass sized
~3×3 cm was palpable in the left submandibular area. The mass was
hard, poorly mobile, without tenderness but with local skin
irritation. Following local application of cactus extract, the
redness and swelling subsided, the symptoms were relieved and the
patient was discharged. After ~1 month, the symptoms of syncope
with decreased heart rate and decreased blood pressure recurred and
on December 21, 2014, the patient was admitted to the Emergency
Department of The First Affiliated Hospital of Nanjing Medical
University (Nanjing, China). Following chest compressions and
intravenous administration of atropine and dopamine, the symptoms
improved. Physical examination revealed that the size of the left
submandibular mass had increased significantly in size to 5×4.5 cm.
The mass was hard, poorly mobile, without tenderness, with normal
color of the overlying skin. As the heart rate and blood pressure
were significantly decreased, it was hypothesized that the cause
may be compression of the left common carotid artery, aortic body
and carotid sinus by the mass. The use of use dopamine and
norepinephrine was continued to restore the blood pressure, and a
computed tomography angiography (CTA) examination of the head and
neck was performed. During the course of the examination, the
symptoms reappeared, but were relieved with active treatment. The
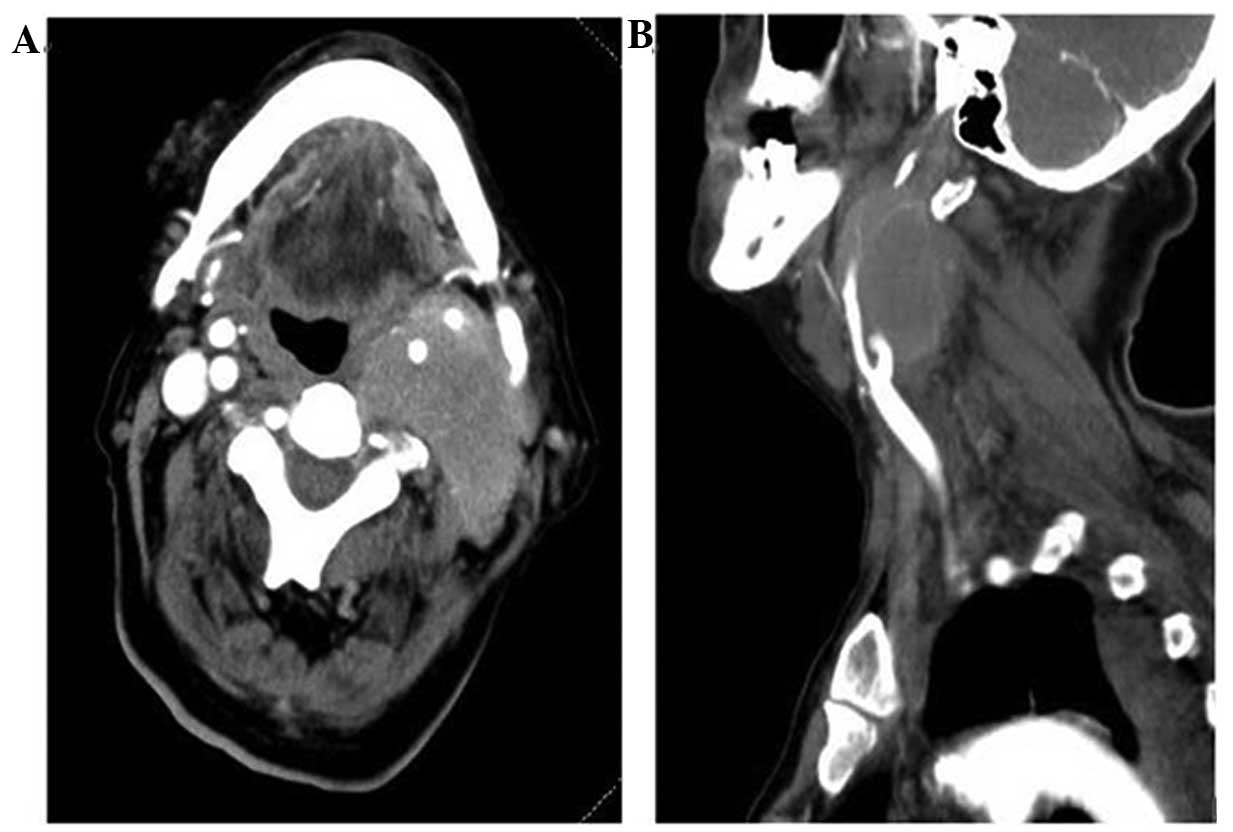
CTA examination results (Fig. 1)
revealed a soft tissue mass in the neck, at the level of the left
carotid bifurcation and above, possibly representing fused lymph
nodes. The left common carotid artery bifurcation and the internal
and external carotid artery segments were embedded in the mass and
there were multiple enlarged lymph nodes in the left neck.
Percutaneous biopsy of the left submandibular mass was immediately
performed. While waiting for the pathology results, the
abovementioned symptoms recurred several times. The pathological
and immunohistochemical results pointed towards the diagnosis of a
malignant tumor of the lymphatic and hematopoietic system: The
tumor cells were CD3−, CD20+++,
Pax-5+++, CD10−, B-cell lymphoma
(Bcl)-6−, multiple myeloma oncogene 1
(MUM1)+++ and Bcl-2+++, CD5−,
CD23+/−, pan-cytokeratin (CK-pan)−,
vimentin−, CD31− and CD34−; the
Ki-67 index was >80%; combined with hematoxylin and eosin
staining, the diagnosis of diffuse large B-cell lymphoma (DLBCL)
with a non-germinal center origin was confirmed. A treatment plan
was immediately designed, including systemic chemotherapy combined
with local radiotherapy to the left submandibular mass. After five
cycles of chemotherapy and seven sessions of radiotherapy, the
symptoms were significantly alleviated and the left submandibular
mass almost disappeared; thus, dopamine was withdrawn. A repeat
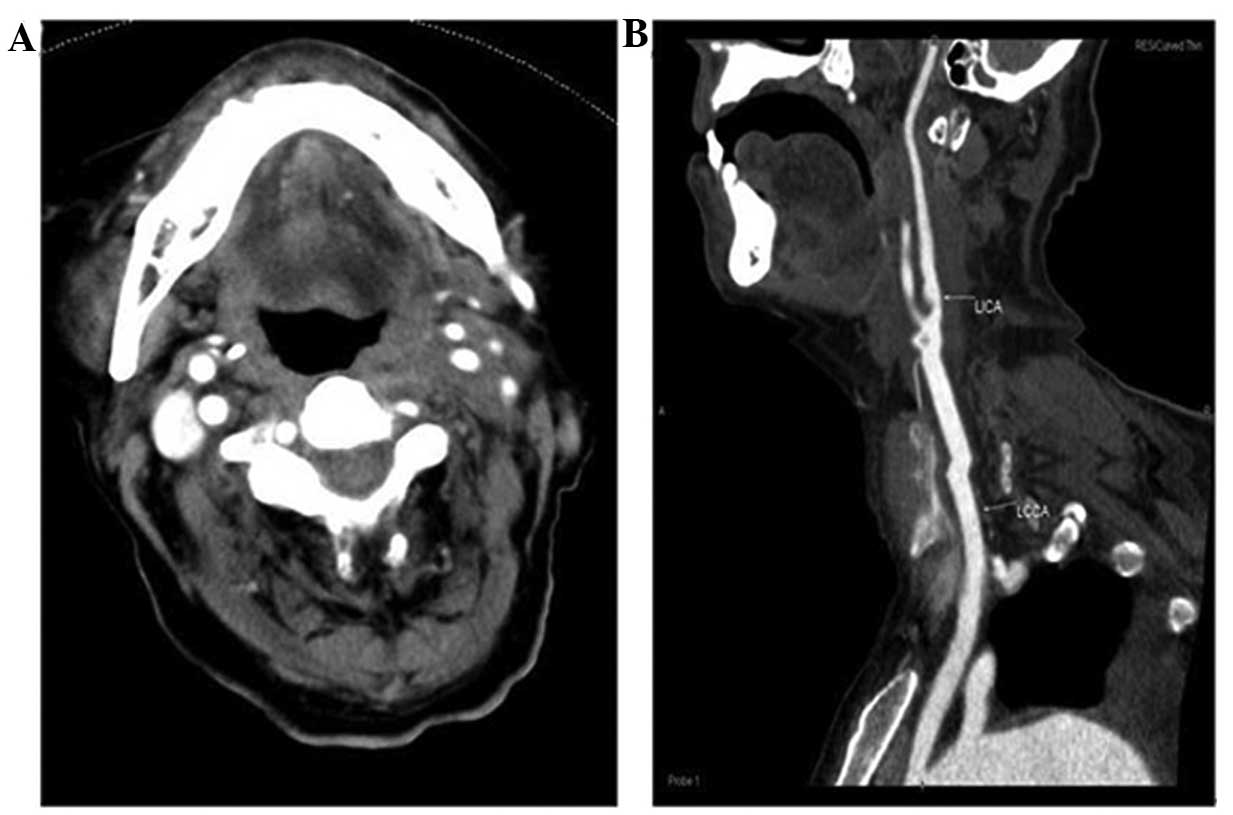
head and neck CTA examination was performed (Fig. 2), and it revealed that the soft
tissue mass at the level of left carotid artery bifurcation had
clearly decreased in size compared with the previous CTA scan.
Thereafter, the patient suddenly developed tenderness in the right
upper abdominal quadrant, and his body temperature and leukocyte
count (neutrophil fraction) increased significantly. An abdominal
ultrasound revealed choledocholithiasis and all the findings taken
together indicated choledocholithiasis accompanied by infection.
Therefore, chemotherapy and radiotherapy were discontinued.
Following antibiotic treatment with cefoperazone-sulbactam, biliary
drainage surgery and symptomatic supportive treatment for ~2
months, the patient's body temperature, leukocyte count and
differential neutrophil count returned to normal; however, the size
of left submandibular mass increased again. Local radiotherapy was
administered for a total of eight sessions, but the growth of the
mass could not be effectively inhibited. Due to the poor general
condition of the patient, treatment was discontinued.
Antitumor traditional Chinese Medicine preparations,
such as Kanglaite and Aidi injections, were used as palliative
treatment, supplemented by immunomodulating agents, such as
lentinan and thymosin. However, the mass progressively increased in
size, and pulmonary infections occurred repeatedly. The patient's
family requested treatment discontinuation and the patient was
discharged from the hospital. Shortly thereafter, the patient
succumbed to the disease.
Discussion
DLBCL is the most common malignant lymphoma subtype
in adults, accounting for ~40% of all cases (1). DLBCL is characterized by significant
heterogeneity and several morphologically diverse variants may be
distinguished. The distinction between these variants potentially
reflects differences in biology and may also be clinically relevant
(2). In addition to these
pathological differences, the clinical presentation may also vary.
Furthermore, there is heterogeneity regarding the molecular events
that drive DLBCL lymphomagenesis. This heterogeneity may be at
least partially be explained by the presence of molecularly defined
subtypes identified in large gene expression profiling studies over
the last several years (3–8). Through applying a classification
according to the cell of origin, in which the DLBCL tumor profiles
are compared to the profiles of normal B cells, several molecular
subtypes may be distinguished. The germinal center B-cell-like
(GCB) DLBCLs are derived from germinal center B cells and,
accordingly, express a variety of genes that are expressed in
normal germinal center B cells. By contrast, activated B-cell-like
(ABC) DLBCLs appear to originate from activated B cells that are
undergoing transition to plasma cells (3,6,9). Primary mediastinal B-cell lymphomas
appear to originate from a B-cell subpopulation in the thymus and
are characterized by a specific gene expression profile (4,5,10). Finally, ~15% of DLBCLs cannot be
assigned to a specific molecular subtype and are referred to as
unclassifiable DLBCL (11). In
particular, the distinction between ABC and GCB DLBCLs is not only
relevant from a scientific standpoint, but also has significant
clinical implications, as these subtypes are characterized by
differences in overall survival when treated with the current
standard treatment of rituximab and CHOP chemotherapy (R-CHOP). The
vast majority of patients diagnosed with GCB DLBCL respond
favorably to R-CHOP, whereas this regimen is less effective in ABC
DLBCL patients (11).
Lymphoma is a malignant neoplasm commonly occurring
in the head and neck that may occur in multiple locations with
variable presentations. Approximately 4–5% of patients with
Hodgkin's lymphoma present with extranodal involvement of the head
and neck compared with 23–30% in those with NHL. The Waldeyer ring
is the most common site of extranodal involvement in the head and
neck, accounting for ~50% of the cases. Other sites of extranodal
involvement include the orbit, parotid gland, brain, nasopharynx,
hypopharynx, larynx, paranasal sinuses and uvula (12,13). Our
patient presented with recurrent syncope accompanied by decreased
blood pressure and heart rate as the main symptoms; a head and neck
CTA examination indicated compression of the left carotid artery
and carotid sinus by the mass. The diagnosis of diffuse large
B-cell NHL was confirmed by percutaneous biopsy of the left
submandibular mass. Immunohistochemical staining was positive for
CD20, Pax-5, MUM1 and Bcl-2, and negative for CD3, CD5, CD10, CD31,
CD34, Bcl-6, CK-pan and vimentin. In contrast with lymphomas
presenting as nodal disease along the jugulodigastric chain, in
this case the lymphoma presented in the extranodal carotid space.
To the best of our knowledge, primary extranodal lymphomas of the
carotid space have not been previously described in the
literature.
The disease in this case was sensitive to
chemotherapy and radiotherapy, but due to the development of late
concurrent choledocholithiasis and infection, this treatment was
discontinued. Although radiotherapy was re-initiated following
antibiotic treatment and bile drainage, its efficacy was poor, and
the mass increased significantly in size. Therefore, the treatment
for DLBCL must have continuity as, following suspension, disease
control may not be feasible.
References
|
1
|
Sabattini E, Bacci F, Sagramoso C and
Pileri SA: WHO Classification of Tumours of Haematopoietic and
Lymphoid Tissues in 2008: An overview. Pathologica. 102:83–87.
2010.PubMed/NCBI
|
|
2
|
Bernd HW, Ziepert M, Thorns C, Klapper W,
Wacker HH, Hummel M, Stein H, Hansmann ML, Ott G, Rosenwald A, et
al: Loss of HLA-DR expression and immunoblastic morphology predict
adverse outcome in diffuse large B-cell lymphoma - analyses of
cases from two prospective randomized clinical trials.
Haematologica. 94:1569–1580. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Alizadeh AA, Eisen MB, Davis RE, Ma C,
Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, et al:
Distinct types of diffuse large B-cell lymphoma identified by gene
expression profiling. Nature. 403:503–511. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rosenwald A, Wright G, Leroy K, Yu X,
Gaulard P, Gascoyne RD, Chan WC, Zhao T, Haioun C, Greiner TC, et
al: Molecular diagnosis of primary mediastinal B cell lymphoma
identifies a clinically favorable subgroup of diffuse large B cell
lymphoma related to Hodgkin lymphoma. J Exp Med. 198:851–862. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Savage KJ, Monti S, Kutok JL, Cattoretti
G, Neuberg D, De Leval L, Kurtin P, Dal Cin P, Ladd C, Feuerhake F,
et al: The molecular signature of mediastinal large B-cell lymphoma
differs from that of other diffuse large B-cell lymphomas and
shares features with classical Hodgkin lymphoma. Blood.
102:3871–3879. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wright G, Tan B, Rosenwald A, Hurt EH,
Wiestner A and Staudt LM: A gene expression-based method to
diagnose clinically distinct subgroups of diffuse large B cell
lymphoma. Proc Natl Acad Sci USA. 100:9991–9996. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shipp MA, Ross KN, Tamayo P, Weng AP,
Kutok JL, Aguiar RC, Gaasenbeek M, Angelo M, Reich M, Pinkus GS, et
al: Diffuse large B-cell lymphoma outcome prediction by
gene-expression profiling and supervised machine learning. Nat Med.
8:68–74. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Monti S, Savage KJ, Kutok JL, Feuerhake F,
Kurtin P, Mihm M, Wu B, Pasqualucci L, Neuberg D, Aguiar RC, et al:
Molecular profiling of diffuse large B-cell lymphoma identifies
robust subtypes including one characterized by host inflammatory
response. Blood. 105:1851–1861. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rosenwald A, Wright G, Chan WC, Connors
JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland
EB, Giltnane JM, et al: The use of molecular profiling to predict
survival after chemotherapy for diffuse large-B-cell lymphoma. N
Engl J Med. 346:1937–1947. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Copie-Bergman C, Plonquet A, Alonso MA,
Boulland ML, Marquet J, Divine M, Möller P, Leroy K and Gaulard P:
MAL expression in lymphoid cells: Further evidence for MAL as a
distinct molecular marker of primary mediastinal large B-cell
lymphomas. Mod Pathol. 15:1172–1180. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lenz G, Wright G, Dave SS, Xiao W, Powell
J, Zhao H, Xu W, Tan B, Goldschmidt N, Iqbal J, et al: Stromal gene
signatures in large-B-cell lymphomas. N Engl J Med. 359:2313–2323.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aiken AH and Glastonbury C: Imaging
Hodgkin and non-Hodgkin lymphoma in the head and neck. Radiol Clin
North Am. 46:363–378, ix-x. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Artese L, Di Alberti L, Lombardo M,
Liberatore E and Piattelli A: Head and neck non-Hodgkin's
lymphomas. Eur J Cancer B Oral Oncol. 31B:299–300. 1995. View Article : Google Scholar : PubMed/NCBI
|