Introduction
Invasion of the hepatic vein, inferior vena cava
(IVC) and pulmonary artery is a conspicuous characteristic in the
majority of advanced cases of hepatocellular carcinoma (HCC). Once
pulmonary artery thrombosis occurs, most patients succumb to
respiratory failure. The major type of malignant tumor in
developing regions is HCC, particularly in China (1). The prognosis is very poor in the
advanced stages of the disease, possibly due to tumor vascular
invasion. HCC patients with pulmonary embolism and IVC invasion
have been reported to survive for ≤2 months without surgery
(2). We herein present the case of a
patient with HCC with a sizeable primary tumor, invasion of the IVC
and right atrium by tumor thrombi and massive bilateral pulmonary
embolism.
Case report
On April 18, 2015, a 55-year-old female patient
presented to the Eastern Hepatobiliary Surgery Hospital with a 6-h
history of sudden thoracodynia, dyspnea and transient coma. The
oxygen partial pressure was 49.9 mmHg, the carbon dioxide partial
pressure was 30.9 mmHg and the blood oxygen saturation was 86.4%
(pH 7.52). Routine abdominal ultrasound revealed a large
low-density mass in the right hepatic lobe. The patient had chronic
hepatitis B for 40 years; there was no history of diabetes,
coronary heart disease or hypertension.
Physical examination on admission revealed a body
temperature of 36.8°C, a heart rate of 100 beats/min, a blood
pressure of 103/67 mmHg, a respiratory rate of 20 breaths/min and
an Eastern Cooperative Oncology Group performance status of 2. The
patient had no ascites, edema, signs of hepatic failure or stigmata
of cirrhosis. The results of the laboratory tests were as follows:
Hemoglobin, 143 g/l (normal, 115–150 g/l); leukocyte count,
4.55×109/l (normal, 3.5–9.5×109/l); platelet
count, 243×109/l (normal, 125–350×109/l);
prothrombin time, 11.5 sec (normal, 11–13 sec); activated partial
thromboplastin time, 27.7 sec (normal, 24–37 sec); total bilirubin,
9.3 µmol/l (normal, 3.42–20.52 µmol/l); albumin, 39.2 g/l (normal,
40–55 g/l); aspartate aminotransferase, 63 U/l (normal, 13–35 U/l);
alanine aminotransferase, 45 U/l (normal, 7–40 U/l); γ-glutamyl
transpeptidase, 113 U/l (normal, 7–45 U/l); α-fetoprotein (AFP),
1,036 µg/l (normal, 0–20 µg/l); abnormal prothrombin, 3,168 mAU/ml
(normal, 0–40 mAU/ml); hepatitis B surface antigen positivity;
hepatitis B e antibody positivity; hepatitis B core antibody
positivity; and hepatitis B virus DNA levels of
7.08×106IU/ml (normal, <50 IU/ml). Blood gas analysis
revealed an oxygen partial pressure of 112 mmHg, a carbon dioxide
partial pressure of 36 mmHg and a blood oxygen saturation of 99%
(pH 7.44). The electrocardiogram (ECG) displayed a normal sinus
rhythm. Chest radiography and echocardiography showed no
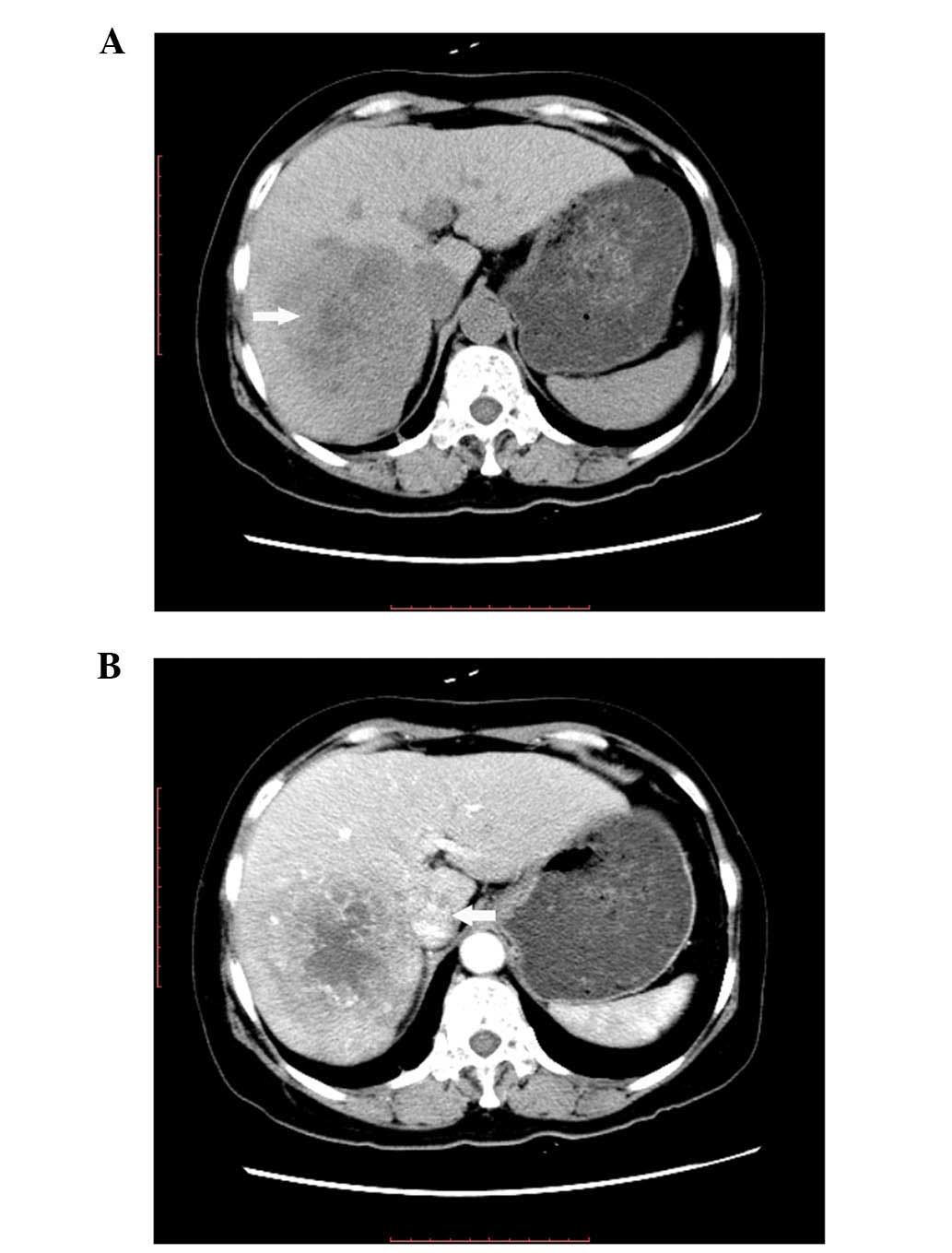
abnormalities; however, triple-phase abdominal computed tomography
(CT) revealed a sizeable lesion (7.1×6.2 cm) in the right hepatic
lobe (Fig. 1A), along with
thrombosis of the IVC (Fig. 1B). The
lesion exhibited typical arterial phase enhancement and
venous/delayed phase washout; based on these findings, the patient
was diagnosed with HCC.
Two days after admission, the patient developed
recurrent chest pain and shortness of breath, with a blood oxygen
saturation of 90% (normal, 95–99%). Urgent blood gas analysis
revealed an oxygen partial pressure of 78 mmHg (determined under
oxygen inhalation via nasal prongs at 3 l/min) and the D-dimer was
elevated to 7,210 µg/l (normal, 0–550 µg/l). The ECG revealed nodal
tachycardia and no abnormal wave shapes. The myocardium zymogram
examination and M-mode echocardiography results were normal; thus,
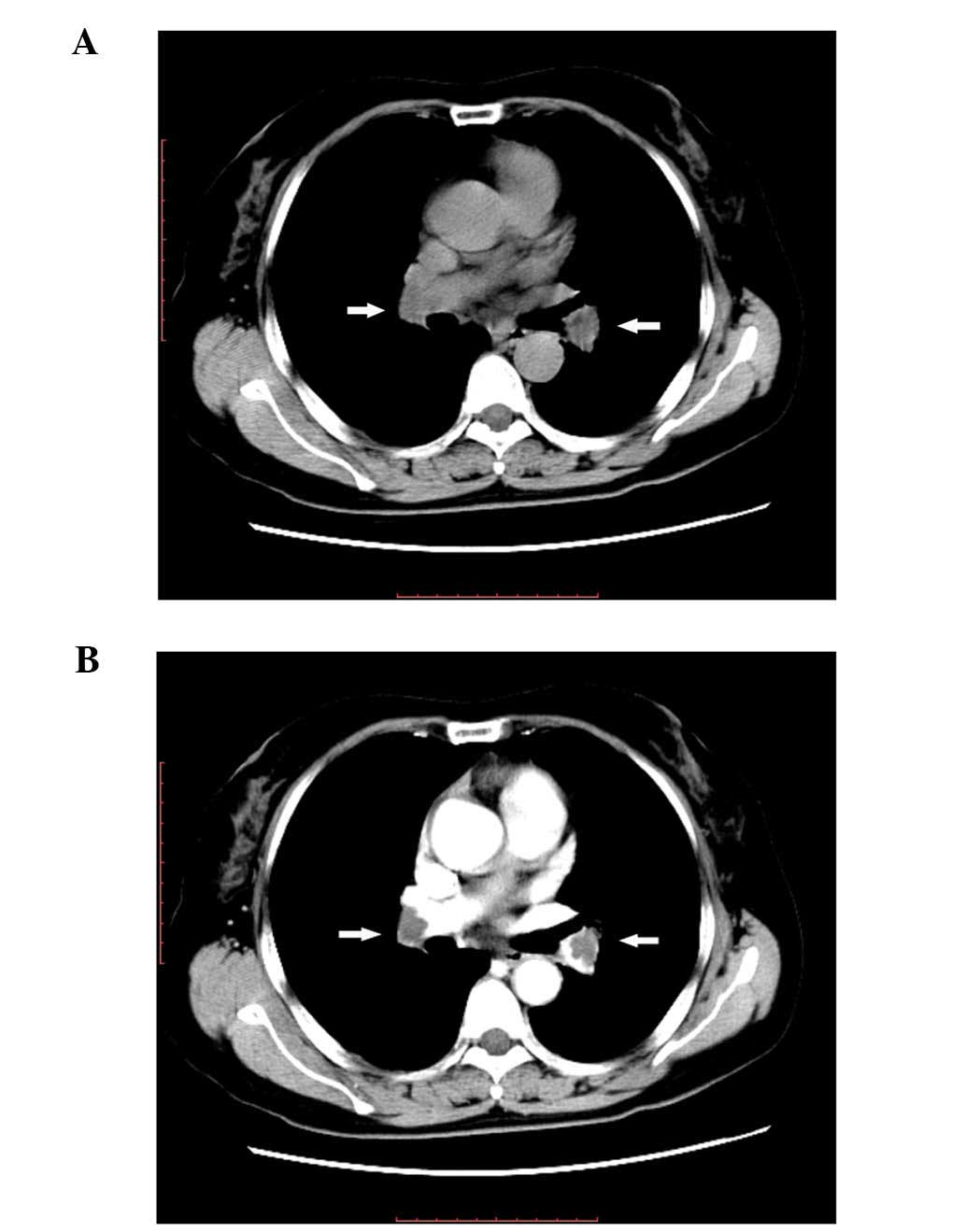
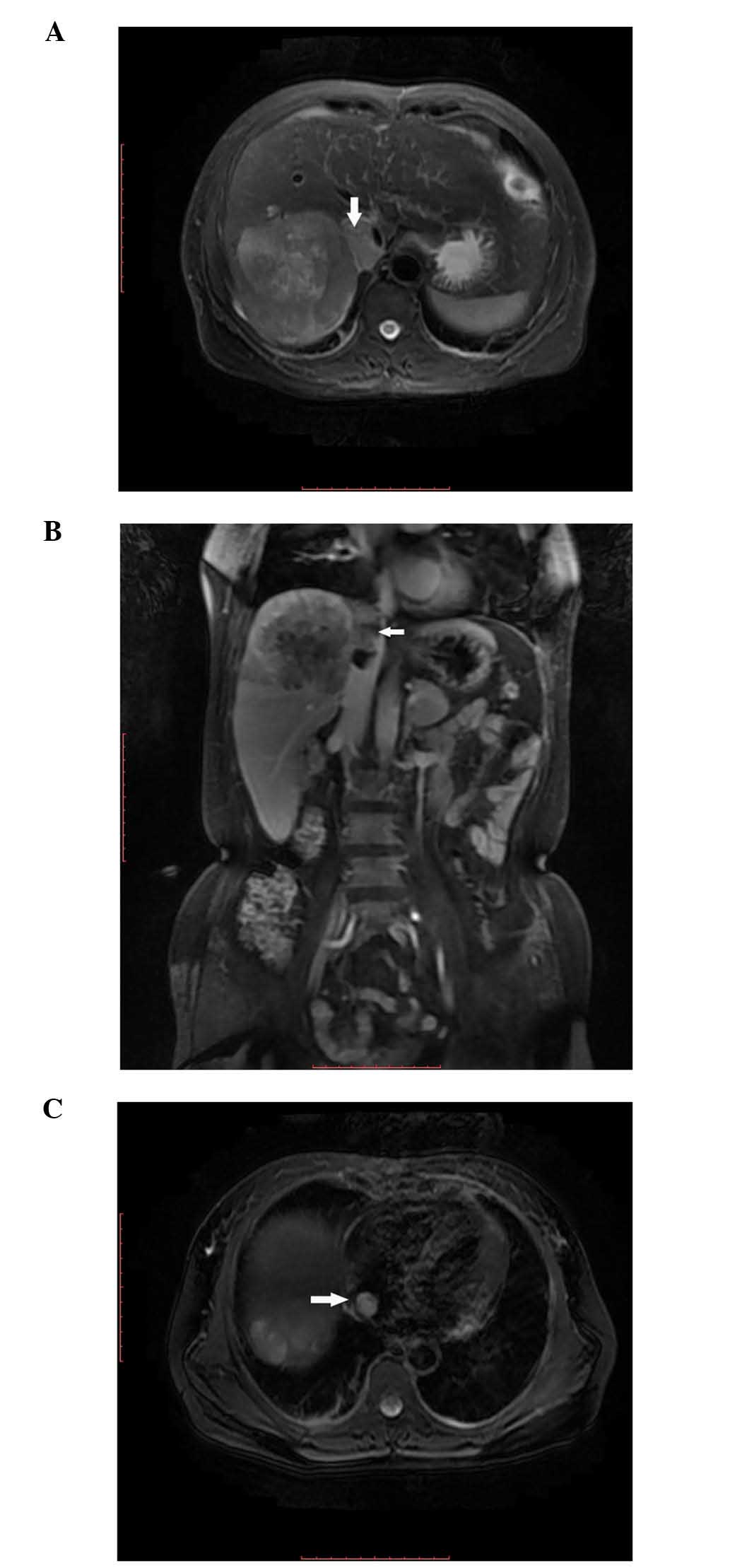
acute myocardial infarction was excluded. Urgent magnetic resonance
angiography (MRA) revealed that the IVC (Fig. 2A and B) and right atrium (Fig. 2C) were invaded by tumor thrombi.
Routine chest CT examination was normal (Fig. 3A) despite the patient's history of
chest pain and shortness of breath. Considering that hematogenous
metastasis is a characteristic feature of HCC, pulmonary artery
metastasis was suspected and an urgent contrast-enhanced CT scan
was performed, revealing nodular filling defects in the main
pulmonary arteries (Fig. 3B), and
the diagnosis of bilateral pulmonary emboli without lung metastasis
was considered.
Based on the aforementioned findings, the final
diagnosis was HCC with IVC and right atrial tumor thrombi, as well
as massive pulmonary embolism. The patient was administered
palliative treatment due to the advanced stage of the disease
according to the Barcelona Clinic Liver Cancer Classification
(3). To prevent further formation
and extension of blood thrombi, anticoagulant therapy with
low-molecular weight heparin calcium was administered (4,100 IU
q12h). The chest pain and shortness of breath resolved, a routine
blood test and coagulation function test revealed no abnormalities,
and the D-dimer level exhibited a decreasing trend. The patient was
in a stable condition following anticoagulant treatment for 3 days
and was discharged from the hospital. Anticoagulant therapy with
low-molecular weight heparin calcium was continued at another local
hospital, but he patient eventually succumbed to sudden pulmonary
thrombosis within 2 months after being discharged, as we were
informed by her family.
Discussion
Primary liver cancer is the fifth most commonly
diagnosed type of cancer and the second leading cause of
cancer-related mortality in men, whereas it is the ninth most
commonly diagnosed type of cancer and the second leading cause of
cancer-related mortality in women worldwide; HCC accounts for the
majority of primary liver cancers (4). The diagnosis of HCC is typically
determined by radiological liver imaging in combination with serum
AFP without the need for biopsy, as there is a consensus that
bioptic proof of HCC is not required in patients with chronic
hepatitis B infection or cirrhosis and non-invasive criteria may be
applied (5,6). Therefore, in our patient, the diagnosis
of HCC was established beased on the 40-year history of chronic
hepatitis B, the high levels of serum AFP and the radiological
findings, which were typical of HCC.
Advanced HCC generally metastasizes to the lungs,
bone, brain and adrenal glands. Vascular invasion and tumor
thrombosis formation are prominent characteristics in the majority
of cases of advanced HCC due to activation of hemostasis (7,8). The
incidence of vascular invasion increases with increasing tumor size
and it has been reported to be 82% in patients with serum AFP
levels >1,000 µg/l and a tumor diameter of >5 cm (9). The most frequent type of tumor
thrombosis in HCC patients is portal vein thrombosis (20–65%),
followed by systemic venous thromboembolism (6%) (8,10). The
incidence of hepatic vein thrombosis in HCC patients is 1.4–4.9%
(11). Tumor thrombosis from HCC
invading the hepatic vein occasionally spreads to the IVC and even
the right atrium, which has been reported in 0.67–3% of the cases
(7,12). In the present case, although the ECG
revealed no abnormalities, MRA revealed a mass extending from the
IVC into the right atrium. Based on the findings of a previous case
study, which demonstrated specific uptake of the contrast medium
gadolinium by tumor tissue and not the thrombus, helped confirm
that the masses in the IVC and right atrium were indeed tumor
thrombi (13). Intra-atrial growth
of HCC may not cause any symptoms per se, but may lead to
pulmonary thrombosis and pulmonary metastasis (14,15).
Primary thrombi in the right atrium are usually immobile and
attached to the atrial wall; however, secondary thrombi are mobile
and may temporarily lodge into the right atrium; thus, thrombi in
the right atrium may enter the pulmonary artery via the blood flow
(10). In the present case, it was
hypothesized that the masses in the pulmonary artery were tumor
thrombi originating from the right atrium, due to the diagnosis of
HCC, the sudden occurrence of the symptoms and the absence of edema
of the lower limbs, excluding the possibility of deep venous
thrombosis.
In the majority of the patients, the symptoms of
pulmonary embolism include dyspnea, chest pain, pre-syncope or
syncope, cough, fever and/or hemoptysis (16). Although these symptoms are
non-specific, once chest pain and shortness of breath appear in HCC
patients in the absence of underlying cardiopulmonary diseases,
pulmonary embolism should be highly suspected.
In the present case, the sudden onset of
thoracodynia, dyspnea and transient coma, a significant reduction
of partial oxygen pressure and a marked rise of D-dimer levels
should draw clinicians' attention to the possibility of HCC with
pulmonary tumor thrombosis. Although a chest X-ray revealed no
abnormalities, a contrast-enhanced chest CT clearly demonstrated
massive bilateral pulmonary artery thrombosis; however, a previous
routine CT without contrast enhancement could not distinguish
between tumor thrombosis and the surrounding tissues due to their
similar density. This illustrates the importance of the chest CT
examination with contrast enhancement, without which the diagnosis
of pulmonary embolism would have been missed, with a high risk of
tumor thrombi being dislodged during subsequent hepatectomy and
tumor thrombosis resection. Indeed, the patient succumbed to
pulmonary embolism within 2 months.
HCC patients with IVC invasion and right atrial
tumor thrombi usually have poor survival, owing to the difficulty
of early diagnosis (17). Resection
may be the only treatment available for tumor thrombi in patients
with HCC (17). According to a
previous study, the 1-year survival rate among HCC patients with
pulmonary embolism and IVC invasion who received surgery was 40%;
however, in the group without surgery, the median survival time was
only 3 days and none of the patients survived for >2 months
(2). In the present case, the
patient and her family refused surgery due to the high associated
risk, although they were informed that surgery may prolong the
patient's survival.
In conclusion, three points are important in the
present case: First, in patients with HCC and tumor thrombus of the
hepatic vein or IVC, symptoms of respiratory distress and chest
pain should raise the suspicion of pulmonary embolism. Second, a
significant increase in D-dimer levels has a laboratory diagnostic
value (18); in addition, routine
thoracic contrast-enhanced CT is necessary, as routine chest CT and
X-ray cannot illustrate extensive pulmonary embolism, resulting in
misdiagnosis with severe consequences. Finally, despite three
events of pulmonary embolism affecting large areas, the patient in
the present study still survived for ~2 months. This may be
attributed to the anticoagulation effect of the low-molecular
weight heparin calcium, which may prevent immediate further
formation and extension of blood thrombi, as well as promote the
collateral circulation around pulmonary arteries via peripheral
blood vessels. Palliative treatment may prolong patient survival,
although the prognosis for HCC patients with vascular invasion is
generally poor.
Acknowledgements
The authors are grateful for the support of the
Innovation Program of Shanghai Municipal Education Commission
(grant no. 12ZZ077).
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lin HH, Hsieh CB, Chu HC, Chang WK, Chao
YC and Hsieh TY: Acute pulmonary embolism as the first
manifestation of hepatocellular carcinoma complicated with tumor
thrombi in the inferior vena cava: Surgery or not. Dig Dis Sci.
52:1554–1557. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Llovet JM, Brú C and Bruix J: Prognosis of
hepatocellular carcinoma: The BCLC staging classification. Semin
Liver Dis. 19:329–338. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lau WY and Lai EC: Hepatocellular
carcinoma: Current management and recent advances. Hepatobiliary
Pancreat Dis Int. 7:237–257. 2008.PubMed/NCBI
|
|
6
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Masci G, Magagnoli M, Grimaldi A, Covini
G, Carnaghi C, Rimassa L and Santoro A: Metastasis of
hepatocellular carcinoma to the heart: A case report and review of
the literature. Tumori. 90:345–347. 2004.PubMed/NCBI
|
|
8
|
Connolly GC, Chen R, Hyrien O, Mantry P,
Bozorgzadeh A, Abt P and Khorana AA: Incidence, risk factors and
consequences of portal vein and systemic thromboses in
hepatocellular carcinoma. Thromb Res. 122:299–306. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sakata J, Shirai Y, Wakai T, Kaneko K,
Nagahashi M and Hatakeyama K: Preoperative predictors of vascular
invasion in hepatocellular carcinoma. Eur J Surg Oncol. 34:900–905.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Panduranga P, Al-Mukhaini M, Ratnam L and
Al-Harthy S: Mobile right atrial thrombus with pulmonary
thromboembolism in a patient with advanced hepatocellular carcinoma
and disseminated tumor thrombosis. Heart Views. 12:173–177. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang YF, Wei W, Guo ZX, Wang JH, Shi M
and Guo RP: Hepatic resection versus transcatheter arterial
chemoembolization for the treatment of hepatocellular carcinoma
with hepatic vein tumor thrombus. Jpn J Clin Oncol. 45:837–843.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Afonso DV, Laranjeira A, Galrinho A and
Fragata J: Metastatic hepatocellular carcinoma: Right atrial tumor
as primary clinical manifestation. Case report. Rev Port Cir
Cardiotorac Vasc. 15:79–81. 2008.(In Portuguese). PubMed/NCBI
|
|
13
|
Lazaros G, Samara C, Nikolakopoulou Z and
Tassopoulos N: Growth of hepatocellular carcinoma into the right
atrium. A case of antemortem diagnosis with magnetic resonance
imaging of the heart. Acta Cardiol. 58:563–565. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pellicelli AM, Barba J, Gomez AJ and
Borgia MC: Echocardiographic follow-up of right atrial tumoral
invasion by hepatocarcinoma: A case report. Cardiologia.
37:151–153. 1992.PubMed/NCBI
|
|
15
|
Martínez Baca-López F, Ramírez-Arias E,
Rayas-Gómez AL, Bernal-Ruiz EA and Saturno-Chiu G: Hepatocellular
carcinoma with invasion into right cardiac cavities: Report of a
case and literature review. J Am Soc Echocardiogr. 17:192–194.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Konstantinides SV, Torbicki A, Agnelli G,
Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M,
Kucher N, et al: 2014 ESC guidelines on the diagnosis and
management of acute pulmonary embolism. Eur Heart J. 35:3033–3069,
3069a-3069k. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fujisaki M, Kurihara E, Kikuchi K,
Nishikawa K and Uematsu Y: Hepatocellular carcinoma with tumor
thrombus extending into the right atrium: Report of a successful
resection with the use of cardiopulmonary bypass. Surgery.
109:214–219. 1991.PubMed/NCBI
|
|
18
|
Torbicki A, Perrier A, Konstantinides S,
Agnelli G, Galiè N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D,
Janssens U, et al: Guidelines on the diagnosis and management of
acute pulmonary embolism: The task force for the diagnosis and
management of acute pulmonary embolism of the European Society of
Cardiology (ESC). Eur Heart J. 29:2276–2315. 2008. View Article : Google Scholar : PubMed/NCBI
|