Introduction
Adenosquamous cell lung cancer (ASCLC) is a type of
non-small-cell lung cancer (NSCLC) and it is a morphologically
mixed tumor, composed of two cell components, namely adenocarcinoma
and squamous cell carcinoma in varying proportions, each
representing ≤10% of the whole tumor (1). Due to its rarity, ASCLC has not received
significant attention in terms of its clinical aspects, with only a
limited number of studies investigating the aggressive biological
characteristics of ASCLC (2–5).
Pemetrexed-containing chemotherapy is currently one
of the highly promising regimens for the treatment of advanced
NSCLC (6). In addition, the
effectiveness of pemetrexed-containing chemotherapy for NSCLCs with
specific genetic changes has been previously reported (7–9). We herein
report a case of recurrent epidermal growth factor receptor (EGFR)
mutation-positive ASCLC successfully treated with
pemetrexed-containing chemotherapy. Of note, this was a rechallenge
with pemetrexed following gefitinib therapy and postoperative
adjuvant pemetrexed-containing chemotherapy.
Case report
A 66-year-old woman with no history of smoking
presented to Mito Medical Center, University of Tsukuba (Tsukuba,
Japan) with a cough and intermittent hemoptysis over the past 8
weeks. Chest radiography and computed tomography (CT) revealed a
large cavitary mass in the lower lobe of the left lung.
Bronchoscopy revealed a tumor occluding the left lower bronchus,
with active bleeding. The patient was initially diagnosed with
adenocarcinoma on the basis of the histopathological examination of
transbrochial biopsy specimens. Distant metastasis was not
detected. The Eastern Cooperative Oncology Group performance status
score was 1. To prevent the deterioration of her respiratory
condition due to hemoptysis, the patient underwent a lobectomy of
the left lower lung and mediastinal lymph node dissection. The
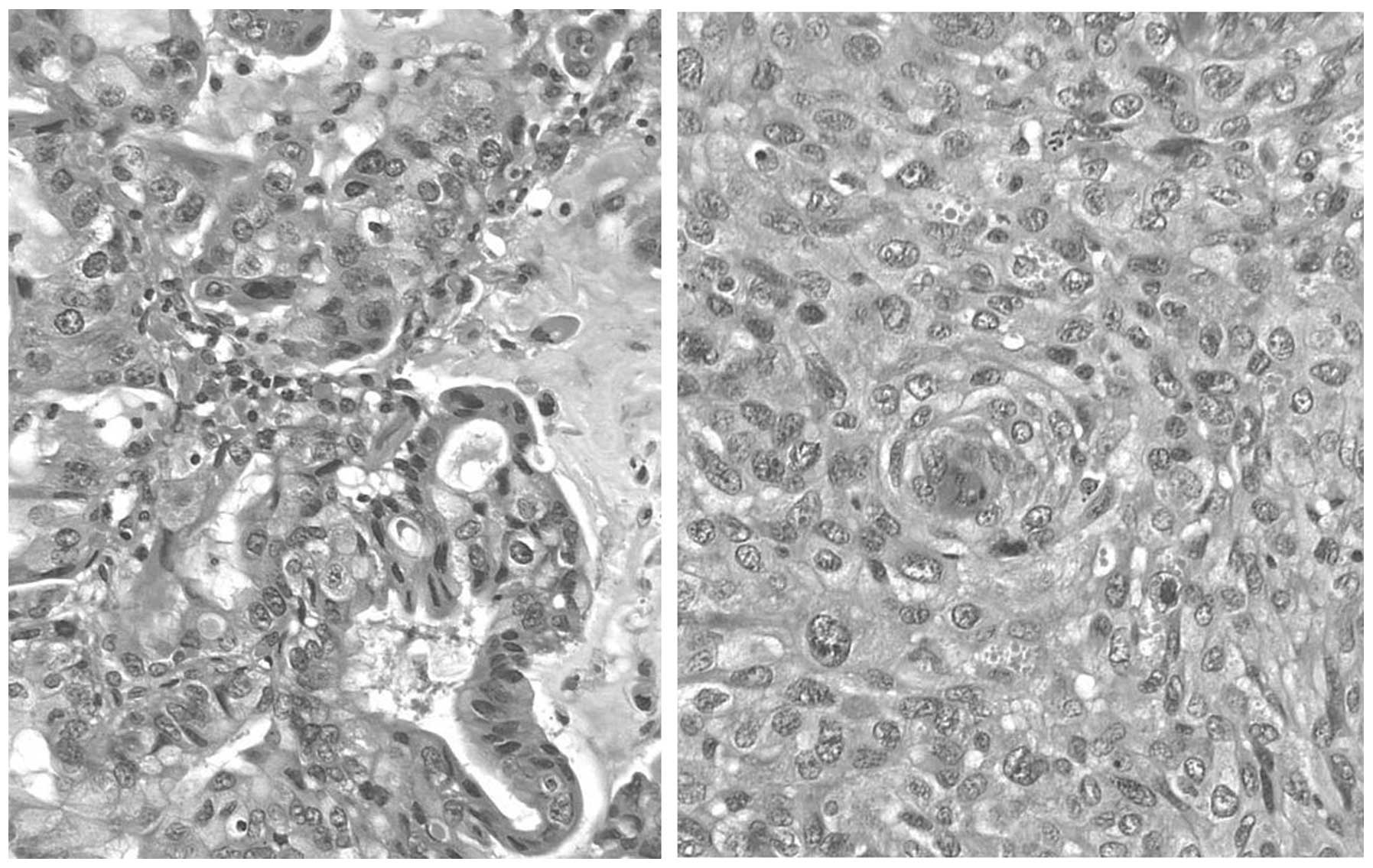
resected tumor consisted of adenocarcinomatous as well as squamous
cell carcinomatous components, with each comprising ≤10% of the
tumor. The final pathological diagnosis was ASCLC (Fig. 1) and the tumor was staged as
pT3bN1M1a. The adenocarcinomatous and squamous cell carcinomatous
components of the surgically resected tumor were precisely
separated by manual microdissection under microscopic observation
to avoid contamination of each sample by different components. An
EGFR exon 19 deletion was identified in both components. Soon after
the surgical resection, the patient received 4 courses of
chemotherapy with carboplatin and pemetrexed. Six months after the
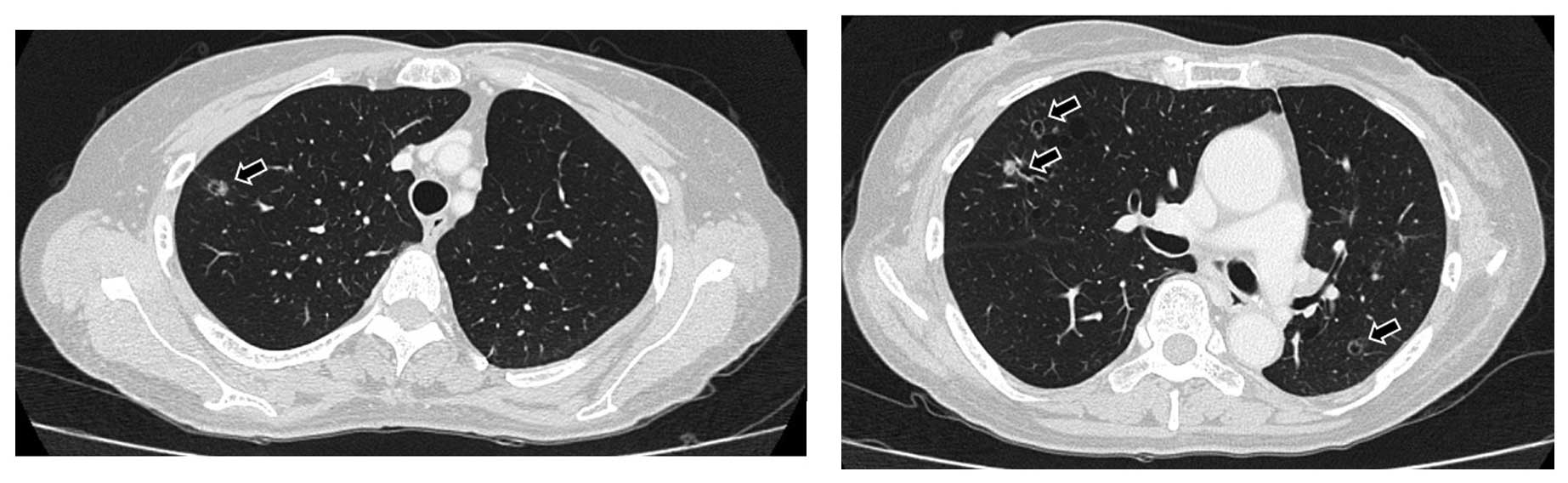
chemotherapy, the patient developed small cavitary metastases sized
≤10 mm in both lungs. Therefore, treatment with 250 mg of gefitinib
therapy once daily was initiated. A chest CT scan revealed
regression of the metastatic cavitary tumors bilaterally, which was
evaluated as partial response (PR). The patient developed a grade 2
skin rash, according to the 2013 National Cancer Institute Toxicity
Criteria (http://ctep.cancer.gov). One year after
the initiation of gefitinib therapy, small cavitary metastases
sized ≤10 mm were again detected in both lungs (Fig. 2). The patient strongly wished to
receive pemetrexed-containing chemotherapy again, due to its mild
adverse event profile. Considering the metastases being confined to
the lungs and her good general condition, the patient received
chemotherapy with carboplatin, pemetrexed and bevacizumab. After
receiving 2 cycles of the chemotherapy, she achieved a PR (Fig. 3) and received an additional 2 cycles
of the regimen. Subsequently, 15 cycles of maintenance therapy with
pemetrexed and bevacizumab were administered. There was no severe
hematological or non-hematological toxicity. Treatment with
bavacizumab-containing chemotherapy has been continued at the
outpatient clinic, without any signs of tumor progression 19 months
after the initiation of pemetrexed-containing chemotherapy.
Discussion
Due to rarity of ASCLC, its clinical and prognostic
aspects have not been extensively investigated. The majority of
available studies report an aggressive biological behavior of ASCLC
(2–5).
In ASCLC, EGFR mutations appear to be important predictive markers
for the response to EGFR-tyrosine kinase inhibitors (TKIs), similar
to the observed favorable outcome in other cell types of NSCLC
(10). However, the frequency of EGFR
abnormalities and the effectiveness of TKIs in EGFR-mutated ASCLC
have not yet been completely evaluated. In patients with resectable
ASCLC, postoperative platinum-based chemotherapy has significantly
improved patient survival and reduced the risk of developing
distant metastases (2). Similar to
other cell types of NSCLC, it is now widely accepted that
postoperative platinum-based chemotherapy is the standard medical
treatment in stage IB-IIIA ASCLC (2).
However, EGFR-mutated ASCLCs have not been extensively investigated
in terms of the effectiveness of chemotherapy with cytotoxic drugs;
moreover, whether EGFR-positive ASCLCs have a more favorable
outcome with such treatment compared with their EGFR-negative
counterparts, remains unknown.
It was recently indicated that pemetrexed-containing
chemotherapy exhibits superior efficacy for NSCLCs with specific
genetic changes (7–9). Although this is only a case report of an
ASCLC patient with EGFR mutation, the outcome in our patient was
consistent with the results of other cell types of NSCLC (10).
Of note, response to pemetrexed-containing
chemotherapy following acquired resistance to EGFR-TKIs in a
patient with advanced NSCLC was recently reported (11): That case was a metastatic
adenocarcinoma of the lung with exon 21 L858R mutation. The patient
was treated with pemetrexed and cisplatin and achieved a PR. After
recurrence, the patient received erlotinib for 6 months. Due to
regrowth in the pleura, the patient underwent pemetrexed
rechallenge, considering the slow progression, good tolerance and
good efficacy of the drug. Due to the satisfactory response, the
authors reported that rechallenge with pemetrexed-containing
chemotherapy should be one of the treatment choices for a
proportion of patients with acquired resistance to TKIs, one of
whom had shown response to previous chemotherapy (11). However, our patient had received
postoperative chemotherapy with platinum and pemetrexed. Six months
after the adjuvant chemotherapy, the patient received gefitinib due
to multiple pulmonary metastases bilaterally, which were well
controlled for 10 months. Pemetrexed rechallenge was selected in
our case, as the patient strongly wished to receive
pemetrexed-containing chemotherapy again, as she had experienced no
severe adverse events with this chemotherapy. Therefore, the
patient received chemotherapy with pemetrexed and bevacizumab for
re-recurrence following gefitinib therapy. The mechanisms
underlying the effectiveness of pemetrexed rechallenge have not
been fully elucidated, but the fact that the patient achieved a
good response may be of value and must be reported. Our results
suggest that, in adition to TKIs, pemetrexed-containing
chemotherapy may be one of the key regimens for the treatment of
EGFR mutation-positive ASCLC patients.
References
|
1
|
Travis WD, Brambilla E, Muller-Hermelink
HK and Harris CC: Pathology and genetics, Tumours of the lung,
pleura, thymus and heart. World Health Organization Classification
of Tumours (Lyon). IARC Press. 2004.
|
|
2
|
Filosso PL, Ruffini E, Asioli S, Giobbe R,
Macri L, Bruna MC, Sandri A and Oliaro A: Adenosquamous lung
carcinomas: A histologic subtype with poor prognosis. Lung Cancer.
74:25–29. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shimizu J, Oda M, Hayashi Y, Nomomura A
and Watanabe Y: A clinicopathologic study of resected cases of a
denosquamous carcinoma of the lung. Chest. 109:989–994. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Riquet M, Perrotin C, Lang-Lazdunski L,
Hubsch JP, Dujon A, Manac'h D, Le Pimpec Barthes F and Briere J: Do
patients with adenosquamous carcinoma of the lung need a more
aggressive approach? J Thorac Cardiovasc Surg. 122:618–619. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gawrychowski J, Bruliński K, Malinowski E
and Papla B: Prognosis and survival after radical resection of
primary adenosquamous lung carcinoma. Eur J Cardiothorac Surg.
27:686–692. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Paz-Ares LG, de Marinis F, Dediu M, Thomas
M, Pujol JL, Bidoli P, Molinier O, Sahoo TP, Laack E, Reck M, et
al: PARAMOUNT: Final overall survival results of the phase III
study of maintenance pemetrexed versus placebo immediately after
induction treatment with pemetrexed plus cisplatin for advanced
nonsquamous non-small-cell lung cancer. J Clin Oncol. 31:2895–2902.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park JH, Lee SH, Keam B, Kim TM, Kim DW,
Yang SC, Kim YW and Heo DS: EGFR mutations as a predictive marker
of cytotoxic chemotherapy. Lung Cancer. 77:433–437. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee SH, Noh KB, Lee JS, Lee EJ, Min KH,
Hur GY, Lee SH, Lee SY, Kim JH, Lee SY, et al: Thymidylate synthase
and ERCC1 as predictive markers in patients with pulmonary
adenocarcinoma treated with pemetrexed and cisplatin. Lung Cancer.
81:102–108. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sánchez Hernández A, José Juan O, Martínez
Vidal J, Blanco R, Maciá S, Galiana Esquerdo G, Aparisi Aparisi F,
Noguera Garde J, Catot S, Gaspá Losa F and García-Piñon F:
Quantification of circulating endothelial cells as a predictor of
response to chemotherapy with platinum and pemetrexed in patients
with advanced non-squamous non-small cell lung carcinoma. Clin
Transl Oncol. 17:281–288. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gazdar AF: Activating and resistance
mutations of EGFR in non-small-cell lung cancer: Role in clinical
response to EGFR tyrosine kinase inhibitors. Oncogene. 28(Suppl 1):
S24–S31. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li S, Zhou F, Ren S and Zhou C: Response
to pemetrexed rechallenge after acquired resistance of EGFR-TKI in
a patient with advanced NSCLC. Lung Cancer. 84:203–205. 2014.
View Article : Google Scholar : PubMed/NCBI
|