Introduction
Oral cancer is one of the most common cancers in the
world and causes a considerable problem to global public health due
to high mortality rates and disfigurement (1,2).
Approximately 90% of malignant oral neoplasms are oral squamous
cell carcinomas (OSCC), followed by adenocarcinoma and, rarely,
other types (3). Despite advances in
treatment for OSCC, the 5-year survival rate remains poor (4–6).
Therefore, investigating the risk factors and developing the early
diagnosis for treatment and prevention of OSCC are urgently
required.
Epidemiological studies have shown that OSCC is
associated with high tobacco use and alcohol consumption (7–9). However,
not all individuals with tobacco and alcohol habits develop these
fatal diseases, suggesting that individual genetic factors may also
be involved in disease etiology. The research results of the human
genome project have demonstrated that 99.9% of the genomes are the
same between individuals, with little difference in single
nucleotide polymorphisms (SNPs). Therefore, interindividual
differences in expression of SNPs may contribute to the variability
in the risk towards various types of malignancies, including OSCC.
Currently, the published evidence shows that there were significant
associations of gene polymorphisms with the susceptibility of
numerous cancers, such as GST and CYP1A1 gene
polymorphisms with squamous cell carcinoma of the lungs and head
and neck cancer, and the 8q24 rsl3281615 polymorphism with the risk
of breast cancer (10–15). However, the associations of OSCC with
CYP1A1 MspI genetic variants are inconsistent (16–25).
Cytochrome P4501A1 (CYP1A1) is a member of the CYP
family that participates in the metabolism of xenobiotics and
endogenous compounds, encoding for the aryl hydrocarbon hydrolase,
which is involved in the activation of polycyclic aromatic
hydrocarbon (PAHs) and aromatic amines, and is expressed in oral
tissue (26). CYP1A1 is able to
activate carcinogenic PAHs and its expression and function are
affected by gene polymorphisms, with more attention focused on the
association of cancer and CYP1A1. According to the previous
studies, the CYP1A1 gene has several SNPs that may alter the
activities of their enzymes and increase carcinogen activation and
yield to carcinogenicity. The first allele variants of the
CYP1A1 gene (CYP1A1*2A or CYP1A1 MspI) are the
most common polymorphisms, which are a transition from T to C in
the 3′ non-coding region resulting in the introduction of an MspI
restriction site and association with an increase in enzyme
activity, thus affecting the risks of carcinoma (27,28). The
MspI restriction site polymorphism results in three genotypes;
wild-type (TT), heterozygous variant (TC) and homozygous variant
(CC) (29).
Considering the significance of the CYP1A1
MspI polymorphism in the occurrence and development of
malignancies, including OSCC, the role of the CYP1A1 MspI
polymorphism in OSCC patients was systematically evaluated through
a meta-analysis.
Materials and methods
Search strategy
Pubmed, Web of Science, China National Knowledge
Infrastructure (CNKI) and WANFANG databases were searched without
language limitations, and the last search was updated on May 3,
2014. The CNKI and WANFANG databases provided studies in Chinese
and English. The search process was designed to primarily identify
all the relevant studies and the search strategies are as follows:
(CytochromeP450 1A1 or P4501A1 or CYP1A1 or CYP1A1*2A
or MspI or T3801C), (genotype or polymorphism or allele or variant)
and (oral squamous cell carcinoma or OSCC or mouth neoplasm or oral
cancer or oral carcinoma or oral tumor). The results were screened
by two investigators according to the title, key words, abstract
and type of study, and irrelevant studies were removed. A manual
review of the references cited in the selected studies was
undertaken to retrieve studies that may have been missed in the
search. Subsequently, the relevant studies were downloaded and
further screened to identify the potentially eligible studies. When
essential data were not provided in the original studies, every
effort was made to contact the authors for confirmation.
Inclusion/exclusion criteria
All the relevant case-control studies were included,
irrespective of languages. In the meta-analysis, the following
criteria were set and reviewed by two independent investigators: i)
Studies should be concerned with the association of the
CYP1A1 MspI polymorphism with oral squamous cell carcinoma
risk, and OSCC cases were histologically confirmed; ii) each trial
should be an observational study (case-control or cohort) of human
subjects; iii) studies must offer the size of the sample, and the
genetic distribution or the original information that can help
infer the results; and iv) when multiple studies from a particular
research group reported data from overlapping samples, the study
reporting the largest dataset was included.
Exclusion criteria included: i) Review studies,
editorials or meta-analysis; ii) case reports or lack of
case-control study; and iii) studies that estimated the risk of
secondary tumors, recurrence or response to treatment. For a
conflicting evaluation, an agreement was reached following a
discussion. When a consensus could not be attained, another
investigator was invited to resolve the dispute and a final result
was generated by the majority. All the studies were viewed in
accordance with the criteria defined above for further
analysis.
Data extraction
All the data were independently reviewed and
extracted with a standardized data-collection form by two
investigators (Shang Xie and Chongdai Luo). Differences between the
investigators were solved by discussion and when necessary, through
consultation. The following characteristics were collected from
each study: Ethnicity, country, sample size, control source,
matching contents, Hardy-Weinberg equilibrium and the gene
distribution of cases and controls. When the data were not clear or
presented by the author in the publication, contact for further
details was attempted.
Quality assessment
The Newcastle-Ottawa scale (NOS) quality evaluation
criteria was performed to evaluate the methodological quality of
the included studies and those with poor quality were excluded
(30,31). The NOS system categorizes into three
dimensions, which are selection, comparability and exposure
(case-control studies), and the three dimensions included eight
items. A star system was used to assess the quality of all the
included studies. The NOS ranges from zero (the lowest) to nine
(the highest) stars. The assessment was performed independently by
two investigators and the discrepancy was resolved by a
discussion.
Statistical analysis
All the data management and analysis for the
meta-analysis was performed with STATA 11.0 software (Stata
Corporation, College Station, TX, USA). The odds ratio (ORs) with
corresponding 95% confidence intervals (CIs) were used to estimate
the associations between the CYP1A1 MspI polymorphism and
OSCC risks. In order to calculate the heterogeneity of the studies,
the χ2 test was used and P<0.05 was considered to
indicate a statistically significant difference (32). The inconsistency index, I2,
was calculated to assess the variation caused by heterogeneity.
When the P-value of the heterogeneity test was >0.10, the
fixed-effects model was performed to calculate the combined OR,
which assumed the same homogeneity of effect size across all the
studies. When the P-value of the heterogeneity test was <0.10,
the between-study heterogeneity was considered to indicate a
statistically significant difference, and a random effect model was
used to estimate the pooled OR. The funnel plot was used to test
the underlying publication bias, and the funnel plot asymmetry was
estimated by Egger's linear regression (33). Sensitivity analyses were performed to
identify the influence of the individual studies on the combined
OR. In the analysis, each study was excluded to assess whether
stability between the remaining studies was reached.
Results
Characteristics of included
studies
A total of 212 studies were retrieved by the
literature search. In total, 171 studies were excluded as they were
irrelevant to CYP1A1 MspI, OSCC or gene polymorphisms, and
were not human studies. Two other potential eligible studies were
obtained by screening the references of reviews. Following more
detailed evaluations for the remaining 43 potential eligible
studies, one study obtained from references did not meet the
purpose of the meta-analysis (34),
and four were reviews (26,35–37).
Following this, six studies only regarded CYP1A1 exon 7, but
not CYP1A1 MspI (38–43). Another sixteen studies were excluded
as one of them presented overlapping data (44) and 15 failed to provide sufficient
genotyping data (45–59). In addition, there were five studies
excluded as the cases were diagnosed as oral cancer only, and the
identification of OSCC was not confirmed (60–64). One
study was excluded as the study only contained the cases and lacked
the controls (65). Finally, 10
studies conformed to the inclusion criteria and were included in
the meta-analysis of CYP1A1 MspI (16–25). The
search process is shown in Fig.
1.
A database with regard to the information extracted
from each included study was established. Summaries of these
studies are presented in Table I,
which includes the first author, ethnicity, country, number and
characteristics of cases and controls, and other necessary
information. Of the 10 studies included in the meta-analysis, seven
studies were performed in Asian countries, two in American
countries and one in European countries. The number of cases and
controls in the studies included varied from 38–446 and 81–727,
respectively. The frequency of the CYP1A1 MspI homozygous
variant allele (C/C) in the cases group varied from 0–30.0%, and
0–10.5% for the control group.
 | Table I.Characteristics of the excluded
studies evaluating the effects of the CYP1A1 MspI
polymorphism on the susceptibility of OSCC. |
Table I.
Characteristics of the excluded
studies evaluating the effects of the CYP1A1 MspI
polymorphism on the susceptibility of OSCC.
|
|
|
|
| Cases, n | Controls, n |
|
|
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Year | First author
(ref) | Ethnicity | Quality assessment
(NOS) | TT | TC | CC | TT | TC | CC | Cases, n | Controls, n | Control source | Matching | HWE (control) |
|---|
| 1999 | Sato (18) | Asian | 8/9 | 56 | 55 | 31 | 62 | 65 | 15 | 142 | 142 | Healthy | Age, gender | 0.738 |
| 1999 | Tanimoto (16) | Asian | 8/9 | 32 | 53 | 15 | 62 | 30 | 8 | 100 | 100 | Hospital | Age, gender | 0.126 |
| 2002 | Kao (21) | Asian | 6/9 | 40 | 52 | 14 | 53 | 79 | 14 | 106 | 146 | Hospital | NA | 0.046 |
| 2003 | Gronau (22) | Caucasian | 8/9 | 55 | 18 | 0 | 100 | 35 | 1 | 73 | 136 | Hospital | Age, gender,
tobacco and alcohol habits | 0.260 |
| 2006 | Gattás (23) | Mixed-race | 8/9 | 25 | 13 | (TC+CC) | 63 | 39 | (TC+CC) | 38 | 102 | Hospital | Age, gender | NA |
| 2007 | Anantharaman
(25) | Asian | 8/9 | 205 | 195 | 46 | 331 | 345 | 51 | 446 | 727 | Hospital, dental
clinic | Age, gender,
tobacco habits | 0.002 |
| 2007 | Cha (24) | Asian | 6/9 | 20 | 30 | 22 | 49 | 97 | 17 | 72 | 163 | Hospital | NA | 0.002 |
| 2008 | Losi-Guembarovski
(20) | Mixed-race | 7/9 | 55 | 27 | 9 | 53 | 23 | 5 | 91 | 81 | Hospital | Age, gender,
tobacco habits | 0.262 |
| 2008 | Sam (19) | Asian | 8/9 | 77 | 86 | 24 | 115 | 91 | 14 | 187 | 220 | Hospital | Age, gender | 0.475 |
| 2012 | Shukla (17) | Asian | 8/9 | 45 | 60 | 45 | 72 | 72 | 6 | 150 | 150 | Hospital | Age, gender,
tobacco habits | 0.020 |
Results of quality assessment
According to the NOS system, all the included
case-control studies were awarded a maximum of four stars in
selection, two stars in comparability and three stars in exposure.
The results of the assessment for the included studies ranged from
six to eight stars (Table I),
indicating that all the included studies were moderate-high
qualities.
Test of heterogeneity and quantitative
synthesis
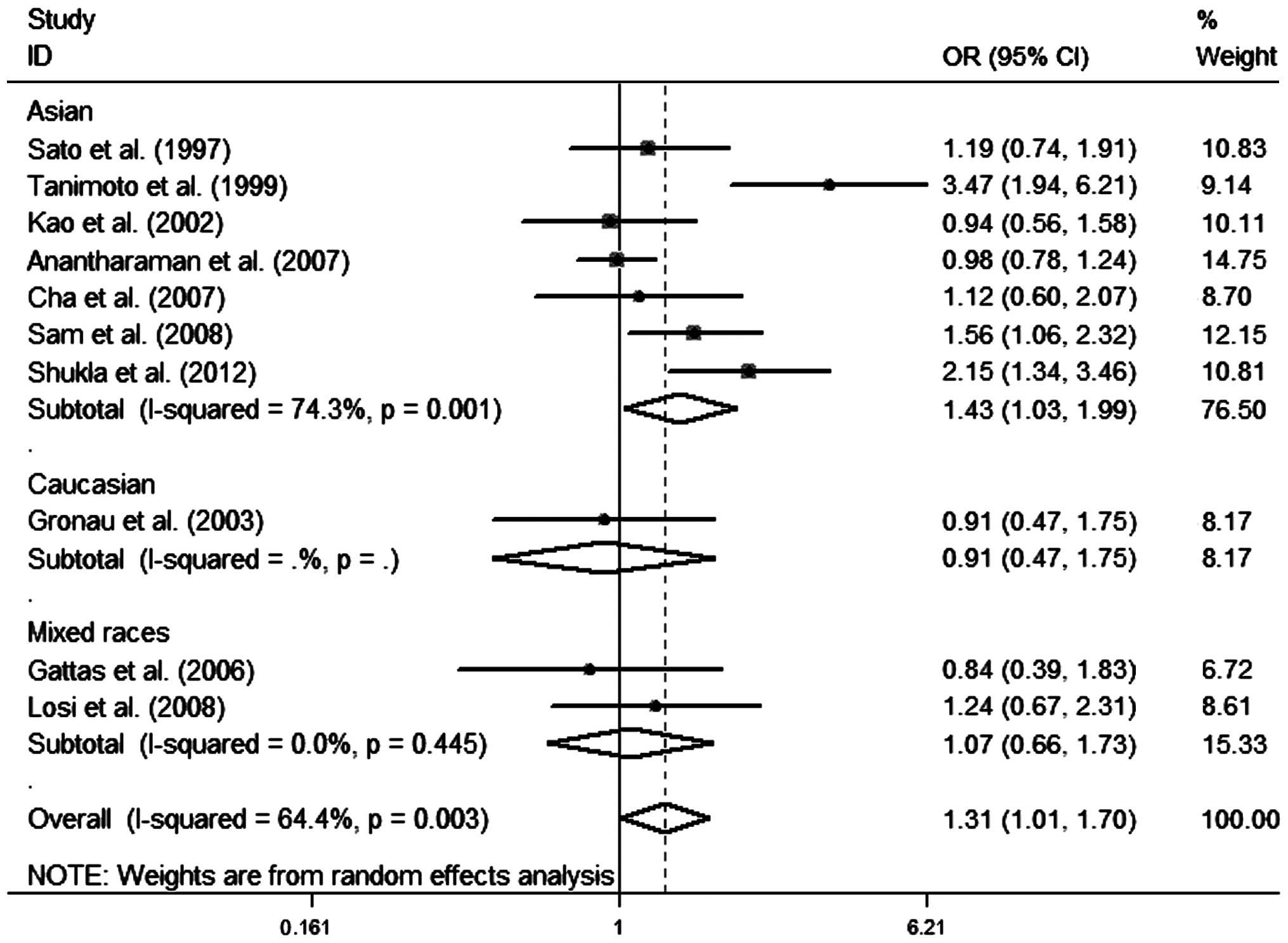
A heterogeneity analysis was performed of the
dominant (CC+TC vs. TT), recessive (CC vs. TC+TT) and additive
models (CC vs. TT), and the results are shown in Table II. Owing to the overall heterogeneity
observed in the dominant (CC+TC vs. TT: I2=64.4%,
P=0.003), recessive (CC vs. TC+TT: I2=57.9%, P=0.015)
and additive models (CC vs. TT: I2=61.0%, P=0.009),
random-effect models were used to synthesize the data, respectively
(Table II). The overall results
suggested that the CYP1A1 gene variants (TC+CC or CC) have
an increased risk of OSCC compared to those individuals with the
positive homozygous carriers (TT). In order to further explore the
observed heterogeneity, subgroup analyses were performed by
ethnicity and 10 studies were divided into three subgroups: the
Asian, Caucasian and mixed-race groups. However, the heterogeneity
remained in the Asian population, but not in the mixed-race and
Caucasian populations. For ethnicity, a significant increased risk
was associated with the genetic variants among the Asian
population, while no associations were found among the mixed ethnic
and Caucasian populations (Fig. 2 and
Table II).
 | Table II.Main results of the heterogeneity
test in the meta-analysis. |
Table II.
Main results of the heterogeneity
test in the meta-analysis.
|
|
| CC+TC vs. TT | CC vs. TC+TT | CC vs. TT |
|---|
|
|
|
|
|
|
|---|
| CYP1A1
MspI | No. of studies
(case/controls) | OR (95% CI) | I2
(%) |
PQ-test | P-value | OR (95% CI) | I2
(%) |
PQ-test | P-value | OR (95% CI) | I2
(%) |
PQ-test | P-value |
|---|
| Total
ethnicity | 3372
(1405/1967) | 1.31 (1.01,
1.70) | 64.4 | 0.003 | 0.043 | 2.38 (1.58,
3.58) | 57.9 | 0.015 | <0.001 | 2.52 (1.60,
3.98) | 61.0 | 0.009 | <0.001 |
| Caucasian | 209 (73/136) | 0.91 (0.47,
1.75) | − | − | 0.775 | 0.62
(0.02, 15.39) | − | − |
0.770 | 0.60
(0.02,15.07) | − | − |
0.758 |
| Asian | 2851
(1203/1648) | 1.43 (1.03,
1.99) | 74.3 | 0.001 | 0.032 | 2.52 (1.60,
3.98) | 67.0 | 0.006 | <0.001 | 2.70 (1.63,
4.49) | 69.5 | 0.003 | <0.001 |
| Mixed-race | 312
(129/183) | 1.07 (0.66,
1.73) |
0.0 | 0.445 | 0.798 | 1.67 (0.54,
5.20) | − | − |
0.378 | 1.73 (0.55,
5.51) | − | − |
0.351 |
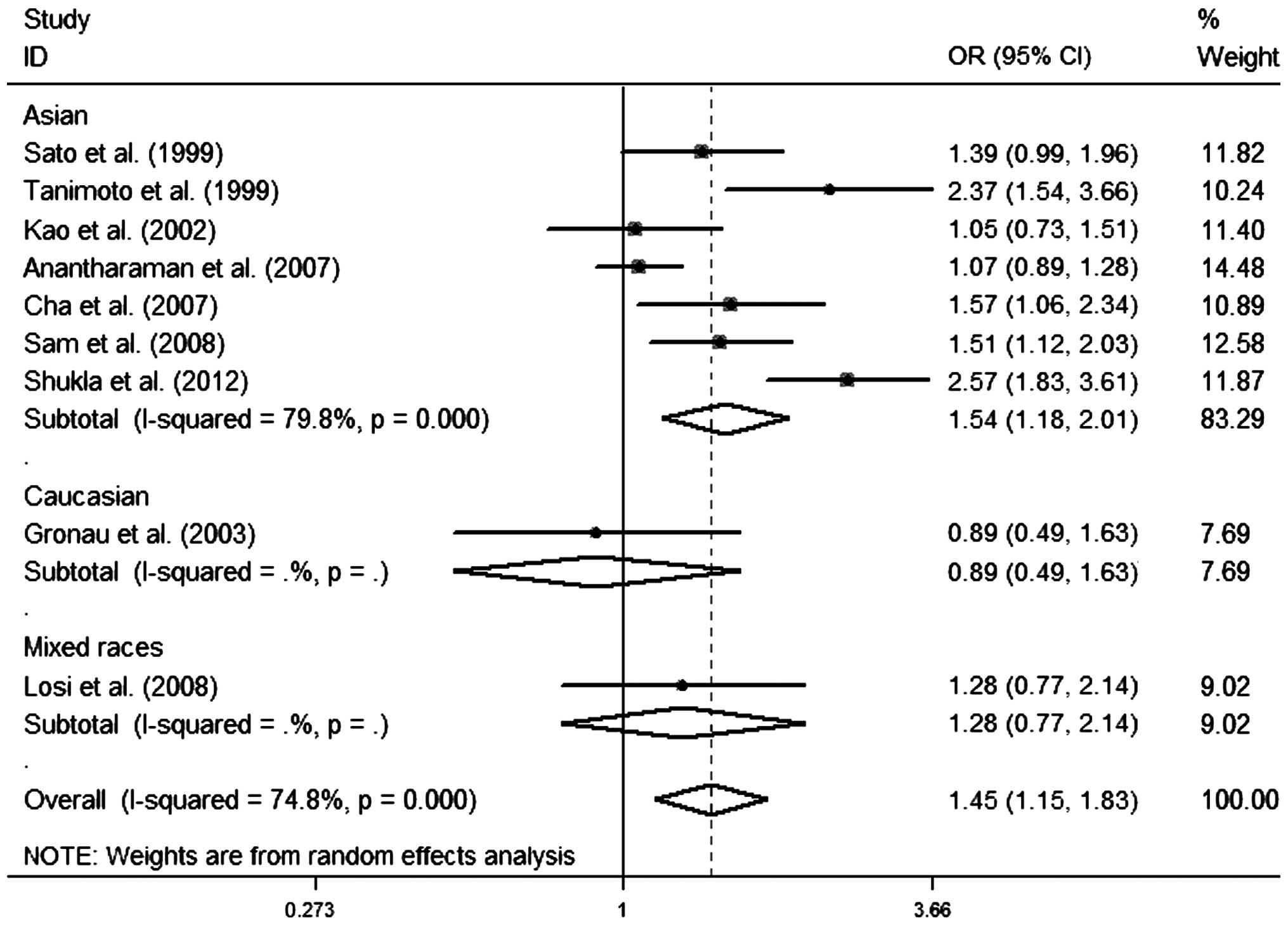
As for the C and T allele of CYP1A1 MspI, the
results of the heterogeneity test and quantitative synthesis of C
vs. T model, the pooled OR, 1.447; 95% CI, 1.146–1.827;
I2=74.8%; PQ- test=0.000; and P<0.05
(Fig. 3) suggested that the C allele
was significantly associated with an increased OSCC risk.
Publication bias analysis
The Begg's funnel plot was used to assess the
possible publication bias. The Egger's linear regression is for the
quantitative evaluation of the meta-analysis funnel plot symmetry
and the results were as follows: i) CC+TC vs. TT model: Begg's
test, P=0.858>0.05 and Egger's linear regression test: t=0.85,
P=0.419>0.05; ii) CC vs. TC+TT model: Begg's test,
P=0.711>0.05 and Egger's linear regression test: t=1.05,
P=0.335>0.05; iii) CC vs. TT model: Begg's test, P=0.266>0.05
and Egger's linear regression test: t=1.20, P=0.276>0.05; and
iv) C vs. T allele model: Begg's test, P=1.000>0.05 and Egger's
linear regression test: t=0.99, P=0.354>0.05. The data of the
four models indicated that the funnel plots were symmetrical for
all.
Sensitivity analysis
In order to assess the stability of the results and
reflect the influence of each study on the pooled ORs, sensitivity
analysis was performed by excluding each case-control study
individually. All the estimates were included between the lower and
upper CI limits, suggesting the stability of the results in the
meta-analysis.
Discussion
Oral cancer is cancer of the mouth, including
squamous cell carcinoma, adenocarcinoma and verrucous carcinoma.
Different histopathological types of cancers may have different
genetic susceptibilities, such as CYP1A1 MspI polymorphism
being a risk factor of squamous cell carcinoma of the lung, but
varies in different histological types (13,66).
Therefore, it is more reasonable to separately evaluate the
association of gene polymorphisms with OSCC, oral adenocarcinoma
and other cancer types.
To the best of our knowledge, this is the first
meta-analysis to assess the association between the CYP1A1
MspI genetic variants and risks of OSCC. Although there are two
previous meta-analyses (67,68) regarding the CYP1A1 MspI
polymorphism and oral cancer, the results did not involve the
single histopathological type and therefore cannot represent the
association of CYP1A1 MspI with the risks of OSCC. Oral
cancer is known to include different histological types, including
squamous cell carcinoma and adenocarcinoma, which may yield to
different susceptibilities of cancer. Therefore, the previous
studies' results may regard all types of oral carcinoma for only
one selection. To obtain a powerful conclusion regarding the risks
of OSCC and CYP1A1 MspI polymorphism, a systematical
meta-analysis was performed in the present study.
In the present meta-analysis, for the overall data
the results of ORs and 95% CIs showed that the C allele of
CYP1A1 MspI played a significant role in the carcinogenesis
process resulting in OSCC, and as for the genotypes, CC and CT+CC
were identified as risk factors for developing OSCC. All the
results indicated that the CYP1A1 MspI polymorphism may
increase the risks of OSCC. The heterogeneity among studies was
observed in the dominant, recessive, additive and C versus T allele
models, respectively. Following the subgroup analysis by ethnicity,
the heterogeneity was not removed indicating that other factors,
such as age, gender, country, source of controls, lifestyle, social
status, smoking and alcohol habits, may also yield to
heterogeneities.
In the subgroup analysis by ethnicity, a key
association between the CYP1A1 MspI polymorphism and risks
of OSCC in the Asian population was confirmed in all four models,
but not in the mixed-race and Caucasian populations, suggesting
that the CYP1A1 MspI gene variants may increase the OSCC
susceptibility in the Asian population. The differences may be
attributed to different ethnicities sharing different gene-gene and
gene-environmental backgrounds. Nevertheless, the conclusion
regarding the mixed-race and Caucasian populations is not of a
sufficient power for the few studies and subjects.
Publication biases were evaluated by funnel plots
and their symmetries, and were further assessed by Begg's test and
Egger's linear regression tests, respectively. No clear biases were
observed, indicating that the publication may yield to little
effects on the results. The sensitivity analysis showed that the
importance of the corresponding pooled ORs was not significantly
changed, suggesting that the pooled ORs were stable.
However, several limitations should be addressed.
First of all, the original studies included data regarding the
Asian, Caucasian and mixed-race populations, and only one study
regarding Caucasian and two mixed-race populations. Secondly, a
subgroup analysis was performed by ethnicity, but the other
factors, such as gender, age, source of control and country, were
not performed due to data limitations. Thirdly, the Asian
population included India, Japan and China, but other Asian
countries were not included. Fourthly, heterogeneity existed, which
may weaken the reliability of the conclusions. In view of these
limitations, the results should be considered with caution.
Overall, despite several limitations the results of
the present analysis showed a clear association between the
CYP1A1 MspI polymorphism and OSCC risk, particularly among
the Asian population. Future studies focusing on the CYP1A1
MspI polymorphism containing larger sample sizes and well-matched
criteria are required to improve the credibility of the
conclusions.
Acknowledgements
The present study was supported by Special Financial
Grants from the China Postdoctoral Science Foundation (no.
2014T70836) and the National Natural Science Foundation of China
(nos. 81371162, 8110762 and 30973336). The authors acknowledge Dr
Wenjie Li (Department of Oral Health Sciences, School of Dentistry,
University of Washington, Seattle, WA, USA) and Dr Xinchen Yang
(Department of Oral Rehabilitation, Faculty of Dentistry,
University of Hong Kong, Sai Ying Pun, Hong Kong, China) for
assistance in collecting the relevant studies.
References
|
1
|
Kademani D: Oral cancer. Mayo Clin Proc.
82:878–887. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Petersen PE: Oral cancer prevention and
control - the approach of the World Health Organization. Oral
Oncol. 45:454–460. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Barnes L, Eveson JW, Reichart P and
Sidransky D: Tumours of the oral cavity and oropharynx. World
Health Organization Classification of Tumours: Pathology and
Genetics of Head and Neck Tumours. 9:(3rd). (Lyon, France). IARC
Press. 166–210. 2005.
|
|
4
|
Chen GS and Chen CH: A study on survival
rates of oral squamous cell carcinoma. Kaohsiung J Med Sci.
12:317–325. 1996.(In Chinese). PubMed/NCBI
|
|
5
|
Lim YC and Choi EC: Surgery alone for
squamous cell carcinoma of the oral cavity: survival rates,
recurrence patterns, and salvage treatment. Acta Otolaryngol.
128:1132–1137. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lo Muzio L, Campisi G, Farina A, et al:
P-cadherin expression and survival rate in oral squamous cell
carcinoma: an immunohistochemical study. BMC Cancer. 5:632005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Blot WJ, McLaughlin JK, Winn DM, et al:
Smoking and drinking in relation to oral and pharyngeal cancer.
Cancer Res. 48:3282–3287. 1988.PubMed/NCBI
|
|
8
|
Ruiz Figuero E, Peláez Carretero MA,
Lapiedra Cerero R, Gómez Esparza G and López Moreno LA: Effects of
the consumption of alcohol in the oral cavity: relationship with
oral cancer. Med Oral. 9:14–23. 2004.PubMed/NCBI
|
|
9
|
Johnson N: Tobacco use and oral cancer: a
global perspective. J Dent Educ. 65:328–339. 2001.PubMed/NCBI
|
|
10
|
Zhang Y, Ni Y, Zhang H, Pan Y, Ma J and
Wang L: Association between GSTM1 and GSTT1 allelic variants and
head and neck squamous cell cancinoma. PLoS One. 7:e475792012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang Y, Yang H, Li L and Wang H:
Glutathione S-transferase T1 gene deletion polymorphism and lung
cancer risk in Chinese population: a meta-analysis. Cancer
Epidemiol. 34:593–597. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pei YL, Zhang HL and Han HG: Polymorphism
of 8q24 rsl3281615 and breast cancer risk: a meta-analysis. Tumor
Biol. 34:421–428. 2013. View Article : Google Scholar
|
|
13
|
Ji YN, Wang Q and Suo LJ: CYP1A1 Ile462Val
polymorphism contributes to lung cancer susceptibility among lung
squamous carcinoma and smokers: a meta-analysis. PloS One.
7:e433972012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hashibe M, Brennan P, Strange RC, et al:
Meta- and pooled analyses of GSTM1, GSTT1, GSTP1, and CYP1A1
genotypes and risk of head and neck cancer. Cancer Epidemiol
Biomarkers Prev. 12:1509–1517. 2003.PubMed/NCBI
|
|
15
|
Feng X, Zhou H-F, Zheng B-S, Shi J-J, Luo
C and Qin J-J: Association of glutathione S-transferase P1 gene
polymorphism with the histological types of lung cancer: a
meta-analysis. Mol Biol Rep. 40:2439–2447. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tanimoto K, Hayashi S, Yoshiga K and
Ichikawa T: Polymorphisms of the CYP1A1 and GSTM1 gene involved in
oral squamous cell carcinoma in association with a cigarette dose.
Oral Oncol. 35:191–196. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shukla D, Kale Dinesh A, Hallikerimath S,
Vivekanandhan S and Venkatakanthaiah Y: Genetic polymorphism of
drug metabolizing enzymes (GSTM1 and CYP1A1) as risk factors for
oral premalignant lesions and oral cancer. Biomed Pap Med Fac Univ
Palacky Olomouc Czech Repub. 156:253–259. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sato M, Sato T, Izumo T and Amagasa T:
Genetic polymorphism of drug-metabolizing enzymes and
susceptibility to oral cancer. Carcinogenesis. 20:1927–1931. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sam SS, Thomas V, Reddy KS, Surianarayanan
G and Chandrasekaran A: CYP1A1 polymorphisms and the risk of upper
aerodigestive tract cancers in an indian population. Head Neck.
30:1566–1574. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Losi-Guembarovski R, Cólus IM, De Menezes
RP, et al: Lack of association among polymorphic
xenobiotic-metabolizing enzyme genotypes and the occurrence and
progression of oral carcinoma in a brazilian population. Anticancer
Res. 28:1023–1028. 2008.PubMed/NCBI
|
|
21
|
Kao SY, Wu CH, Lin SC, et al: Genetic
polymorphism of cytochrome P4501A1 and susceptibility to oral
squamous cell carcinoma and oral precancer lesions associated with
smoking/betel use. J Oral Pathol Med. 31:505–511. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gronau S, Koenig-Greger D, Jerg M and
Riechelmann H: GSTM1 enzyme concentration and enzyme activity in
correlation to the genotype of detoxification enzymes in squamous
cell carcinoma of the oral cavity. Oral Dis. 9:62–67. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gattás GJ, de Carvalho MB, Siraque MS, et
al: Genetic polymorphisms of CYP1A1, CYP2E1, GSTM1, and GSTT1
associated with head and neck cancer. Head Neck. 28:819–826. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cha IH, Park JY, Chung WY, Choi MA, Kim HJ
and Park KK: Polymorphisms of CYP1A1 and GSTM1 genes and
susceptibility to oral cancer. Yonsei Med J. 48:233–239. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Anantharaman D, Chaubal PM, Kannan S,
Bhisey RA and Mahimkar MB: Susceptibility to oral cancer by genetic
polymorphisms at CYP1A1, GSTM1 and GSTT1 loci among indians:
tobacco exposure as a risk modulator. Carcinogenesis. 28:1455–1462.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bartsch H, Nair U, Risch A, Rojas M,
Wikman H and Alexandrov K: Genetic polymorphism of CYP genes, alone
or in combination, as a risk modifier of tobacco-related cancers.
Cancer Epidemiol Biomarkers Prev. 9:3–28. 2000.PubMed/NCBI
|
|
27
|
Petersen DD, McKinney CE, Ikeya K, et al:
Human CYP1A1 gene: cosegregation of the enzyme inducibility
phenotype and an RFLP. Am J Hum Genet. 48:720–725. 1991.PubMed/NCBI
|
|
28
|
Landi MT, Bertazzi PA, Shields PG, et al:
Association between CYP1A1 genotype, mRNA expression and enzymatic
activity in humans. Pharmacogenetics. 4:242–246. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhou SF, Liu JP and Chowbay B:
Polymorphism of human cytochrome P450 enzymes and its clinical
impact. Drug Metab Rev. 41:89–295. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wells GA, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa scale (NOS)
for assessing the quality of nonrandomised studies in
meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.aspAccessed.
February 03–2016
|
|
31
|
Stang A: Critical evaluation of the
Newcastle-Ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analyses. Eur J Epidemiol.
25:603–605. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cochran WG: The combination of estimates
from different experiments. Biometrics. 10:101–129. 1954.
View Article : Google Scholar
|
|
33
|
Egger M, Smith Davey G, Schneider M and
Minder C: Bias in meta-analysis detected by a simple, graphical
test. BMJ. 315:629–634. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Matthias C, Bockmühl U, Jahnke V, Harries
LW, Wolf CR, et al: The glutathione S-transferase GSTP1
polymorphism: effects on susceptibility to oral/pharyngeal and
laryngeal carcinomas. Pharmacogenetics. 8:1–6. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Khlifi R, Messaoud O, Rebai A and
Hamza-Chaffai A: Polymorphisms in the human cytochrome P450 and
arylamine N-Acetyltransferase: susceptibility to head and neck
cancers. Biomed Res Int. 2013:5827682013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liu L, Wu G, Xue F, et al: Functional
CYP1A1 genetic variants, alone and in combination with smoking,
contribute to development of head and neck cancers. Eur J Cancer.
49:2143–2151. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ruwali M and Parmar D: Association of
functionally important polymorphisms in cytochrome P450s with
squamous cell carcinoma of head and neck. Indian J Exp Biol.
48:651–665. 2010.PubMed/NCBI
|
|
38
|
Amtha R, Ching CS, Zain R, et al: GSTM1,
GSTT1 and CYP1A1 polymorphisms and risk of oral cancer: a
case-control study in Jakarta, Indonesia. Asian Pac J Cancer Prev.
10:21–26. 2009.PubMed/NCBI
|
|
39
|
Buch SC, Nazar-Stewart V, Weissfeld JL and
Romkes M: Case-control study of oral and oropharyngeal cancer in
whites and genetic variation in eight metabolic enzymes. Head Neck.
30:1139–1147. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Katoh T: Application of molecular biology
to occupational health field - the frequency of gene polymorphism
of cytochrome P450 1A1 and glutathione S-transferase M1 in patients
with lung, oral and urothelial cancer. J UOEH. 17:271–278. 1995.(In
Japanese). PubMed/NCBI
|
|
41
|
Katoh T, Kaneko S, Kohshi K, et al:
Genetic polymorphisms of tobacco- and alcohol-related metabolizing
enzymes and oral cavity cancer. Int J Cancer. 83:606–609. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Marques CF, Koifman S, Koifman RJ,
Boffetta P, Brennan P and Hatagima A: Influence of cyp1a1, CYP2E1,
GSTM3 and NAT2 genetic polymorphisms in oral cancer susceptibility:
results from a case-control study in Rio de Janeiro. Oral Oncol.
42:632–637. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sugimura T, Kumimoto H, Tohnai I, et al:
Gene-environment interaction involved in oral carcinogenesis:
molecular epidemiological study for metabolic and DNA repair gene
polymorphisms. J Oral Pathol Med. 35:11–18. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Shukla D, Kale AD, Hallikerimath S,
Yerramalla V, Subbiah V and Mishra S: Association between GSTM1 and
CYP1A1 polymorphisms and survival in oral cancer patients. Biomed
Pap Med Fac Univ Palacky Olomouc Czech Repub. 157:304–310.
2013.PubMed/NCBI
|
|
45
|
Anantharaman D, Samant TA, Sen S and
Mahimkar MB: Polymorphisms in tobacco metabolism and DNA repair
genes modulate oral precancer and cancer risk. Oral Oncol.
47:866–872. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Boccia S, Cadoni G, Sayed-Tabatabaei FA,
et al: CYP1A1, CYP2E1, GSTM1, GSTT1, EPHX1 exons 3 and 4, and NAT2
polymorphisms, smoking, consumption of alcohol and fruit and
vegetables and risk of head and neck cancer. J Cancer Res Clin
Oncol. 134:93–100. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Canova C, Richiardi L, Merletti F, et al:
Alcohol, tobacco and genetic susceptibility in relation to cancers
of the upper aerodigestive tract in northern Italy. Tumori.
96:1–10. 2010.PubMed/NCBI
|
|
48
|
Cury NM, Russo A, Galbiatti ALS, et al:
Polymorphisms of the CYP1A1 and CYP2E1 genes in head and neck
squamous cell carcinoma risk. Mol Biol Rep. 39:1055–1063. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ko Y, Abel J, Harth V, et al: Association
of CYP1B1 codon 432 mutant allele in head and neck squamous cell
cancer is reflected by somatic mutations of p53 in tumor tissue.
Cancer Res. 61:4398–4404. 2001.PubMed/NCBI
|
|
50
|
Olivieri EH, da Silva SD, Mendonca FF, et
al: CYP1A2*1C, CYP2E1*5B, and GSTM1 polymorphisms are predictors of
risk and poor outcome in head and neck squamous cell carcinoma
patients. Oral Oncol. 45:e73–e79. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ramadas K, Ramachandran S, Muwonge R and
Pillai MR: Tumor progression in the oral cavity: The significance
of genetic polymorphisms in CYP1A1, GST M1 and XRCC1 in a south
Indian population. Oral Oncol Supplement. (Suppl 3): 69. 2009.
View Article : Google Scholar
|
|
52
|
Sabitha K, Reddy MV and Jamil K: Smoking
related risk involved in individuals carrying genetic variants of
CYP1A1 gene in head and neck cancer. Cancer Epidemiol. 34:587–592.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Sam SS, Thomas V, Reddy KS, Surianarayanan
G and Chandrasekaran A: Gene-gene interactions of drug metabolizing
enzymes and transporter protein in the risk of upper aerodigestive
tract cancers among indians. Cancer Epidemiol. 34:626–633. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sam SS, Thomas V, Reddy KS, Surianarayanan
G and Chandrasekaran A: Gene-environment interactions associated
with CYP1A1 Mspi and GST polymorphisms and the risk of upper
aerodigestive tract cancers in an indian population. J Cancer Res
Clin Oncol. 136:945–951. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sharma R, Ahuja M, Panda NK and Khullar M:
Combined effect of smoking and polymorphisms in tobacco
carcinogen-metabolizing enzymes CYP1A1 and GSTM1 on the head and
neck cancer risk in North Indians. DNA Cell Biol. 29:441–448. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Sharma R, Ahuja M, Panda NK and Khullar M:
Interactions among genetic variants in tobacco metabolizing genes
and smoking are associated with head and neck cancer susceptibility
in North Indians. DNA Cell Biol. 30:611–616. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sharma R, Panda NK and Khullar M:
Hypermethylation of carcinogen metabolism genes, CYP1A1, CYP2A13
and GSTM1 genes in head and neck cancer. Oral Dis. 16:668–673.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Singh AP, Shah PP, Ruwali M, Mathur N,
Pant MC and Parmar D: Polymorphism in cytochrome P4501A1 is
significantly associated with head and neck cancer risk. Cancer
Invest. 27:869–876. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yadav SS, Ruwali M, Pant MC, Shukla P,
Singh RL and Parmar D: Interaction of drug metabolizing cytochrome
P450 2D6 poor metabolizers with cytochrome P450 2C9 and 2C19
genotypes modify the susceptibility to head and neck cancer and
treatment response. Mutat Res. 684:49–55. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Chatterjee S, Dhar S, Sengupta B, et al:
Polymorphisms of CYP1A1, GSTM1 and GSTT1 loci as the genetic
predispositions of oral cancers and other oral pathologies: tobacco
and alcohol as risk modifiers. Indian J Clin Biochem. 25:260–272.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Cordero K, Espinoza I, Caceres D, et al:
Oral cancer susceptibility associated with the CYP1A1 and GSTM1
genotypes in Chilean individuals. Oncol Lett. 1:549–553.
2010.PubMed/NCBI
|
|
62
|
Guo L, Zhang C, Shi S and Guo X:
Correlation between smoking and the polymorphisms of cytochrome
P450 1A1-Msp I and glutathione s-transferase T1 genes and oral
cancer. Hua Xi Kou Qiang Yi Xue Za Zhi. 30:187–191. 2012.(In
Chinese). PubMed/NCBI
|
|
63
|
Masood N, Kayani MA, Malik FA, Mahjabeen
I, Baig RM and Faryal R: Genetic variations in carcinogen
metabolizing genes associated with oral cancer in pakistani
population. Asian Pac J Cancer Prev. 12:491–495. 2011.PubMed/NCBI
|
|
64
|
Matthias C, Bockmühl U, Jahnke V, et al:
Polymorphism in cytochrome P450 CYP2D6, CYP1A1, CYP2E1 and
glutathione S-transferase, GSTM1, GSTM3, GSTT1 and susceptibility
to tobacco-related cancers: studies in upper aerodigestive tract
cancers. Pharmacogenetics. 8:91–100. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Chatterjee S, Chakrabarti S, Sengupta B,
et al: Prevalence of CYP1A1 and GST polymorphisms in the population
of northeastern India and susceptibility of oral cancer. Oncol Res.
17:397–403. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Zhan P, Wang Q, Qian Q, Wei S-Z and Yu
L-K: CYP1A1 MspI and exon7 gene polymorphisms and lung cancer risk:
an updated meta-analysis and review. J Exp Clin Cancer Res.
30:992011. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhuo W, Wang Y, Zhuo X, et al: CYP1A1 and
GSTM1 polymorphisms and oral cancer risk: association studies via
evidence-based meta-analyses. Cancer Invest. 27:86–95. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Zhuo X, Zhao H, Chang A, et al:
Quantitative assessment of CYP1A1*2A variations with oral carcinoma
susceptibility: evidence from 1,438 cases and 2,086 controls.
Cancer Invest. 30:552–559. 2012. View Article : Google Scholar : PubMed/NCBI
|