Introduction
Osteosarcoma is the most common solid malignancy of
the bone, with an incidence of 2–3 per 106,000 individuals, but
8–11 per 106,000 individuals aged 15–19 years (1). Metaphyseal osteosarcoma of the femur
with a pathological fracture is common among children (2); it occurs most frequently around the
knee, whereas ~75% of the cases are located near the epiphyseal
plate (3), with an incidence of
complicating pathological fractures of ~5% (4). However, metaphyseal osteosarcoma in
children has been widely considered as a contraindication for limb
salvage surgery (2). First,
pathological fracture results in loss of the surgical border of the
tumor; thus, radical or wide resection cannot be performed
(5,6).
Second, reconstruction with prosthetic replacement is not suitable
for children who have yet to reach skeletal maturity. Third, due to
the complexity of biological reconstruction and limb shortening in
the future, certain surgeons consider rotationplasty to be a
suitable option for children following tumor resection around the
knee (7). In this study, we present
two cases of pediatric patients who received limb salvage treatment
with preservation of the epiphysis, including wide resection of the
tumor and biological reconstruction by allogeneic bone and fibular
autograft. We recommend this method for children with distal
femoral osteosarcoma complicated by pathological fracture.
Case reports
Case 1
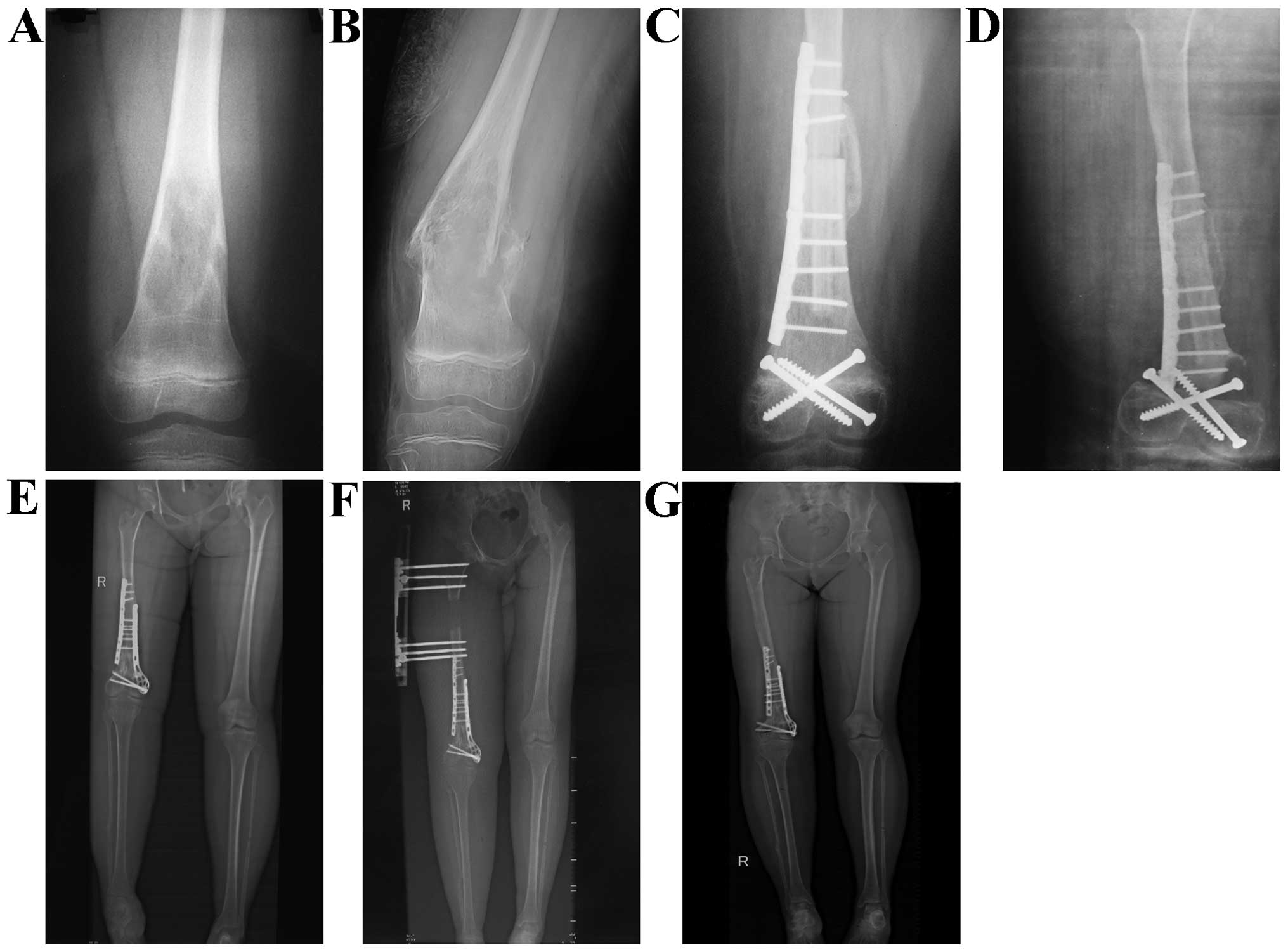
The first patient was a girl aged 11 years who
experienced pain in the lower section of the left thigh for 5
months. X-ray examination at another hospital in March, 2007
revealed bone destruction (Fig. 1A)
and anti-inflammatory treatment was administered, but without
subsidence of the pain. The patient was admitted to the Department
of Orthopedics of The General Hospital of Jinan Military Commanding
Region (Shandong, China) in August, 2007, as the pain had
significantly worsened and the tumor grew rapidly. On physical
examination, edema and deformation were observed. X-ray examination
revealed bone destruction and a fracture of the left distal femur
(Fig. 1B). The left leg was
immobilized with plaster external fixation and the pathological
examination following needle aspiration biopsy confirmed the
diagnosis of osteosarcoma. Preoperative chemotherapy, containing
cisplatin (DDP) 100 mg/m2, doxorubicin (ADM) 20 mg/m2 and
ifosfamide (IFO) 2 g/m2, was immediately administered. After two
cycles, the symptoms gradually improved. Wide resection including
the epiphyseal plate was performed to ensure safe boundaries,
followed by biological reconstruction by allogeneic bone and
avascular fibular autograft for the bone defect. The follow-up
X-ray at 6 months post-operation revealed an external callus in the
proximal bone stump, but not in the distal (Fig. 1C). The follow-up X-ray at 18 months
post-operation revealed successful bone healing in the proximal
end, but allograft bone resorption was obvious in the distal end
(Fig. 1D). A second surgery was
undertaken, which included autogenous bone graft and internal
fixation. The patient resumed normal activity following
postoperative rehabilitation. The patient revisited our hospital in
July, 2012, 5 years after tumor treatment, due to limb shortening
(Fig. 1E). In order to improve limb
function, limb lengthening in the proximal femur with external
fixation was undertaken following X-ray confirmation of epiphyseal
closure. The follow-up X-ray showed an obvious limb lengthening and
the external fixation was removed after that (Fig. 1F–G). On further follow-up, the patient
had good limb function and led a normal life.
Case 2
The second patient was a boy aged 9 years, who was
admitted for dysfunction of the right knee in October, 2012. The
patient had experienced pain in the lower part of the right thigh
for 2 months, and a mass was detected 1 week prior to admission.
The patient also complained of night pain. On physical examination,
there was a deformation of the right femur and elevation of local
skin temperature. Subcutaneous veins were not apparent and a mass
sized 6×6 cm was detected on palpation. Radiography revealed
osteolytic destruction, discontinuity of the cortex, intercalation
fracture with angular deformity and soft tissue edema of the right
distal femur. There was no obvious periosteal reaction or callus
formation (Fig. 2A). The tumor was
confirmed to be osteosarcoma following needle aspiration biopsy.
Preoperative chemotherapy with DDP, ADM and IFO was immediately
administered. After two cycles, the symptoms gradually improved. An
X-ray revealed osteosclerosis and reactive periosteal bone
formation. There was no soft tissue involvement (Fig. 2B). Magnetic resonance imaging (MRI)
revealed that the osteoepiphysis proximal to the metaphyseal region
was not interrupted by the tumor. Moreover, the body of the tumor
had already shrunk and the edema had decreased (Fig. 2C). The patient underwent surgery
following preoperative chemotherapy. A homolateral vascularized
fibular autograft was prepared, as reported previously (9). The lower margin of the tumor was
resected, including the epiphyseal plate, and the other margins
were removed by wide resection (Fig.
2D). After the limb length was restored, an allogeneic bone of
appropriate size was transplanted with the intercalated
vascularized fibular autograft (Fig.
2E). The region was fixed with a locking plate. The peroneal
artery and vein were anastomosed to the lateral superior genicular
artery and vein, respectively. The blood flow in the region of the
distal fibula was immediately restored. Postoperatively, no
complications occurred. The postoperative histological findings
confirmed a negative surgical margin. At 2 weeks post-operation,
chemotherapy, which was identical to the preoperative regimen, was
administered for 10 cycles. Movement of the knee joint was allowed
3 months postoperatively and full weight-bearing mobility was
initiated at 6 months postoperatively. On further follow-up at 8
months post-operation, there was no limb length discrepancy or knee
deformity, and the range of motion in the right knee was 0–100
degrees. Radiography revealed that the transplanted bone had healed
and there was no evidence of metastasis or local recurrence
(Fig. 2F).
Discussion
Osteosarcoma is the most common primary malignant
bone tumor in children and young adults (4,8).
Approximately 5–20% of the patients suffering from osteosarcoma
develop pathological fractures during the course of preoperative
treatment (4,9). The prognostic significance of a
pathological fracture in patients with an osteosarcoma is widely
debated. It is accepted that malignant bone tumors with
pathological fractures often lead to compartment structure damage
and tumor cell spread, which makes surgeons consider amputation as
the most suitable treatment in order to avoid the dissemination of
tumor cells. However, Abudu et al consider amputation to be
a radical resection method for a local tumor, but cannot prolong
survival time (4). With the gradual
development of neoadjuvant chemotherapy, several researchers have
reported that it may be feasible to salvage the limb with
pathological fractures during osteosarcoma therapy (5,10–12). In this study, two pediatric patients
received neoadjuvant chemotherapy, which made the tumor boundaries
clearer and helped achieve a wide resection. Limb salvage surgery
with epiphyseal preservation was successful for the two patients,
and comparable with other osteosarcoma patients without
pathological fractures.
There are several advantages of epiphyseal
preservation in the removal of malignant bone tumors in children.
However, it remains unclear how to achieve safe resection in
osteosarcoma with pathological fractures. Aponte-Tinao et al
(13) reported that a margin of ≥1 cm
of normal bone from the tumor on MRI imaging was a safe resection
margin for osteosarcoma. Epiphyseal preservation may not be
suitable for some patients. When tumor cells are found in the
physeal margin, trans-epiphyseal resection or knee arthroplasty is
considered to be the appropriate surgical treatment, rather than
physeal preservation. Prosthesis replacement in children presents
with a number of difficulties, including non-standard prosthesis
size, prosthesis replaced several times and other surgical
complications, although the new extendable prosthesis is currently
recommended. A previous study indicated that prosthetic survival
rates for large-segment replacements in high-grade bone sarcoma
were 83% at 5 years and 67% at 10 years (14). There are several methods for
biological reconstruction following excision of peri-articular
osteosarcomas around the knee joint, including distraction
osteogenesis, intercalary allograft, vascularized fibular graft,
frozen autograft, or osteoarticular allograft. Manfrini et
al described a case using a fibular graft including the
proximal joint cartilage and the growth plate for reconstruction of
the proximal femur and hip joint in an osteosarcoma patient
(15). In this study, a vascularized
fibular graft and allogeneic bone of similar size were used for
repairing the bone defect for biological reconstruction. The joint
function was preserved and the patients returned to normal activity
after bone healing. Even if shortening does occur, simple
lengthening may solve the problem. The female patient in this study
underwent limb lengthening in the proximal femur with external
fixation after the X-ray confirmed epiphyseal closure.
In children, the intensity of biological
reconstruction following tumor resection is crucial. Aponte-Tinao
et al (13) analyzed 35
osteosarcoma patients with epiphyseal preservation and allograft
reconstruction, with a minimum follow-up of 5 years, and reported
11 fractures (31%) in their series. Weitao et al (16) analyzed 15 patients who underwent
epiphysis-preserving procedures for the treatment of malignant bone
tumors of the lower limb, with a minimum follow-up of 2 years, who
had reconstruction with an intercalary allograft; they reported 13
patients with delayed union (87%). As is well known, bone healing
between allogeneic bone and preserved bone is slow; the
vascularized fibular graft inside the allogeneic bone accelerates
bone healing and the fibular graft combined with allogeneic bone
ensure sufficient bone strength. In this study, allograft bone
resorption occurred distally in case 1, but not in case 2, the
possible reasons being that vascularized fibular graft is superior
to avascular fibular graft, and rigid internal fixation with a
plate is preferred to fixation with screws.
Such cases are not common. Three pediatric patients
with femoral osteosarcoma with pathological fractures were treated
in our hospital between January, 2005 and January, 2015. One
patient underwent knee replacement following an unfavorable outcome
with chemotherapy, and eventually succumbed to lung metastasis 10
months after the operation. In the two patients described herein,
the pathological fracture did not lead to tumor cell dissemination
into the knee joint, which made joint preservation possible.
Another important factor that made limb salvage surgery possible,
was that the osteosarcoma in our two cases responded well to
chemotherapy. The advantages of this reconstruction are
preservation of a normal joint in children, the possibility of
avoiding the joint complications seen with osteoarticular grafts
(eventual need for conversion to total knee arthroplasty, joint
instability) and endoprostheses (loosening, revisions). However,
this biological reconstruction must be performed on a background of
effective chemotherapy, a safe tumor resection margin, and a
surgical team experienced with microsurgical techniques. In
conclusion, limb salvage surgery with epiphyseal preservation is
not contraindicated for pediatric patients with pathological
fractures from femoral osteosarcoma.
References
|
1
|
Stiller CA, Bielack SS, Jundt G and
Steliarova-Foucher E: Bone tumours in European children and
adolescents, 1978–1997. Report from the Automated Childhood Cancer
Information System project. Eur J Cancer. 42:2124–2135. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
San-Julian M, Aquerreta JD, Benito A and
Cañadell J: Indications for epiphyseal preservation in metaphyseal
malignant bone tumors of children: Relationship between image
methods and histological findings. J Pediatr Orthop. 19:543–548.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cara JA and Canadell J: Limb salvage for
malignant bone tumors in young children. J Pediatr Orthop.
14:112–118. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Abudu A, Sferopoulos NK, Tillman RM,
Carter SR and Grimer RJ: The surgical treatment and outcome of
pathological fractures in localised osteosarcoma. J Bone Joint Surg
Br. 78:694–698. 1996.PubMed/NCBI
|
|
5
|
Salunke AA, Chen Y, Tan JH, Chen X, Khin
LW and Puhaindran ME: Does a pathological fracture affect the
prognosis in patients with osteosarcoma of the extremities? A
systematic review and meta-analysis. Bone Joint J. 96-B:1396–1403.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee RK, Chu WC, Leung JH, Cheng FW and Li
CK: Pathological fracture as the presenting feature in pediatric
osteosarcoma. Pediatr Blood Cancer. 60:1118–1121. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Merkel KD, Gebhardt M and Springfield DS:
Rotationplasty as a reconstructive operation after tumor resection.
Clin Orthop Relat Res. 270:231–236. 1991.PubMed/NCBI
|
|
8
|
Glass AG and Fraumeni JF Jr: Epidemiology
of bone cancer in children. J Natl Cancer Inst. 44:187–199.
1970.PubMed/NCBI
|
|
9
|
Jaffe N, Spears R, Eftekhari F, Robertson
R, Cangir A, Takaue Y, Carrasco H, Wallace S, Ayala A and Raymond
K: Pathologic fracture in osteosarcoma. Impact of chemotherapy on
primary tumor and survival. Cancer. 59:701–709. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xie L, Guo W, Li Y, Ji T and Sun X:
Pathologic fracture does not influence local recurrence and
survival in high-grade extremity osteosarcoma with adequate
surgical margins. J Surg Oncol. 106:820–825. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cui Q, Li DF, Liu C, Guo J, Liu SB, Liu
YS, Zhai JM and Zeng Y: Two case-reports of the limb salvage
treatment of osteosarcoma consolidated with obvious pathological
fractures. Pathol Oncol Res. 17:973–979. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zuo D, Zheng L, Sun W, Hua Y and Cai Z:
Pathologic fracture does not influence prognosis in stage IIB
osteosarcoma: A case-control study. World J Surg Oncol. 11:1482013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aponte-Tinao L, Ayerza MA, Muscolo DL and
Farfalli GL: Survival, recurrence and function after epiphyseal
preservation and allograft reconstruction in osteosarcoma of the
knee. Clin Orthop Relat Res. 473:1789–1796. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Malawer MM and Chou LB: Prosthetic
survival and clinical results with use of large-segment
replacements in the treatment of high-grade bone sarcomas. J Bone
Joint Surg Am. 77:1154–1165. 1995.PubMed/NCBI
|
|
15
|
Manfrini M, Innocenti M, Ceruso M and
Mercuri M: Original biological reconstruction of the hip in a
4-year-old girl. Lancet. 361:140–142. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Weitao Y, Qiqing C, Songtao G and Jiaqiang
W: Epiphysis preserving operations for the treatment of lower limb
malignant bone tumors. Eur J Surg Oncol. 38:1165–1170. 2012.
View Article : Google Scholar : PubMed/NCBI
|