Introduction
PACNS is a rare and poorly understood form of
vascular inflammatory disease, occurring in the brain and spinal
cord. The average annual incidence of PACNS has been reported to be
2.4 cases per 1,000,000 person-years worldwide (1). The histopathological examination of
biopsy specimens typically reveals that the arterioles and small
arteries of the parenchyma and/or leptomeninges are affected by
granulomatous inflammation (2).
Non-specific clinical manifestations and variable imaging findings
often lead to an incorrect or delayed diagnosis and treatment
(3), particularly for the extremely
rare form of tumor-like lesions. Furthermore, although a number of
reports have described the characteristics of PACNS, no clinical
case of PACNS in a patient from Northeastern China has previously
been reported. In the present study, the clinical and radiological
features of a case of histopathologically confirmed PACNS were
retrospectively analyzed, in which PACNS was initially mistaken for
malignant glioma.
Case report
A 42-year-old male patient was referred to the
Department of Neurosurgery of our hospital due to a discontinuous
headache and a 7-day history of deterioration, with 1 day of
convulsions and aphasia. Magnetic resonance imaging (MRI) of the
brain (using a Siemens Trio Tim 3.0T MRI scanner; Siemens AG,
Munich, Germany) on admission revealed a tumor-like mass with
edema, which was initially suspected to be a malignant glioma. On
account of a clear shift of the midline, craniotomy was
administered, and the lesion was totally resected (Fig. 1A), while pathological examinations
revealed no identification of any tumoral texture by the surgeon.
Concerned by a possible diagnosis of multiple sclerosis, a 3 day,
high-dose (1,000 mg daily) pulse therapy of methylprednisolone was
initiated. Serum and cerebrospinal fluid (CSF) immune routine
examinations proved to be normal. Oligoclonal bands were negative.
No marked increases in antiviral titers in the serum or the CSF
were observed. One year later, the patient complained of seizures
that had begun 2 months previously, and were characterized by 5 min
episodes of twitching in the left leg that spread to his left arm.
MRI of the brain revealed fluid attenuation inversion recovery
(‘FLAIR’) hyperintensities in the right basal ganglia, and
postoperative changes in the left frontotemporal lobe (Fig. 1B). With great interest, all the
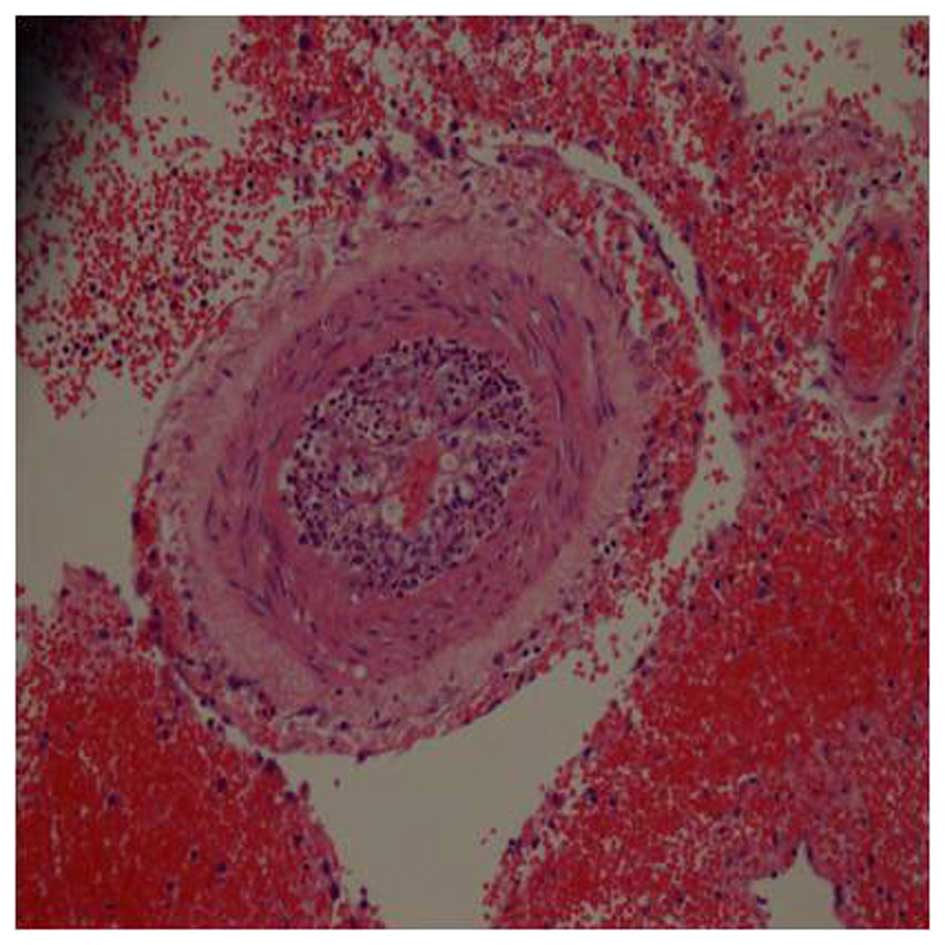
paraffin sections of the mass were carefully rechecked, and
evidence for cerebral lymphocytic vasculitis, predominantly
involving small-sized vessels, was eventually identified (Fig. 2). On the basis of the appearance of
subsequent lesions in the right basal ganglia, the patient was
treated intravenously with methylprednisone at a dose of 1,000
mg/day for 3 days, 500 mg/day for 3 days, 250 mg/day for 3 days,
and 125 mg/day for 3 days, followed by oral prednisolone at 60
mg/day and cyclophosphamide at 100 mg/day for 2 weeks. At one
year's follow-up, the patient had only aphasia, with no twitching
in the limbs.
Discussion
To the best of our knowledge, this is the first case
of clinically and pathologically confirmed PACNS in a patient from
Northeastern China. Given that the prognosis of PACNS may be poor
in the absence of specific therapy, early diagnosis and treatment
is essential. Diagnosis is often delayed due to the extremely
heterogeneous clinical presentations and non-specific MRI features
(4). PACNS presenting as a CNS mass
lesion is extremely rare, and thus, PACNS is usually not considered
in the differential diagnosis of mass lesions. A previous report
indicated that only 3–5% of the cases of PACNS presented as a CNS
mass lesion (1). Furthermore, such
cases are considered to be a fulminant form of focal CNS
vasculitis, and only differ from typical cases in that they are
more likely to be associated with amyloid angiopathy (1). Although usually non-specific, MRI
features, including the involvement of grey and white matter,
patchy contrast enhancement, intralesional hemorrhaging and normal
choline with reduced N-acetyl aspartate on magnetic resonance
spectroscopy, may help to differentiate PACNS from other mass
lesions caused by demyelination or neoplasms (5).
To date, biopsy has remained the gold standard for
confirming the diagnosis of PACNS (6). Pathologically, PACNS can present as
lymphocytic vasculitis, fibrinoid vasculitis or granulomatous
vasculitis (7). The arteries affected
are usually the smaller arteries and microscopic arterioles, and
the presentation typically involves multiple arteries, and is
multi-focal or multi-segmental. In the present case report,
craniotomy was performed on the basis of a clear shift of the
midline, whereas the pathological results predominantly revealed
lymphocytic vasculitis. Whether this histological finding
represents a specific characteristic of PACNS in Chinese patients
remains to be elucidated, due to the small number of cases observed
in the present study and the lack of published studies involving
Chinese patients.
No clinical trials have been performed in patients
with PACNS, and it is not possible to draw firm conclusions based
on outcomes in the current case report due to the non-standardized
nature of the treatment protocols used. Fountain et al
(8) reported a case of PACNS
controlled by administration of cyclophosphamide alone. Carandang
and Grant (9) reported a female
patient with PACNS who responded to steroid therapy alone. However,
Barron et al (10)
demonstrated that steroid therapy alone failed to improve the
condition in their case study. Other reports have recommended
combination therapy, consisting of prednisone and cyclophosphamide
lasting at least 1 year (1). However,
the patient in the present case study demonstrated a good response
to treatment, combining steroid and immunosuppressant therapy. A
high degree of suspicion, along with careful evaluation of the
clinical, MRI and pathological data, is required to differentiate
tumor-mimicking PACNS lesions from actual tumors and for a timely
diagnosis and treatment. Early recognition is important, since
tumor-like vasculitis usually responds poorly to steroid therapy.
Furthermore, early combined therapy with aggressive
immunosuppressive therapy and steroid may help to improve outcomes
in patients with PACNS.
References
|
1
|
Salvarani C, Brown RD Jr, Calamia KT,
Christianson TJ, Weigand SD, Miller DV, Giannini C, Meschia JF,
Huston J III and Hunder GG: Primary central nervous system
vasculitis: Analysis of 101 patients. Ann Neurol. 62:442–451. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
MacLaren K, Gillespie J, Shrestha S, Neary
D and Ballardie FW: Primary angiitis of the central nervous system:
Emerging variants. QJM. 98:643–654. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kraemer M and Berlit P: Primary central
nervous system vasculitis: Clinical experiences with 21 new
European cases. Rheumatol Int. 31:463–472. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Molloy ES, Singhal AB and Calabrese LH:
Tumour-like mass lesion: An under-recognised presentation of
primary angiitis of the central nervous system. Ann Rheum Dis.
67:1732–1735. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Panchal NJ, Niku S and Imbesi SG:
Lymphocytic vasculitis mimicking aggressive multifocal cerebral
neoplasm: MR imaging and MR spectroscopic appearance. AJNR Am
Neuroradiol. 26:642–645. 2005.
|
|
6
|
Kadkhodayan Y, Alreshaid A, Moran CJ,
Cross DT III, Powers WJ and Derdeyn CP: Primary angiitis of the
central nervous system at conventional angiography. Radiology.
233:878–882. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Koopman K, Uyttenboogaart M, Luijckx GJ,
De Keyser J and Vroomen PC: Pitfalls in the diagnosis of reversible
cerebral vasoconstriction syndrome and primary angiitis of the
central nervous system. Eur Neurol. 14:1085–1087. 2007. View Article : Google Scholar
|
|
8
|
Fountain NB and Lopes MB: Control of
primary angiitis of the CNS associated with cerebral amyloid
angiopathy by cyclophosphamide alone. Neurology. 52:660–662. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carandang CG and Grant AL: Delirium and
isolated angiitis of the central nervous system: A case report and
review. CNS Spectrums. 13:209–213. 2008.PubMed/NCBI
|
|
10
|
Barron TF, Ostrov BE, Zimmerman RA and
Packer RJ: Isolated angiitis of CNS: Treatment with pulse
cyclophosphamide. Pediatr Neurol. 9:73–75. 1993. View Article : Google Scholar : PubMed/NCBI
|