Introduction
Nerve root metastasis of carcinoma is rare, and no
cases of cervical cancer metastatic to the nerves have been
reported to date. In reported nerve root metastasis of other
tumors, surgical removal of the involved nerves has been performed,
whereas treatment with radiotherapy was also recommended (1–3). We herein
describe the case of a patient with lumbosacral nerve root
metastasis of recurrent cervical cancer. To the best of our
knowledge, intensity-modulated radiation therapy (IMRT), was
adopted for the first time to treat these lesions.
Case report
A 47 year-old woman was diagnosed with cervical
squamous cell carcinoma in 2013 and underwent radical resection in
a country hospital. The patient was confirmed to have stage IIIa
disease and received one cycle of adjuvant chemotherapy; however,
the details of the adjuvant treatment are not known. The patient
declined further treatment due to personal reasons. Six months
later, the patient presented to our hospital with pain in her right
leg, without dyskinesia. Magnetic resonance imaging (MRI)
examination revealed lymph node metastasis near the right iliac
blood vessels, involving the right iliac and internal obturator
muscles. Subsequently, the patient was treated with 6 courses of
chemotherapy with paclitaxel 210 mg and carboplatin 400 mg, every
21 days (TP regimen) and chemoradiotherapy (IMRT: Primary gross
tumor volume: 55 Gy in 25 fractions; planning target volume: 45 Gy
in 25 fractions; and chemotherapy: cisplatin 40 mg/week) for local
lesions. However, the pain in the right leg was not alleviated;
moreover, the muscle strength decreased, and the patient was nearly
unable to walk. The Visual Analog Scale (VAS) pain score was 8 to
9, the muscle strength of the right leg was level 2+, whereas it
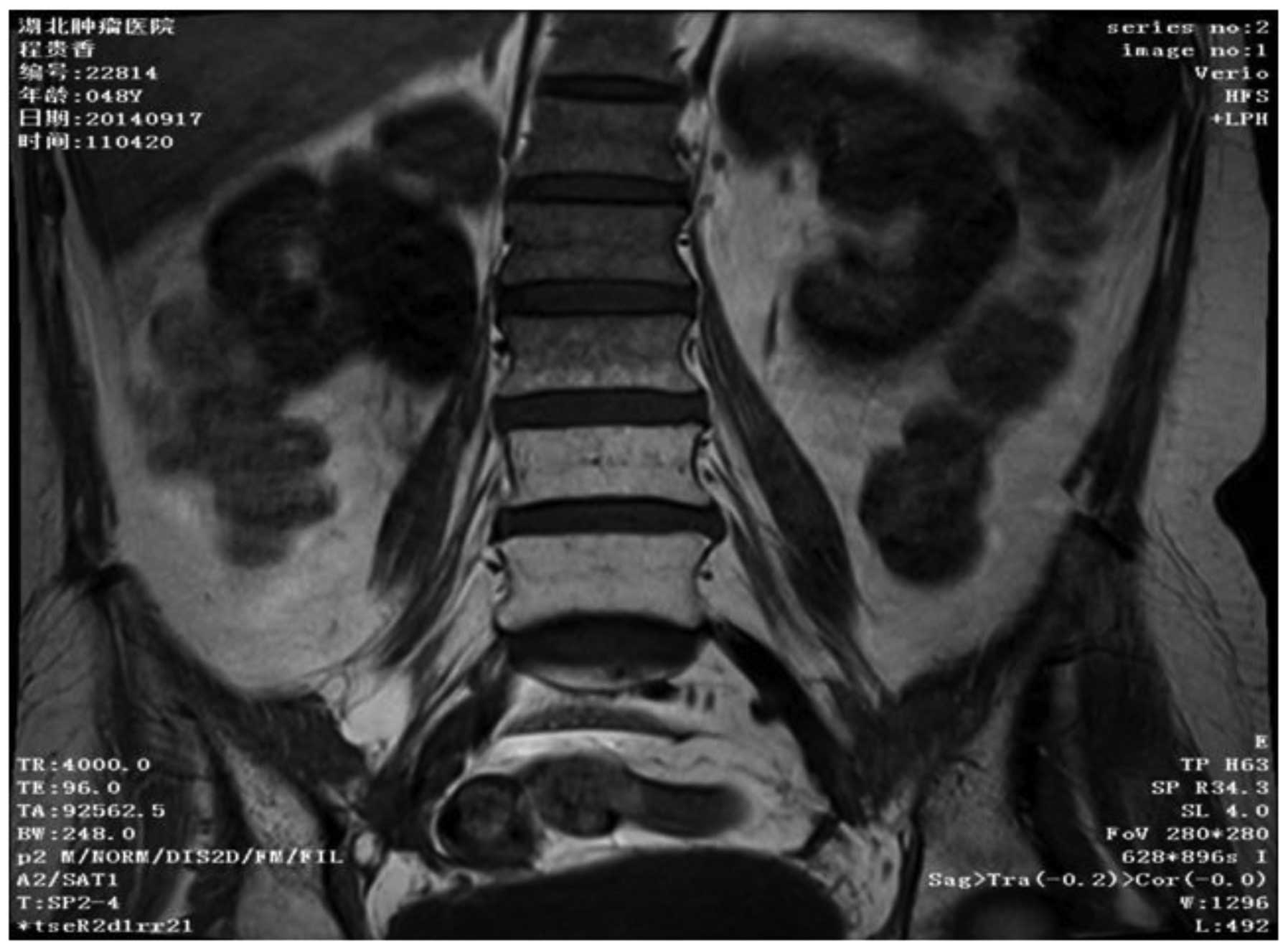
was normal in the left leg. Follow-up pelvic MRI (Fig. 1) and whole-body bone scan did not
reveal any metastases in the bones or muscles of the right lower
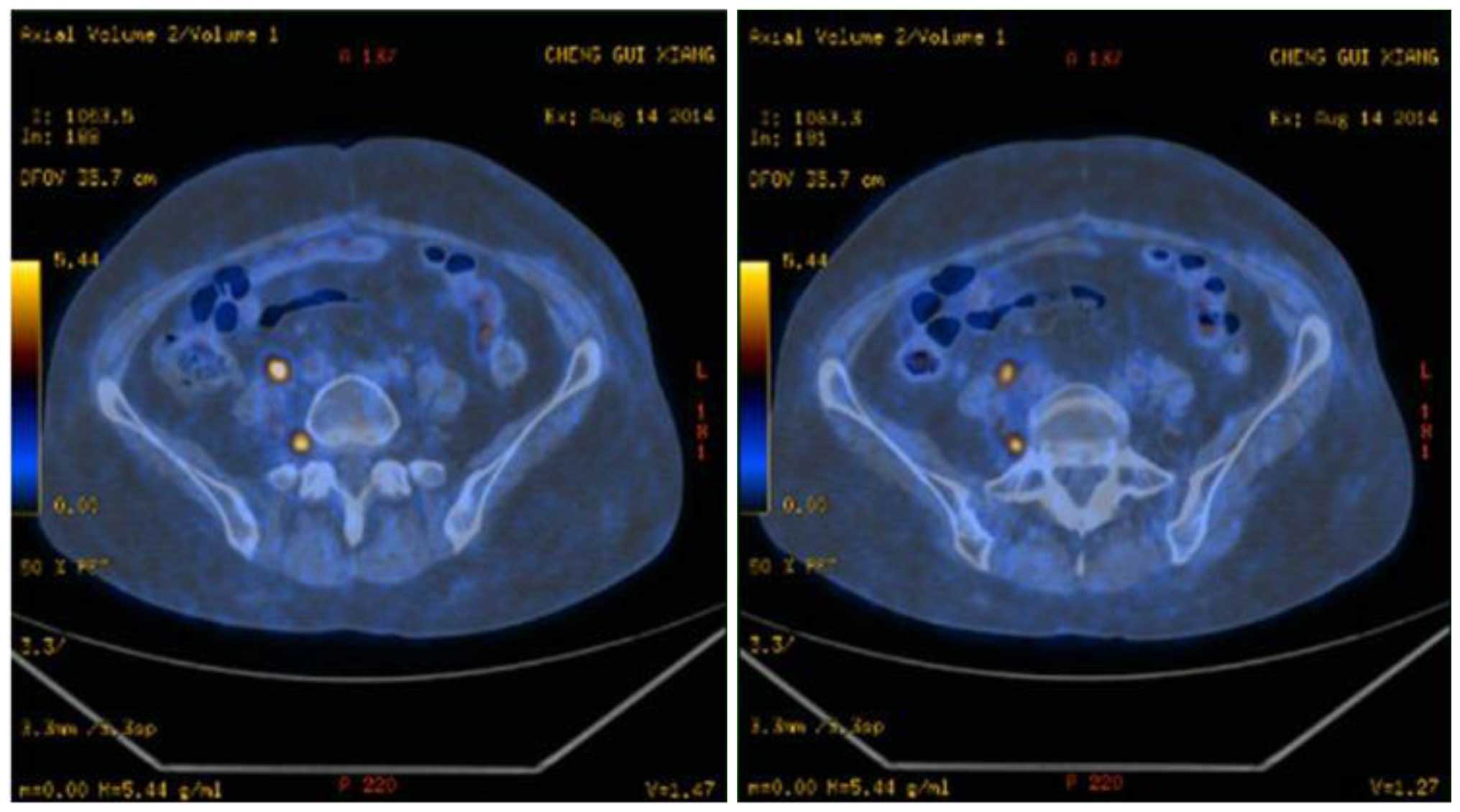
limb. Subsequently, positron emission tomography/computed
tomography (PET/CT) scan was performed (Fig. 2), revealing sacral plexus L5/S1 and
L4/5 nerve thickening, suggesting nerve metastases, which was the
cause of the intolerable leg pain.
Oxycodone 60 mg was administered every 12 h to
control the pain and a second radiotherapy was performed for the
nerve root metastases. The radiation dose was planned to be 40 Gy
in 22 fractions (Fig. 3). However,
after delivering 27 Gy (15 fractions), the patient discontinued
radiotherapy, since there was no obvious improvement in her
symptoms. One month later, the patient experienced a mild pain
relief and improved muscle strength of her right leg. The VAS pain
score decreased to 5 and the muscle strength increased to level 4.
However, the patient finally succumbed to tumor progression 3
months after the radiotherapy.
The patient's family consented to the publication of
the details and radiographic images of this case
Discussion
Cervical cancer is the second leading cause of
cancer-related mortality in women. The recurrence rate for stage
III disease is ≤42%. Distant recurrence is commonly reported in the
following sites: Para-aortic lymph nodes (81%), lungs (21%), and
supraclavicular lymph nodes (7%) (4).
However, no cases on nerve root metastasis from cervical cancer
have been reported to date. Even in other types of cancer, nerve
root metastasis is a rare occurrence. Nerve root metastasis has
been reported in renal (5), prostate
(6) and lung cancer (1), and patients with nerve root metastasis
have a very poor prognosis. However, due to the scarcity of such
cases, there is limited experience regarding their treatment.
Since MRI is of little value in the detection of
nerve root metastasis, it is very easy to miss nerve root
metastasis from cancer and delay its diagnosis and treatment
(3). Similar to malignant peripheral
nerve sheath tumors, PET/CT is more sensitive than MRI for
detection (7). Thus, in patients with
unexplained leg pain, nerve root metastasis should be considered
following exclusion of bone metastasis and PET/CT is considered a
better choice.
Moreover, the choice of treatment for our patient
was complicated. Surgery was employed in the majority of reported
cases of nerve root metastasis from cancer (1–3). Following
surgery, the pain is usually relieved, but the prognosis remains
poor. Radiotherapy may also be another recommendation. The patient
in our case refused to undergo surgery. In fact, since the tumor
was located at a deep site and her health was poor, it is
questionable whether the patient would be able to tolerate a second
surgery. Considering the fact that radiotherapy is effective for
advanced cervical cancer, we employed radiation treatment for this
patient. As it was the second radiation, a palliative dose was
administered. However, after 15 fractions of radiotherapy, the
patient discontinued treatment. Of note, although the patient did
not complete the entire course of radiotherapy, she benefited from
this treatment: Her VAS pain score decreased from >8 to 5, while
the muscle strength of the right leg increased from level 2+ to
4.
In conclusion, our experience suggests that
radiotherapy may be a practical choice for nerve root metastasis
from cervical cancer, particularly for patients with advanced-stage
disease.
Acknowledgements
The present study was partly supported by NFSC
grants (no. 81401913 to Yuan Wu).
References
|
1
|
Slotty PJ, Cornelius JF, Schneiderhan TM,
Alexander KM and Bostelmann R: Pulmonary adenocarcinoma metastasis
to a dorsal root ganglion: A case report and review of the
literature. J Med Case Rep. 7:2122013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Strong C, Yanamadala V, Khanna A, Walcott
BP, Nahed BV, Borges LF and Coumans JV: Surgical treatment options
and management strategies of metastatic renal cell carcinoma to the
lumbar spinal nerve roots. J Clin Neurosci. 20:1546–1549. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Uchida K, Kobayashi S, Yayama T, Muramatsu
J, Kurokawa T, Imamura Y and Baba H: Metastatic involvement of
sacral nerve roots from uterine carcinoma: A case report. Spine J.
8:849–852. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Peiretti M, Zapardiel I, Zanagnolo V,
Landoni F, Morrow CP and Maggioni A: Management of recurrent
cervical cancer: A review of the literature. Surg Oncol.
21:e59–e66. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cabrilo I, Burkhardt K, Schaller K and
Tessitore E: Renal carcinoma relapse presenting as a peripheral
nerve sheath tumor: A case report and brief review of the
literature. Neurochirurgie. 59:128–132. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ladha SS, Spinner RJ, Suarez GA, Amrami KK
and Dyck PJ: Neoplastic lumbosacral radiculoplexopathy in prostate
cancer by direct perineural spread: An unusual entity. Muscle
Nerve. 34:659–665. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Khiewvan B, Macapinlac HA, Lev D,
McCutcheon IE, Slopis JM, Al Sannaa G, Wei W and Chuang HH: The
value of 18F-FDG PET/CT in the management of malignant
peripheral nerve sheath tumors. Eur J Nucl Med Mol Imaging.
41:1756–1766. 2014. View Article : Google Scholar : PubMed/NCBI
|