Introduction
Prostate cancer is the second most common type of
cancer and cause of cancer-related mortality among men worldwide
(1). The prostate cancer burden is
expected to grow to 1.7 million new cases and 499,000 new deaths
worldwide by 2030, simply due to the growth and aging of the global
population (2). Surprisingly, we do
not yet objectively know the optimal treatment for this disease. To
date, radical prostatectomy and radiotherapy are the two most
widely used treatment modalities for men with clinically localized
prostate cancer (3). Although
radiotherapy is a safe and effective procedure for the treatment of
patients with early-stage prostate cancer (4), there are several common and
well-described side effects, which may compromise the quality of
life of the patients, some of which require admission to the
hospital or even surgical intervention, including urinary
incontinence, erectile dysfunction and radiation enteritis
(5,6).
Scrotal edema is another rarely encountered complication, with only
few reports in the literature. We herein report the case of a
patient with radiation enteritis who presented with recurrent
episodes of scrotal edema following pelvic radiotherapy.
Case report
A 59-year-old man was referred to our hospital with
complaints of abdominal pain and abdominal distension for 2 days.
The patient's medical history included prostate adenocarcinoma with
a Gleason score of 5 and an initial prostate-specific antigen (PSA)
level 6.3 ng/ml 3 years prior. The patient had received
radiotherapy by a nearby tertiary level-of-care hospital to a total
dose of 70 Gy within the next 7 weeks after diagnosis.
On admission, the patient's vital signs were stable,
with a blood pressure of 125/78 mmHg and a heart rate of 86 bpm. A
computed tomography (CT) scan revealed multiple gas-fluid levels in
the intestinal tract and intestinal stenosis. The patient was first
treated with fasting, nasogastric tube insertion, intravenous
fluids and inhibition of gastric acid secretion after a presumptive
diagnosis of intestinal obstruction caused by radiation injury.
Surgery was performed on the following day. During surgery, there
was no evidence of ascites, disease recurrence or metastasis;
adhesions and fibrosis were limited to the right side of the
pelvis, which conformed to radiation enteritis. The patient was
submitted to laparoscopic surgery to remove the ileocecum and
terminal ileum, combined with anastomosis of the ileum and the
ascending colon. Postoperatively, the patient received intravenous
fluids and nasogastric enteral nutrition (EN) for 5 days, until his
well intolerance of total EN. Two weeks after the operation, the
patient was allowed on a liquid diet.
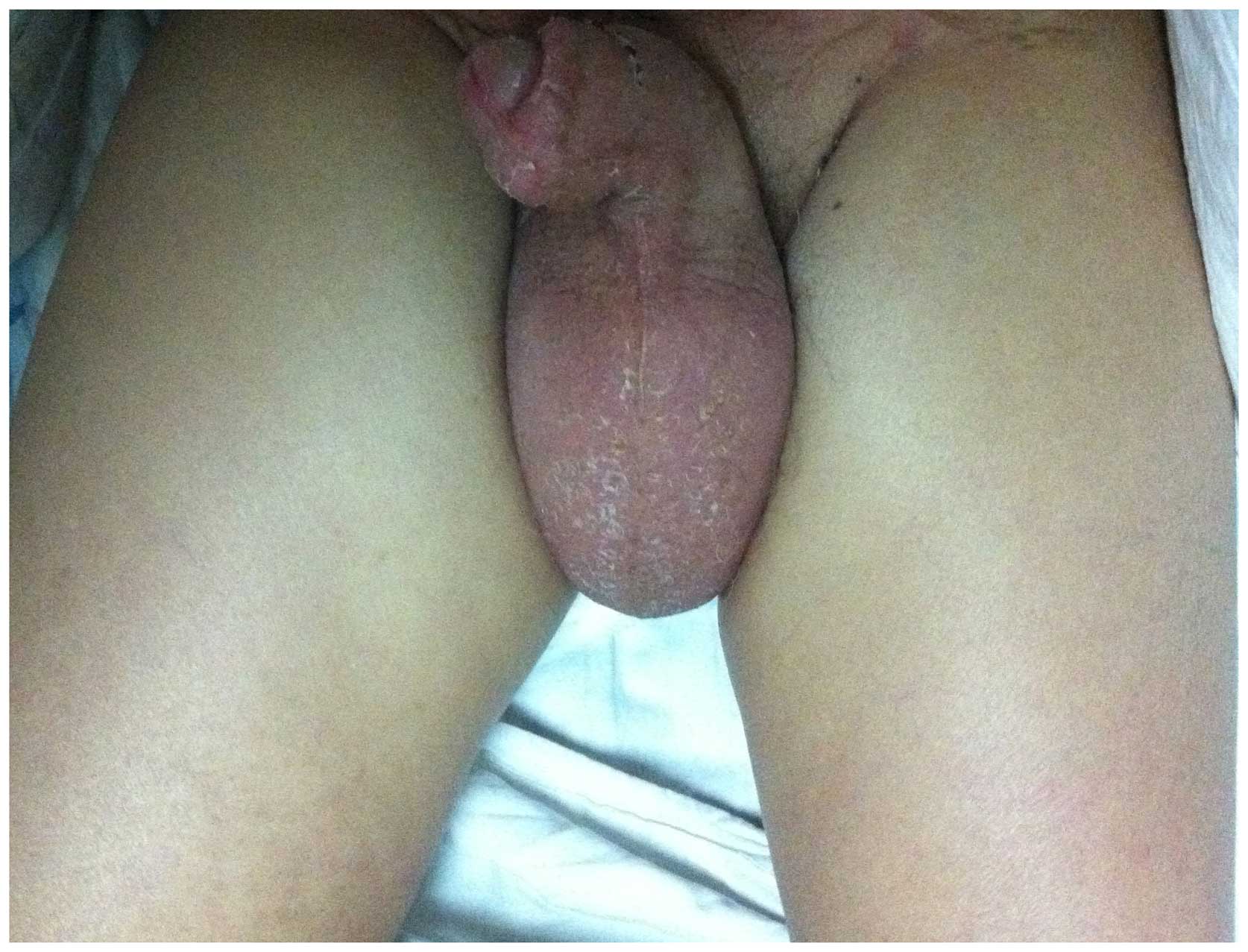
However, on the fourth postoperative day, the
patient complained of painless bilateral scrotal swelling, with
ensuing walking difficulty. There was no associated pain or
tenderness, and the scrotum did not present with other signs of
inflammation. The physical examination revealed significant
bilateral scrotal swelling, with extension of the edema to the
inguinal canals bilaterally and the penile shaft (Fig. 1). The scrotum was erythematous,
without signs of cellulitis or infection. Dipstick urinalysis
revealed no abnormalities and the laboratory results revealed a
normal white blood cell count (7.8×109/l), normal urea
and electrolyte levels, and an erythrocyte sedimentation rate of 2
mm/h. On palpation, the testes and epididymis were normal
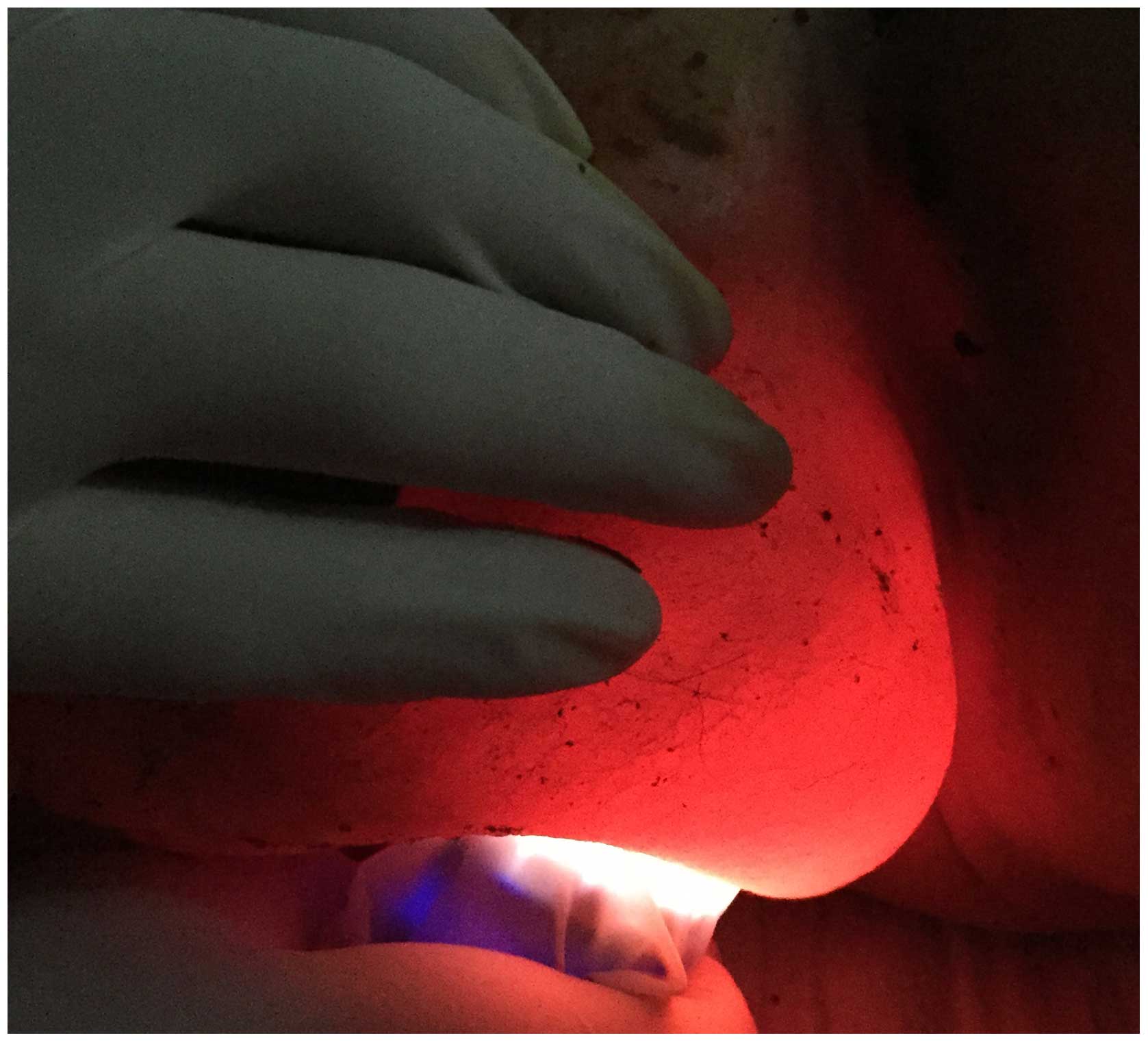
bilaterally, without pain or signs of pulsation. The
transillumination test of the scrotum was positive (Fig. 2). An ultrasound examination revealed
marked bilateral scrotal skin thickening and bilateral hydroceles
(Fig. 3). A penile examination
revealed edema of 90–95% of the penile shaft. The vascular
examination revealed no dependent, distal edema. Following detailed
medical history taking, the patient confirmed recurrent episodes of
scrotal edema 1 year after radiotherapy, and denied the presence of
other chronic illnesses, previous surgeries, history of sexually
transmitted diseases, or drug allergies. Taking into considertion
the patient's medical history, we considered a diagnosis of
secondary lymphedema caused by radiotherapy for prostate cancer.
The patient received treatment with intravenous albumin, diuretics,
and external use of Jin Huang San powder. After 1 week of
conservative treatment, the patient had lost 4 kg in weight and the
scrotal edema was almost entirely resolved.
Discussion
Wilhelm Roentgen discovered ionizing radiation in
1895. Within weeks of his discovery, scientists throughout Europe
and the United States were experimenting with radiation for
diagnostic and therapeutic purposes. Less than 2 years later,
radiation-induced deep tissue injury was first reported by Walsh
(7). Over the last century,
therapeutic radiation techniques have been refined and their
indications have been better defined. Abdominal or pelvic
radiotherapy is now commonly used for primary or adjunctive
treatment of gynecological, genitourinary and colorectal
malignancies. However, radiation-induced injury remains a major
concern, as it may lead to urinary incontinence, erectile
dysfunction, radiation enteritis and lymphedema of the lower
extremities (5,8).
Scrotal edema is a rare side effect of radiotherapy
in men with pelvic cancer; Hunter and Peschel were the first to
report persistent unilateral scrotal edema as a minor
treatment-related complication of radiotherapy in 1989 (9). To date, only few studies have reported
the development of scrotal edema in patients who received pelvic
radiation; however, they offered no further details on the cases
(10–13). Generally, the principal causes of
scrotal edema in adults are localized trauma, abnormalities of the
circulation, localized radiotherapy and lymphadenectomy. Although
the clinical significance of some of the abovementioned risk
factors has not been definitively determined, scrotal edema as a
consequence of localized radiotherapy is occasionally encountered
in patients with malignant pelvic tumors. Snijders-Keilholz et
al reported no increased rate of lymphedema following
postoperative radiotherapy; data from that study demonstrated that
lower limb edema was observed in 11% of irradiated patients vs. 10%
in patients not receiving radiotherapy (14). Kim et al reported an overall
leg edema rate of 13% after a median follow-up of 100 months in 800
patients who received adjuvant radiotherapy between 1979 and 2000
(15). However, in the present case,
we treated a male patient with radiation enteritis, who exhibited
recurrent episodes of scrotal edema following radiotherapy. After
thorough examinations, we concluded that this case may be due to
clinically suspected lymphedema. In terms of pathogenesis,
lymphedema is the result of the accumulation of protein-rich fluid
in the soft tissues secondary to inadequate lymphatic drainage. The
alterations in lymphatic drainage may result from pathological
changes, namely radionecrosis and granulation of small lymphatic
vessels, lymph nodes, and soft tissue surrounding the vessels
(16). These changes develop long
after radiotherapy, which results in the longer latency of
lymphedema appearance.
Recently, a population-based retrospective cohort
study of 32,465 men with localized prostate cancer has quantified
the incidence of several postoperative complications following
treatment with radiotherapy or radical prostatectomy. It was
demonstrated that radiotherapy was associated with a higher rate of
hospital admissions, rectal or anal procedures, open surgical
procedures and secondary malignancies, and lower rates of minimally
invasive urological procedures. Postoperative radiotherapy of
echelon lymph nodes with clinical lymphedema of the drained
extremities is a typical long-term sequel (17). In patients with prostate cancer
treated by radiotherapy, lymphedema of the scrotum has been less
extensively investigated. Due to minimal invasiveness compared with
open surgery, immediate radiotherapy has become possible shortly
after surgery. Several articles have recently described the
occurrence of scrotal edema in patients with prostate cancer as a
result of radiotherapy (10–12), but did not provide a detailed
description of the cases. The present case highlights the fact that
radiation enteritis may present with massive scrotal edema. The
clinical presentation of this case is striking, as edema was
confined to the scrotum, with minimal swelling of the lower limbs
and abdominal region. This striking physical finding is the
consequence of lymphedema possibly caused by pelvic radiation
injury, which may lead to lymphatic obstruction.
In conclusion, scrotal edema is a rare complication
of pelvic radiotherapy. Due to the serious damage of lymphatic
vessels, edema may become persistent, with gradually increasing
severity with each recurrent attack, significantly compromising the
patient's quality of life. Clinical attention should be focused on
possible primary prevention, with attention to detail regarding
radiation dose and applied technique, minimizing the risk of
toxicity during pelvic radiotherapy. Preventive strategies may
include focusing the radiation beam onto the lesion, thus
minimizing the volume of exposed surrounding tissues within the
radiation field, as well as adjusting the radiation dose.
References
|
1
|
Wu Z, Xu S, Zhong C, Gao Y, Liu Q, Zheng
Y, Guo Y, Wang Y, Luo Q and Jiang J: Intramedullary conus
medullaris metastasis from prostate carcinoma: A case report and
review of the literature. Oncol Lett. 7:717–720. 2014.PubMed/NCBI
|
|
2
|
Center MM, Jemal A, Lortet-Tieulent J,
Ward E, Ferlay J, Brawley O and Bray F: International variation in
prostate cancer incidence and mortality rates. Eur Urol.
61:1079–1092. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schirrmacher V, Bihari AS, Stücker W and
Sprenger T: Long-term remission of prostate cancer with extensive
bone metastases upon immuno- and virotherapy: A case report. Oncol
Lett. 8:2403–2406. 2014.PubMed/NCBI
|
|
4
|
Surapaneni A, Schwartz D, Nwokedi E,
Rineer J, Rotman M and Schreiber D: Radiation therapy for
clinically localized prostate cancer: Long-term results of 469
patients from a single institution in the era of dose escalation. J
Cancer Res Ther. 10:951–956. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Phillips R: Prostate cancer:
Post-treatment complications of radiotherapy and prostatectomy. Nat
Rev Urol. 11:1292014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Potosky AL, Davis WW, Hoffman RM, Stanford
JL, Stephenson RA, Penson DF and Harlan LC: Five-year outcomes
after prostatectomy or radiotherapy for prostate cancer: The
prostate cancer outcomes study. J Natl Cancer Inst. 96:1358–1367.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Walsh D: Deep tissue traumatism from
Roentgen ray exposure. Br Med J. 2:272–273. 1897. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Harb AH, Abou Fadel C and Sharara AI:
Radiation enteritis. Curr Gastroenterol Rep. 16:3832014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hunter M and Peschel RE: Testicular
seminoma. Results of the Yale University experience, 1964–1984.
Cancer. 64:1608–1611. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Petrovich Z, Lieskovsky G, Langholz B,
Luxton G, Jozsef G and Skinner DG: Radiotherapy following radical
prostatectomy in patients with adenocarcinoma of the prostate. Int
J Radiat Oncol Biol Phys. 21:949–954. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
de la Taille A, Hayek O, Benson MC,
Bagiella E, Olsson CA, Fatal M and Katz AE: Salvage cryotherapy for
recurrent prostate cancer after radiation therapy: The Columbia
experience. Urology. 55:79–84. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ghafar MA, Johnson CW, De La Taille A,
Benson MC, Bagiella E, Fatal M, Olsson CA and Katz AE: Salvage
cryotherapy using an argon based system for locally recurrent
prostate cancer after radiation therapy: The Columbia experience. J
Urol. 166:1333–1338. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ballo MT, Gershenwald JE, Zagars GK, Lee
JE, Mansfield PF, Strom EA, Bedikian AY, Kim KB, Papadopoulos NE,
Prieto VG, et al: Sphincter-sparing local excision and adjuvant
radiation for anal-rectal melanoma. J Clin Oncol. 20:4555–4558.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Snijders-Keilholz A, Hellebrekers BW,
Zwinderman AH, van de Vijver MJ and Trimbos JB: Adjuvant
radiotherapy following radical hysterectomy for patients with
early-stage cervical carcinoma (1984–1996). Radiother Oncol.
51:161–167. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim JH, Kim HJ, Hong S, Wu HG and Ha SW:
Post-hysterectomy radiotherapy in FIGO stage IB-IIB uterine
cervical carcinoma. Gynecol Oncol. 96:407–414. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Roberge D, Skamene T, Nahal A, Turcotte
RE, Powell T and Freeman C: Radiological and pathological response
following pre-operative radiotherapy for soft-tissue sarcoma.
Radiother Oncol. 97:404–407. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Füller J, Guderian D, Köhler C, Schneider
A and Wendt TG: Lymph edema of the lower extremities after
lymphadenectomy and radiotherapy for cervical cancer. Strahlenther
Onkol. 184:206–211. 2008. View Article : Google Scholar : PubMed/NCBI
|