Introduction
Several studies have reported that patients with
advanced non-small-cell lung cancer (NSCLC) with EGFR-activated
mutations respond remarkably to EGFR tyrosine-kinase inhibitors
(TKIs) (1–4). However, the role of EGFR-TKIs in
patients with wild-type EGFR remains unclear.
Erlotinib is a small-molecule EGFR-TKI that has
improved the overall survival (OS) of patients with previously
treated unselected advanced NSCLC (5). Therefore, erlotinib has been approved as
second-line treatment for such patients.
Smoking status is significantly associated with
tumor response. However, data on the effectiveness of erlotinib
treatment in patients expressing wild-type EGFR are limited.
Thyroid transcription factor-1 (TTF-1) is
tissue-specific, being expressed mainly in the lungs and thyroid
gland. Squamous cell carcinomas of the lung express TTF-1 less
frequently compared with non-squamous cell carcinoma (6,7). A history
of smoking is closely associated with squamous cell carcinoma.
Therefore, the aim of this study was to determine
whether TTF-1 may serve as a predictive biomarker of the efficacy
of erlotinib.
Patients and methods
Patients
The study population comprised patients with
non-squamous (NS)-NSCLC expressing wild-type EGFR, who were treated
with erlotinib as second- or later-line chemotherapy at the Tokyo
Metropolitan Cancer and Infectious Diseases Center, Komagome
Hospital (Tokyo, Japan) between December, 2008 and December, 2013.
The Institutional Review Board of Tokyo Metropolitan Cancer and
Infectious Diseases Center of Komagome Hospital approved the
protocol of this study and waived the need for patient written
informed consent, as routine medical data were analyzed under
complete anonymity.
Erlotinib therapy
All patients underwent a baseline assessment and
received oral erlotinib (150 mg/day) 1 h before meals, until
detection of progressive disease (PD) or intolerable toxicity.
Subsequent doses of erlotinib were modified based on toxicity at
the discretion of the treating physician.
Immunohistochemical analysis of TTF-1
expression
Lung cancer was diagnosed from tissue samples
collected during surgery, bronchoscopy, or computed
tomography-guided biopsy. All the samples were cut into 4-µm
sections and embedded in paraffin. Antigen retrieval was performed
by autoclaving the sections at 121°C for 15 min in citrate buffer
(pH 6.0). The sections were then incubated for 2 h at room
temperature with mouse monoclonal anti-TTF-1 antibody (clone SPT24;
dilution, 1:300; cat. no. NCL-L-TTF-1; Leica Microsystems K.K.,
Tokyo, Japan). Primary antibody binding to the tissue sections was
detected using Elite ABC kits (Vector Laboratories Inc.,
Burlingame, CA, USA). A pathologist (T.H.) who was blinded to the
clinical information reviewed the immunostained sections, which
were considered as positive when cytoplasmic or nuclear staining
was evident.
Statistical methods
Differences in characteristics were evaluated using
the χ2 test. Time-to-treatment failure (TTF) was defined
as the number of days that elapsed between the initiation of
erlotinib treatment and the date of initiation of any type of
subsequent therapy, or a request from the patient to terminate the
erlotinib treatment, or death. Follow-up duration was defined as
the number of days that elapsed from the initiation of erlotinib
treatment until the date of death or last follow-up. Subsequent
therapy included chemotherapy, radiotherapy and tumor
resection.
OS was defined as the number of days that elapsed
between the initiation of erlotinib treatment and death from any
cause. TTF and OS were estimated using the Kaplan-Meier method and
intergroup comparisons were assessed using log-rank tests. The
effects of 6 factors associated with patient characteristics and of
previous chemotherapy on TTF and OS were evaluated using univariate
analysis with the Cox proportional hazards model. Statistical
significance was defined as P<0.05. All statistical data were
analyzed using JMP version 9.0 software (SAS Institute, Cary, NC,
USA).
Results
Patient characteristics
We immunohistochemically analyzed TTF-1 in 26 of 53
patients treated with erlotinib monotherapy as second- or
later-line chemotherapy at our hospital between December, 2008 and
December, 2013. Among them, 20 (77%) and 6 (23%) patients were
considered as TTF-1-positive (group A) and -negative (group B),
respectively. The median age was 65 years (range, 43–77 years). Of
the 26 patients, 12 (46%) and 14 (54%) were male and female,
respectively. The performance status score was 0, 1 and 2 in 5
(19%), 15 (58%) and 6 (23%) patients, respectively, whereas 18
patients (69%) were current or former smokers. Erlotinib was
administered as second-, third- and fourth- or further-line
treatment to 4 (15%), 17 (65%) and 5 (19%) patients, respectively.
There were no significant differences between groups A and B in
these patient characteristics (Table
I).
 | Table I.Patient characteristics according to
the expression of thyroid transcription factor-1 (TTF-1). |
Table I.
Patient characteristics according to
the expression of thyroid transcription factor-1 (TTF-1).
|
| TTF-1 expression |
|
|---|
|
|
|
|
|---|
| Characteristics | Positive (n=20) | Negative (n=6) | P-value |
|---|
| Gender |
|
| 0.47 |
| Male | 10 | 2 |
|
|
Female | 10 | 4 |
|
| Age, years |
|
| 0.06 |
| ≥75 | 20 | 5 |
|
|
<75 | 0 | 1 |
|
| Smoking status |
|
| 0.88 |
|
Never | 6 | 2 |
|
| Ever | 14 | 4 |
|
| Prior
chemotherapy |
|
| 0.37 |
| 1 | 4 | 0 |
|
| 2 | 13 | 4 |
|
| ≥3 | 3 | 2 |
|
| Performance
status |
|
| 0.37 |
| 0 | 5 | 0 |
|
| 1 | 11 | 4 |
|
| 2 | 4 | 2 |
|
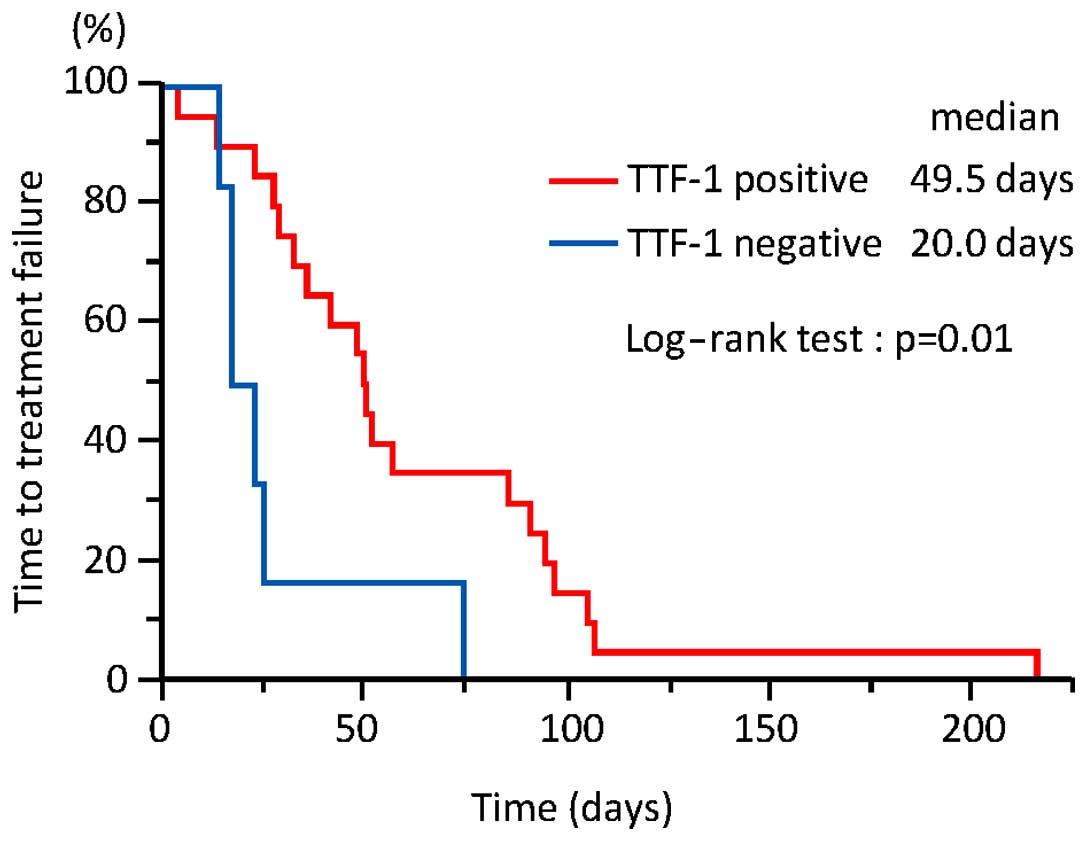
Effects of erlotinib
The median follow-up of the 26 patients was 133 days
(range, 26–873 days). As shown in Fig.
1, the TTF was significantly longer in group A compared with
that in group B [49.5 vs. 20.0 days; 95% confidence interval (CI):
28–90 vs. 14–74 days, respectively; P=0.01]. On univariate
analysis, only TTF-1 was a statistically significant predictor of
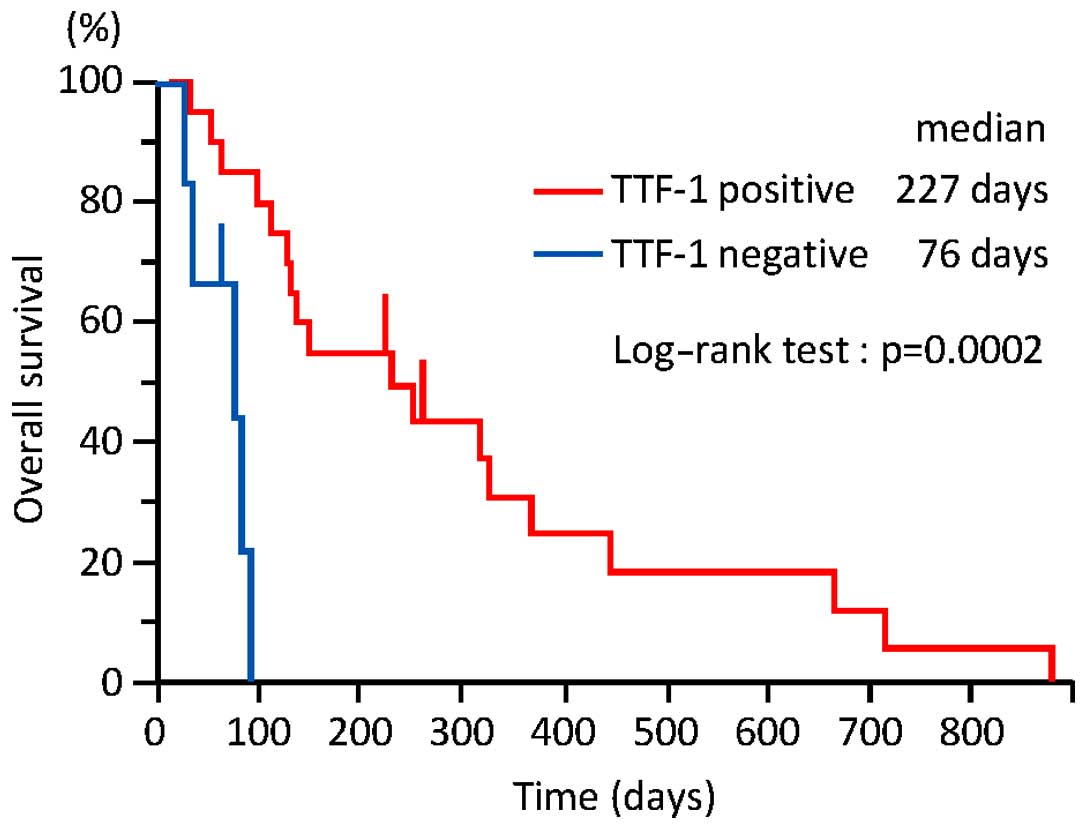
longer TTF (Table II). As shown in
Fig. 2, OS was significantly longer
in group A compared with that in group B (227 vs. 76 days; 95% CI:
110–366 vs. 26–90 days, respectively; P=0.0002). On univariate
analysis, only TTF-1 was a statistically significant predictor of
longer OS (Table III).
 | Table II.Time-to-treatment failure according to
patient characteristics (n=26). |
Table II.
Time-to-treatment failure according to
patient characteristics (n=26).
|
|
| Univariate
analysis |
|---|
|
|
|
|
|---|
| Characteristics | No. of patients
(%) | HR | 95% CI | P-value |
|---|
| Gender |
|
|
| 0.18 |
| Male | 12 (46) | 1.79 | 0.77–4.28 |
|
|
Female | 14 (54) |
|
|
|
| Age, years |
|
|
| 0.19 |
| ≥75 | 1 (4) | 5.79 | 0.30–39.15 |
|
|
<75 | 25 (96) |
|
|
|
| Smoking status |
|
|
| 0.12 |
|
Never | 8 (31) | 0.51 | 0.20–1.19 |
|
| Ever | 18 (69) |
|
|
|
| Prior
chemotherapy |
|
|
| 0.24a/0.24b |
| 1 | 4 (15) | 0.50a/0.42b |
0.12–1.51a |
|
| 2 | 17 (65) |
|
0.08–1.78b |
|
| ≥3 | 5 (19) |
|
|
|
| Performance
status |
|
|
| 0.95c/0.25d |
| 0 | 5 (19) | 1.03c/0.49d |
0.33–2.80c |
|
| 1 | 15 (58) |
|
0.14–1.66d |
|
| 2 | 6 (23) |
|
|
|
| TTF-1 |
|
|
| 0.03 |
|
Positive | 20 (77) | 0.30 | 0.11–0.88 |
|
|
Negative | 6 (23) |
|
|
|
 | Table III.Overall survival according to the
patient characteristics. |
Table III.
Overall survival according to the
patient characteristics.
|
|
| Univariate
analysis |
|---|
|
|
|
|
|---|
| Characteristics | No. of patients
(%) | HR | 95% CI | P-value |
|---|
| Gender |
|
|
| 0.73 |
| Male | 12 (46) | 0.86 | 0.35–2.01 |
|
|
Female | 14 (54) |
|
|
|
| Age, years |
|
|
| 0.09 |
| ≥75 | 1
(4) | 12.16 | 0.57–126.96 |
|
|
<75 | 25 (96) |
|
|
|
| Smoking staus |
|
|
| 0.62 |
|
Never | 8
(31) | 0.80 | 0.31–1.93 |
|
|
Ever | 18 (69) |
|
|
|
| Prior
chemotherapy |
|
|
| 0.09a/0.84b |
| 1 | 4
(15) | 0.38a/0.86b |
0.10–1.15a |
|
| 2 | 17 (65) |
|
0.19–4.40b |
|
| ≥3 | 5
(19) |
|
|
|
| Performance
status |
|
|
| 0.93a/0.88b |
| 0 | 5
(19) | 1.05c/0.90d |
0.33–2.80c |
|
| 1 | 15 (58) |
|
0.23–3.85d |
|
| 2 | 6
(23) |
|
|
|
| TTF-1 |
|
|
| 0.002 |
|
Positive | 20 (77) | 0.10 | 0.02–0.43 |
|
|
Negative | 6
(23) |
|
|
|
Post-erlotinib chemotherapy
As shown in Table IV,
11 (55%) patients in group A were treated with at least one
chemotherapeutic regimen after erlotinib therapy, whereas none of
the patients in group B received post-erlotinib therapy. The
proportion of patients who were treated with chemotherapy following
erlotinib was significantly higher in group A compared with group B
(P=0.0049).
 | Table IV.Post-erlotinib chemotherapy. |
Table IV.
Post-erlotinib chemotherapy.
|
| TTF-1
expression |
|---|
|
|
|
|---|
| Number of patients
receiving post-erlotinib chemotherapy | Positive
(n=20) | Negative (n=6) |
|---|
| 0 | 9 | 6 |
| 1 | 6 | 0 |
| 2 | 4 | 0 |
| 3 | 1 | 0 |
Discussion
The present findings demonstrated that TTF-1
expression is associated with a longer TTF and OS with erlotinib
therapy in patients with NS-NSCLC expressing wild-type EGFR. Thus,
TTF-1 expression may serve as a predictive biomarker of the
effectiveness of erlotinib monotherapy in such patients.
Mutations in EGFR are powerful predictive biomarkers
of the effectiveness of the EGFR-TKIs gefitinib, erlotinib and
afatinib. However, only a limited number of studies have evaluated
the effectiveness of erlotinib in NSCLC patients with wild-type
EGFR.
Shepherd et al reported that erlotinib
improved the OS of patients with previously treated unselected
advanced NSCLC. That study associated never having smoked with
longer progression-free survival (5).
Furthermore, the multivariate logistic regression analysis
significantly associated smoking status with tumor response in a
Japanese phase II study of the effects of erlotinib on previously
treated patients with unselected advanced NSCLC (8). However, these studies did not analyze
TTF-1. We herein demonstrated that TTF and OS tended to be longer
in patients who had never smoked compared with those who previously
or currently smoked, but the trend was not statistically
significant.
Several investigators have reported an association
between TTF-1 expression and the prognosis of NSCLC. A
meta-analysis identified TTF-1 as a good prognostic factor for
patients with NSCLC, with hazard ratios of 0.64 (95% CI: 0.41–1.00)
and 0.53 (95% CI: 0.29–0.95) for NSCLC and for a subgroup with
adenocarcinoma, respectively (9).
By contrast, others have recently reported an
association between TTF-1 expression and chemotherapeutic outcomes.
Grønberg et al associated TTF-1 positivity assessed by
immunohistochemistry with prolonged survival among patients with
NSCLC who participated in a phase III trial comparing pemetrexed
plus carboplatin with gemcitabine plus carboplatin as first-line
chemotherapy (10). Furthermore, Sun
et al analyzed data from patients with NS-NSCLC treated with
pemetrexed-based chemotherapy, and reported a significant
association of high TTF-1 protein expression with longer
progression-free survival and OS; they also reported that TTF-1
positivity is an independent predictive factor of the effectiveness
of EGFR-TKI therapy (11). A
significantly higher proportion of our TTF-1-positive patients were
further treated with chemotherapy after erlotinib, compared with
patients who were TTF-1-negative. Different responses to cytotoxic
chemotherapy, and not only to erlotinib, according to TTF-1
expression may have prolonged OS.
This retrospective study of a small patient cohort
has several limitations. The majority of the specimens were
obtained by transbronchial lung biopsy. In addition, we did not
compare the prognosis of patients who did not receive erlotinib
according to TTF-1 expression.
In conclusion, erlotinib alone is insufficient to
treat patients with previously treated NS-NSCLC expressing
wild-type EGFR. However, TTF-1 expression may be a useful tool for
predicting the effects of erlotinib in such patients. The present
results require confirmation in a large-scale prospective
study.
References
|
1
|
Maemondo M, Inoue A, Kobayashi K, Sugawara
S, Oizumi S, Isobe H, Gemma A, Harada M, Yoshizawa H, Kinoshita I,
et al: Gefitinib or chemotherapy for non-small-cell lung cancer
with mutated EGFR. N Engl J Med. 362:2380–2388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mitsudomi T, Morita S, Yatabe Y, Negoro S,
Okamoto I, Tsurutani J, Seto T, Satouchi M, Tada H, Hirashima T, et
al: Gefitinib versus cisplatin plus docetaxel in patients with
non-small-cell lung cancer harbouring mutations of the epidermal
growth factor receptor (WJTOG3405): An open label, randomised phase
3 trial. Lancet Oncol. 11:121–128. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhou C, Wu YL, Chen G, Feng J, Liu XQ,
Wang C, Zhang S, Wang J, Zhou S, Ren S, et al: Erlotinib versus
chemotherapy as first-line treatment for patients with advanced
EGFR mutation-positive non-small-cell lung cancer (OPTIMAL,
CTONG-0802): A multicentre, open-label, randomised, phase 3 study.
Lancet Oncol. 12:735–742. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rosell R, Carcereny E, Gervais R,
Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R,
Pallares C, Sanchez JM, et al: Erlotinib versus standard
chemotherapy as first-line treatment for European patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(EURTAC): A multicentre, open-label, randomised phase 3 trial.
Lancet Oncol. 13:239–246. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shepherd FA, Rodrigues Pereira J, Ciuleanu
T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S,
Smylie M, Martins R, et al: Erlotinib in previously treated
non-small-cell lung cancer. N Engl J Med. 353:123–132. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Myong NH: Thyroid transcription factor-1
(TTF-1) expression in human lung carcinomas: Its prognostic
implication and relationship with expressions of p53 and Ki-67
proteins. J Korean Med Sci. 18:494–500. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tan D, Li Q, Deeb G, Ramnath N, Slocum HK,
Brooks J, Cheney R, Wiseman S, Anderson T and Loewen G: Thyroid
transcription factor-1 expression prevalence and its clinical
implications in non-small cell lung cancer: A high-throughput
tissue microarray and immunohistochemistry study. Hum Pathol.
34:597–604. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kubota K, Nishiwaki Y, Tamura T, Nakagawa
K, Matsui K, Watanabe K, Hida T, Kawahara M, Katakami N, Takeda K,
et al: Efficacy and safety of erlotinib monotherapy for Japanese
patients with advanced non-small cell lung cancer: A phase II
study. J Thorac Oncol. 3:1439–1445. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Berghmans T, Paesmans M, Mascaux C, Martin
B, Meert AP, Haller A, Lafitte JJ and Sculier JP: Thyroid
transcription factor 1 - a new prognostic factor in lung cancer: A
meta-analysis. Ann Oncol. 17:1673–1676. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Grønberg BH, Lund-Iversen M, Strøm EH,
Brustugun OT and Scott H: Associations between, TS and TTF-1, FR-α,
FPGS, and overall survival in patients with advanced non-small-cell
lung cancer receiving pemetrexed plus carboplatin or gemcitabine
plus carboplatin as first-line chemotherapy. J Thorac Oncol.
8:1255–1264. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sun JM, Han J, Ahn JS, Park K and Ahn MJ:
Significance of thymidylate synthase and thyroid transcription
factor 1 expression in patients with nonsquamous non-small cell
lung cancer treated with pemetrexed-based chemotherapy. J Thorac
Oncol. 6:1392–1399. 2011. View Article : Google Scholar : PubMed/NCBI
|