Introduction
Partial nephrectomy (PN) is the most commonly used
procedure for the treatment of clinical stage T1a renal cancer.
Furthermore, evidence reveals that patients undergoing radical
nephrectomy have a higher overall mortality and cardiovascular
morbidity rate compared with those undergoing PN, even though their
effectiveness in cancer control is equivalent (1,2).
However, PN results in urinary fistula (UF) in 1–6%
of patients (3,4). The majority of these patients are forced
to undergo lengthy hospital stays, since perinephric drains cannot
be removed due to of persistent urine drainage. An effective
management strategy for UF remains to be established.
The present study reported two cases in which
selective artery embolization was useful for the treatment of UF
following PN.
Case reports
Case 1
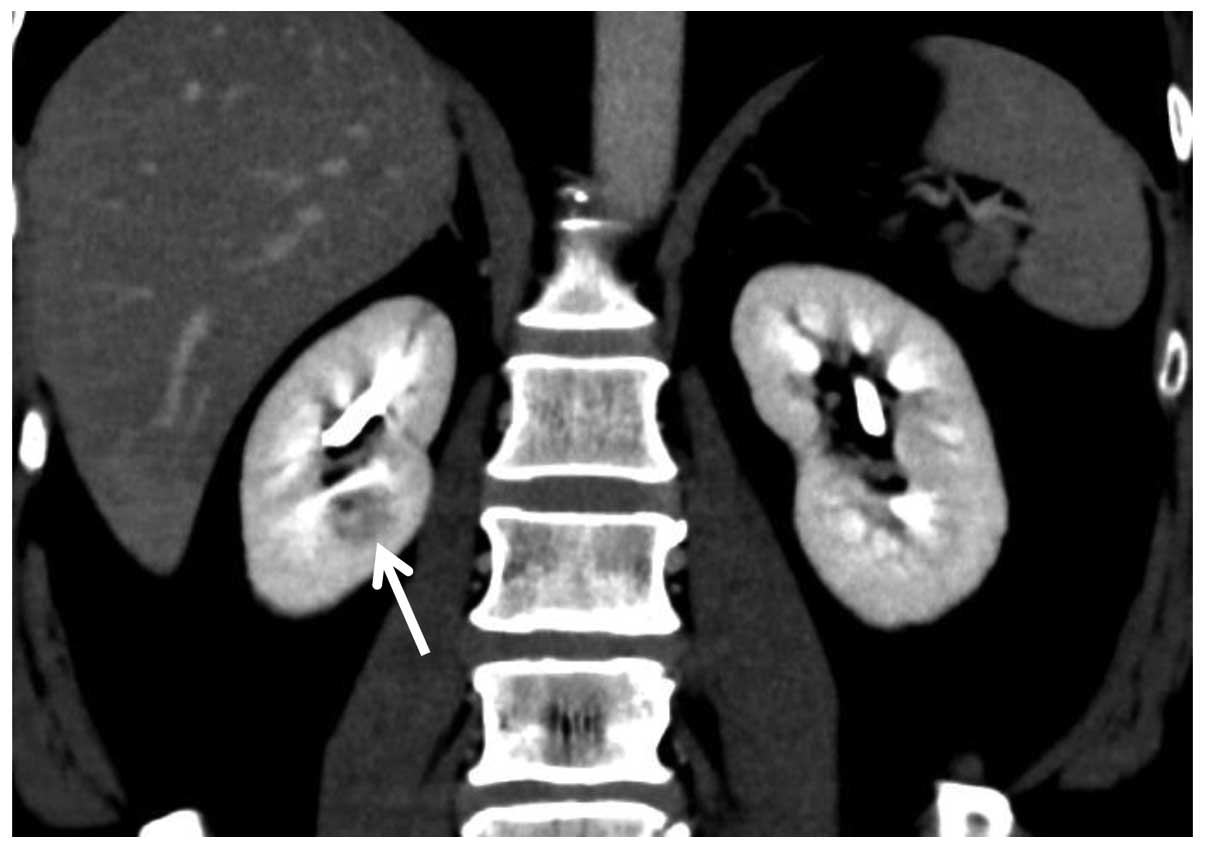
A 51-year-old male, diagnosed with renal cell
carcinoma (RCC) in the right kidney (Fig.
1), received mini-incision PN with renorrhaphy at Toyama
Prefectural Central Hospital (Toyama, Japan). Following the
operation, urine discharge of ~100 ml per day continued from the
retroperitoneal drain. Although ureteral stenting was performed at
post-operation day (POD) 6, the quantity of drainage did not
decrease. A computed tomography (CT) at POD 13 revealed urine
leakage in the upper part of the kidney. Furthermore, the upper
calyx was completely separated from the middle/lower calyx and the
renal pelvis. The upper calyx was not enlarged and it was
considered unlikely that percutaneous drainage could be
successfully performed. Since the UF could not be treated unless
effective urine drainage was obtained, it was unavoidable to
perform an alternative approach, including nephrectomy or
transarterial embolization (TAE) of the entire kidney. However, the
decision was made to perform selective TAE of the upper calyx at
POD 20. Following this procedure, urine output from the drain
stopped immediately. Although fever was observed for a few days,
the patient was able to leave Toyama Prefectural Central Hospital
at POD 29. The serum creatinine level was slightly increased (1.12
to 1.21 mg/dl). Since discharge, no further complications or RCC
recurrences have occurred for 3 years.
Case 2
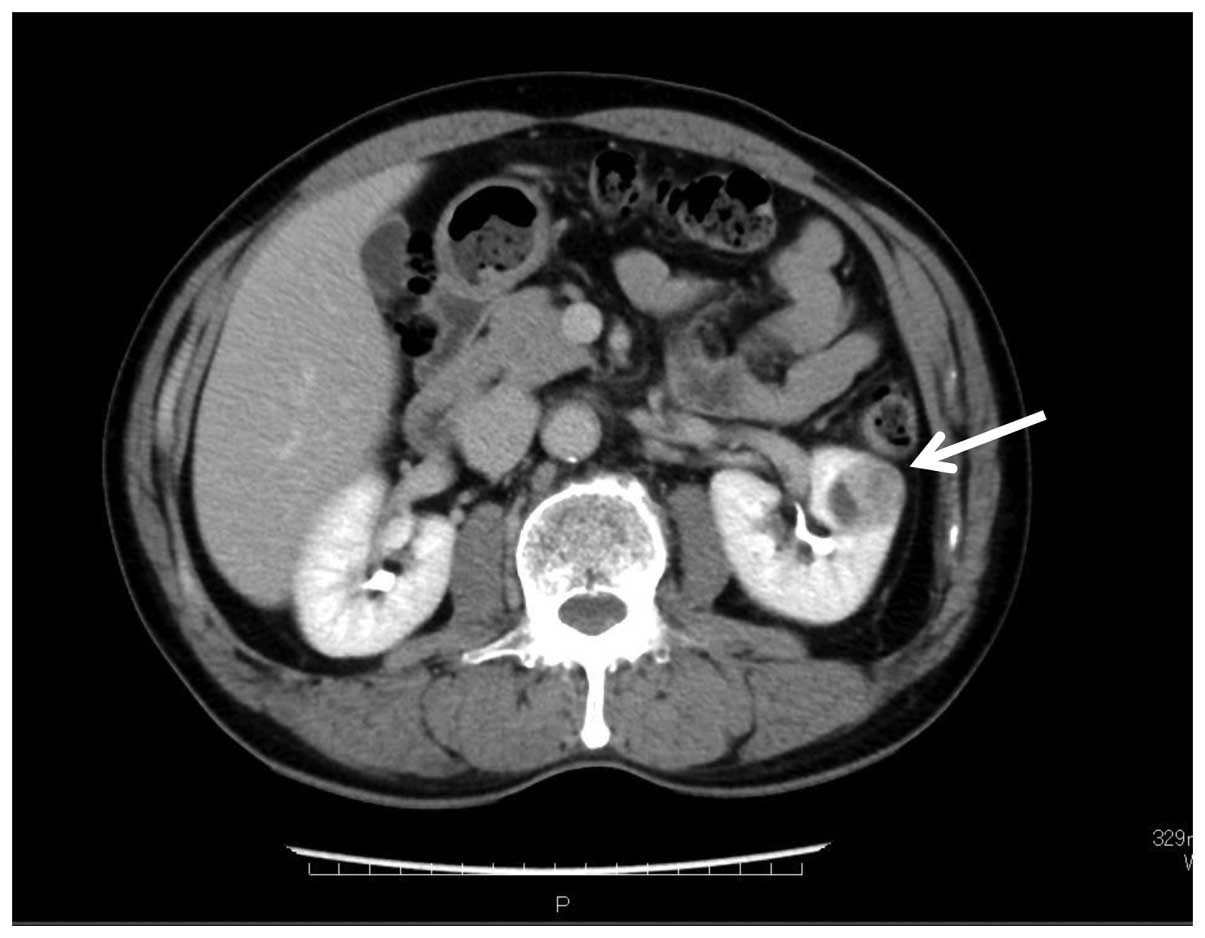
A 66-year-old male, with a diagnosis of RCC in the
left kidney (Fig. 2), received
mini-incision PN with renorrhaphy at Toyama Prefectural Central
Hospital. Following the operation, urine discharge of ~50–100 ml
per day continued from the retroperitoneal drain. Although ureteral
stenting was performed at POD 7, the quantity of drainage did not
decrease. A CT at POD 12 revealed urine leakage in an upper part of
the kidney. Furthermore, the upper calyx was completely separated
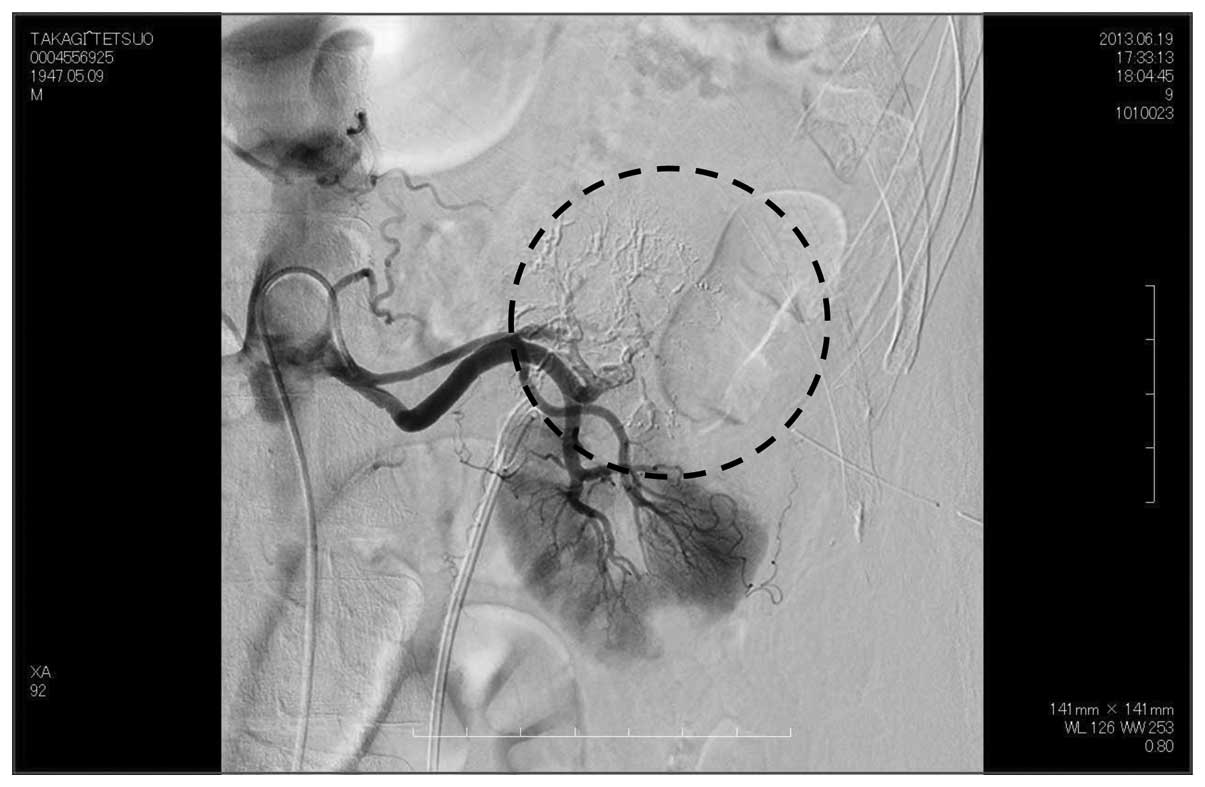
from the middle/lower calyx and the renal pelvis (Fig. 3), and it was slightly enlarged. This
suggested that percutaneous drainage would be difficult to achieve,
and therefore, we considered that selective TAE of the upper
section of the kidney, as previously described in case 1, may be
effective. This procedure was performed at POD 21 (Fig. 4) and resulted in the immediate
cessation of urine output from the drain. Although fever was
observed for a few days, the patient was able to leave Toyama
Prefectural Central Hospital on POD 26. The serum creatinine level
was slightly increased (0.99 to 1.06 mg/dl). Since discharge, no
complications and RCC recurrence have occurred for 2 years.
Discussion
Management of UF following PN can present serious
difficulties. Textbooks state that most UF cases will resolve with
several weeks of conservative therapy unless there is distal
obstruction to the site of leakage (5), and medical literature demonstrates that
many cases of UF are cured only by observation (3). Meeks et al (6) described 21 cases of UF, where a long
mean duration of leakage of 53 days was noted. This previous study
demonstrates that once UF occurs, patients are often confined to
hospital for lengthy time periods.
In the two cases described in the present study, the
upper calyx was completely separated from the middle/lower calyx,
and therefore, prevented successful drainage of the upper calyx. It
was suspected that deep suture of the renal parenchyma and/or the
collecting system during PN resulted in the upper calyx separating
from the renal pelvis in each case. For the treatment of UF,
nephrectomy or TAE of the entire kidney was considererd. However,
selective TAE was attempted in order to resolve UF and to preserve
renal function, and was successful in stopping urine discharge from
the retroperitoneal drain.
To the best of our knowledge, only 4 cases of
selective TAE in the treatment of UF have been previously reported
(7,8).
In one of these cases, urinary drainage persisted from the remnant
of the lower collecting system following hemi-nephrectomy of the
lower-half of a duplex kidney (7).
The other three cases involved horseshoe kidneys, which received
half-side nephrectomies with incisions of the isthmus, and urinary
drainage continued from the residual parenchyma that had originally
drained into the renal pelvis of the resected side (8). In all four cases, no drainage pathways
from the site of UF were observed and selective TAE was
successful.
Therefore, it was observed that UF is unable to
spontaneously resolve if good drainage pathways do not exist.
Finally, from the two cases presented in the present study, the
following was concluded: i) Suture of the collecting system and
renal parenchyma in PN may result in the separation of the renal
calyx from the renal pelvis; ii) Selective TAE of the renal
parenchyma in UF sites appeared to be a highly effective treatment
in such cases.
Glossary
Abbreviations
Abbreviations:
|
PN
|
partial nephrectomy
|
|
POD
|
post-operation day
|
|
RCC
|
renal cell carcinoma
|
|
TAE
|
transarterial embolization
|
|
UF
|
urinary fistula
|
References
|
1.
|
Thompson RH, Boorjian SA, Lohse CM,
Leibovich BC, Kwon ED, Cheville JC and Blute ML: Radical
nephrectomy for pT1a renal masses may be associated with decreased
overall survival compared with partial nephrectomy. J Urol.
179:468–471; discussion 472–473. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Huang WC, Elkin EB, Levey AS, Jang TL and
Russo P: Partial nephrectomy versus radical nephrectomy in patients
with small renal tumors-is there a difference in mortality and
cardiovascular outcomes? J Urol. 181:55–61; discussion 61–62. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Kundu SD, Thompson RH, Kallingal GJ,
Cambareri G and Russo P: Urinary fistulae after partial
nephrectomy. BJU Int. 106:1042–1044. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Minervini A, Vittori G, Antonelli A, Celia
A, Crivellaro S, Dente D, Di Santo V, Frea B, Gacci M, Gritti A, et
al: Open versus robotic-assisted partial nephrectomy: A multicenter
comparison study of perioperative results and complications. World
J Urol. 32:287–293. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Kavoussi LR, Schwartz MJ and Gill IS:
Laparoscopic surgery of the kidney. Kavoussi LR, Novick AC, Partin
AW and Peters CA: Campbell's Urology (10th). (Philadelphia).
Elsevier Saunders. 16682012.
|
|
6.
|
Meeks JJ, Zhao LC, Navai N, Perry KT Jr,
Nadler RB and Smith ND: Risk factors and management of urine leaks
after partial nephrectomy. J Urol. 180:2375–2378. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Mitty HA, Dan SJ, Goldman HJ and Glickman
SI: Urinary fistulas after partial nephrectomy: Treatment by
segmental renal embolization. AJR Am J Roentgenol. 141:101–103.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Stefani P, Selli C, Nicita G, Lapini A and
Dami A: Treatment of urinary fistulas after resection of horseshoe
kidneys by selective arterial embolization. Cardiovasc Intervent
Radiol. 12:18–21. 1989. View Article : Google Scholar : PubMed/NCBI
|