Introduction
Lymphoceles are an abnormal collection of lymphatic
fluid occurring following surgery. They can cause abdominal pain,
deep vein thrombosis or lower urinary tract problems (1). Incidence, for example following open
radical prostatectomy with pelvic lymph node dissection, varies in
the literature between 3 and 14% (2).
While treatment options encompass percutaneous aspiration with or
without instillation of sclerosing agents and laparoscopic
marsupialization, no standard is defined (1,3). Very few
papers have focussed on radiotherapy (RT) as an alternative
treatment option using different doses and techniques (4–7). The aim
of the present analysis was to evaluate outcome and toxicity of a
homogenous treatment schedule and modern technique for patients
with postoperative persistent lymphoceles in the setting of
malignant urological disease.
Case study
Following radical prostatectomy/cystectomy with
lymphadenectomy, 6 patients developed a pelvic lymphocele, which
persisted after percutaneous drainage. Each patient (seven
treatment volumes in total) was treated with external beam RT using
3D planned treatment with virtual simulation after planning CT.
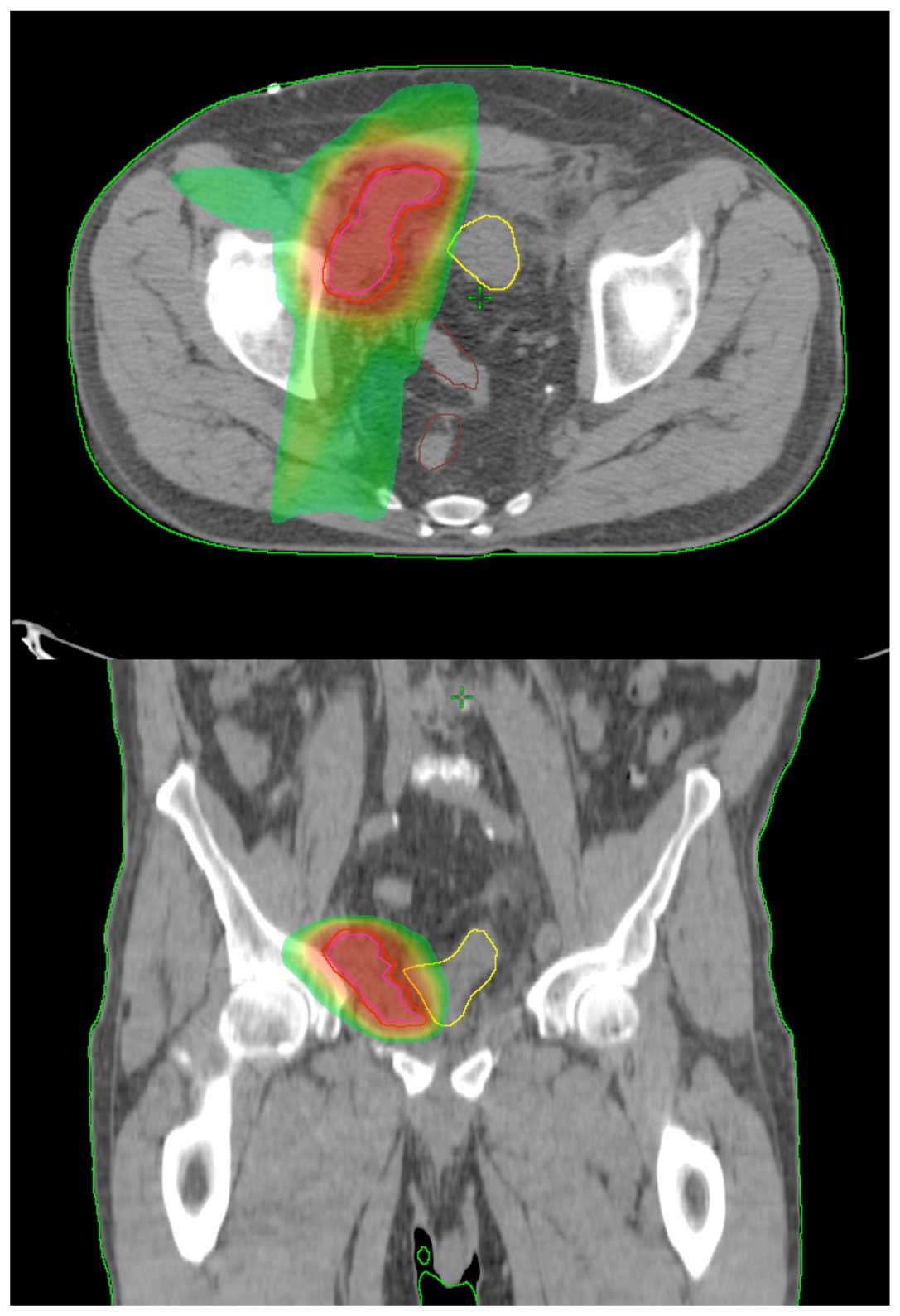
Clinical target volume (CTV) was contoured, including the entire
lymphocele with a margin of 1–2 cm, creating the planning target
volume (PTV). Photons of 6 and 18MV energy were selected and 3–5
coplanar fields were used (Fig. 1).
Of the patients, 1 patient was simultaneously irradiated to the
prostate bed (66 Gy; 2 Gy single dose). Patient and
treatment-associated parameters are summarized in Table I.
 | Table I.Patient and treatment-related
factors. |
Table I.
Patient and treatment-related
factors.
| Factor | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|
| Location | Left inguinal | Left inguinal | Left iliacal | Left and righ
iliacal | Right iliacal | Left inguinal |
| Gender | Male | Male | Male | Male | Male | Male |
| Age at RT | 61 | 75 | 71 | 79 | 70 | 69 |
| Tumor site | Prostate | Bladder | Prostate | Prostate | Prostate | Prostate |
| Interval
surgery-RT | 26 days | 4 months | 18 days | 25 days | 5 months | 3 months |
| Previous treatment
for lymphocele | Percutaneous
drainage | Percutaneous drainage
and slerotic agents | Percutaneous drainage
and doxicyclin | Percutaneous drainage
and slerotic agents | No previous
therapy | Percutaneous
drainage |
| Total/single
dose | 12/1 Gy | 12/1 Gy | 12/1 Gy | 10/1 Gy | 10/1 Gy | 10/1 Gy |
|
|
|
|
|
| In addition to RT to
prostate bed (66 Gy) |
| PTV (ml) | 69 ml | 172 ml | 57 ml | 119 and 88 ml | 114 ml | 76 ml |
| Toxicity | None | None | None | None | None | None |
| Follow up | 16 months | 20 months | 14 months | 24 months | 5 months | 47 months |
| Early response | 150 ml residuum (no
initial value), drainage drawn | 600 to 300 ml | 1,000 to 300 ml | 800 to 300 ml | 150 to 0 ml | Persistent (500
ml) |
| Late response | Resolved | Resolved | Resolved |
| Resolved | Secondary
marsupialization, now no symptoms |
No acute toxicities or chronic side effects were
observed. Of the 6 patients, 5 patients exhibited secretion of
lymph fluid, which was resolved after RT (Table I). In 4 patients, secretion was
already reduced during RT, while 1 patient responded time-delayed
without further therapy (8 weeks after RT) (Table I). In 1 patient, RT caused no effect,
making a marsupialization necessary. Following a mean follow-up of
21 months (range, 5–47 months), no patient suffered from any
symptoms concerning his former lymphoceles. All drainages could be
removed.
Discussion
Persistent lymphoceles are a common problem
following pelvic surgery, particularly when lymphadenectomy is
performed (3). Different approaches
exist for the treatment of persistent lymphoceles but no standard
is defined.
In previous literature, there are four studies
exclusively focusing on RT for persistent lymphoceles (4–6,8). From 1989–1998, Neu et al
(4) treated 29 patients after
vascular surgery with a single daily dose of 1 Gy up to 3–12 Gy.
The majority of patients were treated with electrons (7–18 MeV)
(4). Also, following vascular
surgery, Dietl et al (6)
treated 28 patients for inguinal lymphorrhea with single doses of
2–3 Gy up to 8–15 Gy. An orthovoltage of 120–300 KV energy was used
(6). The study group of Mayer et
al (5) treated patients with
fistulas after different, mostly vascular surgeries in different
localizations with orthovoltage or electrons in majority. The
single doses ranged from 0.3–2.0 Gy with total doses of 1–12 Gy
(5). Previously, Jereczek-Fossa et
al (8) showed RT after
prostatectomy in the presence of asymptomatic lymphoceles to be
feasible for integrating the lymphocele into the treatment plan of
the prostate fossa with maximum doses to the lymphoceles of
5.7–73.3 Gy (8). Taken together,
patient collectives of the above mentioned retrospective studies
are heterogenous in localization, treatment technique, single and
total doses, and primary surgery.
In the present study patients with urological
cancer, primarily prostate cancer, were treated for
inguinal/iliacal lymphoceles with a homogenous treatment schedule.
Contrasting to the other study groups, a more precise RT technique
was applied. Prior to the initiation of the treatment, a planning
CT was performed, on which the planning target volume (lymphocele)
was contoured. Afterwards a 3D treatment plan was generated. This
allowed a more precise and conformal dose coverage of the target
volume and sparing of the organs at risk compared with clinical
approaches. In line with this, no acute or late side effects were
observed.
The response rates (suspended secretion or removal
of drains) varied between 76 and 93% in the literature, and compare
well with the present findings (83%).
A limitation of the present retrospective case
series is without any doubt the small number of patients.
Nevertheless, in the absence of prospective studies, the present
case series is the first, to the best of our knowledge, to show the
effectiveness and safety of modern RT to persistent lymphoceles in
patients with urological cancer.
In conclusion, 3D conformal RT for persistent pelvic
lymphoceles in patients with urological cancer is effective and
very well-tolerated. Urological surgeons must be aware of this
treatment option, particularly following the failure of other
treatment modalities.
References
|
1
|
Raheem OA, Bazzi WM, Parsons JK and Kane
CJ: Management of pelvic lymphoceles following robot-assisted
laparoscopic radical prostatectomy. Urol Ann. 4:111–114. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Musch M, Klevecka V, Roggenbuck U and
Kroepfl D: Complications of pelvic lymphadenectomy in 1,380
patients undergoing radical retropubic prostatectomy between 1993
and 2006. J Urol. 179:923–928; discussion 928–929. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Anheuser P, Treiyer A, Stark E, Haben B
and Steffens JA: Lymphoceles after radical retropubic
prostatectomy. A treatment algorithm. Urologe. 49:832–836. 2010.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Neu B, Gauss G, Haase W, Dentz J and
Husfeldt KJ: Radiotherapy of lymphatic fistula and lymphocele.
Strahlenther Onkol. 176:9–15. 2000.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mayer R, Sminia P, McBride WH, Stranzl H,
Prettenhofer U, Fruhwirth J and Poschauko J: Lymphatic fistulas:
Obliteration by low-dose radiotherapy. Strahlenther Onkol.
181:660–664. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dietl B, Pfister K, Aufschläger C and
Kasprzak P: Radiotherapy of inguinal lymphorrhea after vascular
surgery. A retrospective analysis. Strahlenther Onkol. 181:396–400.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Radiotherapy in benign disorders.
Evidence-based guidelines of the German Association of
Radiooncologists. (DEGRO) Version 1.0. 2013.
|
|
8
|
Jereczek-Fossa BA, Colangione SP, Fodor C,
Russo S, Cambria R, Zerini D, Bonora M, Cecconi A, Vischioni B,
Vavassori A, et al: Radiotherapy in prostate cancer patients with
pelvic lymphocele after surgery: Clinical and dosimetric data of 30
patients. Clin Genitourin Cancer. 13:e223–e228. 2015. View Article : Google Scholar : PubMed/NCBI
|