Introduction
Due to an increasing number of cervical cancer cases
in young women and the postponement of childbearing in recent
decades, ~25% of patients with confirmed diagnosis of cervical
cancer are <40-year-old (1). As a
result, certain patients seek to preserve their fertility.
Therefore, the identification of a less radical approach that aims
to preserve the potential for fertility during the treatment of
patients with cervical carcinoma is crucial.
Since Dargent et al (2) performed the first vaginal radical
trachelectomy (RT) plus pelvic lymphadenectomy (PLAE) in 1987 to
preserve fertility in patients with early cervical cancer, RT via
the vagina (VRT) and the abdomen (ART), as well as laparoscopy
(LRT), have become widespread worldwide for the treatment of stage
Ib1 cervical cancer, in which the tumours are <2 cm. With this
approach, the full-term birth rate has been ~50% (2–5).
Neoadjuvant chemotherapy (NACT) can induce partial or complete
remission of the tumour, which makes it possible to broaden the
indications for the preservation of fertility or to perform more
conservative fertility-sparing surgeries to achieve improved
pregnancy outcomes. The present study reported a case of cervical
cancer of the International Federation of Gynecology and Obstetrics
(FIGO) stage IB2 in which the patient experienced pathological
complete regression (pCR) after NACT and underwent conization (CON)
plus laparoscopic pelvic and para-aortic lymphadenectomy.
Subsequently, this patient experienced a successful pregnancy and
gave birth after a 4-year follow-up period. Additionally, the
relevant literature is reviewed to discuss advancements in NACT and
fertility-sparing surgery in patients with cervical cancer.
Case report
Case data
A 31-year-old woman was admitted to Sun Yat-Sen
University Cancer Center (Guangzhou, China) in March 2010 with a
2-week history of vaginal bleeding following intercourse. The
patient got pregnant and had an induced abortion three times, and
had no child. A gynaecological physical examination revealed a
large cervical cauliflower-like lesion measuring 6×6 cm. A biopsy
confirmed the presence of moderately differentiated squamous cell
cervical carcinoma. The squamous cell carcinoma (SCC) antigen level
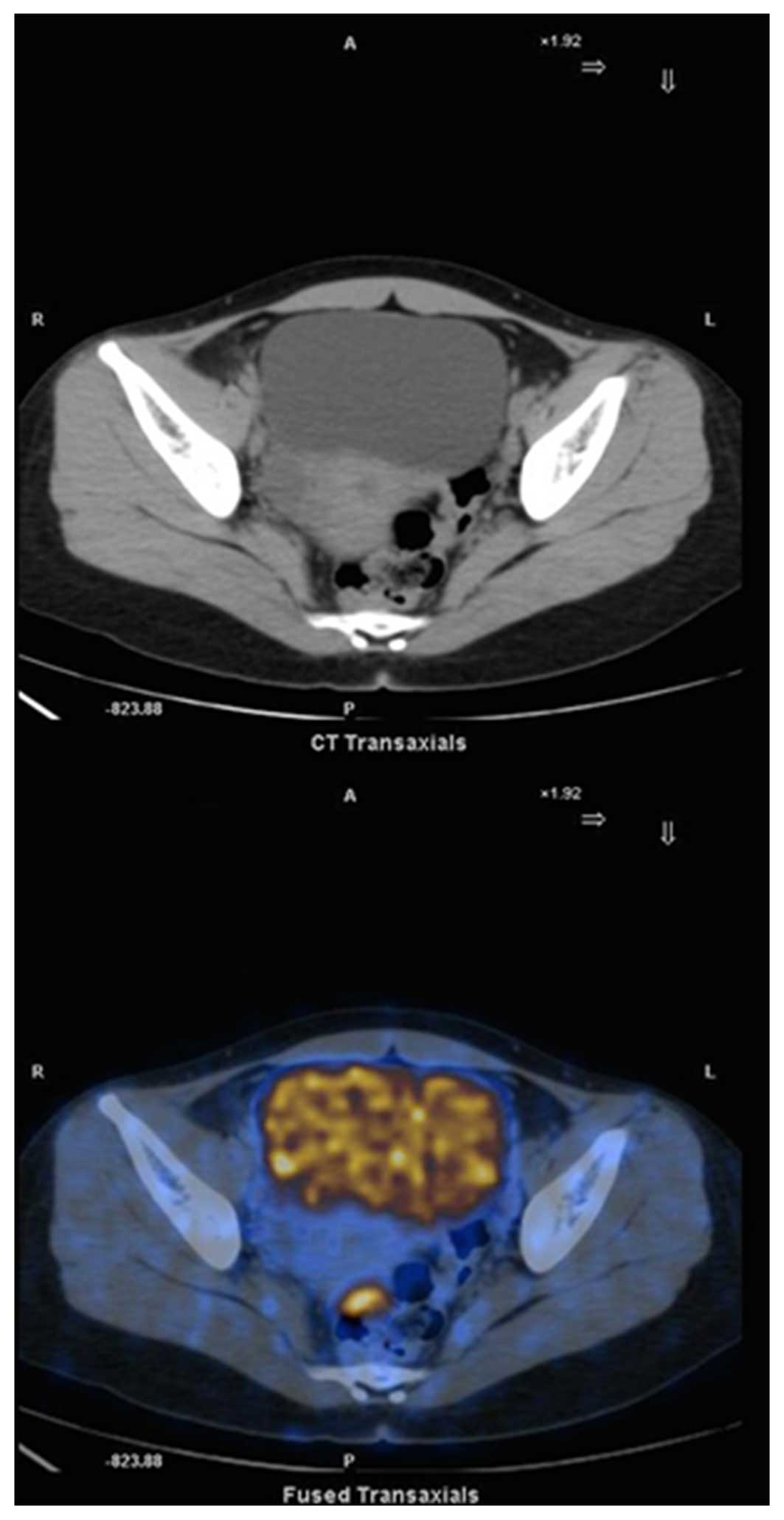
was 4.4 ng/ml (normal range, 0–1.5 ng/ml). A whole-body positron
emission tomography (PET)/computed tomography (CT) scan revealed a
cervical lesion measuring 4.2×6.3 cm with positivity for
fluorodeoxyglucose and slightly increasing radioactive uptake in
the bilateral iliac lymph nodes. Notably, the larger node was
~0.6×0.8 cm and suggested metastasis (Fig. 1). The patient was diagnosed as FIGO
stage IB2 squamous cervical cancer.
Treatment procedure
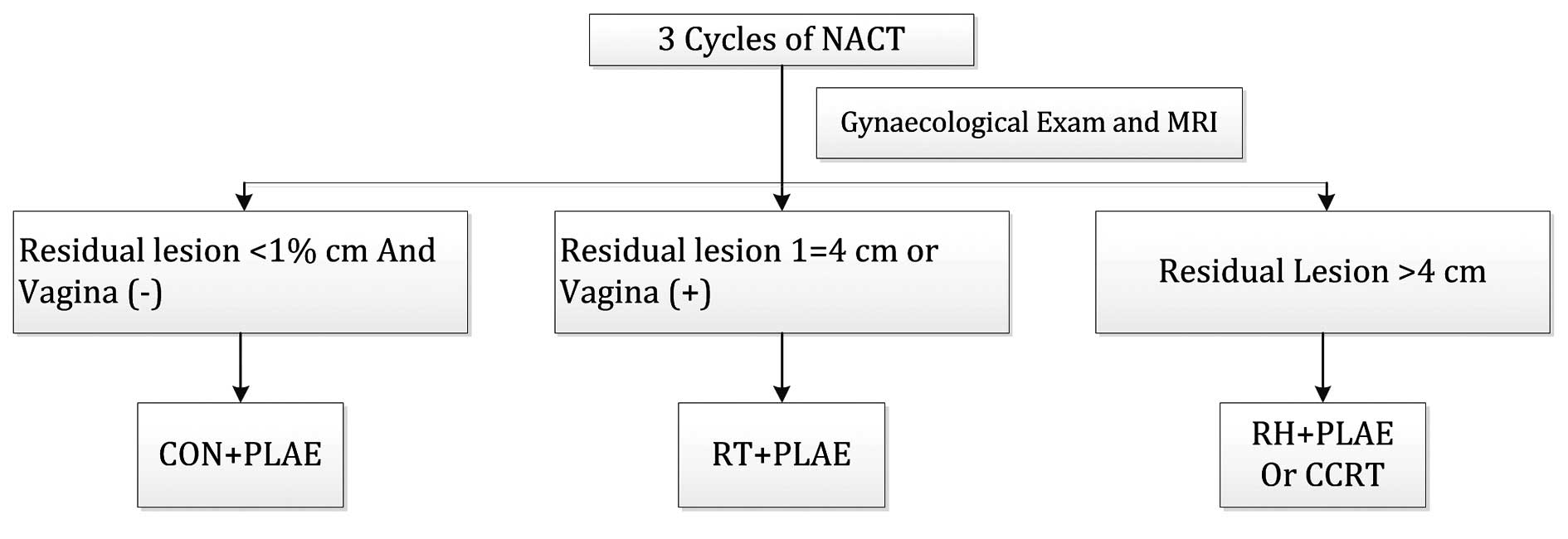
The patient was comprehensively counselled about the
available therapeutic options, including concurrent chemoradiation
or NACT followed by radical hysterectomy plus systematic pelvic
lymphadenectomy, or NACT followed by fertility-sparing surgery.
This nulliparous woman firmly wished to maintain her fertility
potential; therefore, the present study developed an individual
treatment plan following a multidisciplinary team discussion,
extensive counselling and the patient's signing of an informed
consent form (Fig. 2). If NACT was
applied first, any subsequent treatments would depend on the
patient's response to chemotherapy. This individual treatment plan
was approved by the Institutional Review Board of Sun Yat-sen
University Cancer Center.
The patient received three cycles NACT of TP
(paclitaxel 175 mg/m2 and cisplatin 75
mg/m2), which were repeated every 3 weeks. Before the
2nd cycle, the cervical lesion had become noticeably smaller and
measured 1.5×2.5 cm. In addition, the level of SCC antigen
decreased to 1.1 ng/ml (normal range, 0–1.5 ng/ml). The second and
third cycles were administered sequentially as a result of a good
chemotherapeutic response. A gynaecologic examination on the 26th
day after the third NACT treatment revealed no macroscopic residual
tumour in the cervix. The SCC level was 1.3 ng/ml at that time.
Magnetic resonance imaging indicated a slight contrast-enhanced
lesion of ~0.8×1.1 cm in the posterior cervical lip, however,
revealed no enlarged retroperitoneal lymphatic nodes (Fig. 3).
Following extensive discussion and counselling of
the patient, fertility-sparing surgery, which consisted of
conization plus laparoscopic pelvic and para-aortic
lymphadenectomy, was performed on June 13th 2010. First, a
large-sized sample from the posterior cervical lip was biopsied by
loop electrosurgical excision procedure (LEEP), and a laparoscopic
pelvic and para-aortic lymphadenectomy was performed. The cervical
biopsy and all lymph nodes were negative for tumour, according to
an analysis of frozen tissue sections. Next, deep cold-knife
conization was performed and a 3×2.5×2.5 cm piece of cervical
tissue was removed. Upon the final pathological analysis, all lymph
nodes were negative (0/24) and no residual dysplasia or invasive
cancer was observed in the two cervical specimens.
Though pathological complete regression (nodes and
cervix) showed after three cycles of NACT, this patient exhibited a
large size tumor (4.2×6.3 cm) and suspicious bilateral iliac lymph
nodes metastasis (0.6×0.8 cm) on PET/CT prior to treatment, and
radiotherapy was not considered following surgery. Chemotherapy
after surgery may assist with eliminating micrometastasis or
microresidual disease. The patient received another 3 cycles of TP
after surgery.
Emerging data suggested that administration of GnRH
agonists with chemotherapy may reduce the risk of ovarian failure
and improve prospects for fertility (6). Additionally, 3.6 mg Goserelin acetate
was administered by disposable syringe every 28 days during
chemotherapy to protect ovarian function. Menstruation resumed 5
months after the last cycle of chemotherapy.
With the exception of grade III neutropenia
occurring once after the first cycle of chemotherapy after surgery,
no other grade III or grade IV significant toxicities wer
observed.
The patient was followed-up closely every three
months in the first three years and every six months after that.
The patient was recommended to try for pregnancy 24 months
following surgery. The patient's last menstrual period (LMP)
occurred on February 28th 2014. A small volume of genital bleeding
occurred 40 days after her LMP. and an ultrasound and serum HCG
test both confirmed an intrauterine pregnancy. Premature rupture of
the membrane occurred at 27 weeks and 6 days, and the patient was
hospitalized to receive treatments to prevent preterm delivery and
promote foetal lung maturation. As a result of a suspicious
intrauterine infection and early deceleration in the fetal heart
rate monitoring, caesarean section was performed at 29 weeks of
gestation. The immature baby was born weighing 1,460 g and had
Apgar scores of 10 at 1 and 5 min. The infant remained under
observation in the neonatal department for 40 days and was
discharged from the hospital when deemed healthy. At 60 months
after the surgery, the patient was living without the disease and
her child was healthy.
It was >4 years since the fertility-sparing
surgery when the patient delivered the baby, and no sign of
recurrent disease was observed; therefore, radical hysterectomy was
not performed following delivery.
The patient exhibited no recurrent disease until May
2016 (72 months after surgery).
Discussion
The goal of fertility-sparing treatment in early
cervical cancer is to achieve improved pregnancy outcomes without
negatively impacting prognosis. Therefore, the therapeutic effects
of fertility-preserving treatment for cervical cancer consist of
two aspects: i) Oncologic outcomes (e.g. recurrence rate, overall
survival rate, surgery or chemotherapy complications), and ii)
pregnancy and obstetrical outcomes (e.g., pregnancy rate, abortion
rate, premature birth rate, full-term birth rate).
VRT, ART and LRT, plus pelvic lymph node dissection,
is the classic fertility-sparing surgery approach that has been
used worldwide in patients with early-stage cervical cancer,
particularly in those patients with stage Ib1 disease whose tumours
are <2 cm in diameter. VRT was the earliest procedure that was
used in clinical practice and >900 women have benefited from VRT
since the use of this type of surgery was first reported in 1994
(2). The results from the reports of
larger sample sizes have demonstrated that the rate of successful
pregnancy is 65.8%, whereas the full-term delivery rate ranged
between 45 and 75%. The recurrence rate ranged between 3.8 and
4.8%, and the death rate ranged between 1.6 and 1.9% (3,7,8). A systematic analysis, including 29
articles with a total of 485 patients who underwent ART, revealed
the following: A recurrence rate of 3.8%, a death rate of 0.4%, a
successful pregnancy rate of 59.3% and a full-term delivery rate of
46.7% (35/75). Additionally, 10 pregnancies were on-going at the
time of the published reports (4).
With the advantages of few effects to the abdominal organs and a
quick postoperative recovery, LRT is more widely used in
conjunction with laparoscopic surgery. One Asian Gynecologic Cancer
Group study that included 79 patients who underwent LRT, reported a
median follow-up time of 44 months (range, 3–105 months). In that
previous study, 9 patients experienced recurrence and one succumbed
to the disease. A tumour size >2 cm (P=0.039) and an invasion of
>1/2 the depth of the cervical stroma (P=0.016) were significant
risk factors for recurrence. Among these patients, 13 achieved a
total of 17 successful pregnancies and gave birth to 13 healthy
infants, including 7 preterm infants and 6 full-term infants
(5). Challenges remain and continued
research to develop improved fertility-sparing treatment with less
extensive surgery is required.
Previous studies have reported that in patients with
early stage cervical carcinoma who have tumours <2 cm in
diameter, an infiltration depth of <10 mm or of <1/2 the
depth of the cervical stroma, negative pelvic lymph nodes and
absent lymph vascular space invasion (LVSI), the risk of
parametrial involvement was <1% (0 and 0.63%, respectively)
(9,10). Simple extrafascial trachelectomy or
conization, plus pelvic lymphadenectomy with or without sentinel
lymph node detection, has been proposed as a fertility-sparing
surgical approach for selected and informed patients with low-risk
stage IB1 cervical cancer (11,12).
NACT is a feasible option for patients with locally
advanced cervical cancer, since it exhibits a good response rate
that ranges between 78 and 95%. Furthermore, the pCR range betwen
10.3 and 19% (13,14). NACT represents a novel model of
fertility preservation for young patients with cervical cancer
(Table I). The potential effects of
NACT are a reduction in tumour volume, an increased possibility of
obtaining wider uninvolved surgical margins, and a reduction in the
risk of parametrial involvement and LVSI. NACT may allow a greater
number of patients to meet the criteria for fertility-sparing
surgery to be treated using this option. Furthermore, NACT also
allows for a possible decrease in the extent of surgery to preserve
some cervical tissue to achieve an improved pregnancy outcome.
Marchiole et al (15), Tsuji
et al (16) and Lanowska et
al (17) reported that 28
patients whose tumours were >2 cm or who had chemosensitive
bulky disease received NACT, followed by fertility-sparing surgery,
which consisted of RT and lymphadenectomy. Of these cases, one
developed recurrent disease. Palaia et al (18), Tsubamoto et al (19) and Robova et al (20) have reported further progress in
fertility-sparing management using NACT, followed by the less
extensive surgical approach of simple vaginal trachelectomy and
pelvic lymphadenectomy. This method was used in patients who
desired fertility preservation, but did not fulfil the standard
criteria for fertility-sparing surgery (tumours >2 cm or with
deep infiltration of more than half of the stroma). Maneo et
al (21) first proposed
chemo-conization as an alternative to fertility-sparing treatment.
This approach can further reduce the extent of surgery, preserve a
greater amount of cervical tissue and is associated with improved
pregnancy outcomes since it decreases the incidence of miscarriage
in the second trimester, premature rupture of membranes and preterm
delivery often occurs after RT. This treatment approach was
demonstrated to be feasible by Landoni et al (22) and Maneo et al (23), who reported 2 and 16 cases of stage
IB1 cervical cancer, respectively. The patients in those previous
studies were treated with NACT, followed by cold-knife conization
and pelvic lymphadenectomy if the frozen tissue sections of the
residual lesions revealed an infiltration depth of 3 mm or less.
Following a median of 20 and 69 months of follow-up, respectively,
no recurrences occurred and all patients achieved successful
pregnancy outcomes.
 | Table I.Summary of neoadjuvant chemotherapy
and fertility-sparing surgery for cervical cancer. |
Table I.
Summary of neoadjuvant chemotherapy
and fertility-sparing surgery for cervical cancer.
| Author, year | No. of patients | Stage | Tumour size (cm) | Chemotherapy
(frequency and cycles) | Surgery | Follow-up
(months) | Oncological
outcome | Obstetric
outcome | Refs. |
|---|
| Palaia et al,
2011 | 1 | IB2 | NA | TIP (every 3 weeks, 3
cycles) | VST + PLAE | 36 | No recurrence | No intention to
become pregnant. | 17 |
| Marchiole et
al, 2011 | 7 | IB-IIA1 | 3.0–4.5 | TIP (every 3 weeks,
3–4 cycles) | VRT + PLAE | 22 | No recurrence | One women attempted
to conceive and delivered a healthy baby at 17 weeks. | 14 |
| Tsuji et al,
2012 | 1 | IB2 | NA | DDP + MMC (IA.)
(every 3 weeks, 2 cycles) | ART + PLAE | 64 | No recurrence | Premature membrane
ruptured after 27 weeks and delivered at 28 weeks. | 15 |
| Lanowska et
al, 2014 | 20 | NA | 2.1–5 | TIP (every 3 weeks,
2–3 cycles) | VRT + PLAE | 23 | One case of
recurrence | Seven women attempted
to conceive. Seven pregnancies were noted in five women, and four
children were born, two of whom were premature (31 weeks 2 days and
33 weeks 4 days of gestation). One pregnancy is ongoing. | 16 |
| Tsubamot et
al, 2012 | 12 | IB1 | >3 cm | DDP. IA + nedaplatin
IV (every 3 weeks, 3 cycels). DDP. IA + irinotecan IV (every 3
weeks, 3 cycles) | VST + PLAE | 65, 86 and 120 | No recurrence | No intention to
become pregnant. | 18 |
|
|
| IB2 |
|
| Robova et al,
2014 | 21 | IB1 | >2 cm | DDP + ifosfamide
(SCC) or Doxorubicin (ACC) (every 10–14 days, 3 cycles) | VST + PLAE (8–10 mm
of cervical stroma was preserved) | Median, 42 | Four women
experienced recurrence after fertility-sparing surgery and two
succumbed to the disease. | 20 had spared
fertility and 10 became pregnant (50%). Eight women delivered 10
babies (6 full-term and 4 preterm); 2 miscarried in the second
trimester (one woman) and 1 miscarried in the first trimester. | 19 |
|
| 7 | IB2 |
|
| Landoni et al,
2007 | 8 | IB1 | <3 cm | TEP (ACC) or TIP
(SCC) (every 3 weeks, 3 cycles) (patients with a tumour diameter of
more than 2 cm and less than 3 cm) | CKC + PLAE | 20 | No recurrence | Three pregnancies,
each resulted in full-term pregnancies and healthy babies. | 21 |
|
| 3 | IA2 |
|
| Maneo et al,
2008 | 16 | NA | 1–3 cm | TIP (every 3 weeks, 3
cycles) | CKC + PLAE | 69 | No recurrence | Nine women attempted
to conceive and 10 pregnancies occurred in six patients. Nine
babies were delivered. One woman experienced a first-trimester
miscarriage. | 22 |
Vercellino et al (24) proposed another treatment plan option
that performing laparoscopic node assessment prior to NACT to rule
out node positive patients (24). In
their cohort of cases, the pelvic and/or para-aortic lymph nodes
metastasis rate (67%, 12/18) were much higher compared with those
in other reports of early stage cervical cancer. According to the
present treatment plan, CT, MRI or PET/CT was used to rule out
patients with lymph nodes metastasis. If no obvious lymph nodes
metastasis are observed, it is preferred that NACT is used first,
due to chemotherapy resulting in the best effect when the
retroperitoneal space is untouched. Li et al (25) put forward the argument that adjuvant
chemotherapy alone after surgery does not sacrificed the survival
outcome, even in the group of patients with high risk factors after
surgery, compared with adjuvant radiotherapy. Additionally, no
positive lymph nodes were identified after surgery in the present
case. It was inferred that it would be safe to have adjuvant
chemotherapy alone after surgery for this patient who had small
size suspicious pelvic lymph nodes on PET/CT prior to surgery.
The patient with stage IB2 squamous cell cervical
carcinoma (tumor diameter, 6 cm) in the present sreport exhibited a
good response to NACT, and no macroscopic lesions or residual
tumour were detected after three cycles of NACT treatment. Since
pCR was determined by examination of frozen tissue sections after
biopsy by LEEP and pelvic lymph node dissection, the patient
ultimately underwent deep cervical conization to preserve fertility
function. During long-term follow-up, the patient remained
recurrence-free and achieved a successful pregnancy through the
third trimester. The patient gave birth to a healthy baby at 29
weeks.
Currently, few studies have reviewed
fertility-sparing treatments with NACT, followed by conservative
surgery, for patients with cervical cancer. The present report
suggested that it may be possible for more patients to preserve
their fertility through careful evaluation of an optimal response
to NACT and through individualized fertility-sparing approaches and
surgery. Additionally, it may also be possible for patients to
experience improved pregnancy and obstetrical outcomes without a
concomitant sacrifice of oncologic outcomes even in cases of
locally advanced cervical cancer.
Although the present results are preliminary and
await further supporting data, these results, together with those
of published articles, offer a new perspective for the management
of early cervical cancer in young women who seek to preserve their
fertility.
References
|
1
|
Howlader N, Noone AM, Krapcho M, Garshell
J, Miller D, Altekruse SF, et al: SEER Cancer Statistics Review,
1975-2011. National Cancer Institute; Bethesda, MD: http://seer.cancer.gov/csr/1975_2011/Based on
November SEER data submission. Accessed. April 30–2014
|
|
2
|
Dargent D, Martin X, Sacchetoni A and
Mathevet P: Laparoscopic vaginal radical trachelectomy: A treatment
to preserve the fertility of cervical carcinoma patients. Cancer.
88:1877–1882. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Plante M, Gregoire J, Renaud MC and Roy M:
The vaginal radical trachelectomy: An update of a series of 125
cases and 106 pregnancies. Gynecol Oncol. 121:290–297. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pareja R, Rendón GJ, Sanz-Lomana CM,
Monzón O and Ramirez PT: Surgical, oncological, and obstetrical
outcomes after abdominal radical trachelectomy-a systematic
literature review. Gynecol Oncol. 131:77–82. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park JY, Joo WD, Chang SJ, Kim DY, Kim JH,
Kim YM, Kim YT and Nam JH: Long-term outcomes after
fertility-sparing laparoscopic radical trachelectomy in young women
with early-stage cervical cancer: An Asan gynecologic cancer group
(AGCG) study. J Surg Oncol. 110:252–257. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moore HC, Unger JM and Albain KS: Ovarian
protection during adjuvant chemotherapy. N Engl J Med.
372:2269–2270. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Speiser D, Mangler M, Köhler C, Hasenbein
K, Hertel H, Chiantera V, Gottschalk E and Lanowska M: Fertility
outcome after radical vaginal trachelectomy: A prospective study of
212 patients. Int J Gynecol Cancer. 21:1635–1639. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lanowska M, Mangler M, Spek A, Grittner U,
Hasenbein K, Chiantera V, Hertel H, Schneider A, Köhler C and
Speiser D: Radical vaginal trachelectomy (RVT) combined with
laparoscopic lymphadenectomy: Prospective study of 225 patients
with early-stage cervical cancer. Int J Gynecol Cancer.
21:1458–1464. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Stegeman M, Louwen M, van der Velden J,
ten Kate FJ, den Bakker MA, Burger CW and Ansink AC: The incidence
of parametrial tumor involvement in select patients with early
cervix cancer is too low to justify parametrectomy. Gynecol Oncol.
105:475–480. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Frumovitz M, Sun CC, Schmeler KM, Deavers
MT Dos, Reis R, Levenback CF and Ramirez PT: Parametrial
involvement in radical hysterectomy specimens for women with
early-stage cervical cancer. Obstet Gynecol. 114:93–99. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Palaia I, Musella A, Bellati F, Marchetti
C, Di Donato V, Perniola G and Benedetti Panici P: Simple
extrafascial trachelectomy and pelvic bilateral lymphadenectomy in
early stage cervical cancer. Gynecol Oncol. 126:78–81. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fagotti A, Gagliardi ML, Moruzzi C, Carone
V, Scambia G and Fanfani F: Excisional cone as fertility-sparing
treatment in early-stage cervical cancer. Fertil Steril.
95:1109–1112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu T, Li S, Chen Y, Shen J, Li X, Huang K,
Yang R, Wu L, Chen Z, Jia Y, et al: Matched-case comparison of
neoadjuvant chemotherapy in patients with FIGO stage IB1-IIB
cervical cancer to establish selection criteria. Eur J Cancer.
48:2353–2360. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wan T, Huang H, Liu JH, Li Z and Feng YL:
Response to neoadjuvant chemotherapy on locally advanced cervical
cancer and long-term follow-up outcome. Zhonghua Yi Xue Za Zhi.
90:3045–3048. 2010.PubMed/NCBI
|
|
15
|
Marchiole P, Tigaud JD, Costantini S,
Mammoliti S, Buenerd A, Moran E and Mathevet P: Neoadjuvant
chemotherapy and vaginal radical trachelectomy for
fertility-sparing treatment in women affected by cervical cancer
(FIGO stage IB-IIA1). Gynecol Oncol. 122:484–490. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tsuji N, Butsuhara Y, Yoshikawa H,
Terakawa K and Nagano T: Pregnancy after neoadjuvant chemotherapy
followed by abdominal radical trachelectomy in stage IB2 cervical
cancer: A case report. Gynecol Oncol Case Rep. 4:13–15. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lanowska M, Mangler M, Speiser D,
Bockholdt C, Schneider A, Köhler C, Vasiljeva J, Al-Hakeem M and
Vercellino GF: Radical vaginal trachelectomy after laparoscopic
staging and neoadjuvant chemotherapy in women with early-stage
cervical cancer over 2 cm: Oncologic, fertility, and neonatal
outcome in a series of 20 patients. Int J Gynecol Cancer.
24:586–593. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Palaia I, Musella A, Loprete E, Achilli C,
Perniola G and Panici PB: Neoadjuvant chemotherapy plus
fertility-sparing surgery in locally advanced cervical cancer: Case
report. J Minim Invasive Gynecol. 18:121–122. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tsubamoto H, Kanazawa R, Inoue K, Ito Y,
Komori S, Maeda H and Hirota S: Fertility-sparing management for
bulky cervical cancer using neoadjuvant transuterine arterial
chemotherapy followed by vaginal trachelectomy. Int J Gynecol
Cancer. 22:1057–1062. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Robova H, Halaska MJ, Pluta M, Skapa P,
Matecha J, Lisy J and Rob L: Oncological and pregnancy outcomes
after high-dose density neoadjuvant chemotherapy and
fertility-sparing surgery in cervical cancer. Gynecol Oncol.
135:213–216. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Maneo A: Chemo-conization: A more
conservative approach. In: Presented at the annual meeting of the
international gynecologic cancer society; 2004;
|
|
22
|
Landoni F, Parma G, Peiretti M, Zanagnolo
V, Sideri M, Colombo N and Maggioni A: Chemo-conization in early
cervical cancer. Gynecol Oncol. 107(1): Suppl 1. S125–S126. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Maneo A, Chiari S, Bonazzi C and Mangioni
C: Neoadjuvant chemotherapy and conservative surgery for stage IB1
cervical cancer. Gynecol Oncol. 111:438–443. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vercellino GF, Piek JM, Schneider A,
Köhler C, Mangler M, Speiser D and Chiantera V: Laparoscopic lymph
node dissection should be performed before fertility preserving
treatment of patients with cervical cancer. Gynecol Oncol.
126:325–329. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li S, Hu T, Chen Y, Zhou H, Li X, Cheng X,
Yang R, Wang S, Xie X and Ma D: Adjuvant chemotherapy, a valuable
alternative option in selected patients with cervical cancer. PLoS
One. 8:e738372013. View Article : Google Scholar : PubMed/NCBI
|