Introduction
Malignant pleural mesothelioma (MPM) is a high-grade
malignancy of the chest that develops from mesothelial cells of the
serosal membranes. The incidence of MPM is low and differs among
different countries worldwide, from 7/million inhabitants in Japan
to 40/million inhabitants in Australia annually (1). MPM is closely associated with a history
of asbestos exposure. The major clinical manifestations of MPM are
pleural effusion, chest pain, dyspnea and emaciation. If the
kidneys are invaded, the patients may present with anasarca and/or
renal insufficiency. However, the clinical manifestations of MPM
are usually non-specific and insidious and should not be used alone
as diagnostic criteria. The diagnosis of MPM should be based on
immunohistochemical examination of the pleural tissue. The specific
and sensitive positive markers include anti-calretinin (CR),
anti-epithelial membrane antigen, anti-cytokeratin (CK) 5/6,
anti-D2-40 (podoplanin), anti-mesothelin and, particularly,
anti-Wilms tumour antigen-1. Other makers are of negative
diagnostic value, including anti-Ber-EP4, anti-thyroid
transcription factor-1 (TTF-1) and monoclonal anti-carcinoembryonic
antigen (CEA) (1). The concept of
paraneoplastic glomerulopathy was introduced by Galloway in 1922.
Moreover, nephrotic syndrome secondary to malignant pleural
mesothelioma is rarely reported. We herein report the case of a
young man with a pleural mesothelial malignancy presenting
subsequent to the manifestation of membranous nephropathy.
Case report
A 23-year-old man was admitted to our hospital on
September 5, 2014. The chief complaint was edema of the lower limbs
for 4 years, abdominal pain for 7 months and chest oppression for 5
months. The patient first noticed edema in the lower limbs 4 years
prior and visited a local hospital. The laboratory data revealed
positive urine protein (10.39 g/day) and hypoalbuminemia (serum
albumin 15 g/l) and the patient was diagnosed with nephrotic
syndrome. The renal biopsy confirmed the diagnosis of membranous
nephropathy. Prednisone was administered (60 mg/day and gradually
reduced). However, the patient reported that the edema reappeared
several times. In addition, abdominal pain developed 7 months prior
to admission. Laboratory examinations revealed a 24-h urine total
protein of 5.28 g and a serum albumin level of 21 g/l. Thrombosis
of the portal, splenic, superior mesenteric and renal veins and the
inferior vena cava was identified on computed tomography (CT) and
ultrasound scans performed in the local hospital. The patient
underwent inferior vena cava filter implantation and infusion
catheter-directed thrombolysis, and was initiated on tacrolimus (1
mg, twice per day). The pain was relieved and urine protein
fluctuated between 0.68 and 13.6 g/day. The patient had poor
appetite with a feeling of chest oppression that had developed 5
months prior and he was referred to our hospital. Physical
examination revealed weakness and malnutrition. On palpation of the
lymph nodes, the cervical and supraclavicular lymph nodes were
found to be enlarged. The examination of the abdomen revealed
distention and shifting dullness. In addition, there was edema of
the lower limbs.
Laboratory results
The laboratory values were as follows: hemoglobin 73
g/l, 24-h urine total protein 13.6 g, serum creatinine 88 µmol/l,
albumin 16.9 g/l, total cholesterol 6.9 mmol/l and triglycerides
2.17 mmol/l. The cancer antigen 125 level was 4,190 U/ml. The
anti-phospholipase A2 receptor (PLA2R) antibody was negative.
pneumonia and massive bilateral pleural effusion were identified on
CT, whereas positron emission tomography-CT positron emission
tomography-CT revealed enlarged lymph nodes with high uptake in the
bilateral supraclavicular, peristernal, diaphragmatic, abdominal
and retroperitoneal regions. Several areas of nodular pleural
thickening and mass-like peritoneal thickening exhibiting high
uptake were also observed. These are generally considered to be
signs of inflammation, although they may occasionally indicate
malignant tumors. Thus, lymph node biopsy was performed and
revealed malignant cell invasion or metastasis.
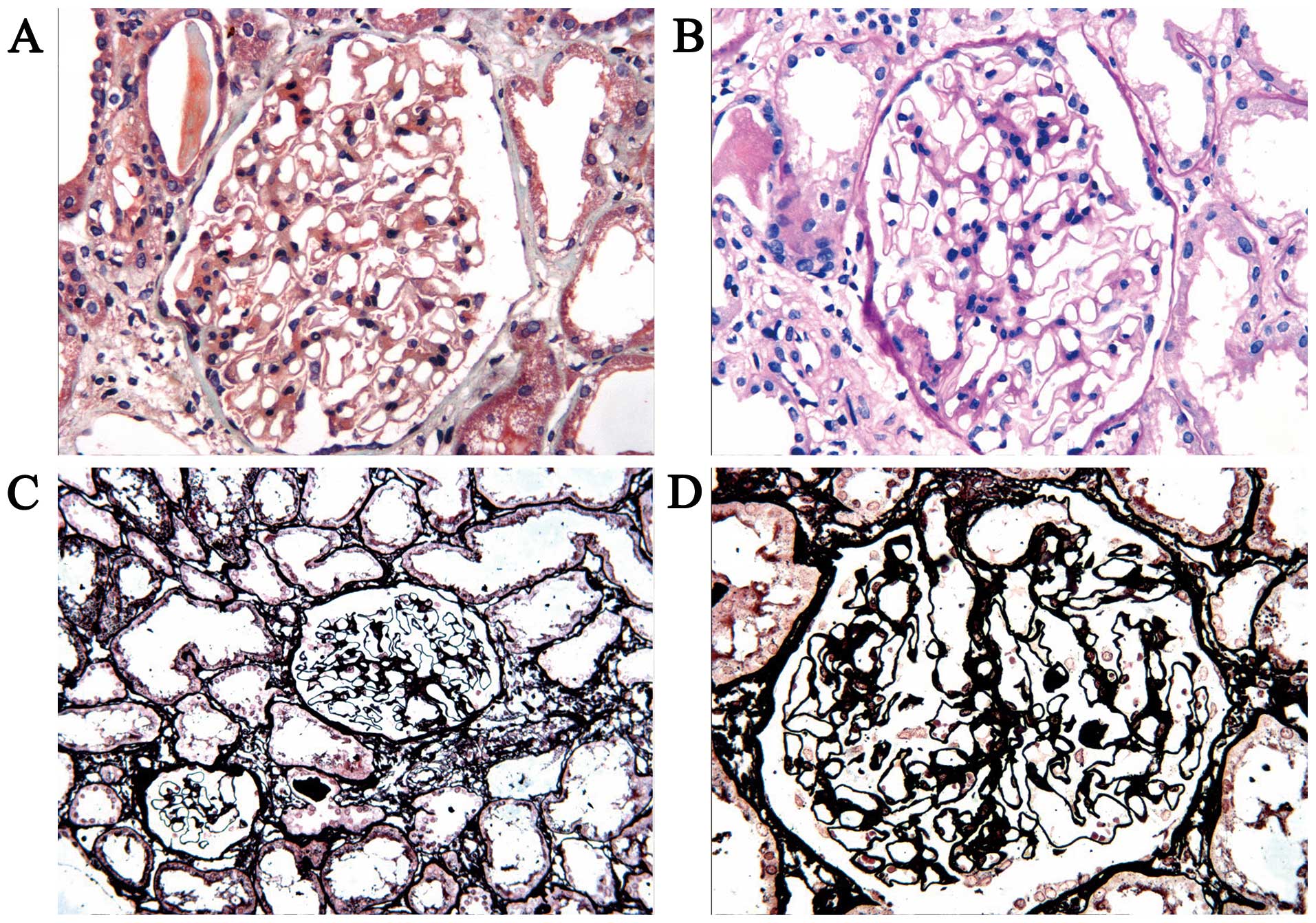
Pathological examination of renal tissue sections
was performed by the pathologist of our hospital. The
immunofluorescent stains for immunoglobulin (Ig)G and IgM, IgA and
C3 were negative. Under a light microscope, the glomeruli exhibited
a mild hypercellularity of the mesangial cells and matrix, basement
membrane thickening and a stiff appearance. However, no spikes were
observed (Fig. 1).
On pleural biopsy examination, epithelial cells
arranged in papillary formations or sheets were observed, with
blood clots and fibrillar connective tissue. Some of the nuclei had
inclusion bodies. On immunohistochemical examination, CK19, CD5,
CR, HBME-1, Ki-67, WT-1 and CK5/6 were positive, whereas TTF-1 and
CEA were negative (Fig. 2).
The patient was diagnosed with pleural mesothelioma
associated with membranous nephropathy. Pemetrexed and cisplatin
combination chemotherapy was administered (pemetrexed 850 mg with
cisplatin 60 mg, once per month). After the first cycle of
chemotherapy, the urine protein was reduced to 1+ on urine routine
tests. However, the patient developed myelosuppression and did not
receive the second cycle of chemotherapy in time; the 24-h urine
total protein increased to 13.78 g. After 5 months, the patient was
in a stable condition and received the second cycle of
chemotherapy. However, pemetrexed and cisplatin-induced
myelosuppression developed again and the patient succumbed to the
disease 2 weeks after the second cycle due to extensive
dissemination and severe infection.
Written informed consent was obtained from the
patient's family for the publication of the case details.
Discussion
In the present case, the patient's first clinical
manifestation was nephrotic syndrome. The result of renal biopsy
result was membranous nephropathy stage I, and the anti-PLA2R
antibody was negative; 4 years later, he was diagnosed with MPM and
the proteinuria was aggravated with the progression of the MPM. the
patient was diagnosed with membranous nephropathy associated with
MPM. Furthermore, membranous nephropathy secondary to MPM is
possible; membranous nephropathy may be idiopathic or secondary,
with the common causes of the secondary type being infection,
systemic lupus erythematosus, malignancy or medication. Anti-PLA2R
may be used for the differential diagnosis of idiopathic and
secondary membranous nephropathy (2).
Mesothelioma is a tumor derived from mesothelial
tissue, often involving the peritoneum, pleura and pericardium.
Approximately 80% of pleural mesotheliomas have been linked to
asbestos exposure. However, malignant mesothelioma and nephrotic
syndrome have been less extensively investigated. A total of 7
cases of nephrotic syndrome associated with malignant mesothelioma
have been reported in the English literature (3–9); the
details of these 7 cases are listed in Table I.
 | Table I.Cases of nephrotic syndrome associated
with malignant mesothelioma in the literature. |
Table I.
Cases of nephrotic syndrome associated
with malignant mesothelioma in the literature.
| Authors (Refs.) | Age, years | Gender | Tumor site | Renal biopsy
result | Main treatment | Outcome |
|---|
| Schroeter et
al (3) | 68 | Male | Pleura | MCN | Prednisone +
cyclophosphamide + doxorubicin hydrochloride + dacarbazine | Died |
| Tanaka et al
(4) | 77 | Male | Pleura | MPG | Carboplatin +
etoposide + glucocorticoid | Died |
| Dogan et al
(5) | 42 | Female | Pleura | Refused | Debulking
surgery | Improvement |
| Galesic et al
(6) | 67 | Male | Pleura | MN | Methylprednisolone in
respiratory decompensation | Died |
| Suzuki et al
(7) | 64 | Male | Pleura | MCN | Prescription of a
diuretic and anticoagulant | Died of respiratory
failure |
| Bacchetta et
al (8) | 63 | Male | Tunica vaginalis
testis | MCN | Prednisolone +
cisplatin + pemetrexed + radiotherapy | Died of disease
progression |
| Farmer and Goldsmith
(9) | 66 | Male | Pleura, pericardium,
brain | MCN | Prednisolone
respiratory + circulatory failure | Died of |
Among the 7 cases reviewed, 6 had a history of
asbestos exposure, 1 had a history of prolonged tobacco exposure
and in only 1 case the renal pathology result indicated membranous
nephropathy (the pleural mesothelioma was diagnosed on autopsy). In
the present case, the patient did not have a history of asbestos or
tobacco exposure; he had membranous nephropathy, was diagnosed with
malignant mesothelioma by means of a pleural biopsy and received
the treatment for both conditions.
The prognosis of patients with membranous
nephropathy and MPM is poor and the patients usually succumb to the
cancer. The current treatment of MPM is multimodality therapy,
including surgical resection, radiation therapy, chemotherapy and
immunotherapy. The combination of cisplatin and pemetrexed is used
as first-line treatment for MPM. Compared with cisplatin alone,
combination chemotherapy was shown to improve the median survival
from 9.3 to 12.1 months (10,11). In our case, the patient received
treatment with pemetrexed and cisplatin; however, he only received
one cycle of chemotherapy and finally succumbed to the disease 6
months after the first cycle.
In summary, we herein present a case of membranous
nephropathy associated with MPM. Based on the diagnosis and
treatment of this case, we hypothesize that there are certain
correlations between malignant mesothelioma and membranous
nephropathy. Thus, when a patient is diagnosed with membranous
nephropathy, secondary factors must be excluded.
References
|
1
|
Scherpereel A, Astoul P, Baas P, Berghmans
T, Clayson H, de Vuyst P, Dienemann H, Galateau-Salle F, Hennequin
C, Hillerdal G, et al: Guidelines of the European respiratory
society and the European society of thoracic surgeons for the
management of malignant pleural mesothelioma. Eur Respir J.
35:479–495. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Santos FR: Membranous glomerulonephritis:
New insights in pathophysiology and therapeutic approach. J Bras
Nefrol. 36:59–62. 2014.(In Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schroeter NJ, Rushing DA, Parker JP and
Beltaos E: Minimal-change nephrotic syndrome associated with
malignant mesothelioma. Arch Intern Med. 146:1834–1836. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanaka S, Oda H, Satta H, Takizawa T,
Tochikubo O, Takagi N, Ishii M and Kaneko T: Nephrotic syndrome
associated with malignant mesothelioma. Nephron. 67:510–511. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dogan M, Ozal G, Savas B, Gungor M, Utkan
G, Yalcin B and Icli F: Malign peritoneal mesothelioma with
nephrotic syndrome. Bratisl Lek Listy. 113:43–45. 2012.PubMed/NCBI
|
|
6
|
Galesic K, Bozic B, Heinzl R,
ScukanecSpoljar M and Bozikov V: Pleural mesothelioma and
membranous nephropathy. Nephron. 84:71–74. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Suzuki S, Toyoshima M, Nihashi F, Tsukui
H, Baba S, Sugimura H and Suda T: An autopsy case of malignant
pleural mesothelioma associated with nephrotic syndrome. Intern
Med. 53:243–246. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bacchetta J, Ranchère D, Dijoud F and Droz
JP: Mesothelioma of the testis and nephrotic syndrome: A case
report. J Med Case Rep. 3:72482009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Farmer CK and Goldsmith DJ: Nephrotic
syndrome and mesenteric infarction secondary to metastatic
mesothelioma. Postgrad Med J. 77:333–334. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
vanZandwijk N, Clarke C, Henderson D, Musk
AW, Fong K, Nowak A, Loneragan R, McCaughan B, Boyer M, Feigen M,
et al: Guidelines for the diagnosis and treatment of malignant
pleural mesothelioma. J Thorac Dis. 5:E254–E307. 2013.PubMed/NCBI
|
|
11
|
Vogelzang NJ, Rusthoven JJ, Symanowski J,
Denham C, Kaukel E, Ruffie P, Gatzemeier U, Boyer M, Emri S,
Manegold C, et al: Phase III study of pemetrexed in combination
with cisplatin versus cisplatin alone in patients with malignant
pleural mesothelioma. J Clin Oncol. 21:2636–2644. 2003. View Article : Google Scholar : PubMed/NCBI
|