Introduction
Bladder cancer is a very common cancer of the
urinary system and the ninth most common type of cancer worldwide,
with a reported 386,000 new cases leading to 150,000 deaths
worldwide in 2014 (1). The majority
of bladder cancer cases (90–95%) are urothelial carcinomas, with
squamous cell carcinoma and adenocarcinoma representing only 3 and
2% of the cases, respectively (2,3). The
mucinous adenocarcinoma subtype is extremely rare (4). According to a previous study, there is a
progressive change from mucinous metaplasia to mucinous adenoma to
mucinous adenocarcinoma (5). Patients
with bladder exstrophy and urachal remnants are at higher risk of
developing bladder adenocarcinoma (6). It was also suggested that chronic
inflammatory processes of the bladder mucosa induce metaplastic
changes to the more protective squamous cell or glandular-type
epithelium (7).
Bladder adenocarcinoma is resistant to chemotherapy
and radiation, and surgery is currently considered the most
effective treatment option (8). Thus,
early diagnosis is crucial; however, early diagnosis may be
difficult, as the clinical characteristics of bladder mucinous
adenocarcinoma are similar to those of other bladder cancers. The
most common symptoms are hematuria, suprapubic pain, and dysuria
(9). The most effective diagnostic
investigations are urinary cytology, cystoscopy, and biopsy
followed by histopathological evaluation. Due to the rarity of this
tumor, and the relative lack of clinical reports, we herein report
the case of a patient with mucinous adenocarinoma of the bladder to
help elucidate the characteristics of this tumor.
Case report
The patient was a 59-year-old female, menopausal,
non-smoker and non-drinker, who presented with epigastric pain for
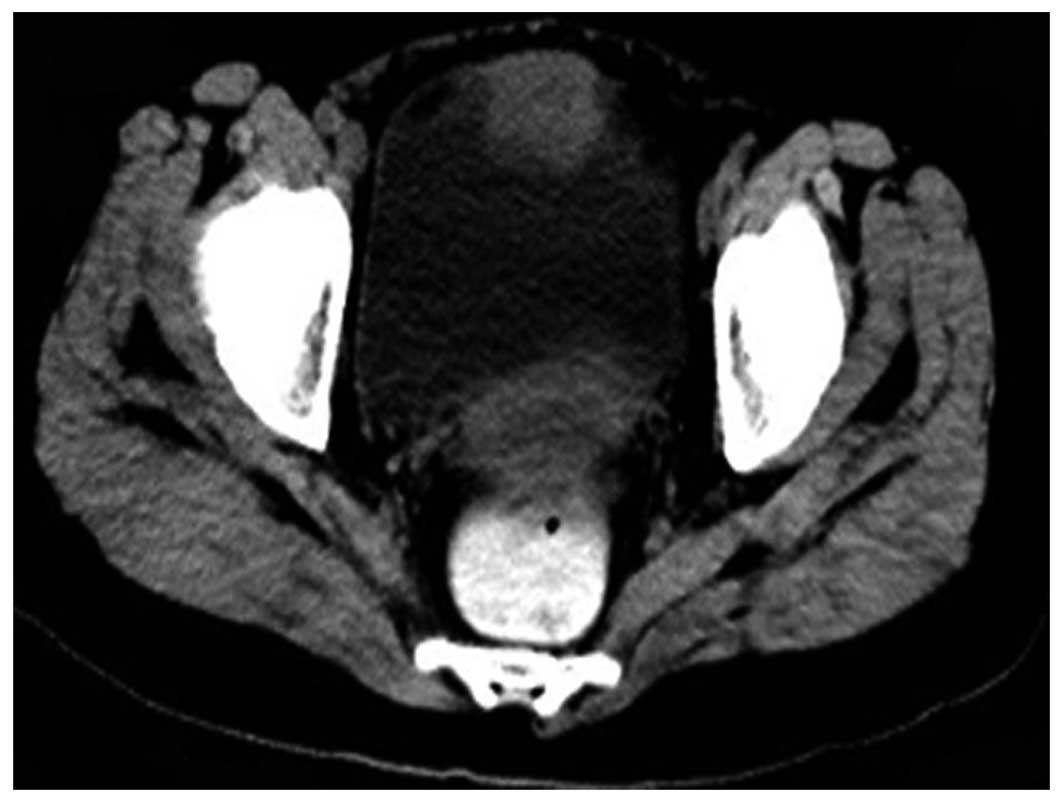
5 months. The computed tomography (CT) scan of the abdomen revealed
a mass located in the anterior bladder wall, sized 5.0×3.4 cm. The
surrounding bladder wall was thickened, with no abnormal findings
in the pelvic cavity (Fig. 1).
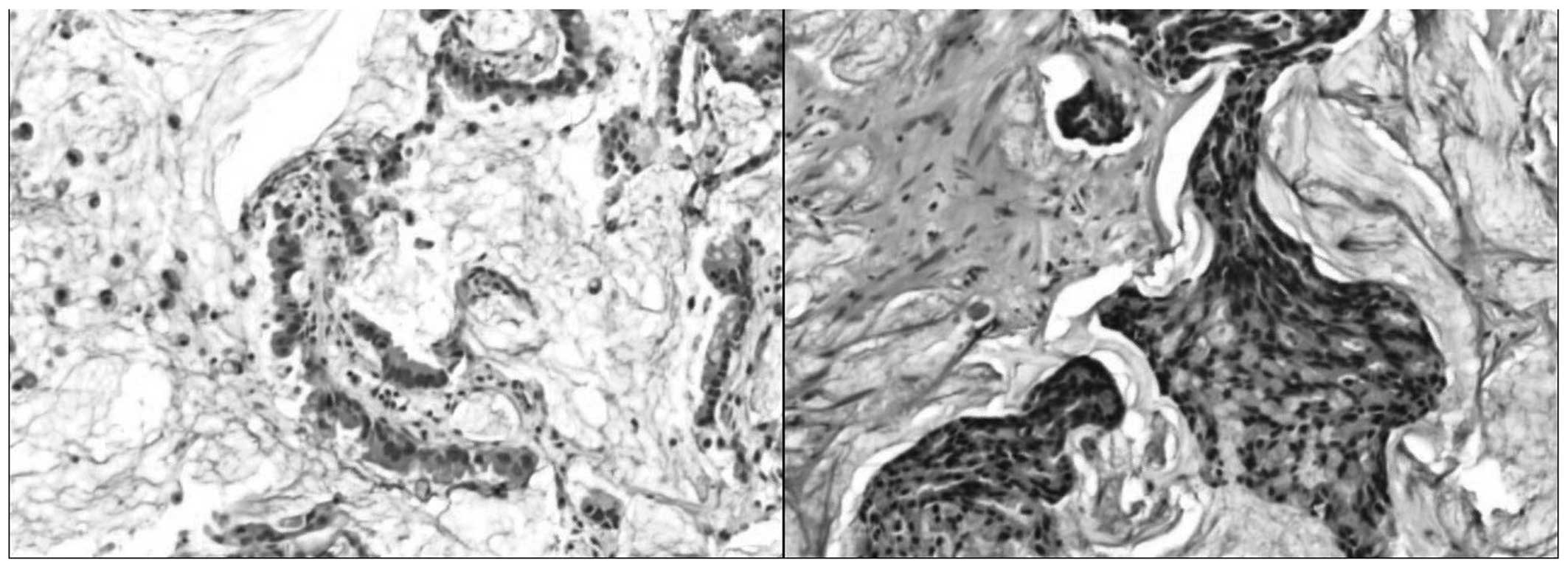
Transurethral resection of the bladder tumor with electrocautery
was undertaken to investigate the tumor. The pathological results
revealed the presence of a significant amount of mucus, with
irregular cell cords surrounding the mucus pools. Therefore, the
suspected diagnosis was mucinous bladder adenocarcinoma (Fig. 2).
Radical resection and bilateral ureterostomy was
planned; however, when the abdominal cavity was opened, the tumor
was found to have invaded the greater omentum and peritoneum.
Therefore, the cancer of the patient was considered as advanced,
with significant local invasion and, thus, inoperable. Three months
later, the patient succumbed to the disease.
Discussion
Mucinous adenocarcinoma of the bladder is a rare
type of cancer, accounting for <2% of all bladder cancers
(10). It usually appears at the
bladder dome, trigone and lateral wall. There are three hypotheses
regarding the histological origin: The first is urachal remnants in
the bladder; the second is a vestigial embryonal gland in the
transitional epithelium of the bladder; and the third is the
transitional epithelium of the bladder undergoing glandular
metaplasia. Glandular cystitis is widely considered as a
precancerous condition for bladder adenocarcinoma. The mucosa in
bladder adenocarcinoma is not smooth, resembling edematous surface
villi, or even papilloma-like changes on cystoscopy. The
accumulation of secretions and associated infection may promote the
development of adenocarcinoma.
As the adenocarcinoma cells secrete copious amounts
of mucus, mucous floccules may be discharged from the bladder
during micturition or cystoscopy. The main primary symptom is
hematuria, with or without signs of irritation of the bladder. A
proportion of the patients may only present with signs of bladder
irritation and difficulty urinating.
Distinguishing between mucinous bladder
adenocarcinoma and urachal carcinoma is crucial, but may be
challenging, as their presentations may be similar. The primary
clinical signs of bladder adenocarcinoma are hematuria and dysuria,
whereas mucusuria is observed in ~90% of urachal carcinomas.
Furthermore, the treatment of urachal carcinoma is partial
cystectomy with en bloc resection of the urachus, rather than
radical cystectomy. In addition, urachal carcinoma has a better
prognosis and high survival rate compared with mucinous
adenocarcinoma of the bladder (11).
The prognostic factors of the cancer include tumor
stage, grade and subtype. According to a previous study, if the
cancer is limited to the bladder, the survival rate may exceed 75%
(6). At this stage, the ultrasound
appearance may resemble urinary tract infection (6). Grignon et al identified 5 ubtypes
of bladder adenocarcinoma: i) Papillary; ii) mucinous; iii)
signet-ring cell; iv) adenocarcinoma not otherwise specified; and
v) mixed. The signet-ring cell type has a poorer prognosis compared
with that of the other types of adenocarcinoma (12).
The growth pattern of adenocarcinoma cells mainly
involves infiltration into the deep muscular layer; thus,
cystoscopy and B-mode ultrasound may be unable to assess the extent
of infiltration. Therefore, the majority of bladder mucinous
adenocarcinoma patients are stage T2 or T3 at diagnosis.
When a tumor is identified at the bladder dome,
trigone or lateral wall, or in patients presenting with mucous
floccules discharged from the bladder during micturition or
cystoscopy, the presence of bladder adenocarcinoma should be taken
into consideration. Tumor tissue biopsy and CT are required.
Several random biopsy samples and regular follow-up visits are also
required for patients with glandular cystitis. Bladder
adenocarcinoma is resistant to chemotherapy and radiation; thus,
for patients with confirmed or highly suspicious mucinous
adenocarcinoma of the bladder, timely radical resection is
warranted.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (no. 81101922), the
Science and Technology Development Fund Project of Shenzhen (nos.
JCY20130402114702124 and JCY20150403091443329) and funds from the
Guangdong Key Medical Subject.
References
|
1
|
Chavan S, Bray F, Lortet-Tieulent J,
Goodman M and Jemal A: International variations in bladder cancer
incidence and mortality. Eu Urol. 66:59–73. 2014. View Article : Google Scholar
|
|
2
|
Black PC, Brown GA and Dinney CP: The
impact of variant histology on the outcome of bladder cancer
treated with curative intent. Urol Oncol. 27:3–7. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kantor AF, Hartge P, Hoover RN and
Fraumeni JF Jr: Epidemiological characteristics of squamous cell
carcinoma and adenocarcinoma of the bladder. Cancer Res.
48:3853–3855. 1988.PubMed/NCBI
|
|
4
|
Sigalas K, Tyritzis SI, Trigka E,
Katafigiotis I, Kavantzas N and Stravodimos KG: A male presenting
with a primary mucinous bladder carcinoma: A case report. Cases J.
3:492010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang BY, Aguilar J, Yang M, Wang P and Li
B: Mucinous metaplasia in urothelial tract may be the precancerous
lesion of mucinous adenocarcinoma: Report of two cases and review
of literature. Int J Clin Exp Med. 7:285–289. 2014.PubMed/NCBI
|
|
6
|
Santos BM, de Souza JD, Lima RS and de
Lima EM: Mucinous bladder adenocarcinoma: Case report and
literature review. Case Rep Urol. 2015:7831092015.PubMed/NCBI
|
|
7
|
Bullock PS, Thoni DE and Murphy WM: The
significance of colonic mucosa (intestinal metaplasia) involving
the urinary tract. Cancer. 59:2086–2090. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baffigo G, Delicato G, Bianchi D, Signore
S, Tartaglia E, Corvese F, Perla A, Marino B, Santeusanio G and
Ferdinandi V: Mucinous adenocarcinoma of the urinary bladder. Am J
Case Rep. 13:99–101. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zaghloul MS, Nouh A, Nazmy M, Ramzy S,
Zaghloul AS, Sedira MA and Khalil E: Long-term results of primary
adenocarcinoma of the urinary bladder: A report on 192 patients.
Urol Oncol. 24:13–20. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bates AW and Baithun SI: Secondary
neoplasms of the bladder are histological mimics of nontransitional
cell primary tumours: Clinicopathological and histological features
of 282 cases. Histopathology. 36:32–40. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wright JL, Porter MP, Li CI, Lange PH and
Lin DW: Differences in survival among patients with urachal and
nonurachal adenocarcinomas of the bladder. Cancer. 107:721–728.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fiter L, Gimeno F, Martin L and Tejeda L
Gómez: Signet-ring cell adenocarcinoma of bladder. Urology.
41:30–33. 1993. View Article : Google Scholar : PubMed/NCBI
|