Introduction
Cancer-related secondary lymphedema is a
pathological condition that develops following obstruction of the
lymphatic system by direct invasion, metastasis, surgical removal,
or irradiation of the lymph nodes (1). Lymphedema may occur months to years
following treatment for breast and gynecological cancers with lymph
node removal, or obstruction of the lymphatic system by irradiation
or metastases (1,2). We recently encountered two advanced lung
adenocarcinoma patients with lower limb lymphedema, who achieved
long-term survival with epidermal growth factor receptor
(EGFR)-tyrosine kinase inhibitors (TKIs) or anaplastic lymphoma
kinase (ALK)-TKIs. To the best of our knowledge, these are the
first advanced lung adenocarcinoma cases who developed lymphedema
in the lower extremities long after receiving molecular-targeted
therapies.
Case reports
Case 1
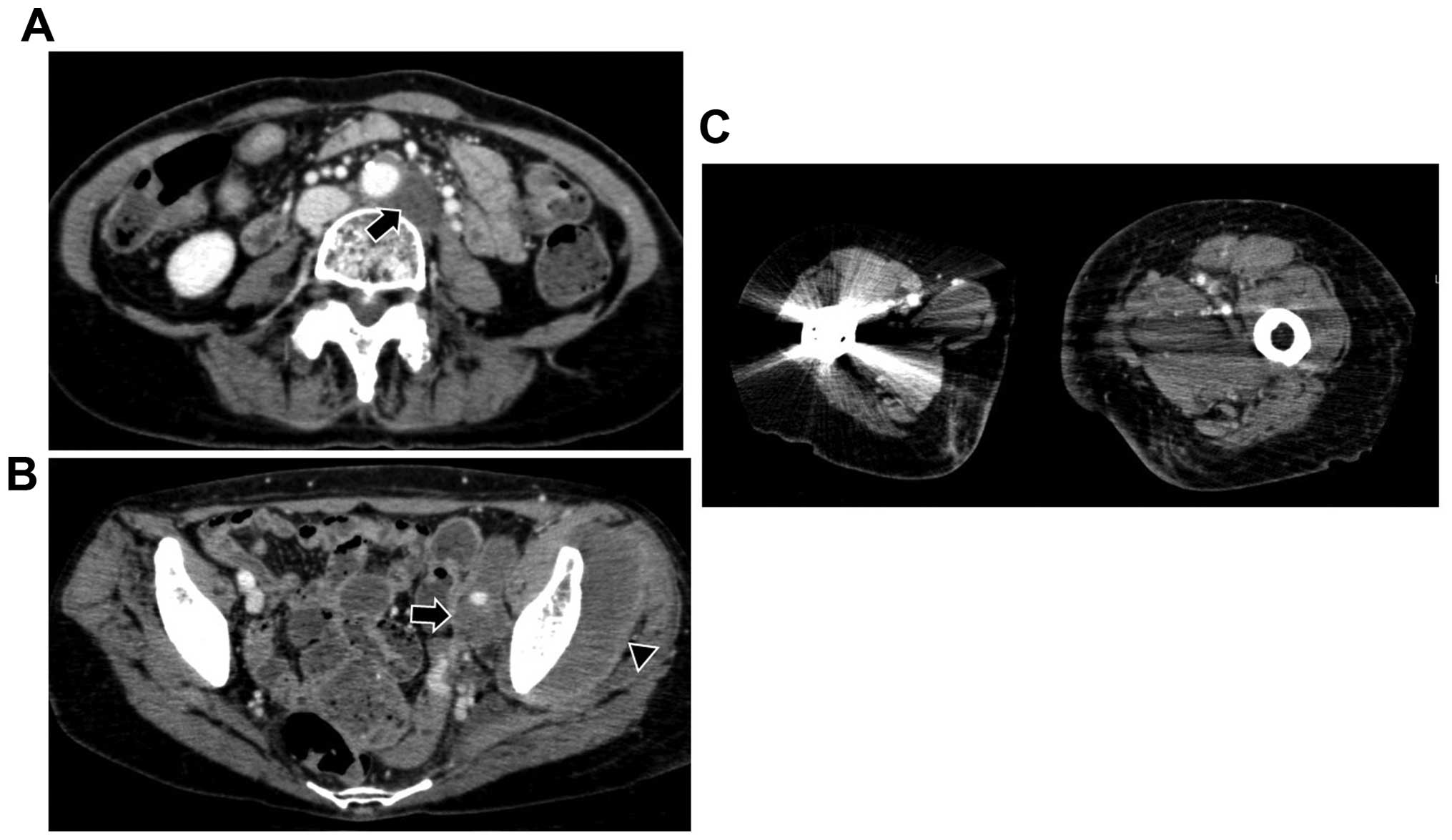
A 63-year-old female patient was diagnosed with
T2aN3M1b lung adenocarcinoma with an EGFR mutation (exon 19
deletion). The patient had received 5 types of chemotherapeutic
regimens, including two types of EGFR-TKIs. At 33 months after
therapy initiation, the patient developed intra-abdominal lymph
node, pelvic bone and left femoral metastases, and severe edema in
the left leg (Fig. 1). Within a
2-week period, the edema expanded to involve the right leg. The
patient was diagnosed with lymphedema due to lymphatics obstruction
by the intra-abdominal lymph node, pelvic bone and femoral
metastases. No edema was observed in other sites, including the
trunk, upper extremities and face. Radiation therapy for the
metastatic sites was unsuccessful in controlling lymphedema and the
patient succumbed to lung adenocarcinoma 2 months after the
development of lymphedema.
Case 2
A 41-year-old male patient was diagnosed with
T4N3M1b lung adenocarcinoma with an ALK fusion gene. The patient
had received 4 types of chemotherapeutic regimens, including two
types of ALK inhibitors. At 37 months after the initiation of
therapy, the patient developed liver and intra-abdominal lymph node
metastases, with edema in both lower limbs. The patient was
diagnosed with lymphedema due to lymphatics obstruction by
intra-abdominal lymph node metastases. There was no edema in other
sites, including the trunk, upper extremities and face. No specific
therapy was successful in controlling lymphedema and the patient
succumbed to lung adenocarcinoma 1 month after the development of
lymphedema.
Discussion
Survival among patients with advanced lung
adenocarcinoma has steadily improved (3). The cornerstone of management for lung
adenocarcinoma with a specific genetic etiology, such as EGFR
mutations and ALK fusion gene, is molecular-targeted therapy, with
the aim being long-term administration. Therefore, survival,
particularly in those with a specific genetic etiology, has
significantly improved (3–5). Improvements in survival, however, may be
accompanied by long-term sequelae, including meningitis
carcinomatosa, an issue that has recently attracted attention
(6,7).
Cancer-related secondary lymphedema of the
extremities is a pathological condition that develops following
obstruction of the lymphatic system by direct invasion or
metastasis, or treatments such as surgical removal or irradiation
(1). However, lymphedema, which is
acute or chronic edema associated with disruption of the lymphatic
system, is a perplexing and poorly understood clinical entity
(1,2).
It is well-documented in the literature that patients with breast
cancer experience lymphedema of the upper extremities secondary to
surgical resection of lymph vessels and nodes, from radiation or
obstruction of the lymphatic system by metastatic cancer (1). Petrek and Heedan reported that the
incidence of lymphedema in breast cancer patients ranged from 6 to
30% (8). The incidence may vary
according to the source of patients, duration of follow-up and
measurement techniques; in addition, the definition of lymphedema
may vary across studies. In general, reports with shorter follow-up
reported lower incidences of lymphedema (8). Patients with gynecological cancers
experience lymphedema in the lower extremities (1,2). Beesley
et al reported that approximately one-fifth of ovarian
cancer patients develop lymphedema (9). Rehabilitation therapy for post-treatment
effects from cancer and its treatment is required to improve
functioning and quality of life (10). In patients with distant metastatic
recurrence and a poor performance status, however, rehabilitation
may be challenging.
We herein report two cases of patients with advanced
lung adenocarcinoma who developed lymphedema in the lower
extremities following long-term survival with the use of EGFR-TKIs
or ALK-TKIs. Both patients had developed intra-abdominal lymph node
metastases, which may have caused obstruction of the lymphatic
system. No therapy was able to control lymphedema and the patients
succumbed to the disease shortly after the development of
lymphedema. Metastases to lower parts of the body, including the
intra-abdominal lymph nodes, may increase the risk of lymphedema by
further lymphatics obstruction in these patients. To the best of
our knowledge, these are the first two reported cases of lymphedema
in the lower extremities following molecular-targeted therapies for
advanced non-small-cell lung cancer (NSCLC). It should be kept in
mind that lymphedema in the lower extremities may develop long
after successful therapy with molecular-targeted therapy in
advanced NSCLC patients with a specific genetic etiology.
References
|
1
|
Jakes AD and Twelves C: Breast
cancer-related lymphoedema and venepuncture: A review and
evidence-based recommendations. Breast Cancer Res Treat.
154:455–461. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Casey C, Chen LM and Rabow MW: Symptom
management in gynecologic malignancies. Expert Rev Anticancer Ther.
11:1077–1089. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bareschino MA, Schettino C, Rossi A,
Maione P, Sacco PC, Zeppa R and Gridelli C: Treatment of advanced
non small cell lung cancer. J Thorac Dis. 3:122–133.
2011.PubMed/NCBI
|
|
4
|
Thomas A, Liu SV, Subramaniam DS and
Giaccone G: Refining the treatment of NSCLC according to
histological and molecular subtypes. Nat Rev Clin Oncol.
12:511–526. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gerber DE, Gandhi L and Costa DB:
Management and future directions in non-small cell lung cancer with
known activating mutations. Am Soc Clin Oncol Educ Book.
2014:e353–e365. 2014. View Article : Google Scholar
|
|
6
|
Togashi Y, Hayashi H, Nakagawa K and
Nishio K: Clinical utility of erlotinib for the treatment of
non-small-cell lung cancer in Japanese patients: Current evidence.
Drug Des Devel Ther. 8:1037–1046. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Le Rhun E, Taillibert S and Chamberlain
MC: Carcinomatous meningitis: Leptomeningeal metastases in solid
tumors. Surg Neurol Int. 4(Suppl 4): S265–S288. 2013.PubMed/NCBI
|
|
8
|
Petrek JA and Heelan MC: Incidence of
breast carcinoma-related lymphedema. Cancer. 83:(12 Suppl
American). S2776–S2781. 1998. View Article : Google Scholar
|
|
9
|
Beesley V, Janda M, Eakin E, Obermair A
and Battistutta D: Lymphedema after gynecological cancer treatment:
Prevalence, correlates and supportive care needs. Cancer.
109:2607–2614. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Loh SY and Musa AN: Methods to improve
rehabilitation of patients following breast cancer surgery: A
review of systematic reviews. Breast Cancer (Dove Med Press).
7:81–98. 2015.PubMed/NCBI
|